Abstract
Background
Adolescent depression and suicide are pressing public health concerns, and identifying key differences among suicide ideators and attempters is critical. The goal of the current study is to test whether depressed adolescent suicide attempters report greater anhedonia severity and exhibit aberrant effort-cost computations in the face of uncertainty.
Methods
Depressed adolescents (n = 101) ages 13–19 years were administered structured clinical interviews to assess current mental health disorders and a history of suicidality (suicide ideators = 55, suicide attempters = 46). Then, participants completed self-report instruments assessing symptoms of suicidal ideation, depression, anhedonia, and anxiety as well as a computerized effort-cost computation task.
Results
Compared with depressed adolescent suicide ideators, attempters report greater anhedonia severity, even after concurrently controlling for symptoms of suicidal ideation, depression, and anxiety. Additionally, when completing the effort-cost computation task, suicide attempters are less likely to pursue the difficult, high value option when outcomes are uncertain. Follow-up, trial-level analyses of effort-cost computations suggest that receipt of reward does not influence future decision-making among suicide attempters, however, suicide ideators exhibit a win-stay approach when receiving rewards on previous trials.
Limitations
Findings should be considered in light of limitations including a modest sample size, which limits generalizability, and the cross-sectional design.
Conclusions
Depressed adolescent suicide attempters are characterized by greater anhedonia severity, which may impair the ability to integrate previous rewarding experiences to inform future decisions. Taken together, this may generate a feeling of powerlessness that contributes to increased suicidality and a needless loss of life.
Keywords: Adolescence, Suicide, Depression, Anhedonia, Reward Dysfunction
Introduction
Adolescent depression and suicide are serious public health concerns. The lifetime prevalence of depression in adolescence is 11% (Avenevoli et al., 2015), and depressive episodes are associated with poor psychosocial functioning (e.g., greater discord with parents, lower academic performance), more frequent engagement in risky behaviors (e.g., substance use, precocious sexual behaviors), and suicidality (Auerbach et al., 2010; Frojd et al., 2008). Presently, suicide is the second leading cause of death among youth ages 13–18 (Centers for Disease Control and Prevention, 2013), and depressed adolescents have a 6-fold greater likelihood of making a suicide attempt (Nock et al., 2013). Nevertheless, the explicit link between depression and suicidality remains unclear. For adolescents, depression is among the strongest predictors of suicidal ideation and plans but shows a weaker relationship with suicide attempts, and critically, only a third of adolescent ideators make an attempt (Nock et al., 2013). However, few prior studies have examined potential mechanisms that can explain how depression contributes to the transition from ideation to attempt.
Both depression and suicide are characterized by diminished motivation and deficits in reward processing (Auerbach et al., 2014a; Dombrovski et al., 2013). In animal studies, dysfunction within the mesocorticolimbic pathway contributes to reduced social drive and reward pursuit, which has been depicted as a depression-like behavior (Mintz et al., 2005; Strekalova et al. 2004). Among humans, anhedonia – a reduced ability to experience pleasure – is a core feature in depression (Pizzagalli et al., 2005), and both depressed adolescents (Boger et al., 2014; Forbes et al., 2009) and adults (Bogdan and Pizzagalli, 2006; Pizzagalli et al., 2008) exhibit reward dysfunction, which may be a promising phenotype of depression. Converging evidence from neuroimaging studies characterizing the neuropathology of these reward deficits has highlighted dysfunction within the anterior cingulate cortex (Steele et al., 2007) and striatum (Pizzagalli et al., 2009). Less research has examined behavioral and neural correlates of anhedonia in suicide, although studies have revealed that suicide attempters show aberrant reward signaling (Dombrovski et al., 2013) and abnormal striatum structure (Ahearn et al., 2001; Vang et al., 2010), compared with non-suicidal individuals.
Indeed, anhedonia may be a promising predictor of suicidal behavior, as it has long been theorized that suicide is a decision to escape from intolerable conditions when there is no expectation of relief (Baumeister, 1990; Hawton et al., 1982; Nock and Kazdin, 2002). Along these lines, Nock and Kazdin (2002) posit that for many, the experience of anhedonia is insufferable, especially because it tends to be chronic and stable over time (Clark et al., 1984). Although there seem to be clear theoretical connections between anhedonia and suicidal behaviors, results have been equivocal. In adults, anhedonia predicted suicide completions in severe psychiatric patients within 1 year of assessment (Fawcett et al., 1990). These findings were largely replicated in an independent sample: anhedonia was present in early (i.e., 1 year of the assessment) but not late (after 1 year of the assessment) suicide completions (Coryell and Young, 2005). Other research, however, found that anhedonia did not prospectively predict suicide attempts. Rather, there was a stronger relationship between low anhedonia and increased likelihood of suicidal behaviors, and the researchers suggested that the presence of high energy and elevated emotion might be a necessary condition for suicidality (Loas, 2007; Watson and Kucala, 1978).
Comparatively less research, however, has been conducted in youth. In a study of children ages 6–13 admitted to an acute psychiatric facility, anhedonia was associated with the presence of a suicide attempt even after controlling for depressed mood. Moreover, greater anhedonia severity distinguished psychiatric inpatient suicide attempters and ideators (Nock and Kazdin, 2002). Similarly, in a study of adolescents, higher levels of anhedonia distinguished youth reporting a history of both suicide attempts and nonsuicidal self-injury from those with no suicide attempt history and current nonsuicidal self-injury (Brausch and Gutierrez, 2010). Yet, the study did not account for the potential influence of current depressive symptoms or suicidal ideation, which makes it challenging to ascertain the unique effect of anhedonia on suicide attempt status. By contrast, another adolescent study found that greater anhedonia was correlated with suicidal ideation but not intent (i.e., suicide plan); the study did not assess the occurrence of suicide attempts (Chabrol et al., 2007). Although this research is a promising start to parsing the effect of anhedonia on suicide attempts in youth, important gaps remain, particularly in understanding how anhedonia may contribute to suicide attempts among depressed adolescents.
