Abstract
Objective
Recent research suggests that self-esteem may be associated with improved parasympathetic nervous system functioning. This study tested whether high self-esteem is associated with decreased ambulatory systolic blood pressure (ASBP) reactivity to anxiety in healthy adults during the waking hours of a normal day.
Methods
Each of 858 participants completed a short version of the Rosenberg Self-Esteem Scale and then wore an ABP monitor which took two blood pressure readings per hour for 24 hours. Immediately after each blood pressure reading, participants completed an electronic diary report that included an anxiety rating on a 100-point visual analog scale (VAS). Using multilevel models, we assessed the association of momentary anxiety, high trait self-esteem, and their interaction on momentary ASBP, with adjustment for age, sex, race, ethnicity, and body mass index. Sensitivity analyses were conducted examining psychological factors associated with self-esteem: sense of mastery, optimism, social support, and depressive symptoms.
Results
On average, a 1-point increase in cube root-transformed anxiety was associated with a 0.80 mmHg (SE=0.09, p<0.001) increase in ASBP, and the interaction of high self-esteem and momentary anxiety was significant, such that this effect was 0.48 (SE=0.20, p=0.015) less in individuals with high self-esteem compared to all others. Results for self-esteem remained significant when adjusting for sex and psychological factors.
Conclusions
Momentary increases in anxiety are associated with acute increases in ASBP, and high self-esteem buffers the effect of momentary anxiety on blood pressure. Thus, high self-esteem may confer cardiovascular benefit by reducing the acute effects of anxiety on systolic blood pressure.
Keywords: ambulatory blood pressure, anxiety, self-esteem, ecological momentary assessment, autonomic, cardiovascular
Self-esteem is a foundational psychological construct. Few other constructs have been found to influence so many different aspects of human functioning and well-being. People with high self-esteem, on average, are happier, suffer fewer mental disorders, enjoy greater interpersonal and career success, and cope better with the trials and tribulations of life than people with low self-esteem.1 Although there are drawbacks to high but unstable self-esteem,2 the noted benefits of high self-esteem across many domains have led researchers over the years to theorize that high self-esteem may also have beneficial effects on physical health e.g.,3,4–6. Despite important progress toward elucidating biological mechanisms by which self-esteem may affect physical health, few studies have examined these processes as they occur in the context of people’s daily lives.
Self-esteem, the cardiovascular system, and health
In the last decade or so, there has been a resurgence of interest in connections between self-esteem, anxiety, and the cardiovascular system. Large prospective cohort studies have documented that anxiety is associated with increased risk for cardiovascular disease (CVD) and mortality in initially healthy participants.7 The mechanisms by which anxiety is hypothesized to influence CVD incidence and mortality are numerous, but one primary candidate is through hypertension (high blood pressure)8 or transient increases in blood pressure even in normotensives. Acute blood pressure elevations are regulated primarily by the autonomic nervous system, which activates the cardiovascular system in order to prepare the body to respond to threats. Systolic blood pressure is particularly responsive to fluctuations in anxiety and stress.9–11 Chronic feelings of anxiety are thought to lead to chronically high blood pressure due to the accumulation of momentary blood pressure responses to threat.12,13 Finally, this increased blood pressure is harmful to the coronary arteries, contributing to arterial stiffness, plaque formation, plaque rupture, and acute coronary events.14 Hypertension is the strongest predictor of cardiovascular risk, and anxiety has been associated with hypertension both cross-sectionally and prospectively.13,15
A number of theories of self-esteem converge on its potential to buffer the effects of stress and anxiety, and potentially reduce blood pressure reactivity to stressful or anxiety-provoking experiences.16–19 Indeed, the anxiety-buffering function of self-esteem is a fundamental postulate of Terror Management Theory (TMT). Martens et al.20 recently extended this analysis to propose that high self-esteem buffers the cardiovascular response to perceptions of threat. According to TMT, humans derive a sense of security from feelings of meaning and self-worth that come from living up to the standards set forth by shared symbolic worldviews. Measures of self-esteem, then, indicate the extent to which an individual feels securely situated within a functioning worldview, and is thereby less vulnerable to feelings of anxiety and their cardiovascular sequelae. Martens et al. demonstrated in two studies that experimentally manipulated increases in self-esteem were associated with increased cardiac vagal tone (an indicator of parasympathetic autonomic activity), and in two small correlational studies that daily ratings of self-esteem averaged over two weeks were positively associated with resting cardiac vagal tone.21
In a similar vein, studies have shown that experimentally manipulated boosts to self-esteem can buffer cardiovascular responses to laboratory induced psychological stress22,23 while negative self-relevant feedback can impair physiological recovery from stress.24 Taken together, these findings suggest that when feeling threatened or anxious, high self-esteem may buffer individuals against the cardiovascular consequences of those feelings. However, to our knowledge, no study has yet tested the fundamental prediction that individuals with high self-esteem demonstrate a blunted cardiovascular response to momentary feelings of anxiety as they navigate their daily lives.
Present study
The present study tests the anxiety buffering effect of high trait self-esteem throughout the waking hours of a 24-hour period in a large sample of working adults using ecological momentary assessment (EMA) of anxiety and ambulatory blood pressure monitoring (ABPM). We tested the hypotheses that high self-esteem would be associated with less reported anxiety and lower average awake ambulatory systolic blood pressure (ASBP) during the 24-hour monitoring period. More importantly, we also examined the novel hypothesis that high self-esteem would (partially) buffer the increase in blood pressure that is otherwise observed in response to momentary experiences of anxiety. While previous studies have shown an association of self-esteem with cardiovascular functioning and self-reports of anxiety, this is the first study to directly test the hypothesis that self-esteem functions as a buffer against the acute cardiovascular effects of momentary anxiety outside the laboratory.
