Abstract
BACKGROUND:
The quality of chest compressions can be significantly improved after training of rescuers according to the latest national guidelines of China. However, rescuers may be unable to maintain adequate compression or ventilation throughout a response of average emergency medical services because of increased rescuer fatigue. In the present study, we evaluated the performance of cardiopulmonary resuscitation (CPR) in training of military medical university students during a prolonged basic life support (BLS).
METHODS:
A 3-hour BLS training was given to 120 military medical university students. Six months after the training, 115 students performed single rescuer BLS on a manikin for 8 minutes. The qualities of chest compressions as well as ventilations were assessed.
RESULTS:
The average compression depth and rate were 53.7±5.3 mm and 135.1±15.7 compressions per minute respectively. The proportion of chest compressions with appropriate depth was 71.7%±28.4%. The average ventilation volume was 847.2±260.4 mL and the proportion of students with adequate ventilation was 63.5%. Compared with male students, significantly lower compression depth (46.7±4.8 vs. 54.6±4.8 mm, P<0.001) and adequate compression rate (35.5%±26.5% vs. 76.1%±25.1%, P<0.001) were observed in female students.
CONCLUSIONS:
CPR was found to be related to gender, body weight, and body mass index of students in this study. The quality of chest compressions was well maintained in male students during 8 minutes of conventional CPR but declined rapidly in female students after 2 minutes according to the latest national guidelines. Physical fitness and rescuer fatigue did not affect the quality of ventilation.
KEY WORDS: Basic life support, Cardiopulmonary resuscitation, Chest compression, Ventilation, Military
INTRODUCTION
Out-of-hospital cardiac arrest (OHCA), a major worldwide public health problem, is the leading cause of non-traumatic death in the military population.[1–3] It is well recognized that early initiation of cardiopulmonary resuscitation (CPR) may lead to the return of spontaneous circulation in victims with cardiac arrest.[4,5] The high quality of CPR, which is defined as adequate compression depth and rate, complete chest recoil, minimized interruption and avoidance of excessive ventilation, is an important determinant for the resuscitation and survival of these victims.[6]
Because the quality of CPR is a prerequisite for good outcomes, the latest AHA and ERC guidelines not only encourage bystanders CPR for all rescuers regardless of training but also emphasize the rescuers to push to a depth of at least 50 mm at a rate of at least 100 compressions per minute, to allow full chest recoil, and to minimize interruptions in chest compressions. Additionally, trained rescuers should also provide ventilations with a compression/ventilation ratio of 30:2.[7,8]
Recent studies[9–11] have shown that the quality of chest compressions was significantly improved when rescuers were trained to perform deeper compression under the latest guidelines. However, deeper compression required greater effort and increased physical exertion might cause rapid rescuer fatigue.[10] Rescuer fatigue adversely affected the performance of CPR and the quality of chest compressions was significantly declined within 1–3 minutes in manikin studies.[13–16] Simulation studies[12,14] also demonstrated that there was a huge inter-individual distribution in the quality of CPR and that individuals with lighter body weight or smaller stature were prone to have rescuer fatigue.
From the military perspective, first aid training for soldiers not only helps to preserve combat power in the combat zone, but also saves lives in medical assistance for natural disaster. Since its introduction in the army, best clinical experience has been combined with the best available evidence to provide all soldiers with life-saving skills.[17] CPR for primary cardiac arrest in the military population also presents unique logistical and treatment challenges.[18] However, the performances of CPR in military healthcare providers are still unknown. In the present study, we evaluated the performance of conventional CPR in military medical university students 6 months after training following the 2010 AHA guidelines. We also compared the quality of CPR between males and females during a prolonged basic life support (BLS). The study was conducted at a medical training center of the Third Military Medical University Affiliated Southwest Hospital. Ethical approval was waived for this observational manikin study.
METHODS
Study design and participants
This retrospective study was designed to evaluate the quality of CPR in military medical university students and compared the performance between males and females 6 months after training following the 2010 AHA guidelines.
One hundred and twenty undergraduate volunteers from Third Military Medical University were recruited to participate in this study between November 2013 and June 2014. Among the students, 60 (56 males) were from the School of Basic Medicine and 60 (51 males) from the School of Biomedical Engineering. The majority (89.2%)of the students were males because the proportion of female students was nearly 10% in military medical universities. All of the students were inexperienced in CPR since BLS training was not a mandatory part of the student’s curriculum.