Anhedonia impairs the ability to integrate rewarding experiences (Pizzagalli et al., 2005), which is essential for informing future decisions, and consequently, this might be one path that leads to attempting suicide. Specifically, as anhedonia is characterized by marked diminishment in pleasure in previously enjoyed activities (Pizzagalli et al., 2008), these experiences are not viewed as positive, and therefore, they are unlikely to increase the likelihood of engaging in them in the future. A possible downstream consequence is that anhedonic individuals tend to make abnormal effort-cost computations. Meaning, they avoid previously enjoyed activities as they overestimate the cost (i.e., effort expenditure) and underestimate the benefit (i.e., future reward) (Gold et al., 2012; Gold et al., 2013) – especially when the perceived benefit is uncertain – which reduces engagement in pursuing rewards across social (e.g., spending time with friends) and experiential (e.g., playing sports) domains. Over time, this decreases the opportunity to experience pleasure, which may contribute to the chronicity of anhedonia and increased suicidality.
The goal of the current study is to test whether depressed adolescent suicide attempters show increased anhedonic behaviors compared with ideators that have comparable symptom severity across depression, anxiety, and suicidal ideation. As the two groups do not differ on key clinical variables, any resulting differences cannot be attributed to symptom severity. We tested the following a priori hypotheses. First, we hypothesized that relative to ideators, suicide attempters would report greater levels of anhedonia even after controlling for current symptom severity. Second, for individuals experiencing anhedonia, the value of future rewards may not offer sufficient motivation to pursue goal-directed behaviors, particularly when: (a) the reward is uncertain and (b) the costs (i.e., effort expenditure) to obtain the rewards are perceived as outweighing the benefits (Gold et al., 2013). This abnormal effort-cost computation may be more pronounced in suicide attempters reporting more severe anhedonia, and thus, we hypothesized that compared to suicide ideators, attempters will be less likely to pursue uncertain, but not certain, rewards. Last, using a fine-grained approach to examine the effort-cost computation deficit, trial-level data analysis will demonstrate that suicide ideators and attempters differ in their behavior following receipt of rewards. Specifically, we hypothesize that for suicide attempters, reward receipt will not influence the pursuit of future rewards. By contrast, suicide ideators will be more likely to exhibit a win-stay approach – repeat the selection of an option after receiving a reward.
Methods
Participants
Participants included 101 adolescents (82 female, 19 male) ages 13–19 years (M = 15.50, SD = 1.48) recruited upon admission to a short-term, acute residential psychiatric facility. Inclusion criteria included a primary diagnosis of major depressive disorder or dysthymia and the presence of suicidal ideation (i.e., ≥4 on Beck’s Scale for Suicide Ideation (Beck et al., 1979). Exclusion criteria included a history of hypomania/mania or psychosis. Based on results of the suicide assessment (i.e., self-report and interview), depressed adolescents were exclusively classified as: (a) a suicide ideator (n = 55) if there was current suicidal ideation with no lifetime history of suicide attempt or (b) a suicide attempter (n = 46) if there was current suicidal ideation and a report of a suicide attempt in the past year.
Suicide ideators and suicide attempters differed in age (15.78 ± 1.52 vs. 15.15 ± 1.37 years; t[99] = 2.17, p = 0.033) and gender composition (suicide ideators = 72.7% female; suicide attempters = 91.3% female; χ2 [1, N = 101] = 5.17, p = 0.017) but not race (χ2 [3, N = 101] = 2.00, p = 0.57) or family income (χ2 [5] = 2.92, p = 0.71). Across participants, the following races were endorsed: 82.7% White, 9.2% multicultural (i.e., endorsed more than one race), 7.1% Asian, and 1.0% Black or African American. With regards to income distribution, participants reported the following: 2.6% = less than $10,000, 12.8% = $10,000 to $25,000, 17.9% = $25,000 to $50,000, 10.3% = $50,000-$75,000, 30.8% = $75,000 to $100,000, and 25.6% = more than $100,000.
Procedure
The Institutional Review Board provided approval, and data collection occurred within the broader context of a quality assurance program in which patients admitted to an acute child and adolescent residential program receive clinical assessments at admission and prior to discharge from the hospital. At admission, parents and adolescents 18 and older provided written consent, and youth under 18 years of age provided assent. Trained graduate students and BA-level research assistants not affiliated with clinical care on the residential unit completed the assessments. Initially, adolescents were administered clinical interviews assessing current and past psychopathology as well as history of self-injurious and suicidal behaviors. Then, adolescents filled out a series of self-report instruments measuring symptoms of suicidal ideation, depression, anhedonia, and anxiety. Last, participants completed an experimental task examining reward valuation, effort, and decision-making (described below).