Method
The present study uses data from the multi-site Masked Hypertension Study,25 an investigation of the relationship of different blood pressure measures to cardiovascular target organ damage. The study was approved by the Institutional Review Boards of Columbia University Medical Center and Stony Brook University. Participants were employees recruited through workplace blood pressure screenings between 2005–2011 at two universities, their medical centers, and a financial investment firm. All participants gave informed consent to participate. Eligibility for the study was restricted to employees (at least 17.5 hours/week) aged 21 or older. Exclusion criteria included any of the following: a screening clinic systolic blood pressure (SBP) > 160 mmHg or diastolic blood pressure (DBP) > 105 mmHg, evidence of secondary hypertension other than a history of pregnancy-induced hypertension, taking antihypertensive medications or other medications that are known to affect blood pressure (e.g., steroids, tricyclic antidepressants), any self-reported cardiovascular disease, history of chronic renal disease, liver disease, adrenal disease, thyroid disease, being pregnant, or reported active substance abuse or a severe debilitating psychiatric disorder. Of the 1010 individuals who enrolled in this study, 894 completed the first four (of five) visits, thereby providing the ABPM and EMA data necessary for inclusion in this report. Of these 894, 32 were missing data on the trait self-esteem measure, the ABPM device failed for 1 and the electronic diary device failed for 3, resulting in a final sample size for the present analyses of 858 participants. The mean age was 45 ± 10 years (range 21–81), 41% were men, 28% identified as members of racial/ethnic minority groups (including 12% Hispanic and 7% Black), and 92% had more than a high school education, including 39% with more than 4 years of college. Importantly, the mean awake ambulatory systolic blood pressure in the sample was 123.1 mmHg (SD=10.3) – well within the normotensive range (<120 mmHg is optimal, >140 mmHg indicates hypertension).
At recruitment, participants were given a psychosocial questionnaire battery to complete at home which included an assessment of trait self-esteem. During the third of five study visits, participants were outfitted with an ABP monitor, programmed to take a blood pressure reading every 28 minutes, and an electronic diary on which they made entries immediately after each blood pressure reading. Participants returned the ABPM and electronic diary at the end of the 24-hour monitoring period.
Materials
Self-esteem assessment
As part of the questionnaire battery completed by participants, trait self-esteem was measured using a 4-item short form26 of the Rosenberg Self-Esteem Scale (I feel that I have a number of good qualities; I am able to do things as well as most other people; I feel that I am a person of worth, or at least on an equal basis as others; I take a positive attitude toward myself), rated on a scale of 0 “Strongly Disagree” to 3 “Strongly Agree” (α = 0.85). The self-esteem scores have a bimodal distribution (see Figure 1), with a modal score of 8 but more than 25% had the maximum possible score. Participants in this top quartile who endorsed “Strongly Agree” for all 4 items (total score= 12) were categorized as having high self-esteem. The remaining participants reported a mean self-esteem score of 8.8 (SD = 1.3). Issues with the dichotomous approach to categorizing self-esteem are addressed later in the Results section, where sensitivity analyses examining the effect of alternative strategies for handling self-esteem are reported.
Figure 1.
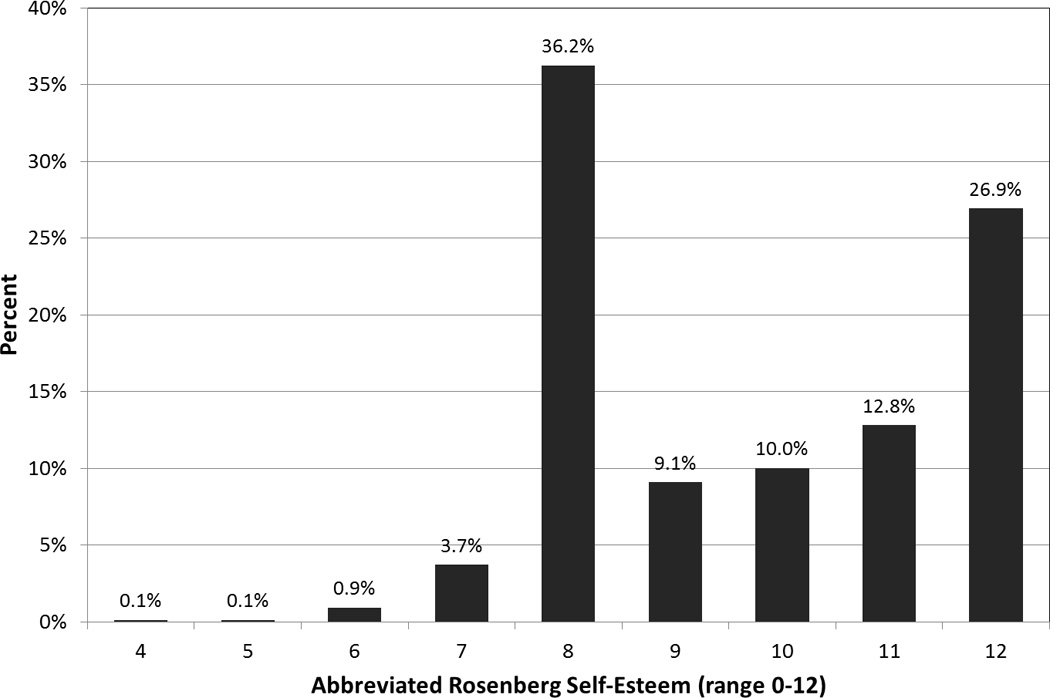
The distribution of the trait measure of self-esteem, N=858
Ecological momentary assessment (EMA) of anxiety
Immediately after each awake blood pressure reading, participants used a pre-programmed electronic diary (Palm Pilot Tungsten 3) to answer questions regarding their situation, activities and affect immediately prior to the blood pressure assessment. Participants rated their anxiety on a 2.5” horizontal visual analog scale (VAS) by responding to the question “Just before [your] BP [was taken], how anxious/tense were you feeling?” using anchors of “not at all” and “very much.” The distribution of anxiety ratings (0 to 100 points) were positively skewed, with the person-specific standard deviations (or inter-quartile ranges) also being highly correlated with the person-specific means (or medians); these problematic distributional properties were minimized by transforming the raw scores to their cube root (0→0.55, 1→1, 8→2, 27→3, 64→4, and 100→4.64). We considered several transformations to address these problematic distributional properties, and found that the cube-root transformation was most effective (see Footnote 1).
Ambulatory blood pressure monitoring (ABPM)
Participants underwent 24-h ABPM using a non-invasive portable BP monitor (SpaceLabs, Model 90207, Snoqualmie, WA, USA). Briefly, a BP cuff was fitted to the participant’s non-dominant arm with cuff size determined by upper arm circumference. BP measures were obtained at 28-min intervals throughout the subsequent 24 hours.
