Abstract
A link between hyperthyroidism and pulmonary hypertension has been reported, but the underlying mechanisms of these two conditions have not been clearly identified. The aim of this study was to determine the clinical correlates of pulmonary hypertension in patients with Graves’ disease. Among 50 consecutive patients with Graves’ disease referred for echocardiography, 18 patients (36 %) had pulmonary hypertension measured by continuous-wave Doppler echocardiography (pulmonary artery systolic pressure >35 mmHg). The patients with pulmonary hypertension had significantly higher pulmonary vascular resistance (PVR), cardiac output and thyroid-stimulating hormone receptor antibody (TRAb) compared to those without (p < 0.001, p = 0.028 and p < 0.001, respectively). Pulmonary artery systolic pressure had a good correlation with TRAb (r = 0.74, p < 0.001), but was not related to free T4 (r = 0.12, p = 0.419) and free T3 (r = 0.22, p = 0.126). To determine the important variables present in patients with Graves’ disease that may be related to pulmonary artery systolic pressure, 4 variables (PVR, cardiac output, TRAb and free T3) were used in the multivariate analysis. In addition to PVR (standard regression coefficient = 0.831, p < 0.001) and cardiac output (standard regression coefficient = 0.592, p < 0.001), TRAb (standard regression coefficient = 0.178, p < 0.001) emerged as a significant variable related to pulmonary artery systolic pressure. Thus, in addition to the effect of thyroid hormone on the cardiovascular system, autoimmune-mediated pulmonary vascular remodeling may play a role in Graves’ disease-linked elevated pulmonary artery systolic pressure.
Keywords: Pulmonary hypertension, Hyperthyroidism, Echocardiography, Autoimmunity
Introduction
Characteristic clinical manifestations of hyperthyroidism are those resulting from the effects of thyroid hormone on the cardiovascular system [1, 2]. Common cardiovascular signs of hyperthyroidism include sinus tachycardia, atrial arrhythmias, increased cardiac output, widened pulse pressure and elevated pulmonary artery pressure [1–7]. Although Doppler echocardiography may be imprecise in determining actual pressures compared to invasive evaluation, it is performed as a noninvasive screening test that can detect pulmonary hypertension [8–11]. A high prevalence of pulmonary hypertension, detected by Doppler echocardiography, has been observed in patients with hyperthyroidism [4–6]. However, pathophysiologic link between hyperthyroidism and pulmonary hypertension remains unclear. Because studies with a limited number of patients have looked into the association between hyperthyroidism and elevated pulmonary artery pressure, we designed a study to determine the clinical correlates of elevated pulmonary artery systolic pressure in patients with Graves’ disease.
Subjects and methods
Patients’ characteristics
This observational study was performed in 59 consecutive patients with recently diagnosed Graves’ disease (within 12 weeks of diagnosis) recruited from the echocardiography laboratory of the Kochi Medical School Hospital. All the patients were referred to the echocardiography laboratory by physicians from the endocrinology outpatient clinic. The main inclusion criteria for enrolment were no history of heart disease (congenital heart disease, coronary artery disease, valvular heart disease or cardiomyopathy), lung disease, liver disease, or collagen vascular disease. We excluded patients who were taking vasoactive drugs (calcium channel blockers, alpha-adrenergic blockers, angiotensin converting enzyme inhibitors and angiotensin receptor blockers). Lung disease was excluded by chest radiography and careful chart reviews. Patient evaluation included a medical history, physical examination and laboratory studies. The diagnosis of Graves’ disease was made by the findings of sustained hyperthyroidism; serum-free thyroxine (T4) level >1.79 ng/dL, free triiodothyronine (T3) >4.0 pg/mL with concomitant decrease in thyroid-stimulating hormone (TSH) levels, elevated TSH receptor antibody (TRAb) levels (>2 IU/L ), increased blood flow in the thyroid gland on ultrasonography and a diffuse goiter. All samples were prepared and analyzed in accordance with the ethical recommendations of the hospital’s committee on human research and written informed consent was obtained from all subjects.