Instruments
Assessment of psychopathology and suicidality
The Mini International Neuropsychiatric Interview (MINI-KID) (Sheehan et al., 2010) for children and adolescents is a structured diagnostic interview designed to assess current and past psychopathology for children and adolescents using DSM-IV criteria. The MINI-KID possesses good psychometric properties in diagnosing psychopathology in youth. The Self-Injurious Thoughts and Behaviors Interview (SITBI) (Nock et al., 2007) is a structured clinical interview assessing the presence, frequency, and severity of suicidal thoughts and behaviors, and it has been used and validated for use with adolescent inpatients (Auerbach et al., 2014b; Venta and Sharp, 2014). The current study assessed the presence or absence of a suicide attempt in the past year and lifetime. Prior to administering interviews, graduate students and BA-level research assistants received approximately 25 hours of training including, didactics, role-playing, and direct observation.
Suicidal Ideation
The Beck’s Scale for Suicide Ideation (SSI) (Beck et al., 1979) is a 21-item self-report instrument that assesses current suicidal ideation. Item scores range from 0 to 2, and each item is composed of 3 statements ranging in severity from the least (e.g., “I have no wish to die”) to the most (e.g., “I have a moderate to strong wish to die”) severe. Scores range from 0 to 42, and higher scores connote greater levels of suicidal ideation. A cutoff of ≥4 has been identified as a threshold for clinical-levels of suicidal ideation (Holi et al., 2005). The internal consistency was excellent (Cronbach’s α= .94).
Depression Symptoms
The Center for Epidemiologic Studies Depression Scale (CES-D) (Radloff, 1977) is a 20-item self-report inventory assessing depressive symptom severity for the previous week. Items are rated on a scale from 0 (rarely or none of the time) to 3 (most or all of the time), and scores range from 0 to 60, with higher scores indicating more severe depressive symptoms. Exemplar items include, “I had trouble keeping my mind on what I was doing,” “I felt I could not shake off the blues even with the help from my friends and family,” and “My sleep was restless.” In our sample, the internal consistency was excellent (Cronbach’s α = .93).
Anhedonia Symptoms
The Snaith-Hamilton Pleasure Scale (SHAPS) (Snaith et al., 1995) is a 14-item self-report inventory assessing hedonic capacity. Item scores range from 1 (strongly disagree) to 4 (strongly agree). Each item was reverse coded, and thus, scores ranged from 14 to 56 with higher scores indicating greater symptom severity. Sample items include, “I would enjoy seeing other people’s smiling faces” and “I would enjoy a cup of tea or coffee or my favorite drink.” Previous research using the SHAPS with adolescents recruited from acute psychiatric facilities has demonstrated strong reliability and validity (Boger et al., 2014). In the current study, the internal consistency was excellent (Cronbach’s α = .88).
Anxiety Symptoms
The Multidimensional Anxiety Scale for Children (MASC) (March et al., 1997) is a 39-item self-report inventory assessing current anxiety symptoms across four domains: physical symptoms (e.g., “I get shaky or jittery”), harm avoidance (e.g., “I check things out first”), social anxiety (e.g., “I worry about other people laughing at me”), and separation anxiety/panic (e.g., “The idea of going away to camp scares me”). Item scores range from 0 (Never true about me) to 3 (Often true about me) with total scores ranging from 0 to 117, and higher scores indicate greater anxiety severity. Internal consistency was excellent (Cronbach’s α = .91).
Experimental Task
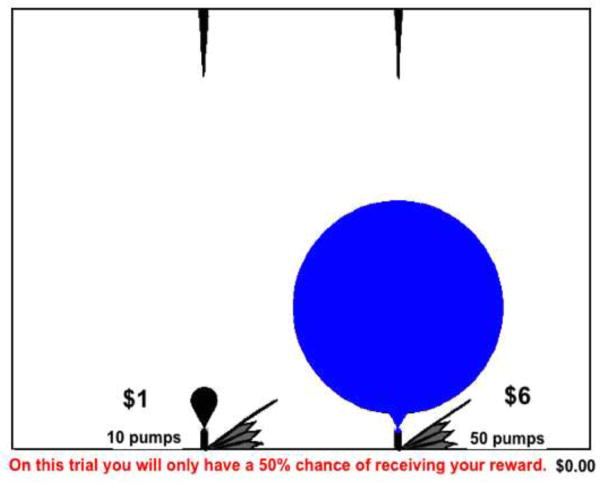
The effort-cost computational task (ECCT) tests the impact of reward value and probability on making low and high effort decisions (Gold et al., 2013). Participants are instructed to make a decision between two response alternatives displayed on the screen: (a) an easy option with a lower reward value (i.e., $1) and (b) a difficult option with a higher reward value (i.e., $3–7). The effortful task requires inflating a virtual balloon by pressing alternating left-right keys on a keyboard until it pops. Participants are free to select either the easy or difficult option on a given trial. For each trial, there is a 50% or 100% probability of receiving the reward, and on the 50% probability trials, this was displayed along the bottom of the screen. Whereas easy alternatives only require 10 key presses to obtain the reward (i.e., $1), all difficult option trials require 50 key presses to receive the reward (i.e., $3, $4, $5, $6, or $7). The task is composed of 60 trials, 30 trials with 100% probability and 30 trials with 50% probability. In each probability condition (i.e., 50% and 100%), there are 6 trials of each type ($1 vs. $3, $1 vs. $4, $1 vs. $5, $1 vs. $6, $1 vs. $7) (see trial schema Figure 1). Participants are informed that the top 3 scores receive a $50 gift card, and therefore, participants are incentivized to always choose the effortful or high reward value response to maximize total reward.
Figure 1. Effort-Cost Computation Task Schema.