Covariates
Known demographic correlates of blood pressure were treated as covariates in all analyses. Age, sex (male=1), Black race (Black=1), and Hispanic ethnicity (Hispanic=1) were self-reported at baseline. Body mass index (BMI) was not assessed until the fifth and final visit to the clinic. Due to missing data for 26 of the 858 participants, we did not include BMI in the primary analyses. However, we performed a sensitivity analysis in which we re-estimated Models 1, 2, and 3 (see below) on the 832 participants with BMI data and the results were unchanged.
Supplementary analyses were conducted to determine whether constructs related to self-esteem (mastery, optimism, social support, depression; assessed in the same psychosocial battery as self-esteem) might function similarly, or confound any association of self-esteem with momentary anxiety, ASBP, or the anxiety-ASBP relationship.
Mastery (α= 0.79) was assessed using the 7-item Pearlin Mastery scale.27 Participants rated their level of agreement (1=strongly disagree to 5=strongly agree) with items such as “I have little control about things that happen to me.”
Optimism (α= 0.80) was assessed using the 10-item Life Orientation Test (LOT-R).28 Participants indicated their degree of agreement with statements such as “In uncertain times, I usually expect the best,” using a 5-point response scale ranging from (0=strongly disagree to 4=strongly agree).
Social Support (α= 0.89) was assessed using the 12-item Interpersonal Support Evaluation List (ISEL).29 Participants indicated their degree of agreement with statements such as “There are several people that I trust to help solve my problems ” using a 4-point response scale ranging from (0=definitely false to 3=definitely true).
Depression (α= .90) was assessed using the 21-item Beck Depression Inventory,30 which measures depressive symptoms based on DSM-IV criteria.
Analytic strategy
We examined the hypotheses that high self-esteem would be associated with less reported anxiety and lower mean awake blood pressure. More importantly, we also examined the novel hypothesis that high self-esteem would help to buffer the increase in blood pressure that is otherwise expected in response to momentary experiences of anxiety. We estimated 3 multilevel models. Model 1 controlled for demographic factors and simultaneously tested a) whether the association between momentary anxiety and ambulatory systolic blood pressure (ASBP) differed significantly across participants and b) whether, on average, momentary anxiety was associated with higher ASBP. Model 2 tested whether there was an independent association of high trait self-esteem with ASBP. Model 3 tested whether the relationship of momentary anxiety to ASBP differed by level of self-esteem (the buffering hypothesis). Model specifications were:
Model 1: SBPit = (B0+δ0i) + B1×Malei + B2×Blacki + B3×Hispanici + B4×Agei + (B5+δ1i)×Anxietyi + εit
Model 2: SBPit = (B0+δ0i) + B1×Malei + B2×Blacki + B3×Hispanici + B4×Agei + (B5+δ1i)×Anxietyi + B6×Self-esteemi + εit
Model 3: SBPit = (B0+δ0i) + B1×Malei + B2×Blacki + B3×Hispanici + B4×Agei + (B5+δ1i)×Anxietyit + B6×Self-esteemi + B7×(Self-esteemi×Anxietyit) + εit
where,
SBPit: systolic blood pressure of person “i” at time “t”,
Bj are fixed effects (i.e., regression coefficients),
δ0i and δ1i are random, person-specific effects for the intercept and the within-person effect of momentary anxiety on SBP, and
εit is the within-person residual.
δ0i and δ1i are assumed to have a multivariate normal distribution with the mean of each equal to zero, causing B0 and B5 to equal the average of all people’s intercepts and average coefficient of Anxiety, respectively.
The εit are assumed to be the sum of two normally distributed components, each having a mean of zero for each person; the first component is assumed to have a first-order autocorrelation pattern with the correlation being an exponential function of the time interval between blood pressure readings; the second component is assumed to have no autocorrelation. This error structure, in conjunction with the random intercept, is the multilevel modeling equivalent of the Kenny and Zautra trait-state-error model.31,32
The significance of each Bj was tested using a t-statistic, calculated as the ratio of the coefficient to its estimated standard error. The Satterthwaite estimate of degrees of freedom is used.
The above models were estimated using the Proc MIXED procedure in SAS (version 9.3; Cary, NC) and were evaluated using 2-tailed, α=0.05 tests of significance. Further details are given in Footnote 2.
Finally, we conducted sensitivity analyses to determine whether other psychological constructs (mastery, optimism, depression) might operate similarly to the hypothesized effects of self-esteem.
Results
Participants
Demographic and study data for participants are presented by self-esteem level in Table 1. In total, the 858 participants completed 20,916 EMA anxiety reports within 6 minutes of an ambulatory blood pressure reading (mean number of reports= 24, SD=7.4). The mean (cube root transformed) anxiety rating in the sample was 1.99 (SD=0.88). When we compute each participant’s median anxiety rating (untransformed), the mean of these medians is 13.2 (SD=16.1). While most of the untransformed anxiety scores were fairly low, 25% of participants had at least one score >=72, 50% of participants have at least one score >=52 and 75% of participants have at least one score >=27. It is important to note that because we analyzed the cube root of anxiety, which ranges from 0.55 to 4.64, more than 90% of participants have at least one score that is above the midpoint of this range. Thus, in the transformed scale, participants used the full range.
Table 1.