Study protocol
The conventional 180-minute instructor-based BLS training course was conducted according to the 2010 AHA guidelines for CPR and emergency cardiovascular care (chest compression/ventilation ratio of 30:2). The instructor/participant ratio was 1:4.
After the training and a short break, BLS skill assessment was conducted according to 1-rescuer adult BLS skills testing sheet for 2 minutes. Those who failed to pass the test were exercised under the supervision of the instructor until they finally passed.
Half a year later, the students were invited to participate in assessment of their CPR performance in a simulated cardiac arrest scenario. During the evaluation of resuscitation skills, all students were individually tested and not allowed to communicate with each other. Every student was required to perform 20 cycles of 30:2 CPR. CPR was performed using the Resusci Anne Skill Reporter manikin (Leardal Medical Corporation, Stavanger, Norway) that was placed on the floor. No feedback was provided to the students during the entire CPR procedure.
Measurements
Comprehensive demographic information was collected for all students, including age, gender, height, weight, and calculated body mass index (BMI). CPR data were collected by Resusci Anne SkillReporter (Leardal Medical Corporation, Stavanger, Norway) every 5 cycles of CPR.
Quality of chest compression was assessed by mean compression depth, mean compression rate, the proportion of compressions with appropriate depth (at least 50 mm) and proportion of participants with mean compression depth greater than 50 mmutes. The quality of ventilation was evaluated by mean ventilation volume, the proportion of ventilations with adequate volume (within 400–1 000 mL), the proportion of ventilations with excessive volume (>1 000 mL), and the proportion of participants with mean ventilation volume between 400–1 000 mL.
Statistical analysis
The data were presented as mean±SD. Normal distribution was confirmed with the Kolmogorov-Smirnov test. Continuous variables were compared with parametric Student’s t test or the Mann-Whitney U test for nonparametric data. Changes in performance of CPR over time within subjects were analyzed using Friedman’s non-parametric repeated measures and analysis of variance (ANOVA) with Dunn’s multiple comparisons correction used as appropriate. The relationship between the demographic characteristics and quality of chest compressions (proportion of compressions with appropriate depth) was analyzed with bivariate correlation analysis. For the comparison of categorical variables such as the proportion of gender, the chi-square test was used. P<0.05 was considered statistically significant.
RESULTS
All of the 120 students completed the BLS training courses. Two students (1 male and 1 female) were dropped out from the study because they refused to perform the skill test. After 6 months, 115 students (103 males, 89.6%) participated in the evaluation. The mean age of these students was 22.9±1.0 years. The average height, body weight and BMI were 172.4±6.3 cm, 64.4±9.5 kg and 21.6±2.3 kg/m2, respectively.
Overall performance
The mean time to finish 20 cycles 30:2 CPR was 7.7±0.9 minutes. An average of 5.3±18.5 wrong hand placement and 4.6±12.9 incomplete chest recoil was reported in every student during the entire CPR period. The average compression depth and rate were 53.7±5.3 mm and 135.1±15.74 compressions per minute respectively. The average proportion of compressions with appropriate depth was 71.7%±28.4%. A total of 91 (79.1%, 88 males and 3 females) students showed average compression depth greater than 50 mm, and 107 (93.0%, 99 males and 8 females) students showed average depth greater than 45 mm.
Figure 1 illustrates the changes in performances of chest compression during the entire CPR period. The compression rate obviously increased but the adequate compression rate decreased after 4 minutes of CPR compared with the first 2 minutes of CPR. The compression rate increased from 129.9±16.8 to 134.4±17.6 compressions per minute (P=0.002), the adequate compression rate decreased from 85.1%±22.0% to 69.6%±31.5% (P=0.001), and the proportion of students with mean compression depth greater than 50 mm decreased from 82.6% to 69.6% (P=0.03) during the last 2 minutes of CPR.
Figure 1.
