Abstract
BACKGROUND:
The quality of treatment for critically ill children varies widely at different hospitals. This study aimed to analyze the characteristics of mortality in a pediatric emergency department (PED) at a tertiary children’s hospital in Guangzhou, China and to investigate the risk factors associated with the mortality.
METHODS:
The mortality of pediatric patients at the hospital from 2011 to 2013 was retrospectively analyzed using descriptive statistics.
RESULTS:
Altogether 466 919 patients visited the PED during the period and 43 925 of them were admitted for further observation. In 230 deaths, the ratio of boys to girls was 1.4:1, and their age ranged from 2 hours to 16 years (median, 5 months). The time from admission to death ranged from 0 to 216 hours (median, 1.5 hours). There were 92 (40%) patients who died within 24 hours after admission and 104 (45.2%) patients who died on arrival. The prominent causes of the deaths were respiratory diseases, neuromuscular disorders, cardiovascular diseases, and sepsis, most of which were ascribed to severe infection. Sixty-five deaths were associated with more than one concomitant problem. The top concomitant problems were congenital malformation, low gestational age, and severe birth asphyxia.
CONCLUSIONS:
In our center, 40% of the patients in the PED died of fatal acute diseases, and pneumonia was the first leading cause of the deaths. Almost half of the deaths occurred on arrival and the rest were due to end-stage malignant diseases. This study emphasized the importance of prevention of birth deficits by reducing deaths in infants and children.
KEY WORDS: Pediatric emergency department, Mortality, Developing counties
INTRODUCTION
Pediatric emergency medicine is still in its infancy in many regions of the world, although it is a mature discipline in developed regions.[1] In China, emergency medicine has undergone tremendous changes since the 1980s; however, it is an area that needs a precise definition of specialty and formal training, particularly in pediatric emergency medicine. Because of the large population and its distribution, access to emergency care and its quality remain a significant challenge to the healthcare system in China.[2] Hence, the quality of emergency care for critically ill children varies widely in different hospitals. Tertiary children’s hospitals and their emergency services provide healthcare to the vast majority of ill children, resulting in serious overcrowding that could influence the quality of care[3] in pediatric emergency departments (PEDs). However, there are few studies on the quality of emergency services and on characteristics of the deaths in PEDs in China. In contrast, studies from other countries have described the characteristics of the deaths in urban emergency departments (EDs),[4,5] but few of them have focused on children rather than adults. In this study, we analyzed the characteristics of child deaths in the PED of Guangzhou Women and Children’s Medical Center in south China. We aimed to investigate risk factors associated with the deaths, which may contribute to the better management of patients in PEDs.
METHODS
Study design and setting
We retrospectively analyzed the deaths reported in the PED of the Guangzhou Women and Children’s Medical Center from January 1, 2011 to November 30, 2013. The center is the largest tertiary children’s medical center in Guangzhou, South China. This center, consisting of first aid rooms and observation rooms with 50 beds, has approximately 160 000 visits annually and about 15 000 patients admitted for observation. The demographic and clinical data for each patient were kept in an electronic medical record system since December 2011, except patients who died on arrival and their data were recorded by handwritten notes. The study was approved by the Institutional Research and Ethics Committee in the medical center.
Data collection and processing
We reviewed the medical records for all deaths during the period and extracted the demographic and medical information about age, sex, mode of arrival, time to death, diagnosis or underlying cause of death, and concomitant problems. Patients were divided into the following subgroups based on age: newborns (<1 month old), infants (1 month to 1 year old), toddlers (1–3 years old), preschoolers (3–5 years old), schoolchildren (5–10 years old), and early adolescence and adolescence (10–18 years old). The underlying cause of death and concomitant problems were determined via reviewing the medical record and classified according to the International Classification of Diseases, 9th edition. The cause of death was defined as uncertain when it was too difficult to be identified. The time from admission to death was categorized as follows: 0 hours (patients were declared as dead on arrival (DOA) or in cardiopulmonary arrest with no response to resuscitation on arrival), less than 6 hours, 6 to 24 hours, 24 to 48 hours, and over 48 hours.
Data analysis
The data were collated and analyzed by descriptive statistical methods using MS Excel and SPSS version 13.0.
RESULTS
During the period from 2011 to 2013, 466 919 patients were treated in the PED. Among them, 43 925 patients were admitted to the observation area, and 230 patients died, with a mortality rate of 0.5 cases per 1 000 visits and 5.2 cases per 1 000 admissions in the observation area. The age of the deaths ranged from less than 1 day (2 hours) to 16 years. There were 32 (13.9%) patients who were transported by the emergency transportation system. No autopsies were conducted on any of the deaths.