Participant characteristics by self-esteem (N=858)
| High Self-Esteem (N=231) |
Low and Moderate Self-Esteem (N=627) |
Test statistic | p-value* | |
|---|---|---|---|---|
| Sex, N(%) male | 86 (37.2%) | 265 (42.3%) | Fisher’s exact | 0.21 |
| Black race, N(%) | 21 (9.1%) | 39 (6.2%) | Fisher’s exact | 0.17 |
| Hispanic ethnicity, N(%) | 31 (13.4%) | 71 (11.3%) | Fisher’s exact | 0.41 |
| Age, years (mean ± sd) | 44.8 ± 10.9 | 45.3 ± 10.2 | t856 = −0.65 | 0.52 |
| Body mass index, kg/m2 (mean ± sd)† | 28.3 ± 5.3 | 27.3 ± 5.3 | t830 = 2.37 | 0.018 |
| Median anxiety score (mean ± sd) | 10.5 ± 14.5 | 14.1 ± 16.5 | Mann-Whitney Z = −3.49 |
<0.001‡ |
| Mean anxiety(1/3) score (mean ± sd) | 1.80 ± 0.87 | 2.06 ± 0.87 | t856 = −3.80 | <0.001 |
| Mean systolic blood pressure (mean ± sd) | 123.4 ± 10.6 | 123.0 ± 10.2 | t856 = 0.57 | 0.57 |
| Hypertension status, N(%) | 10 (4.3%) | 34 (5.4%) | Fisher’s exact | 0.60 |
Based on t-test or Fisher’s exact test, unless otherwise stated
9 (3.9%) of those with high self-esteem and 17 (2.7%) of those with low or moderate self-esteem did not complete the last visit and therefore are missing data for body mass index.
p-value based on Mann-Whitney test because the distribution of Median Anxiety scores is highly skewed
The mean ASBP reading in the sample was 123.1 mmHg (SD=10.3). The two self-esteem groups did not differ on mean ASBP or any demographic variable, all p’s > 0.15 (see Table 1); however, mean body mass index was somewhat greater in the high self-esteem group (difference= 1.0 kg/m2, t830=2.37, p=0.018). Participants with high self-esteem (N=231) reported significantly less anxiety over the course of the 24-hour EMA and ABP monitoring period than did participants with less self-esteem [mean= 1.80 (0.87) vs. 2.06 (0.87)], t856=−3.80, p< 0.001. In a multilevel regression model predicting momentary anxiety from self-esteem, controlling for demographic factors, the corresponding adjusted mean anxiety levels were 1.81 and 2.05, t853=−3.66, p< 0.001; the only significant demographic predictor of mean EMA anxiety was Black/African American race, with Blacks having lower EMA anxiety, t864=−2.39, p= 0.02.
Momentary anxiety and ambulatory blood pressure
Model 1 tested a) whether the relationship of momentary anxiety to ambulatory systolic blood pressure (ASBP), treated as a random effect, differed significantly among participants and b) whether, on average, the relationship was positive. On average, a 1-point increase in cube root-transformed anxiety was associated with a 0.80 mmHg (SE=0.09, t499=9.32, p<0.001) increase in ASBP. There was also significant variation among participants in the relationship; the estimated standard deviation of the slopes was 0.90 (Δ −2LL=15.91, df=2, p<0.001). Figure 2 depicts the mean relationship between momentary ratings of anxiety and concurrent ASBP readings, as well as the variability in that relationship across participants.
Figure 2.
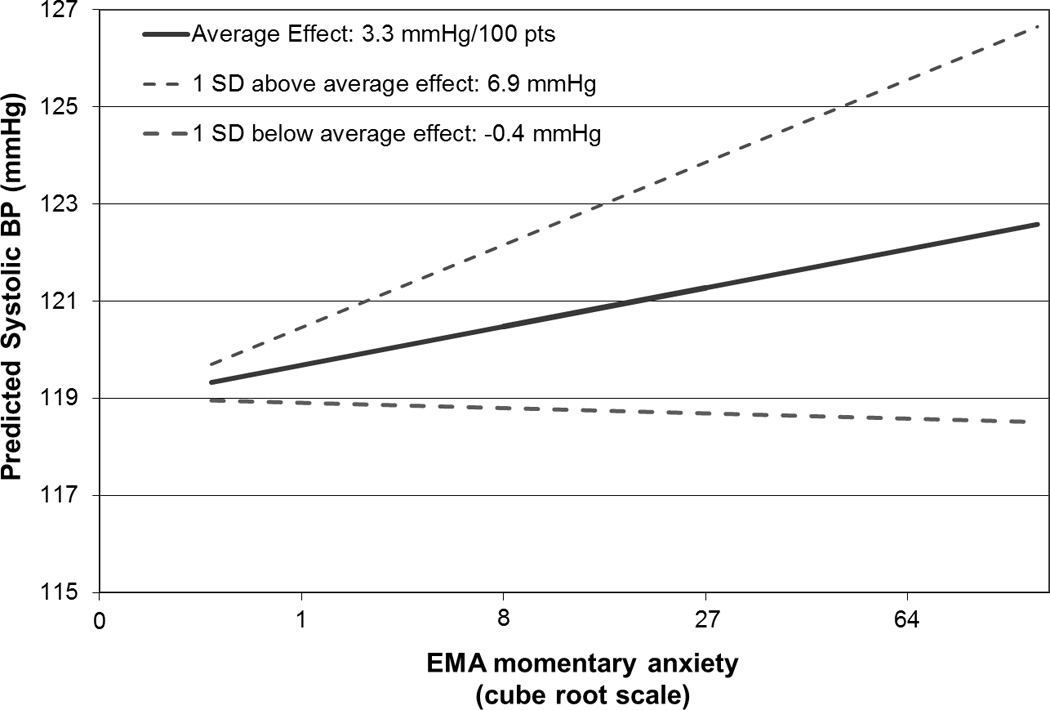
Mean predicted ambulatory systolic blood pressure across levels of momentary anxiety in participants with average systolic blood pressure reactivity to momentary anxiety, and participants with 1 SD greater and 1 SD lesser systolic blood pressure reactivity to momentary anxiety
Moderation of the effect of momentary anxiety on ambulatory blood pressure by self-esteem
Model 2 tested whether high self-esteem had an independent association with ASBP, and found that it did not, Δ −2LL=2.00, df=1, p=0.16. Model 3 tested whether high self-esteem modified the effect of momentary anxiety on ASBP. This analysis revealed that Model 3 provided a significant improvement over Model 2, Δ −2LL=5.92, df=1, p=0.015, and that the interaction of high self-esteem and momentary anxiety was significant, B= 0.48 (SE=0.20), t556=2.43, p=0.015. Figure 3 depicts the interaction of high self-esteem and momentary anxiety on ASBP, which suggests that ASBP in participants with low self-esteem is more strongly affected by momentary anxiety than ASBP in participants with high self-esteem.
Figure 3.