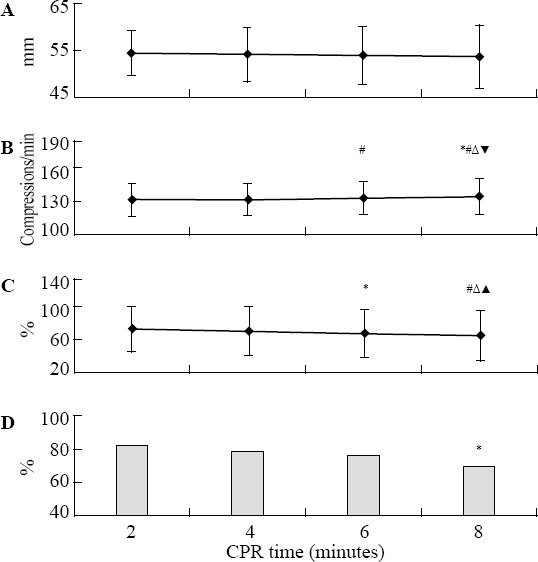
Performance of chest compressions during the 8-minute conventional cardiopulmonary resuscitation (CPR) with mean compression depth (A), mean compression rate (B), the proportion of compressions with appropriate depth (C), and the proportion of students with mean compression depth greater than 50 mm (D). *P<0.05, #P<0.01 vs. CPR 2 minutes; ΔP<0.01 vs. CPR 4 minutes; ▲P<0.05, ▼P<0.01 vs. CPR 6 minutes.
Bivariate correlation analysis showed that quality of chest compression associated with body weight (r=0.425, P<0.001), gender (r=0.385, P<0.001), BMI (r=0.352, P<0.001) and height (r=0.344, P<0.001).
The mean hands-off time for 2 ventilations in each CPR cycle was 9.7±2.1 seconds and the average ventilation volume was 847.2±260.4 mL. The adequate ventilation rate was 30.7%±25.8% and a excessive ventilation volume was 55.6%±35.3%. A total of 73 (63.5%, 37 males and 6 females) students had a mean ventilation volume ranging from 400 to 1 000 mL. The mean ventilation volume was significantly increased after 4 minutes of CPR but still below the upper limit of adequate ventilation of 1 000 mL (Figure 2). Both the proportion of ventilations with adequate volume and the proportion of students with a mean ventilation volume within 400–1 000 mL were remained unchanged during the entire CPR period.
Figure 2.
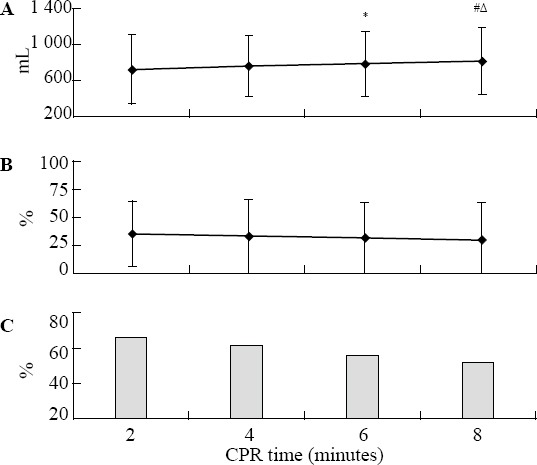
Overall performance of ventilations during the 8-minute conventional CPR with ventilation volume (A), the proportion of ventilations with adequate volume (within 400–1 000 mL) (B), the proportion of students with a mean ventilation volume between 400–1 000 mL (C). *P<0.05, #P<0.01 vs. CPR 2 minutes; ΔP<0.05 vs. CPR 4 minutes.
Performance of CPR between male and female students
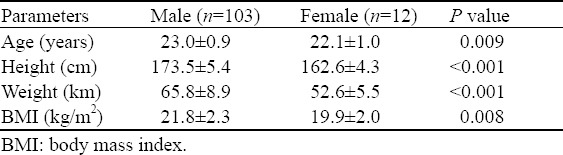
Table 1 shows the characteristics of male and female students. The female students were younger in age (22.1±1.0 vs. 23.0±0.9 year, P=0.009), shorter in height (162.6±4.3 vs. 173.5±5.4 cm, P<0.001), lighter in body weight (52.6±5.5 vs. 65.8±8.9 kg, P<0.001) and smaller in BMI (19.9±2.0 vs. 21.8±2.3 kg/cm2, P=0.008) compared with male students.