Note. ECCT sample trial in which the high effort decision (i.e., difficult option) was selected in the 50% probability condition.
Data Analytic Overview
Before completing omnibus analyses, outliers were removed when reaction time exceeded mean ±3 standard deviations (n = 3). SPSS (version 20.0) General Linear Model software with Greenhouse-Geisser corrections was utilized. Consistent with past research using the ECCT (Gold et al., 2013), we examined how decision-making varied as a function of probability. Thus, separate Group (Suicide Ideators [SI], Suicide Attempters [SA]) x Value ($3, $4, $5, $6, $7) repeated-measures Analysis of Covariance (RMANCOVA) were conducted for 50% and 100% conditions. As there were group differences in age and gender, these variables were included as covariates1. Additionally, current depressive symptoms, anxious symptoms, and suicidal ideation were included as covariates to determine whether significant effects predict above and beyond current symptoms and suicidality2. Next, within the 50% condition only, trial-level data was utilized to examine the effect of reward receipt versus omission on subsequent selection of the difficult option. To examine these differences, a Group x Reward (Reward, No Reward) RMANCOVA was completed in the 50% condition. For each analysis, eta-squared effect sizes (η2) were computed where: (a) .02 – .12 = small, (b) .13 – .25 = medium, and (c) ≥.26 = large.
Results
Examination of Group Differences
Means, standard deviations, and results from the independent samples t-tests for suicidal ideation, depressive symptoms, anhedonia, and anxious symptoms are reported in Table 1, and partial correlations for baseline self-report instruments while controlling for current depressive symptoms is included in Table 2. In line with our hypothesis, suicide attempters reported significantly greater levels of anhedonia, and this difference remained after concurrently controlling for depressive symptoms, anxious symptoms, and suicidal ideation (F1,96 = 4.05, p = 0.047, η2 = 0.04). There were no group differences between ideators and attempters for suicidal ideation, depressive symptoms, or anxious symptoms.
Table 1.
Comparison of Depressed Suicide Attempters versus Non-Attempters across Symptoms
| Suicide Attempters (n = 46) | Suicide Ideators (n = 55) | df | t | p | d | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||||
| Suicidal Ideation | 17.59 | 10.07 | 14.75 | 7.10 | 99 | 1.66 | 0.101 | 0.33 |
| Depressive Symptoms | 21.24 | 9.73 | 19.39 | 10.17 | 99 | 0.93 | 0.355 | 0.19 |
| Anhedonia Symptoms | 40.47 | 7.16 | 37.49 | 6.73 | 99 | 2.14 | 0.035 | 0.43 |
| Anxious Symptoms | 65.07 | 17.85 | 64.25 | 17.16 | 99 | 0.23 | 0.817 | 0.05 |
Note. Beck’s Scale for Suicide Ideation = Suicidal Ideation; Center for Epidemiologic Studies Depression Scale = Depressive Symptoms; Snaith-Hamilton Pleasure Scale = Anhedonia Symptoms; Multidimensional Anxiety Scale for Children = Anxious Symptoms.
Table 2.
Partial Correlations among Baseline Symptom Instruments Controlling for Depressive Symptoms
| 1 | 2 | 3 | |
|---|---|---|---|
| 1. Suicidal Ideation | -- | ||
| 2. Anhedonia Symptoms | −.02 | -- | |
| 3. Anxious Symptoms | .01 | .22* | -- |
Note.
p < .05,
p < .01,
p < .001;
Beck’s Scale for Suicide Ideation = Suicidal Ideation; Center for Epidemiologic Studies Depression Scale = Depressive Symptoms; Snaith-Hamilton Pleasure Scale = Anhedonia Symptoms; Multidimensional Anxiety Scale for Children = Anxious Symptoms.
Effort-Cost Computations: Suicide Ideators versus Suicide Attempters
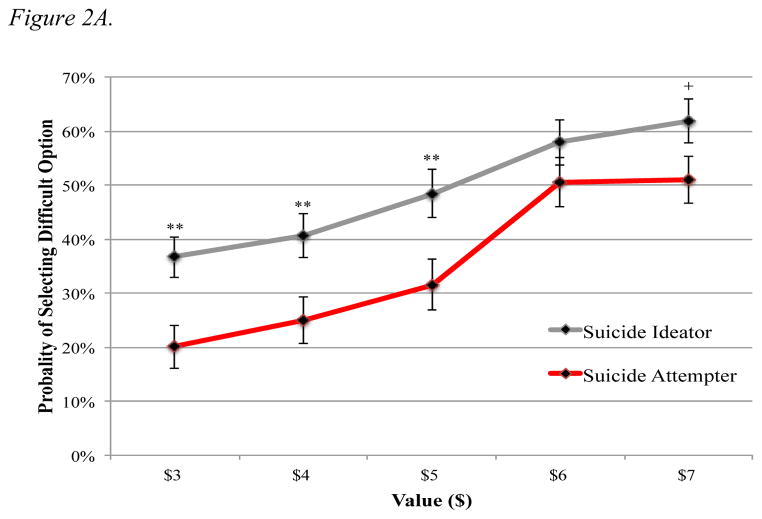
Uncertain Trials (50% Probability)
The Group x Value RMANCOVA revealed a main effect for Group, as compared to suicide ideators, the suicide attempters selected the high-effort response less frequently across values (F1,91 = 7.51, p = 0.007; η2 = 0.08). When examining the between-group simple effects as a function of value, significant differences emerged at lower ($3 – p = 0.004; $4 – p = 0.011; $5 – p = 0.012) but not higher ($6 – p = 0.248; $7 – p = 0.081) values (see Figure 2A). These effects were not qualified by a Group x Value interaction (F3.12,91 = 1.04, p = 0.376; η2 = 0.01). Additionally, there was no correlation between self-reported anhedonia and total money earned on difficult trials (r = −.07, p = .64).