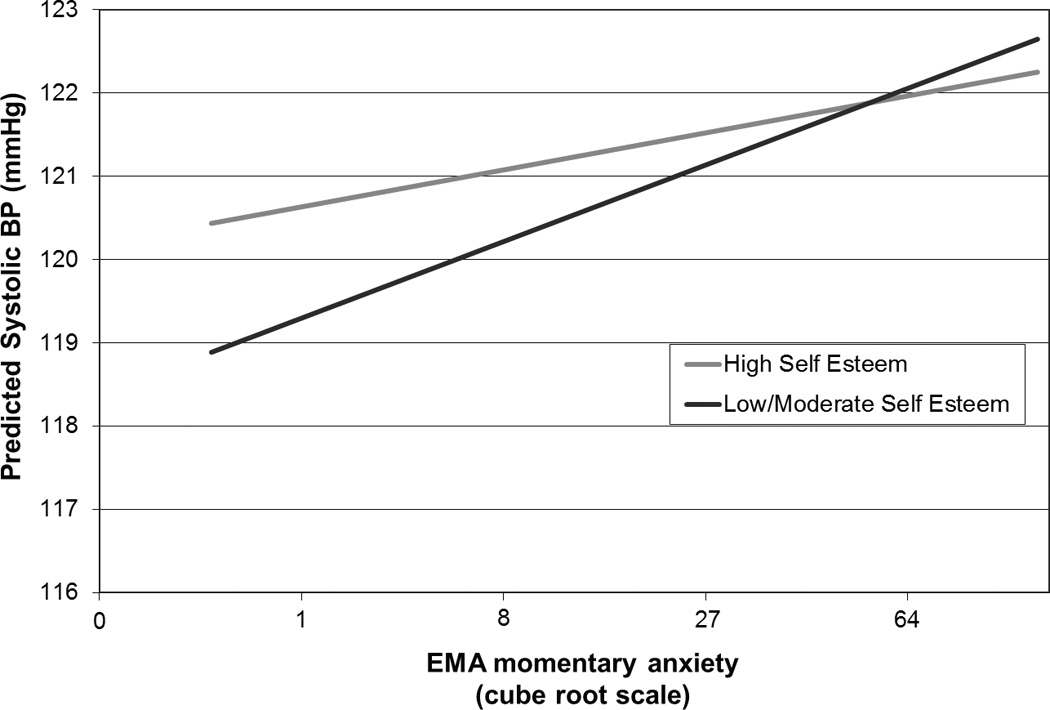
Mean predicted ambulatory systolic blood pressure across levels of momentary anxiety in participants with high and low levels of self-esteem
Sensitivity analyses
In order to determine whether the moderation of anxiety’s association with ASBP by self-esteem was sensitive to the categorization strategy used to create self-esteem groups, we conducted two sensitivity analyses. In the first sensitivity analysis, we re-estimated the model above after categorizing self-esteem into 3 groups based on self-esteem scores (≤ 8, 9–11, ≥ 12). In the second sensitivity analysis, we estimated the same model, using the continuous self-esteem score.
In the first sensitivity analysis, the effect of anxiety on ASBP was roughly twice as large in the low and medium self-esteem groups [B=0.90 (SE=0.13) and B=0.95 (SE=0.15), respectively] as in the high self-esteem group [B=0.44 (SE=0.17)]. The differences in these effects were statistically significant [B=0.45 (SE=0.21), t559=2.11, p= 0.035 for low versus high and B=0.50 (SE=0.23), t516=2.25, p= 0.025 for medium versus high, respectively]. In the second sensitivity analysis, the interaction of continuous self-esteem and anxiety was not statistically significant at an alpha level of .05, B= −0.08 (SE=0.05), t524=−1.69, p= 0.092, though it was in the predicted direction.
Supplemental analyses
To test whether related psychological constructs had similar moderating effects as self-esteem, or whether adjustment for related constructs might render self-esteem’s effects nonsignificant, we conducted three sets of analyses. In each, we first replaced self-esteem with one of three related constructs in the model specified above, or entered the construct as a covariate in the model with self-esteem included.
In the equivalent model replacing self-esteem with continuous sense of mastery, sense of mastery was positively associated with ambulatory SBP (i.e., main effect was significant, t884=2.59, p=0.010); however, while the interaction with momentary anxiety was negative (same direction as self-esteem), it was not statistically significant (t545=−1.18, p=0.24). In a model with both binary self-esteem and sense of mastery, the interaction of self-esteem with EMA anxiety remained almost unchanged (B=0.45, compared to its previous value of 0.48) and statistically significant (t545=2.21, p=0.027); the main effect of sense of mastery remained significantly positive (t822=2.05, p=0.040) and the interaction of mastery with EMA anxiety remained non-significantly negative (t542=−0.60, p=0.55).
Similarly, when we replaced self-esteem with the continuous LOT-R score, the main effect of optimism on ambulatory SBP was non-significant (t803=−0.18, p=0.86), and the interaction with momentary anxiety was positive (opposite direction) and not significant (t503=0.45, p=.66). In a model with both binary self-esteem and optimism, the interaction of self-esteem with EMA anxiety increased slightly in magnitude and was statistically significant (B=0.55, t554=2.72, p=0.007); the main effect of optimism remained non-significant (t809=−0.88, p=0.380) and the interaction of optimism with EMA anxiety remained positive and non-significant (t515=1.21, p=0.23).
Also, when we replaced self-esteem with continuous BDI score, the main effect of depressive symptoms on ambulatory SBP was not significant (t817=0.46, p=0.65), and the interaction with momentary anxiety was negative and not significant (t445=−0.95, p=.34). In a model with both binary self-esteem and BDI score, the interaction of self-esteem with EMA anxiety remained positive and significant (t548=2.65, p=0.008); the main effect of depressive symptoms was non-significantly positive (t817=0.96, p=0.34) and the interaction of depressive symptoms with EMA anxiety was non-significantly negative (t450=−1.49, p=0.14).
In the same manner as the above supplemental analyses, we tested whether sex or social support influenced the primary study results. We tested for a moderating effect of the interaction of gender and anxiety, and it was non-significant (p=0.33), and the interaction of self-esteem with anxiety was unchanged (B=0.49, p=0.013). Similarly, neither the main effect of social support nor the interaction of ISEL*anxiety was significant, and the interaction of self-esteem with anxiety was unchanged (B=0.50, p=0.012).