Table 1.
Comparison of characteristics of male and female students
The performance of CPR between male and female students 6 months after training is shown in Table 2. Significantly lower compression depth (46.7±4.8 vs. 54.6±4.8 mm, P<0.001) and adequate compression rate (35.5±26.5 vs. 76.1±25.1 %, P<0.001) were observed in female students compared with the male students. Although the compression rate was relatively lower during the first 6 minutes, it was still above 100 compressions per minute. There was no statistical difference in compression depth, compression rate, and adequate compression rate during the 8-minute CPR for male students. But rescuer fatigue became obvious after 2 minutes of CPR for female students and the average compression depth was dropped from 49.1±5.3 mm to 46.1±5.3 mm (P=0.01). No significant differences were observed in quality of ventilation between male and female students.
Table 2.
Quality of cardiopulmonary resuscitation between male and female students 6 months after training
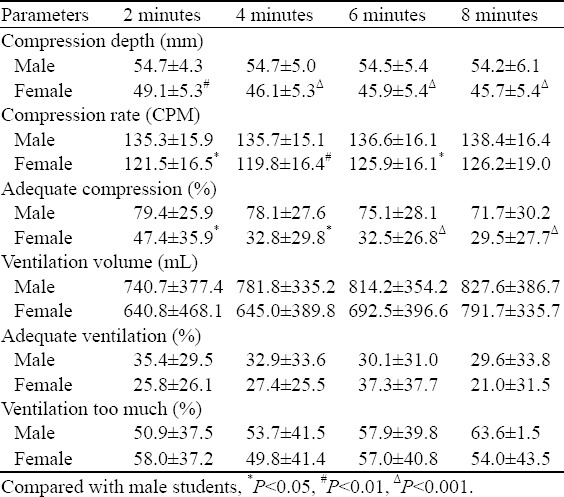
Bivariate correlation analysis revealed that the quality of chest compression related to body weight (r=0.306, P<0.001) and BMI (r=0.304, P<0.001) in male students.
DISCUSSION
We assessed the performance of CPR 6 months after training in military medical university students. We found that (1) the skills of CPR were retained after 6 months of training and average compression depth was above 50 mm for 8 minutes of conventional 30:2 CPR in this cohort of students; (2) male students could maintain a high quality of chest compression for 8 minutes while a significant decay was observed in female students after 2 minutes of CPR; and (3) physical fitness and rescuer fatigue did not affect the quality of ventilation.
CPR is one of the most vital therapeutic options for patients with cardiac arrest. The probability of survival decreases significantly after 4 minutes without CPR in witnessed arrests.[19] For a victim to have a good chance, a bystander must start CPR early and effectively since emergency medical service providers generally can’t get to a scene within 6 to 8 minutes.[20,21] Thousands of lives could be saved every year by implementing bystander CPR because effective bystander CPR provided immediately after sudden cardiac arrest could double or triple a victim’s chance of survival.[22]
However, the quality of chest compressions is influenced by age, gender, body weight and time passed since the most recent BLS training of the bystanders.[23] Rescuer fatigue, which is regarded as the primary reason for deterioration of quality of chest compressions during CPR over time, has been investigated in a number of simulation and clinical studies with varying results.[14,15,24–26] In an earlier manikin study, Ochoa et al[24] demonstrated that rescuer fatigue was appreciated quickly for hospital staff and compression depth degraded after only 1 minute of CPR delivery. Ashton et al[14] found that the quality of chest compressions decayed within 3 minutes of CPR and this effect was greater in female doctors and nurses due to their smaller stature in another manikin study. Bjørshol et al[25] observed that there was no decline in quality of chest compression during 10 minutes of BLS with different compression ventilation ratios for professional paramedics. In another simulated manikin study, Bjørshol et al[15] also demonstrated that only half of the paramedics achieved guideline recommended compression depth during a prolonged advanced life support, but rescuer fatigue within the first 2 minutes was rare. Sugerman et al[26] reported that compression depth decay became evident after 90 seconds of CPR, but compression rate did not change during actual in-hospital CPR with audiovisual feedback.