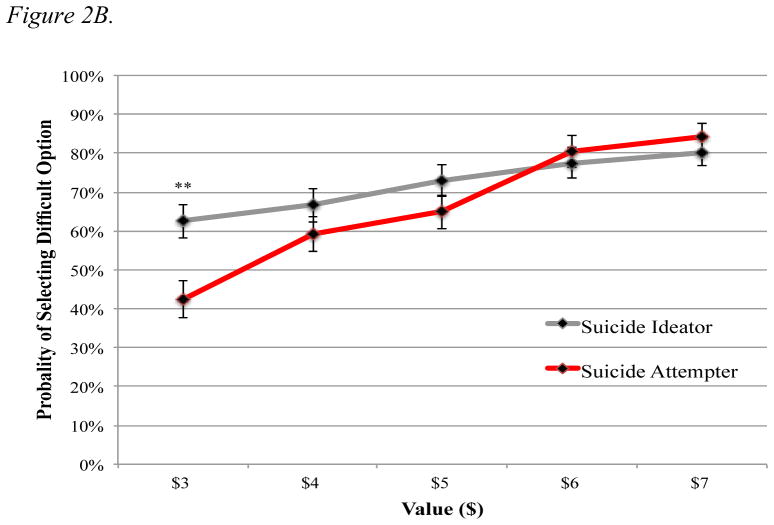
Figure 2.
Figure 2A. Probability of Selecting Difficult Option in Uncertain Trials (50% Probability)
Figure 2B. Probability of Selecting Difficult Option for Certain Trials (100% Probability)
Note. **p ≤0.01; + < 0.09; Probability of selecting difficult option among depressed suicide ideators (n = 52) and suicide attempters (n = 46) for (A) 50% probability and (B) 100% probability of receiving reward value; The Group X Value interaction was significant in Figure 2B but not Figure 2A.
Certain Trails (100% Probability)
The Group x Value RMANCOVA indicated no significant effect for Group (F1,91 = 1.41, p = 0.239; η2 = 0.02); however, there was a Group x Value interaction (F2.66,91 = 5.91, p = 0.001; η2 = 0.06). Between-group effects simple effects emerged for $3 (p = .003) but not for the higher values ($4 – p = 0.253; $5 – p = 0.192; $6 – p = 0.622; $7 p – = 0.424) (Figure 2B). There was, however, no association between anhedonic symptoms and total money earned on difficult trials (r = −.17, p = .12).
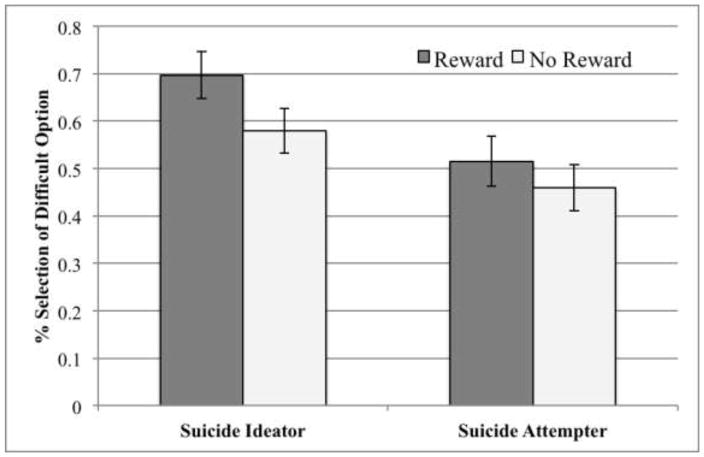
Trial-Level Effort Allocation
Trial-level data examined the impact of reward receipt on subsequent selection of difficult trials within the 50% probability. Only the 50% probability condition was examined, as the 100% condition did not provide variable outcomes (i.e., receipt of reward was certain). The trial-level model examined the effect of reward receipt versus reward omission on a participant’s likelihood of selecting the difficult option in the proceeding trial within the 50% condition. The Group x Reward (Reward, No Reward) RMANCOVA indicated a main effect for Group (F1, 89 = 5.69, p = 0.019; η2 = 0.06) as suicide ideators were more likely to select the difficult option following rewarded trials. This main effect was not qualified by a Group x Reward interaction (F1,89 = 0.80, p = 0.373; η2 = 0.01). Despite the null interaction, when decomposing the between- and within-group effects, interesting findings emerged. When probing the between-group simple effects, compared with suicide attempters, ideators were more likely to select the difficult option following receipt of reward in previous trials (p = 0.016), and there were no differences in the selection of the difficult option in trials following no reward (p = 0.089) (see Figure 3). Further, within-group effects suggested that whereas suicide ideators were more likely to select the difficult option following reward receipt versus no reward (p = 0.014), there were no differences in selection among suicide attempters (p = 0.260).
Figure 3. Impact of Reward Receipt on Effort-Cost Computations in Selecting Difficult Trials for the 50% Probability Condition.
Note. *p < .05; Probability of suicide ideators (n = 50) and suicide attempters (n = 46) selecting difficult option in trials following reward or no reward in difficult trials within the 50% condition.