Thus, the self-esteem results held when we controlled for sex, sense of mastery, optimism, social support, or depressive symptoms. The self-esteem results appear to be specific to self-esteem, given that when we estimated models that replaced self-esteem with any of these related constructs, none of them significantly moderated the effect of EMA anxiety on ASBP.
Discussion
To our knowledge, this is the first study to test the hypothesized anxiety-buffering function of high self-esteem in the daily lives of a large community sample of employed adults. Results indicate support for two of the guiding hypotheses: that participants with high self-esteem would experience less anxiety throughout the course of the day, and that they would evince less cardiovascular reactivity, as measured by increased ASBP, when they did feel anxious. There was no significant mean difference in ASBP by self-esteem level, only a differential momentary association of anxiety with ASBP.
It is important to note that these participants were young and most (95%) were normotensive, with the mean blood pressure for the sample at a nearly optimal level. Thus, the lack of an association between self-esteem and mean ASBP is not overly surprising. However, the momentary association of anxiety with increased blood pressure is important, because anxiety is thought to contribute to risk for cardiovascular disease through repeated acute increases in blood pressure leading to a consistent upward shift in mean blood pressure.33 At this young age and cardiovascular health, such long-term effects may not yet be evident.
As hypothesized, the buffering of anxiety’s impact on ASBP was specific to self-esteem. Models that either replaced self-esteem with related constructs such as sense of mastery, optimism, or depression – or included those variables as covariates – suggested that the effect of self-esteem was both specific and robust. Overall, these findings provide some evidence for Martens et al.’s (2008) conceptualization of self-esteem as a psychological support that buffers the individual’s cardiovascular system by creating the conditions for the parasympathetic branch of the autonomic nervous system to hold down physiological stress and threat responding (perhaps through its effect on cardiac vagal tone).
In addition to filling a critical gap in the literature by showing that self-esteem can affect cardiovascular responses to anxiety outside the laboratory, the present findings may have implications for understanding some of the diverse phenomena in which self-esteem and anxiety are implicated. Consider, for example, the link between anxiety disorders, CVD and mortality. Anxiety disorders are often associated with both the development7 and exacerbation34 of CVD, and may also feature impairment of an individual’s sense of self-worth. The present results show that self-esteem deficits are associated with both greater anxiety and greater blood pressure responses to anxiety, and thus provocatively suggest that self-esteem deficits may play a role in the connection between such disorders and the development of CVD. Such a possibility is consistent with the Anxiety Buffer Disruption Theory of posttraumatic stress disorder (PTSD), which proposes that the experience of a traumatic event undercuts the protective functions of worldviews, including self-esteem,35,36 which may account for some of the cardiotoxic effects of PTSD.
Limitations
This study should be interpreted with its limitations in mind. First, although brief – and even single item - assessments of self-esteem have demonstrated reliable construct validity,37 the measure of self-esteem used here was a short version of a trait measure of self-esteem. Further, other research has shown that many domains of self-esteem exist,38 and that self-esteem fluctuates over the course of a day, with implications for parasympathetic activity.39 Thus, there may be nuances in the relationship between self-esteem and cardiovascular reactivity to anxiety that were not captured in the current study. In addition, future research should incorporate experimental designs, as well as self-esteem ratings along with anxiety ratings in electronic diary studies, to test the causal order that the present theoretical model postulates.
Second, both the main effect of anxiety on blood pressure and the effect of self-esteem on the anxiety-blood pressure association were small. Perhaps more comprehensive or nuanced assessments of momentary anxiety and self-esteem would have uncovered stronger associations. However, self-esteem is but one of a number of factors that determine an individual’s reactivity to momentary anxiety or stress, including genetic factors,40 perceived coping resources, environmental factors, and the total demands placed on the individual. Also, the interaction of self-esteem and anxiety on blood pressure was somewhat sensitive to the categorization of self-esteem, in that the interaction failed to reach statistical significance when self-esteem was used as a continuous score (p=0.092). However, the non-normal distribution of the self-esteem variable, as well as the consistent results of the other two categorization strategies, suggest that high self-esteem indeed buffers against blood pressure reactivity to momentary feelings of anxiety, as hypothesized.
Of course, this is an observational study, and the caveats inherent in observing large numbers of people in naturalistic settings versus smaller numbers in experimental settings apply. Further experimental evidence, perhaps by manipulating self-esteem and inducing anxiety while observing blood pressure reactivity, is needed to confirm our findings and to make stronger causal statements.
Further, this study was conducted in a relatively homogenous sample of working adults. It is possible that these results may not generalize to unemployed or low SES groups. Also, the participants were a healthy population, since those with existing cardiovascular disease or taking blood pressure lowering medication were excluded. As such, these results may not generalize to those with established cardiovascular disease or on hypertensive medications. Finally, although BMI had no effect on our findings, we did not assess overall fitness level or diet, so it is unclear whether these variables might exert some influence.
Conclusion
The results of this large study of psychological influences on blood pressure in daily life suggest that high self-esteem plays a role in buffering the adverse cardiovascular effects of moment-to moment fluctuations in anxiety. While the effect sizes observed for both anxiety and self-esteem’s buffering effect were small, they are consistent with theoretical models of psychological influences on blood pressure. Moreover, the insights derived here stem from the ecological capture of “a day in the life”, suggesting for the first time how self-esteem might operate to protect the cardiovascular system from cardiotoxic responses to daily anxiety. As such, the cumulative cardiovascular effects of these small but consistent associations may be of vital importance for both the conceptual understanding of self-esteem and cardiovascular processes, and also practical efforts to identify the keys to reducing risks for cardiovascular disease.
Acknowlegements
We are indebted to the study participants and research staff of the Masked Hypertension Study, without whose cooperation and dedication this study would not have been possible.
Sources of funding. This work was supported by grant P01-HL47540 (PI: J Schwartz) from the National Heart, Lung, and Blood Institute. The research was also supported in part by National Center for Advancing Translational Sciences (formerly the National Center for Research Resources) of the National Institutes of Health, through Grant MO1-RR10710 (Stony Brook University) and Grant UL1-TR000040 (formerly Grant UL1-RR024156, Columbia University). The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH.