The effect of rescuer fatigue on chest compressions in accordance with the 2010 AHA/ERC guidelines has also been investigated in simulation studies. McDonald et al[13] reported that the quality of chest compression decreased over time and falling most rapidly within the first 2 minutes of conventional CPR in 62 health science students. Yang et al[10] investigated the quality of chest compressions during compression-only CPR under the latest guidelines and its effect on rescuer fatigue in undergraduate volunteers. The authors found that both depth and number of compressions in appropriate depth dropped rapidly after 1 minute of CPR. In a recent clinical study, Kampmeier et al[11] documented that mean compression depth increased from 47.1 mm to 49.6 mm after the implementation of new guidelines, but the proportion of chest compressions reaching the minimal required depth decreased from 73.9% to 49.1%.
In the present study a relative faster compression rate was observed and the results were consistent with those of other two studies that a push fast recommendation caused increased chest compression rates.[10,27] However, the mean compression depth was maintained at an optimal level and 79.1% of students achieved an average compression depth of >50 mm during the 8-minute conventional CPR at 6-month retention test. Although a relative decrease in the proportion of compressions with appropriate depth was observed after 4 minutes, the adequate compression rate of 67.3% during the last 2 minutes of CPR was still encouraging. There were three major factors for the high quality of chest compression. Firstly, since the majority of students were male and their stature played a considerably role in the performance of chest compression, and a high quality of chest compression was therefore observed.[12] When evaluated separately, the recommended compression depth was maintained stably in male students while a significant decay was present in female students after 2 minutes of CPR because of their physiologic differences. Secondly, the physical agility for military students was relatively stronger because of routine military training. Compared with the results reported by McDonald et al,[13] the ratio of adequate compressions was higher in this population even though their body weight, height and BMI were comparable. We suspected that the physical fitness of the students was enhanced because of military training, and that rescuer fatigue was insignificant in the students. Thirdly, compared with conventional CPR, more physical exertion was required and rescuer fatigue might be greater when compression-only CPR was performed. As a recommended alternative to conventional CPR for untrained lay rescuers, compression-only CPR was attractive because it was easier to perform and delivered a greater number of chest compressions than conventional CPR. However, two manikin studies[28,29] have confirmed that the quality of chest compressions declined rapidly within 2 minutes in compression-only CPR due to the increased number of chest compression delivery. In the present study, the students took around 9.7 seconds to give 2 ventilations in each cycle of CPR, resulting in a total of 40.2% interruption in chest compressions during the testing period. The longer hands-off time caused by ventilations might serve as a rest to recovery from fatigue and resulted in prolonged high quality of chest compressions in conventional CPR.
We observed that there was no deterioration in quality of ventilation over the 8-minute course of CPR. Despite an apparent increase in mean ventilation volume after 4 minutes, both the proportion of ventilations with adequate volume and the proportion of students with mean ventilation volume between 400–1 000 mL were remained unchanged. Additionally, although the ratio of adequate ventilation was lower and nearly half of the ventilations were over sized when each of the individual ventilations was analyzed, the average volume was still within the adequate range and 63.5% of the students delivered a satisfactory ventilation in terms of mean ventilation volume. At the same time, gender, physical fitness and rescuer fatigue did not influence the quality of ventilations.
Even though CPR performed by layperson bystanders improves the odds of survival from OHCA, only about 4.5%%–22.9% of victims received bystander CPR in Asia.[21,30] The rate was lower than that (28%–46%) of bystander CPR in America and Europe.[31–33] Barriers for implementation of bystander CPR include fear of possible harm to victims, concern for incorrect or poor CPR, legal liability, etc.[34,35] The challenge is therefore to train more people capable of performing CPR. The results of the current study support BLS training in military, police and armed police forces, especially in communities with a low prevalence rate of bystander CPR.[36,37] Since the majority of the participants are males and the decay in the quality of CPR was unobvious during a prolonged BLS, such personnel may enhance the survival from OHCA when trained as first-aid providers.