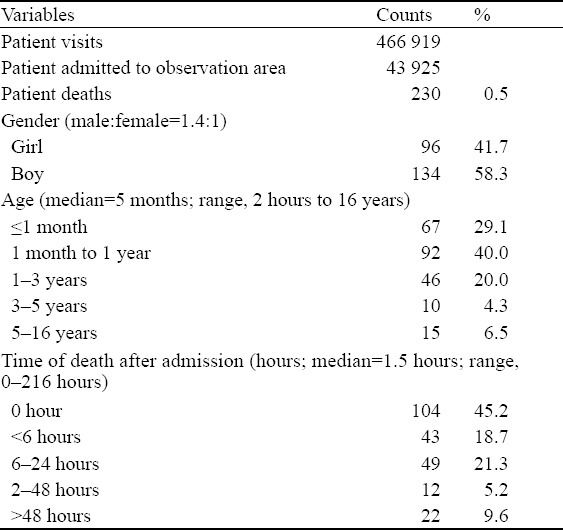
Demographic characteristics of patients and chronological distribution
Table 1 shows the deaths stratified by gender, age, and time to death. Two hundred and five (89.1%) deaths occurred in patients under 3 years old. One hundred and fifty-nine infants (1 month to 1 year old) accounted for 69.1% of the deaths in total. The number of boys was greater than that of girls, with a ratio of 1.4:1. One hundred and four (45.2 %) patients died on arrival. Ninety-two (40%) patients died within 24 hours after their admission into the observation area. Twenty-two (9.6%) patients died over 48 hours upon admission. Forty-eight (46.2%) of the DOA patients were newborns; forty patients (38.5%) were infants; eleven patients (10.6%) were toddlers; and five patients (4.8%) were older than three years.
Table 1.
Demographic characteristics and chronological distribution of the deaths
The underlying causes of the deaths
Table 2 shows the underlying causes of the deaths. The internal diseases (n=161, 65.1%), surgery diseases (n=6, 2.6%; including intestinal perforation and obstruction), accidents or unintentional injuries (n=13, 5.7%; including drowning, trauma, asphyxia caused by foreign body aspiration or infant asphyxia, and poisoning), and uncertain causes (n=50, 21.7%) were responsible for the deaths in this study. Among the internal disease-related deaths, respiratory diseases, neuromuscular disorders, and cardiovascular diseases were diagnosed at high frequencies. Further, the deaths due to respiratory diseases were most frequently associated with severe pneumonia (82.4%, 28/34). The deaths caused by neuromuscular disorders mostly were found with intracranial infection (45.5%, 15/33), such as Enterovirus 71 infection. The cardiovascular diseases-associated deaths largely were ascribed to congenital heart disease complicated with heart failure (62.1%, 18/29). Other causes for the deaths in our study population included the hematological diseases, malignant tumors (mainly leukemia), or digestive diseases including congenital biliary atresia and diarrheal disease. As the internal disease-related deaths were further divided into three subgroups, namely the DOA group, within 24 hours group, and over 24 hours group (Figure 1), cardiovascular diseases, respiratory diseases, and hematological /malignant diseases were the most dominant causes of death for the three groups, respectively.
Table 2.
The underlying causes of the deaths and concomitant problems
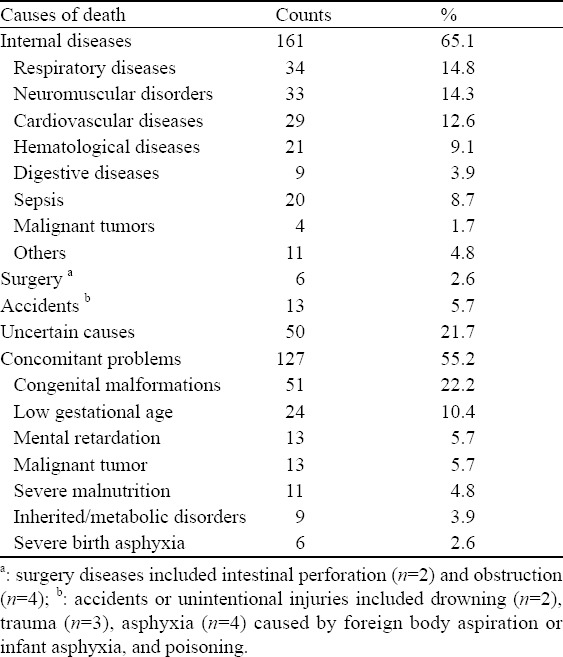
Figure 1.
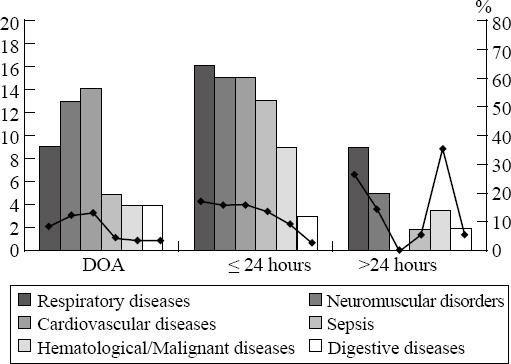
The causes of the deaths for each subgroup of patients. Patients were divided into three subgroups based on their death time, including the dead on arrival (DOA) subgroup, the within 24 hours subgroup, and the over 24 hours subgroup. Columns and dots in black line represent the numbers and the proportions of deaths associated with each type of diseases/disorders in the subgroup, respectively.