Discussion
The alarming prevalence rates of depression and suicidality in adolescents underscore the enormity of the present public health concern (Avenevoli et al., 2015; Nock et al., 2013). To our knowledge, the study is the first to report key differences in abnormal effort-cost computations in depressed adolescent suicide ideators and attempters with comparable symptom severity. Results indicated that compared to depressed suicide ideators, depressed suicide attempters reported greater anhedonia severity, even after controlling for current symptom severity and suicidal ideation. Moreover, when probing putative differences in reward processing, relative to adolescent suicide ideators, attempters were less likely to pursue high value rewards when outcomes were uncertain. As a whole, these findings suggest that anhedonia may play a key role in predicting risk for suicidality in youth.
Anhedonia, Effort-Cost Computations, and Suicidality
Extant research has debated the role of anhedonia in the context of suicidality. Whereas some research has indicated that suicide attempters are characterized by greater anhedonia (Fawcett et al., 1990; Nock and Kazdin, 2002), other studies indicate that lower levels of anhedonia may be a necessary condition for suicide attempts and completions (Loas, 2007). Our findings confirm that among depressed adolescents, anhedonia severity is greater among suicide attempters versus ideators. Although our findings conflict with studies showing an inverse association between anhedonia and the frequency suicide attempts and completions, there are important developmental differences to consider. Namely, adolescents are closer to the beginning of what, for many, may be a long disease course. Among adults, Loas and colleagues assert that lower anhedonia is a necessary condition for making an attempt because this decision and the ensuing actions require sufficient energy. For some, lower anhedonia may dovetail with a period of wellness, and one possibility is that they may experience a fear of relapse. That is, the worry about experiencing a future episode may trigger suicidal behaviors; yet, additional research is needed to investigate this more explicitly. Although our findings strongly support the role of anhedonia in adolescent suicide attempts, it is conceivable that it may operate differently in younger and older individuals.
Our results suggest that depressed adolescent suicide attempters are characterized by a disruption in their hedonic capacity, which may serve to color their worldview. Specifically, the receipt of reward, or pleasure more generally, may act as a signpost to guide future course (e.g., pursuing enjoyed activities, spending time with peers). However, among depressed individuals with anhedonia, these signposts may be compromised. Indeed, Olino and colleagues (2011) found that compared to healthy youth, depressed adolescents exhibited less striatal activation during reward anticipation following winning outcomes on previous trials. This finding suggests that depressed youth may not be integrating (from a neurobiological perspective) preceding experiences to inform future expectations. For suicide attempters, greater anhedonia coupled with an inability to incorporate rewarding experiences (e.g., spending time with friends) may foster feelings of powerlessness and hopelessness. Patients may not integrate signposts of past experiences that provided pleasure, which decreases the likelihood of pursuing these activities in the future. Consequently, it may contribute to a more chronic course of depression and possibly the manifestation of comorbid disorders (e.g., substance use disorders). Taken together, it may not be surprising that these deficits increase the likelihood for the occurrence of suicidal behaviors.
Limitations
It is important to note several limitations in our approach. First, the study included a relatively modest sample size (n = 101), which may impact the generalizability of these findings. Second, the current study examined suicide in the context of depression; however, the pathway to suicide is equifinal and occurs in the context of an array of disorders (e.g., bipolar disorder, borderline personality disorder) (Nock et al., 2013). Therefore, future research is needed to determine whether anhedonia and associated reward dysfunction may contribute to suicidality across these and other disorders. Last, the majority of our sample was female adolescents, which is not uncommon given gender differences in major depressive disorder (Avenevoli et al., 2015). Nonetheless, future research should aim to replicate these findings with a more balanced gender distribution.
Conclusions
Adolescent suicide attempters are characterized by greater anhedonia severity, which may contribute to an inability to integrate previous rewarding experiences that, ideally, should inform future decision-making. These results highlight the importance of identifying key differences among suicide ideators and attempters, as this will, ultimately, better inform the development of suicide models that improve identification of: (a) ideators at greatest risk to make a suicide attempt and (b) attempters most likely to re-attempt. Development of an improved understanding of suicide risk is essential, as it will prevent the needless loss of life.
Highlights.
Suicide is the second leading cause of death among adolescents.
Adolescent suicide attempters are characterized by greater anhedonia severity.
Depressed suicide attempters do not integrate rewarding experiences.
Acknowledgments
Role of Funding Source
Dr. Auerbach was partially supported through funding from: NIMH K23MH097786, the Kaplen Fellowship on Depression awarded by Harvard Medical School, the Tommy Fuss Fund, and the Simches Fund. Dr. Stewart was supported, in part, through the Skip Pope Award for Young Investigators awarded by McLean Hospital. The funding sources did not assist with study design, data acquisition, or data analysis. Manuscript preparation and submission was managed by the authors.
The authors are appreciative of the ongoing support and collaboration with the staff from the Adolescent Residential Treatment program at McLean Hospital.
Footnotes
Given the smaller percentage of male participants, we conducted analyses while including/excluding male participants, and there were no differences in the results.
Results remained the same across analyses when suicidal ideation, depressive symptoms, and anxious symptoms were excluded as covariates; however, the inclusion of these variables provides a more conservative test of the a priori hypotheses.
Conflict of Interest
Conflicts of Interest: none
Contributions
We confirm that the final manuscript has been read and approved by all named authors and that there are no other persons who satisfied criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us.