Certain limitations need to be addressed in our study. Firstly, we evaluated the performance of CPR in military medical university students during a prolonged BLS, but no comparable non-military students served as controls. Secondly, these participants used for this study represented a physically fit cohort in military medical university, but the performance of CPR was not representative to the general population of the army, police or armed police forces. Thirdly, we demonstrated that the quality of conventional CPR could be well maintained for up to 8 minutes in male students, but their performance on the compression-only CPR is still unknown. Finally, CPR in simulated scenario couldn’t appropriately take into account those issues such as chest-wall molding and physiologic differences in cardiac arrest victims so that their performance in a real situation of CPR still needs to be investigated.
In conclusion, performance of CPR was related to body weight, gender and BMI of participants in this cohort of military medical university students. The quality of chest compressions was well maintained for males during 8 minutes of conventional CPR but declined rapidly for females after 2 minutes. Physical fitness and rescuer fatigue did not affect the quality of ventilation.
Footnotes
Funding: This study was supported by a grant from the National Natural Science Foundation of China (NSFC81271656, YL).
Ethical approval: Ethical approval was waived for this observational manikin study.
Conflicts of interest: The authors declare that there are no conflicts of interest related to the publication of this paper.
Contributors: Wang J proposed the study, analyzed the data and wrote the first draft. All authors contributed to the design and interpretation of the study and to further drafts.
REFERENCES
- 1.Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81:1479–1487. doi: 10.1016/j.resuscitation.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Eckart RE, Scoville SL, Campbell CL, Shry EA, Stajduhar KC, Potter RN, et al. Sudden death in young adults: a 25-year review of autopsies in military recruits. Ann Intern Med. 2004;141:829–834. doi: 10.7326/0003-4819-141-11-200412070-00005. [DOI] [PubMed] [Google Scholar]
- 3.Tarmey NT, Parka CL, Bartelsa OJ, Koniga TC, Mahoney PF, Mellor AJ. Outcomes following military traumatic cardiorespiratory arrest: a prospective observational study. Resuscitation. 2011;82:1194–1197. doi: 10.1016/j.resuscitation.2011.04.018. [DOI] [PubMed] [Google Scholar]
- 4.Wissenberg M, Lippert FK, Folke F, Weeke P, Hansen CM, Christensen EF, et al. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. J Am Med Assoc. 2013;310:1377–1384. doi: 10.1001/jama.2013.278483. [DOI] [PubMed] [Google Scholar]
- 5.Nolan J, Soar J, Eikeland H. The chain of survival. Resuscitation. 2006;71:270–271. doi: 10.1016/j.resuscitation.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Meaney PA, Bobrow BJ, Mancini ME, Christenson J, de Caen AR, Bhanji F, et al. Cardiopulmonary resuscitation quality: improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation. 2013;128:417–435. doi: 10.1161/CIR.0b013e31829d8654. [DOI] [PubMed] [Google Scholar]
- 7.Travers AH, Rea TD, Bobrow BJ, Edelson DP, Berg RA, Sayre MR, et al. Part 4: CPR overview: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S676–684. doi: 10.1161/CIRCULATIONAHA.110.970913. [DOI] [PubMed] [Google Scholar]
- 8.Nolan JP, Soar J, Zideman DA, Biarent D, Bossaert LL, Deakin C, et al. ERC Guidelines Writing Group. European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation. 2010;81:1219–76. doi: 10.1016/j.resuscitation.2010.08.021. [DOI] [PubMed] [Google Scholar]