Measurements
Blood samples were collected from the antecubital vein within 24 h of the echocardiography. Serum albumin was measured by a dye-binding bromocresol green procedure and C-reactive protein (CRP) was measured by latex agglutination immunoassay using a JCA-BM2250 analyzer (Japan Electron Optics Laboratory, Tokyo, Japan). White blood cells were measured by the direct current detection method using a Sysmex SE 9000 (Sysmex, Kobe, Japan). Blood samples were also analyzed for free T4, free T3, TSH and TRAb by the electrochemiluminescence immunoassay using Modular Analytica E170 (Roche Diagnostics, Rotkreuz, Switzerland).
Echocardiography
Transthoracic echocardiography was performed with a Philips ultrasound iE 33 phased-array sector scanner (Philips, Bothell, USA) or a Sequoia 512 (Siemens, Erlangen, Germany) using a 3.75 or 2.5 MHz transducer by an experienced echocardiographer. Conventional M-mode and 2D echocardiographic measurements were performed in the standard manner [12–14]. Doppler recordings of tricuspid regurgitation were performed in the apical 4-chamber view. The regurgitation jet was recorded by means of continuous-wave Doppler, and the maximum velocity was used to calculate the transtricuspid pressure gradient by means of the modified Bernoulli equation [13]. Pulmonary artery systolic pressure was calculated as the sum of the transtricuspid pressure gradient in conjunction with an echocardiographic estimation of right atrial pressure. Echocardiographic estimation of right atrial pressure was performed based on inferior vena cava size and collapsibility, according to the previously established criteria [15]. Measurement of cardiac output was performed at rest from the apical 2D echocardiograms using a modified Simpson technique and multiplying stroke volume by heart rate. Pulmonary vascular resistance (PVR) was estimated by Doppler echocardiography using the equation proposed by Lindqvist et al.: PVR = (pulmonary artery mean pressure − 10)/cardiac output, where pulmonary artery mean pressure = pulmonary artery systolic pressure × 0.61 + 2 mmHg [16, 17]. All classic views were recorded on videotape for subsequent analysis by physicians who were board certified in echocardiography.
Statistical analysis
Results are reported as the mean value ± standard deviation. Statistical analysis between the 2 groups was performed by the Student’s t test or the Mann–Whitney test for continuous variables and the Fisher exact probability test for discrete variables. Correlation coefficients between the 2 continuous variables were obtained using the linear regression analysis. Multiple regression analysis was performed to identify the variables independently related to pulmonary artery systolic pressure. A p value <0.05 was considered significant.
Results
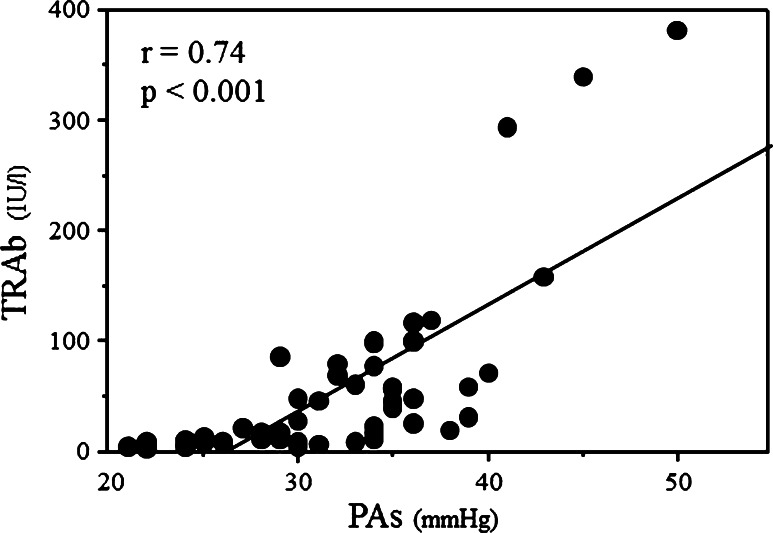
Among 59 patients with Graves’ disease, pulmonary artery systolic pressure could not be determined in 9 patients (18 %) due to the absence of tricuspid regurgitation. Therefore, this study consists of 50 patients. Eighteen patients (36 %) had pulmonary hypertension (pulmonary artery systolic pressure >35 mmHg). There were no significant differences in age, gender distribution, cardiac output, free T4, free T3, TSH, creatine phosphokinase, CRP levels, cholesterol, serum albumin, white blood cells or incidence of medical therapy (beta-blocker and/or thiamazole) between patients with and without pulmonary hypertension (Tables 1, 2). Cardiac output, PVR and TRAb were significantly higher in patients with pulmonary hypertension compared to those without. Pulmonary artery systolic pressure had a good correlation with TRAb (r = 0.74, p < 0.001) (Fig. 1), but was not related to free T4 (r = 0.12, p = 0.419) and free T3 (r = 0.22, p = 0.126).