Abbreviations
- ASBP
ambulatory systolic blood pressure
- ABPM
ambulatory blood pressure monitor
- CVD
cardiovascular disease
- EMA
ecological momentary assessment
- mmHg
millimeters of mercury
- SD
standard deviation
- TMT
terror management theory
Footnotes
Conflicts of interest The authors have no conflicts to report.
Following the recommendation of Tukey,41 we recoded values of “0” to 0.17 before applying the cube root transformation. Thus, 0→0.17, and 0.17(1/3) = 0.55.
See Schwartz and Stone 2007 (Schwartz JE, Stone AA. The analysis of real-time momentary data: A practical guide; in Stone AA, Shiffman S, Atienza AA, Nebeling L (eds): The science of real-time data capture: Self-report in health research. Oxford, Oxford University Press, 2007, pp 76–113.) for a full discussion of these and other models for analyzing medium-intensity multilevel data.
Author contributions: D. Edmondson was responsible for the hypotheses tested in the manuscript. All authors contributed to the study design. J.E. Schwartz was responsible for data collection. J.E. Schwartz and W. Chaplin performed the data analysis and interpretation. D. Edmondson drafted the paper, and J. Arndt, C. Alcantara and J.E. Schwartz provided critical theoretical input and manuscript revisions. All authors approved the final version of the paper for submission.
References
- 1.Mruk CJ. Self-esteem research, theory, and practice: Toward a positive psychology of self-esteem. Springer Publishing Company; 2006. [Google Scholar]
- 2.Baumeister RF, Smart L, Boden JM. Relation of threatened egotism to violence and aggression: the dark side of high self-esteem. Psychological review. 1996;103(1):5. doi: 10.1037/0033-295x.103.1.5. [DOI] [PubMed] [Google Scholar]
- 3.Creswell JD, Lam S, Stanton AL, Taylor SE, Bower JE, Sherman DK. Does self-affirmation, cognitive processing, or discovery of meaning explain cancer-related health benefits of expressive writing? Personality and Social Psychology Bulletin. 2007;33(2):238–250. doi: 10.1177/0146167206294412. [DOI] [PubMed] [Google Scholar]
- 4.Shimizu M, Pelham BW. The unconscious cost of good fortune: implicit and explicit self-esteem, positive life events, and health. Health Psychology. 2004;23(1):101. doi: 10.1037/0278-6133.23.1.101. [DOI] [PubMed] [Google Scholar]
- 5.Stinson DA, Logel C, Zanna MP, Holmes JG, Cameron JJ, Wood JV, Spencer SJ. The cost of lower self-esteem: Testing a self-and social-bonds model of health. Journal of Personality and Social Psychology. 2008;94(3):412. doi: 10.1037/0022-3514.94.3.412. [DOI] [PubMed] [Google Scholar]
- 6.Trzesniewski KH, Donnellan MB, Moffitt TE, Robins RW, Poulton R, Caspi A. Low self-esteem during adolescence predicts poor health, criminal behavior, and limited economic prospects during adulthood. Developmental psychology. 2006;42(2):381. doi: 10.1037/0012-1649.42.2.381. [DOI] [PubMed] [Google Scholar]
- 7.Roest AM, Martens EJ, de Jonge P, Denollet J. Anxiety and risk of incident coronary heart disease: a meta-analysis. Journal of the American College of Cardiology. 2010;56(1):38–46. doi: 10.1016/j.jacc.2010.03.034. [DOI] [PubMed] [Google Scholar]
- 8.Paterniti S, Alpérovitch A, Ducimetière P, Dealberto M-J, Lépine J-P, Bisserbe J-C. Anxiety But Not Depression Is Associated With Elevated Blood Pressure in a Community Group of French Elderly. Psychosomatic Medicine. 1999 Jan 1;61(1):77–83. doi: 10.1097/00006842-199901000-00013. 1999. [DOI] [PubMed] [Google Scholar]
- 9.Brondolo E, Rosen RC, Kostis JB, Schwartz JE. Relationship of physical symptoms and mood to perceived and actual blood pressure in hypertensive men: A repeated-measures design. Psychosomatic medicine. 1999;61(3):311–318. doi: 10.1097/00006842-199905000-00010. [DOI] [PubMed] [Google Scholar]
- 10.James GD, Yee L, Harshfield GA, Blank SG, Pickering TG. The influence of happiness, anger, and anxiety on the blood pressure of borderline hypertensives. Psychosomatic Medicine. 1986;48(7):502–508. doi: 10.1097/00006842-198609000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Schwartz JE, Warren K, Pickering TG. Mood, location and physical position as predictors of ambulatory blood pressure and heart rate: Application of a multi-level random effects model. Annals of Behavioral Medicine. 1994 [Google Scholar]
- 12.Harburg E, Julius S, McGinn NF, McLeod J, Hoobler S. Personality traits and behavioral patterns associated with systolic blood pressure levels in college males. Journal of chronic diseases. 1964;17(5):405–414. doi: 10.1016/0021-9681(64)90101-8. [DOI] [PubMed] [Google Scholar]
- 13.Jonas BS, Franks P, Ingram DD. Are symptoms of anxiety and depression risk factors for hypertension? longitudinal evidence from the National Health and Nutrition Examination Survey I Epidemiologic Follow-up Study. Archives of family medicine. 1997;6(1):43. doi: 10.1001/archfami.6.1.43. [DOI] [PubMed] [Google Scholar]
- 14.Sloan RP, Shapiro PA, Bagiella E, Myers MM, Gorman JM. Cardiac Autonomic Control Buffers Blood Pressure Variability Responses to Challenge: A Psychophysiologic Model of Coronary Artery Disease. Psychosomatic Medicine. 1999 Jan 1;61(1):58–68. doi: 10.1097/00006842-199901000-00010. 1999. [DOI] [PubMed] [Google Scholar]
- 15.Markovitz J, Matthews KA, Kannel WB, Cobb JL, D'Agostino RB. Psychological predictors of hypertension in the framingham study: Is there tension in hypertension? JAMA: The Journal of the American Medical Association. 1993;270(20):2439–2443. [PubMed] [Google Scholar]
- 16.Sherman DK, Cohen GL. The psychology of self-defense: Self-affirmation theory. Advances in experimental social psychology. 2006;38:183–242. [Google Scholar]
- 17.Steele CM. The psychology of self-affirmation: Sustaining the integrity of the self. Advances in experimental social psychology. 1988;21:261–302. [Google Scholar]