- 9.Mpotos N, Lemoyne S, Wyler B, Deschepper E, Herregods L, Calle PA, et al. Training to deeper compression depth reduces shallow compressions after six months in a manikin model. Resuscitation. 2011;82:1323–1327. doi: 10.1016/j.resuscitation.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 10.Yang Z, Li H, Yu T, Chen C, Xu J, Chu Y, et al. Quality of chest compressions during compression-only CPR: a comparative analysis following the 2005 and 2010 American Heart Association guidelines. Am J Emerg Med. 2014;32:50–54. doi: 10.1016/j.ajem.2013.09.043. [DOI] [PubMed] [Google Scholar]
- 11.Kampmeier TG, Lukas RP, Steffler C, Sauerland C, Weber TP, Van Aken H, et al. Chest compression depth after change in CPR guidelines—improved but not sufficient. Resuscitation. 2014;85:503–508. doi: 10.1016/j.resuscitation.2013.12.030. [DOI] [PubMed] [Google Scholar]
- 12.Hasegawa T, Daikoku R, Saito S, Saito Y. Relationship between weight of rescuer and quality of chest compression during cardiopulmonary resuscitation. J Physiol Anthropol. 2014;33:16. doi: 10.1186/1880-6805-33-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McDonald CH, Heggie J, Jones CM, Thorne CJ, Hulme J. Rescuer fatigue under the 2010 ERC guidelines, and its effect on cardiopulmonary resuscitation (CPR) performance. Emerg Med J. 2013;30:623–627. doi: 10.1136/emermed-2012-201610. [DOI] [PubMed] [Google Scholar]
- 14.Ashton A, McCluskey A, Gwinnutt CL, Keenan AM. Effect of rescuer fatigue on performance of continuous external chest compressions over 3 mins. Resuscitation. 2002;55:151–155. doi: 10.1016/s0300-9572(02)00168-5. [DOI] [PubMed] [Google Scholar]
- 15.Bjørshol CA, Sunde K, Myklebust H, Assmus J, Søreide E. Decay in chest compression quality due to fatigue is rare during prolonged advanced life support in a manikin model. Scand J Trauma Resusc Emerg Med. 2011;19:46. doi: 10.1186/1757-7241-19-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vaillancourt C, Midzic I, Taljaard M, Chisamore B. Performer fatigue and CPR quality comparing 30: 2 to 15: 2 compression to ventilation ratios in older bystanders: A randomized crossover trial. Resuscitation. 2011;82:51–56. doi: 10.1016/j.resuscitation.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 17.Hodgetts TJ, Hanlan CG, Newey CG. Battlefield First Aid: a simple, systematic approach for every soldier. J R Army Med Corps. 1999;145:55–59. doi: 10.1136/jramc-145-02-02. [DOI] [PubMed] [Google Scholar]
- 18.Adams BD, Carr B, Raez A, Hunter CJ. Cardiopulmonary resuscitation in the combat hospital and forward operating base: use of automated external defibrillators. Mil Med. 2009;174:584–587. doi: 10.7205/milmed-d-01-8108. [DOI] [PubMed] [Google Scholar]
- 19.Abella B, Aufderheide T, Eigel B, Hickey RW, Longstreth WT, Jr, Nadkarni V, et al. Reducing Barriers for Implementation of Bystander-Initiated CPR. Circulation. 2008;117:704–709. doi: 10.1161/CIRCULATIONAHA.107.188486. [DOI] [PubMed] [Google Scholar]
- 20.Renkiewicz GK, Hubble MW, Wesley DR, Dorian PA, Losh MJ, Swain R, et al. Probability of a shockable presenting rhythm as a function of EMS response time. Prehosp Emerg Care. 2014;18:224–230. doi: 10.3109/10903127.2013.851308. [DOI] [PubMed] [Google Scholar]
- 21.Yan L, Huang Y, Li SS. Cardiac arrest: a case-based review. World J Emerg Med. 2014;5:171–174. doi: 10.5847/wjem.j.issn.1920-8642.2014.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wissenberg M, Lippert FK, Folke F, Weeke P, Hansen CM, Christensen EF, et al. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA. 2013;310:1377–1384. doi: 10.1001/jama.2013.278483. [DOI] [PubMed] [Google Scholar]
- 23.Takei Y, Nishi T, Matsubara H, Hashimoto M, Inaba H. Factors associated with quality of bystander CPR: the presence of multiple rescuers and bystander-initiated CPR without instruction. Resuscitation. 2014;85:492–498. doi: 10.1016/j.resuscitation.2013.12.019. [DOI] [PubMed] [Google Scholar]