Table 1.
Clinical characteristics
| Pulmonary hypertension | p value | ||
|---|---|---|---|
| Present (n = 18) | Absent (n = 32) | ||
| Age (years) | 54 ± 12 | 49 ± 14 | 0.135 |
| Men/women | 4/14 | 6/26 | 0.768 |
| Cardiac output (l/min) | 6.33 ± 1.37 | 5.55 ± 1.48 | 0.028 |
| PVR (WU) | 2.52 ± 0.57 | 1.79 ± 0.55 | <0.001 |
| Medication | |||
| Beta-blocker | 11 (61 %) | 19 (59 %) | 0.904 |
| Thiamazole | 14 (78 %) | 24 (75 %) | 0.825 |
PVR pulmonary vascular resistance
Table 2.
Biochemical and serologic findings
| Pulmonary hypertension | p value | ||
|---|---|---|---|
| Present (n = 18) | Absent (n = 32) | ||
| Free T4 (ng/dL) | 3.61 ± 1.69 | 3.40 ± 1.91 | 0.492 |
| Free T3 (pg/mL) | 11.33 ± 5.32 | 9.21 ± 5.52 | 0.125 |
| TSH (µU/mL) | 0.008 ± 0.005 | 0.010 ± 0.013 | 0.679 |
| TRAb (lU/L) | 115 ± 110 | 29 ± 31 | <0.001 |
| Creatine phosphokinase (U/L) | 65 ± 52 | 52 ± 33 | 0.419 |
| C-reactive protein (mg/dL) | 0.128 ± 0.149 | 0.156 ± 0.152 | 0.332 |
| Cholesterol (mg/dL) | 163 ± 43 | 158 ± 34 | 0.694 |
| Albumin (g/L) | 41.4 ± 4.5 | 40.0 ± 5.0 | 0.266 |
| White blood cells (/µL) | 5811 ± 1655 | 5381 ± 1597 | 0.374 |
T3 triiodothyronine, T4 thyroxine, TRAb thyroid-stimulating hormone receptor antibody, TSH thyroid-stimulating hormone
Fig. 1.
Correlation between pulmonary artery systolic pressure and TRAb. PAs pulmonary artery systolic pressure, TRAb thyroid-stimulating hormone receptor antibody
To determine the important variables present in patients with Graves’ disease that may be related to pulmonary artery systolic pressure, 4 variables (PVR, cardiac output, TRAb and free T3) were used in the multivariate analysis. From the analysis, in addition to PVR (standard regression coefficient = 0.831, p < 0.001) and cardiac output (standard regression coefficient = 0.592, p < 0. 001), TRAb (standard regression coefficient = 0.178, p < 0.001) emerged as a significant variable related to pulmonary artery systolic pressure.
Discussion
The effects of thyroid hormone on the heart and vasculature are increase in heart rate, left ventricular contractility and blood volume, and decrease in systemic vascular resistance [1, 4]. However, the symptoms and signs of Graves’ disease result not only from direct and indirect effects of hyperthyroidism but also caused by autoimmune process of Graves’ disease [1–6]. Association between hyperthyroidism and pulmonary hypertension has been described, but the underlying mechanisms of these 2 conditions have not been clearly identified. Among our patients with Graves’ disease, elevated pulmonary artery systolic pressure was found in 36 % by Doppler echocardiography, a widely used method for estimating pulmonary artery systolic pressure, which is consistent with previous reports that elevated pulmonary artery systolic pressure is a relatively common complication in patients with Graves’ disease.