With respect to roles in the project and manuscript, Dr. Auerbach designed the study, completed preliminary analyses, and prepared the majority of the manuscript. Mr. Millner also assisted with the study conceptualization, and he took a lead role in completing trial-level analyses. Dr. Stewart assisted with data analyses and manuscript preparation. Ms. Esposito played a key role in data collection and data management. Additionally, she conducted preliminary analyses and assisted with manuscript preparation.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ahearn EP, Jamison KR, Steffens DC, Cassidy F, Provenzale JM, Lehman A, Krishnan KR. MRI correlates of suicide attempt history in unipolar depression. Biological Psychiatry. 2001;50(4):266–270. doi: 10.1016/s0006-3223(01)01098-8. [DOI] [PubMed] [Google Scholar]
- Auerbach RP, Admon R, Pizzagalli DA. Adolescent depression: Stress and reward dysfunction. Harvard Review of Psychiatry. 2014a;22(3):139–148. doi: 10.1097/HRP.0000000000000034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach RP, Kim JC, Chango JM, Spiro WJ, Cha C, Gold J, Nock MK. Adolescent nonsuicidal self-injury: Examining the role of child abuse, comorbidity, and disinhibition. Psychiatry Research. 2014b;220(1):579–584. doi: 10.1016/j.psychres.2014.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach RP, Tsai B, Abela JRZ. Temporal relationships among depressive symptoms, risky behavior engagement, perceived control, and gender in a sample of adolescents. Journal of Research on Adolescence. 2010;20(3):726–747. [Google Scholar]
- Avenevoli S, Swendsen J, He JP, Burstein M, Merikangas KR. Major depression in the national comorbidity survey-adolescent supplement: Prevalence, correlates, and treatment. Journal of the American Academy of Child and Adolescent Psychiatry. 2015;54(1):37–44. e32. doi: 10.1016/j.jaac.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumeister RF. Suicide as escape from self. Psychological Review. 1990;97(1):90–113. doi: 10.1037/0033-295x.97.1.90. [DOI] [PubMed] [Google Scholar]
- Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: The Scale for Suicide Ideation. Journal of Consulting and Clinical Psychology. 1979;47(2):343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- Bogdan R, Pizzagalli DA. Acute stress reduces reward responsiveness: implications for depression. Biological Psychiatry. 2006;60(10):1147–1154. doi: 10.1016/j.biopsych.2006.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boger KD, Auerbach RP, Pechtel P, Busch AB, Greenfield SF, Pizzagalli DA. Co-occurring depressive and substance use disorders in adolescents: An examination of reward responsiveness during treatment. Journal of Psychotherapy Integration. 2014;24(2):109–121. doi: 10.1037/a0036975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brausch AM, Gutierrez PM. Differences in non-suicidal self-injury and suicide attempts in adolescents. Journal of Youth and Adolescence. 2010;39(3):233–242. doi: 10.1007/s10964-009-9482-0. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Web-based injury statistics query and reporting system. National Center for Injury Prevention and Control, CDC; 2013. Available from: http://www.cdc.gov/injury/wisqars/leadingcauses.html. [Google Scholar]
- Chabrol H, Rodgers R, Rousseau A. Relations between suicidal ideation and dimensions of depressive symptoms in high-school students. Journal of Adolescence. 2007;30(4):587–600. doi: 10.1016/j.adolescence.2006.07.003. [DOI] [PubMed] [Google Scholar]
- Clark DC, Fawcett J, Salazar-Grueso E, Fawcett E. Seven-month clinical outcome of anhedonic and normally hedonic depressed inpatients. The American journal of Psychiatry. 1984;141(10):1216–1220. doi: 10.1176/ajp.141.10.1216. [DOI] [PubMed] [Google Scholar]
- Coryell W, Young EA. Clinical predictors of suicide in primary major depressive disorder. The Journal of Clinical Psychiatry. 2005;66(4):412–417. doi: 10.4088/jcp.v66n0401. [DOI] [PubMed] [Google Scholar]
- Dombrovski AY, Szanto K, Clark L, Reynolds CF, Siegle GJ. Reward signals, attempted suicide, and impulsivity in late-life depression. JAMA Psychiatry. 2013;70:1020–1030. doi: 10.1001/jamapsychiatry.2013.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fawcett J, Scheftner WA, Fogg L, Clark DC, Young MA, Hedeker D, Gibbons R. Time-related predictors of suicide in major affective disorder. The American Journal of Psychiatry. 1990;147(9):1189–1194. doi: 10.1176/ajp.147.9.1189. [DOI] [PubMed] [Google Scholar]
- Forbes EE, Brown SM, Kimak M, Ferrell RE, Manuck SB, Hariri AR. Genetic variation in components of dopamine neurotransmission impacts ventral striatal reactivity associated with impulsivity. Molecular Psychiatry. 2009;14(1):60–70. doi: 10.1038/sj.mp.4002086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frojd SA, Nissinen ES, Pelkonen MU, Marttunen MJ, Koivisto AM, Kaltiala-Heino R. Depression and school performance in middle adolescent boys and girls. Journal of Adolescence. 2008;31(4):485–498. doi: 10.1016/j.adolescence.2007.08.006. [DOI] [PubMed] [Google Scholar]