- 24.Zhang FL, Yan L, Huang SF, Bai XJ. Correlations between quality indexes of chest compression. World J Emerg Med. 2013;4:54–58. doi: 10.5847/wjem.j.issn.1920-8642.2013.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bjørshol CA, Søreide E, Torsteinbø TH, Lexow K, Nilsen OB, Sunde K. Quality of chest compressions during 10 min of single-rescuer basic life support with different compression: ventilation ratios in a manikin model. Resuscitation. 2008;77:95–100. doi: 10.1016/j.resuscitation.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 26.Sugerman NT, Edelson DP, Leary M, Weidman EK, Herzberg DL, Vanden Hoek TL, et al. Rescuer fatigue during actual in-hospital cardiopulmonary resuscitation with audiovisual feedback: a prospective multicenter study. Resuscitation. 2009;80:981–984. doi: 10.1016/j.resuscitation.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hong MY, Tsou JY, Tsao PC, Chang CJ, Hsu HC, Chan TY, et al. Push-fast recommendation on performing cardiopulmonary resuscitation causes excessive chest compression rates, a manikin model. Am J Emerg Med. 2014;32:1455–1459. doi: 10.1016/j.ajem.2014.08.074. [DOI] [PubMed] [Google Scholar]
- 28.Nishiyama C, Iwami T, Kawamura T, Ando M, Yonemoto N, Hiraide A, et al. Quality of chest compressions during continuous CPR;comparison between chest compression-only CPR and conventional CPR. Resuscitation. 2010;81:1152–1155. doi: 10.1016/j.resuscitation.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 29.Hong DY, Park SO, Lee KR, Baek KJ, Shin DH. A different rescuer changing strategy between 30: 2 cardiopulmonary resuscitation and hands-only cardiopulmonary resuscitation that considers rescuer factors: a randomised cross-over simulation study with a time-dependent analysis. Resuscitation. 2012;83:353–359. doi: 10.1016/j.resuscitation.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 30.Ong ME, Shin SD, Tanaka H, Ma MH, Nishiuchi T, Lee EJ, et al. Rationale, Methodology, and Implementation of a Dispatcher-assisted Cardiopulmonary Resuscitation Trial in the Asia-Pacific (Pan-Asian Resuscitation Outcomes Study Phase 2) Prehosp Emerg Care. 2015;19:87–95. doi: 10.3109/10903127.2014.942482. [DOI] [PubMed] [Google Scholar]
- 31.Stiell I, Nichol G, Wells G, De Maio V, Nesbitt L, Blackburn J, et al. Health-related quality of life is better for cardiac arrest survivors who received citizen cardiopulmonary resuscitation. Circulation. 2003;108:1939–1944. doi: 10.1161/01.CIR.0000095028.95929.B0. [DOI] [PubMed] [Google Scholar]
- 32.Lateef F, Anantharaman V. Bystander cardiopulmonary resuscitation in prehospital cardiac arrest patients in Singapore. Prehosp Emerg Care. 2001;5:387–390. doi: 10.1080/10903120190939562. [DOI] [PubMed] [Google Scholar]
- 33.SOS-KANTO study group. Cardiopulmonary resuscitation by bystanders with chest compression only (SOS-KANTO): an observational study. Lancet. 2007;369:92092–92096. doi: 10.1016/S0140-6736(07)60451-6. [DOI] [PubMed] [Google Scholar]
- 34.Abella BS, Aufderheide TP, Eigel B, Hickey RW, Longstreth WT, Jr, Nadkarni V, et al. Reducing barriers for implementation of bystander-initiated cardiopulmonary resuscitation: a scientific statement from the American Heart Association for healthcare providers, policymakers, and community leaders regarding the effectiveness of cardiopulmonary resuscitation. Circulation. 2008;117:704–709. doi: 10.1161/CIRCULATIONAHA.107.188486. [DOI] [PubMed] [Google Scholar]
- 35.Coons SJ, Guy MC. Performing bystander CPR for sudden cardiac arrest: behavioral intentions among the general adult population in Arizona. Resuscitation. 2009;80:334–340. doi: 10.1016/j.resuscitation.2008.11.024. [DOI] [PubMed] [Google Scholar]
- 36.White RD, Asplin BR, Bugliosi TF, Hankins DG. High discharge survival rate after out-of-hospital ventricular fibrillation with rapid defibrillation by police and paramedics. Ann Emerg Med. 1996;28:480–485. doi: 10.1016/s0196-0644(96)70109-9. [DOI] [PubMed] [Google Scholar]
- 37.White RD, Bunch TJ, Hankins DG. Evolution of a community-wide early defibrillation programme experience over 13 years using police/fire personnel and paramedics as responders. Resuscitation. 2005;65:279–283. doi: 10.1016/j.resuscitation.2004.10.018. [DOI] [PubMed] [Google Scholar]