Increase in cardiac output and/or elevated PVR are the 2 major pathophysiologic factors determining the elevation of pulmonary artery systolic pressure. The factors related to the increased cardiac output in patients with hyperthyroidism are increases of heart rate and myocardial contractility due to the effects of hyperthyroidisms on the sympathetic nerve system, and a decrease of the systemic vascular resistance largely due to excessive nitric oxide production [18]. Furthermore, increase in cardiac output is also observed in hyperthyroidism due to an increase in blood volume resulting from increased net tubular reabsorption of sodium [19]. In contrast to the effect of thyroid hormone to decrease systemic vascular resistance, it has been suggested that pulmonary vascular resistance is not decreased by hyperthyroidism [20]. Thyroid hormones may affect the pulmonary vasculature by affecting the sympathetic nervous system or alteration of the energy metabolism; enhanced catecholamine sensitivity, decrease in cholinergic tone, increased metabolism of the intrinsic pulmonary vasodilating substances and decreased metabolism of the vasoconstrictors, which together will account for an increase in the PVR [1–3, 21, 22]. Moreover, an increase in cardiac output could cause endothelial damage, and hence increase PVR. In this study, the patients with pulmonary arterial hypertension had significantly higher cardiac output and PVR compared to those without. Our data indicate that increased cardiac output and PVR due to excessive thyroid hormone were the factors associated with an elevation of pulmonary artery pressure in our patients with Graves’ disease.
Antithyroid antibodies are a marker for generalized immune activation. Chu et al. [23] demonstrated a high prevalence of autoimmune thyroid disease in prospective series of pulmonary hypertension and suggested an autoimmune pathogenetic link between these 2 conditions. On the other hand, Merces’ reported that elevated cardiac output partially explains the pathogenesis for pulmonary hypertension in hyperthyroidism, and they did not support the autoimmune pathogenesis for pulmonary hypertension [4]. In our patients with Graves’ disease, despite no significant correlation between pulmonary artery systolic pressure and free T3, TRAb had a good positive correlation with pulmonary artery systolic pressure. Graves’ disease is an autoimmune disease in which excessive amount of thyroid hormone is produced by TRAb. TRAb binds to the TSH receptors and chronically stimulates them resulting in an abnormally high production of thyroid hormones. Therefore, almost all patients with Graves’ hyperthyroidism have detectable TRAb that has a major pathogenic role in Graves’ disease; persistent elevation correlates with disease activity, while remission is usually accompanied by a decrease in their activity [24, 25]. The discrepancy between the 2 studies is probably due to the lower incidence of autoimmune hyperthyroidism in Merces’ study (54 % for antiperoxidase antibody and 35 % for antithyroglobulin antibody) compared to our study (100 % for TRAb). Nicolls et al. [26] reported the role of autoimmunity in the development of pulmonary hypertension. They indicated the endothelial cell destruction by immune-mediated injury, which results in the generation of rapidly proliferative apoptosis-resistant endothelial cells, leading to vascular remodeling and hence the development of pulmonary hypertension. Considering the results that TRAb was found to be an important factor associated with elevated pulmonary artery systolic pressure by the multivariate analysis, our data indicate that pathogenic autoantibodies targeting endothelial cells could cause endothelial damage or dysfunction and play a role in Graves’ disease-linked elevated pulmonary artery systolic pressure.
Three limitations of our study should be addressed. First, pulmonary artery systolic pressure was estimated non-invasively. Although echocardiography may be imprecise in determining actual pressure compared to invasive evaluation of pulmonary artery systolic pressure, considering the fact that echocardiography may underestimate pulmonary artery systolic pressure in patients with severe pulmonary hypertension and overestimate pulmonary artery systolic pressure in patients with normal pressures, our conclusion would probably not be altered by an invasive measurement. Moreover, invasive measurement is not ethical or practical in outpatients. Second, we may have underestimated the prevalence of pulmonary hypertension because pulmonary artery systolic pressure could not be determined in 9 patients (18 %) due to the absence of tricuspid regurgitation. Nonetheless, data obtained by cardiac catheterization show that moderate or severe pulmonary hypertension is almost always associated with tricuspid regurgitation. Third, medical therapy was started in most of the patients at the time of cardiovascular evaluation because clinician judged it was necessary to start treatment. However, all the patients were in hyperthyroid state with elevated TRAb and remission is usually accompanied by decrease in TRAb activity.
In conclusion, in addition to the effect of thyroid hormone on the cardiovascular system, autoimmune-mediated pulmonary vascular remodeling may play a role in Graves’ disease-linked elevated pulmonary artery systolic pressure.
Conflict of interest
None.