- Gold JM, Strauss GP, Waltz JA, Robinson BM, Brown JK, Frank MJ. Negative symptoms of schizophrenia are associated with abnormal effort-cost computations. Biological Psychiatry. 2013;74(2):130–136. doi: 10.1016/j.biopsych.2012.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold JM, Waltz JA, Matveeva TM, Kasanova Z, Strauss GP, Herbener ES, Frank MJ. Negative symptoms and the failure to represent the expected reward value of actions: behavioral and computational modeling evidence. Archives of General Psychiatry. 2012;69(2):129–138. doi: 10.1001/archgenpsychiatry.2011.1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K, Cole D, O’Grady J, Osborn M. Motivational aspects of deliberate self-poisoning in adolescents. The British journal of Psychiatry. 1982;141:286–291. doi: 10.1192/bjp.141.3.286. [DOI] [PubMed] [Google Scholar]
- Holi MM, Pelkonen M, Karlsson L, Kiviruusu O, Ruuttu T, Heila H, Marttunen M. Psychometric properties and clinical utility of the Scale for Suicidal Ideation (SSI) in adolescents. BMC Psychiatry. 2005;5:8. doi: 10.1186/1471-244X-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loas G. Anhedonia and suicide: A 6.5-yr. follow-up study of patients hospitalised for a suicide attempt. Psychological Reports. 2007;100(1):183–190. doi: 10.2466/pr0.100.1.183-190. [DOI] [PubMed] [Google Scholar]
- March JS, Parker JD, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, and validity. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(4):554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- Mintz M, Ruedi-Bettschen D, Feldon J, Pryce CR. Early social and physical deprivation leads to reduced social motivation in adulthood in Wistar rats. Behavior and Brain Reseach. 2005;156(2):311–320. doi: 10.1016/j.bbr.2004.08.017. [DOI] [PubMed] [Google Scholar]
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, Kessler RC. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Holmberg EB, Photos VI, Michel BD. Self-Injurious Thoughts and Behaviors Interview: Development, reliability, and validity in an adolescent sample. Psychological Assessment. 2007;19(3):309–317. doi: 10.1037/1040-3590.19.3.309. [DOI] [PubMed] [Google Scholar]
- Nock MK, Kazdin AE. Examination of affective, cognitive, and behavioral factors and suicide-related outcomes in children and young adolescents. Journal of Clinical Child and Adolescent Psychology. 2002;31(1):48–58. doi: 10.1207/S15374424JCCP3101_07. [DOI] [PubMed] [Google Scholar]
- Olino TM, McMakin DL, Dahl RE, Ryan ND, Silk JS, Birmaher B, Axelson DA, Forbes EE. “I won, but I’m not getting my hopes up”: Depression moderates the relationship of outcomes and reward anticipation. Psychiatry Research: Neuroimaging. 2011;194(3):393–395. doi: 10.1016/j.pscychresns.2011.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizzagalli DA, Holmes AJ, Dillon DG, Goetz EL, Birk JL, Bogdan R, Fava M. Reduced caudate and nucleus accumbens response to rewards in unmedicated individuals with major depressive disorder. The American Journal of Psychiatry. 2009;166(6):702–710. doi: 10.1176/appi.ajp.2008.08081201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizzagalli DA, Iosifescu D, Hallett LA, Ratner KG, Fava M. Reduced hedonic capacity in major depressive disorder: evidence from a probabilistic reward task. Journal of Psychiatric Research. 2008;43(1):76–87. doi: 10.1016/j.jpsychires.2008.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizzagalli DA, Jahn AL, O’Shea JP. Toward an objective characterization of an anhedonic phenotype: A signal-detection approach. Biological Psychiatry. 2005;57(4):319–327. doi: 10.1016/j.biopsych.2004.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, Wilkinson B. Reliability and validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID) The Journal of Clinical Psychiatry. 2010;71(3):313–326. doi: 10.4088/JCP.09m05305whi. [DOI] [PubMed] [Google Scholar]
- Snaith RP, Hamilton M, Morley S, Humayan A, Hargreaves D, Trigwell P. A scale for the assessment of hedonic tone the Snaith-Hamilton Pleasure Scale. The British Journal of Psychiatry. 1995;167(1):99–103. doi: 10.1192/bjp.167.1.99. [DOI] [PubMed] [Google Scholar]
- Steele JD, Kumar P, Ebmeier KP. Blunted response to feedback information in depressive illness. Brain. 2007;130(Pt 9):2367–2374. doi: 10.1093/brain/awm150. [DOI] [PubMed] [Google Scholar]
- Strekalova T, Spanagel R, Bartsch D, Henn FA, Gass P. Stress-induced anhedonia in mice is associated with deficits in forced swimming and exploration. Neuropsychopharmacology. 2004;29(11):2007–2017. doi: 10.1038/sj.npp.1300532. [DOI] [PubMed] [Google Scholar]
- Vang FJ, Ryding E, Traskman-Bendz L, van Westen D, Lindstrom MB. Size of basal ganglia in suicide attempters, and its association with temperament and serotonin transporter density. Psychiatry Research. 2010;183(2):177–179. doi: 10.1016/j.pscychresns.2010.05.007. [DOI] [PubMed] [Google Scholar]
- Venta A, Sharp C. Extending the concurrent validity of the Self-Injurious Thoughts and Behaviors Interview to inpatient adolescents. Journal of Psychopathology and Behavioral Assessment. 2014;36(4):675–682. [Google Scholar]
- Watson CG, Kucala T. Anhedonia and death. Psychological Reports. 1978;43(3 Pt 2):1120–1122. doi: 10.2466/pr0.1978.43.3f.1120. [DOI] [PubMed] [Google Scholar]