- 18.Greenberg J, Pyszczynski T, Solomon S. Public self and private self. Springer; 1986. The causes and consequences of a need for self-esteem: A terror management theory; pp. 189–212. [Google Scholar]
- 19.Taylor SE, Kemeny ME, Reed GM, Bower JE, Gruenewald TL. Psychological resources, positive illusions, and health. American Psychologist. 2000;55(1):99–109. doi: 10.1037//0003-066x.55.1.99. [DOI] [PubMed] [Google Scholar]
- 20.Martens A, Greenberg J, Allen J. Self-Esteem and Autonomic Physiology: Parallels Between Self-Esteem and Cardiac Vagal Tone as Buffers of Threat. Personality and Social Psychology Review. 2008;12(4):370. doi: 10.1177/1088868308323224. [DOI] [PubMed] [Google Scholar]
- 21.Martens A, Greenberg J, Allen JJB, Hayes J, Schimel J, Johns M. Self-esteem and autonomic physiology: Self-esteem levels predict cardiac vagal tone. Journal of Research in Personality. 2010;44(5):573–584. [Google Scholar]
- 22.Creswell JD, Welch WT, Taylor SE, Sherman DK, Gruenewald TL, Mann T. Affirmation of personal values buffers neuroendocrine and psychological stress responses. Psychological Science. 2005;16(11):846–851. doi: 10.1111/j.1467-9280.2005.01624.x. [DOI] [PubMed] [Google Scholar]
- 23.Taylor SE, Lerner JS, Sherman DK, Sage RM, McDowell NK. Are self-enhancing cognitions associated with healthy or unhealthy biological profiles? Journal of Personality and Social psychology. 2003;85(4):605. doi: 10.1037/0022-3514.85.4.605. [DOI] [PubMed] [Google Scholar]
- 24.Papousek I, Paechter M, Lackner HK. Delayed psychophysiological recovery after self-concept-inconsistent negative performance feedback. International Journal of Psychophysiology. 2011 doi: 10.1016/j.ijpsycho.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 25.Shimbo D, Newman JD, Schwartz JE. Masked hypertension and prehypertension: diagnostic overlap and interrelationships with left ventricular mass: the masked hypertension study. American journal of hypertension. 2012;25(6):664–671. doi: 10.1038/ajh.2012.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Low CA, Matthews KA, Kuller LH, Edmundowicz D. Psychosocial predictors of coronary artery calcification progression in postmenopausal women. Psychosom Med. 2011 Nov-Dec;73(9):789–794. doi: 10.1097/PSY.0b013e318236b68a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pearlin LI, Schooler C. The structure of coping. Journal of health and social behavior. 1978:2–21. [PubMed] [Google Scholar]
- 28.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. Journal of personality and social psychology. 1994;67(6):1063. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 29.Cohen S, Mermelstein R, Kamarck T, Hoberman HM. Social support: Theory, research and applications. Springer; 1985. Measuring the functional components of social support; pp. 73–94. [Google Scholar]
- 30.Beck AT, Steer R, Brown G. The psychological corporation. San Antonio, TX: 1996. Beck depression inventory. [Google Scholar]
- 31.Kenny DA, Zautra A. The trait-state-error model for multiwave data. Journal of consulting and clinical psychology. 1995;63(1):52. doi: 10.1037//0022-006x.63.1.52. [DOI] [PubMed] [Google Scholar]
- 32.Edmondson D, Shaffer JA, Chaplin WF, Burg MM, Stone AA, Schwartz JE. Trait anxiety and trait anger measured by ecological momentary assessment and their correspondence with traditional trait questionnaires. Journal of research in personality. 2013;47(6):843–852. doi: 10.1016/j.jrp.2013.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Steptoe A, Kivimäki M. Stress and cardiovascular disease: an update on current knowledge. Annual review of public health. 2013;34:337–354. doi: 10.1146/annurev-publhealth-031912-114452. [DOI] [PubMed] [Google Scholar]
- 34.Edmondson D, Richardson S, Falzon L, Davidson KW, Mills MA, Neria Y. Posttraumatic stress disorder prevalence and risk of recurrence in acute coronary syndrome patients: A meta-analytic review. PLoS ONE. 2012 Mar;7(6):e38915. doi: 10.1371/journal.pone.0038915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Edmondson D, Chaudoir S, Mills M, Park C, Holub J, Bartkowiak J. From shattered assumptions to weakened worldviews: Trauma symptoms signal anxiety buffer disruption. Journal of Loss and Trauma. 2011;16:358–385. doi: 10.1080/15325024.2011.572030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kesebir P, Luszczynska A, Pyszczynski T, Benight C. Posttraumatic stress disorder involves disrupted anxiety-buffer mechanisms. Journal of Social and Clinical Psychology. 2011;30(8):819–841. [Google Scholar]
- 37.Robins RW, Hendin HM, Trzesniewski KH. Measuring global self-esteem: Construct validation of a single-item measure and the Rosenberg Self-Esteem Scale. Personality and social psychology bulletin. 2001;27(2):151–161. [Google Scholar]
- 38.Crocker J, Luhtanen RK, Cooper ML, Bouvrette A. Contingencies of self-worth in college students: Theory and measurement. Journal of personality and social psychology. 2003;85(5):894–908. doi: 10.1037/0022-3514.85.5.894. [DOI] [PubMed] [Google Scholar]
- 39.Seery MD, Blascovich J, Weisbuch M, Vick SB. The relationship between self-esteem level, self-esteem stability, and cardiovascular reactions to performance feedback. Journal of personality and social psychology. 2004;87:133–144. doi: 10.1037/0022-3514.87.1.133. [DOI] [PubMed] [Google Scholar]
- 40.Ditto B. Familial influences on heart rate, blood pressure, and self-report anxiety responses to stress: Results from 100 twin pairs. Psychophysiology. 1993;30(6):635–645. doi: 10.1111/j.1469-8986.1993.tb02089.x. [DOI] [PubMed] [Google Scholar]
- 41.Tukey JW. Exploratory data analysis. Reading Ma. 1977:231. [Google Scholar]