References
- 1.Weetmen AP. Graves’ disease. N Engl J Med. 2000;343:1236–1248. doi: 10.1056/NEJM200010263431707. [DOI] [PubMed] [Google Scholar]
- 2.Klein I, Danzi S. Thyroid disease and the heart. Circulation. 2007;116:1725–1735. doi: 10.1161/CIRCULATIONAHA.106.678326. [DOI] [PubMed] [Google Scholar]
- 3.Nakchbandi IA, Wirth JA, Inzucchi SE. Pulmonary hypertension caused by Graves` thyrotoxicosis. Normal pulmonary hemodynamics restored by 131I treatment. Chest. 1999;116:1483–1485. doi: 10.1378/chest.116.5.1483. [DOI] [PubMed] [Google Scholar]
- 4.Merce J, Ferras S, Oltra C, Sanz E, Vendrell J, Simon I, Camprubi M, Bardaji A, Ridao C. Cardiovascular abnormality in hyperthyroidism: a prospective Doppler echocardiographic study. Am J Med. 2005;118:126–131. doi: 10.1016/j.amjmed.2004.08.018. [DOI] [PubMed] [Google Scholar]
- 5.Marvisi M, Zambrelli P, Brianti M, Civardi G, Lampugnani R, Delsignore R. Pulmonary hypertension is frequent in hyperthyroidism and normalizes after therapy. Eur J Int Med. 2006;17:267–271. doi: 10.1016/j.ejim.2005.11.023. [DOI] [PubMed] [Google Scholar]
- 6.Siu CW, Zhang XH, Yung C, Kung AWC, Lau CP, Tse HF. Hemodynamic changes in hyperthyroidism-related pulmonary hypertension: a prospective echocardiographic study. J Clin Endocrinol Metab. 2007;92:1736–1742. doi: 10.1210/jc.2006-1877. [DOI] [PubMed] [Google Scholar]
- 7.Kim BH, Cho KI, Kim SM, Kim N, Han J, Kim JY, Kim IJ. Heart rate reduction with ivabradine prevents thyroid hormone-induced cardiac remodelling in rat. Heart Vessels. 2013;28:524–535. doi: 10.1007/s00380-012-0304-z. [DOI] [PubMed] [Google Scholar]
- 8.Yock PG, Popp RL. Noninvasive estimation of right ventricular systolic pressure by Doppler ultrasound in patients with tricuspid regurgitation. Circulation. 1984;70:657–662. doi: 10.1161/01.CIR.70.4.657. [DOI] [PubMed] [Google Scholar]
- 9.Stephen B, Dalal P, Berger M, Schweitzer P, Hecht S. Noninvasive estimation of pulmonary diastolic pressure in patients with tricuspid regurgitation by Doppler echocardiography. Chest. 1999;116:73–77. doi: 10.1378/chest.116.1.73. [DOI] [PubMed] [Google Scholar]
- 10.Grunig E, Janssen B, Mereles D, Barth U, Borst MM, Vogt IR, Fisher C, Olschewski H, Kuecherer HF, Kubler W. Abnormal pulmonary artery pressure response in asymptomatic carriers of pulmonary hypertension gene. Circulation. 2000;102:1145–1150. doi: 10.1161/01.CIR.102.10.1145. [DOI] [PubMed] [Google Scholar]
- 11.McGoon M, Gutterman D, Steen V, Barst R, MaCrory DC, Fortin TA, Loyd JE. Screening, early detection, and diagnosis of pulmonary arterial hypertension: ACCP evidence-based clinical practice guidelines. Chest. 2004;126:14S–34S. doi: 10.1378/chest.126.1_suppl.14S. [DOI] [PubMed] [Google Scholar]
- 12.Henry WL, Gardin JM, Ware JH. Echocardiographic measurements in normal subjects from infancy to old age. Circulation. 1980;62:1054–1060. doi: 10.1161/01.CIR.62.5.1054. [DOI] [PubMed] [Google Scholar]
- 13.Currie PJ, Seward JB, Chan KL, Fyfe DA, Hagler DJ, Mair DD, Reeder GS, Nishimura RA, Tajik AJ. Continuous wave Doppler determination of right ventricular pressure: a simultaneous Doppler-catheterization study in 127 patients. J Am Coll Cardiol. 1985;6:750–756. doi: 10.1016/S0735-1097(85)80477-0. [DOI] [PubMed] [Google Scholar]
- 14.AmanoH Toyoda S, Arikawa T, Inami S, Otani N, Nishi Y, Kitagawa Y, Taguchi I, Abe S, Inoue T. Left ventricular function in pulmonary hypertension. Heart Vessels. 2013;28:505–509. doi: 10.1007/s00380-012-0272-3. [DOI] [PubMed] [Google Scholar]
- 15.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stwart WJ. Chamber quantification writing group; American society of echocardiography’s guidelines and standards committee; European association of echocardiography. Recommendations for chamber quantification: a report from the American society of echocardiography’s guidelines and standards committee and the chamber quantification writing group, developed in conjunction with the European association of echocardiography, a branch of the European society of cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 16.Chemla D, Castelain V, Humbert M, Hebert JL, Simonneau G, Lecarpentier Y, Herve P. New formula for predicting mean pulmonary artery pressure using systolic pulmonary artery pressure. Chest. 2004;126:1313–1317. doi: 10.1378/chest.126.4.1313. [DOI] [PubMed] [Google Scholar]
- 17.Lindqvist P, Soderberg S, Gonzalez MC, Tossavainen E, Henein MY. Echocardiography based estimation of pulmonary vascular resistance in patients with pulmonary hypertension: a simultaneous Doppler echocardiography and cardiac catheterization study. Eur J Echocardiogr. 2011;12:961–966. doi: 10.1093/ejechocard/jer222. [DOI] [PubMed] [Google Scholar]
- 18.Napoli R, Biondi B, Guardasole V, MatarMazzo M, Pardo F, Angelini V, Fazio S, Sacca L. Impact of hyperthyroidism and its correlation on vascular reactivity in humans. Circulation. 2001;104:3076–3080. doi: 10.1161/hc5001.100621. [DOI] [PubMed] [Google Scholar]
- 19.Klein I, Levey GS. The cardiovascular system in thyrotoxicosis. In: Braverman LE, Utiger RD, editors. Werner and Ingbar’s the thyroid. 7. Philadelphia: Lippincott-Raven; 1996. pp. 607–615. [Google Scholar]
- 20.Danzi S, Klein I. Thyroid hormone and blood pressure regulation. Curr Hypertens Rep. 2003;5:513–520. doi: 10.1007/s11906-003-0060-7. [DOI] [PubMed] [Google Scholar]
- 21.Arroliga AC, Dweik RA, Rafanan AL. Primary pulmonary hypertension and thyroid disease. Chest. 2000;118:1224–1225. doi: 10.1378/chest.118.4.1224. [DOI] [PubMed] [Google Scholar]
- 22.Hyman AL, Kadowitz PJ. Enhancement of alpha and beta-adrenoreceptor responses by elevations in vascular tone in pulmonary circulation. Am J Physiol. 1986;250:H1109–H1116. doi: 10.1152/ajpheart.1986.250.6.H1109. [DOI] [PubMed] [Google Scholar]
- 23.Chu JW, Kao PN, Faul JL, Doyle RL. High prevalence of autoimmune thyroid disease in pulmonary arterial hypertension. Chest. 2002;122:1668–1673. doi: 10.1378/chest.122.5.1668. [DOI] [PubMed] [Google Scholar]
- 24.Massart C, Gibassier J, d’Herbomez M. Clinical value of M22 based assay for TSH-receptor antibody (TRAb) in the follow-up of antithyroid drug treated Graves’ disease: comparison with the second generation human TRAb assay. Clin Chim Acta. 2009;407:62–66. doi: 10.1016/j.cca.2009.06.033. [DOI] [PubMed] [Google Scholar]
- 25.Kamijo K. Study on cutoff value setting for differential diagnosis between Graves’ disease and painless thyroiditis using the TRAb (Elecsys TRAb) measurement via the fully automated electrochemiluminescence immunoassay system. Endocr J. 2010;57:895–902. doi: 10.1507/endocrj.K10E-199. [DOI] [PubMed] [Google Scholar]
- 26.Nicolls MR, Tarasevicience-Stwart L, Rai PR, Badesch DB, Voelkel NF. Autoimmunity and pulmonary hypertension: a perspective. Eur Respir J. 2005;26:1110–1118. doi: 10.1183/09031936.05.00045705. [DOI] [PubMed] [Google Scholar]