Concomitant problems
The incidence of concomitant problems was frequently seen in the deaths (55.2%, 127/230). Table 2 shows the numbers and percentages of deaths associated with the categorized concomitant problems. The patient could have more than one concomitant problem, which was very common in DOA cases as shown in Figure 2. Sixty-five (62.5%) DOA cases displayed concomitant problems, and the top three problems were congenital malformations (n=28, 26.9%), low gestational age with low birth weight (n=19, 18.3%), and severe birth asphyxia (n=6, 5.8%).
Figure 2.
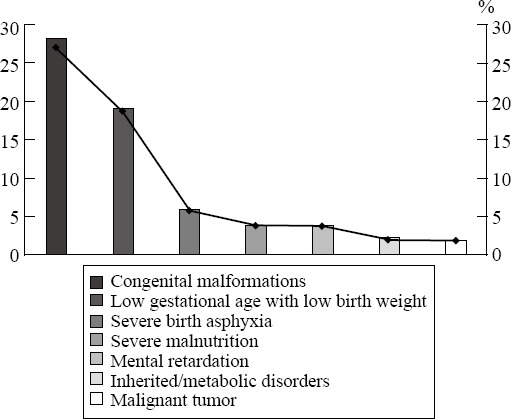
The concomitant problems of patients who died on arrival. The numbers (columns) and percentages (dots in line) of deaths associated with the concomitant problems are shown.
DISCUSSION
Mortality reflects both the severity of illness and the quality of treatment for children in pediatric emergency departments (PEDs). The risk factors associated with the mortality of children under 5 years old in developing countries are largely unknown. Here, we described the epidemiological characteristics of 230 deaths in the period from 2011 to 2013 in the PED of the largest tertiary children’s hospital in South China. This study may provide clues for the future studies on the mortality in PEDs.
Despite of rapid economy development, China is still a developing country. We reported a 0.5 death per 1 000 visits in the PED or 5.2 deaths per 1 000 admissions to the observation area in our medical center. This was lower than 37.9 deaths per 1 000 admissions from the study of Robison et al[6] and the rate of 5% from the study of Ayrton et al.[7] Both of the two reports are from developing countries. But, our rate was still higher than the rate of 1.7 deaths per 10 000 patient visits from the study of Maniktala et al[8] in the United States. Every year, approximately 10 million children under 5 years old die in the world and most of them are in developing countries.[9] We have noticed a high mortality (93.4%) for children less than 5 years old in the PED in our hospital. In an effort to achieve the global goal of a low child and infant mortality,[10] the World Health Organization’s Millennium Development Goal 4 aims to reduce the child and infant mortality in the world by two-thirds by 2015. Worldwide, the professionals working on pediatric emergency medicine are seeking to improve the quality of emergency care for children with serious illnesses and injuries in developing countries.[11–12] To accomplish this goal and also for the design of appropriate interventions, it is important to find out the risk factors associated with child mortality.
Maniktala et al[8] found that sudden infant death syndrome, also referred as dead on arrival, accounted for 31% of the deaths in the PED in a non-trauma center. In our study, we found that almost half (n=104, 45.2%) of the deaths occurred before their arrival at the PED and that nearly three-quarters (71.6%, 48/67) of the newborns and half (43.4%, 40/92) of the infants died on arrival. However, it would be difficult to determine whether the patients died of sudden infant death syndrome without consent from the parents for autopsies. Our analysis showed that more than half of the deaths (54.7%, 127/230) and approximately two-thirds (62.5%, n=65) of DOA cases had one or more concomitant problems, primarily involving severe birth asphyxia, congenital malformations, low birth weight, and/or low gestational age. The rate of concomitant problems in our study is close to that (54%) in the study of Maniktala et al.[8] These observations found that the inborn problems and birth defects are risk factors for a high incidence of DOA in infants. The high incidence of birth defects could possibly result from the policy change regarding marriage registration.[13] Other objective or subjective factors may contribute to the high incidence of DOA, such as the family’s financial condition[14–16] and subsequent attitude toward the care for a child from both the family and healthcare providers.[17,18] The high DOA rate involved a complex of factors and partially implicated inadequate maternal and infant healthcare, which is anticipated to be improved by more efforts from multiple aspects, including the strategic government assistance to poor families.[19,20]
Patients with acute infectious diseases typically died within 24 hours upon their admissions to the PED. The fatal diseases primarily were severe pneumonia caused by influenza A virus, pulmonary edema, brainstem encephalitis caused by enterovirus 71 infection, or septic shock, regardless of the inborn problems such as congenital complicated heart diseases or metabolic disorders. Accidents were not the significant causes of the deaths in our study. Since our hospital is located in downtown with a large population and heavy traffic, accident victims are preferentially transported to the nearest hospital.[21,22] Therefore, the hospital location possibly led to the low number of accident cases in our study.
A fraction of the deaths, primarily consisting of patients with end-stage malignant diseases, occurred over 24 hours or even 7 days after the patients were admitted into the PED. Principally, the time of staying in the PED should be less than 48 hours. But, in practice, many reasons such as the shortage of inpatient beds and the attitude from both families and physicians may compromise the guidelines. It has been shown that the delay in transfer to an intensive care unit (ICU) was associated with a higher mortality.[23] Thus, to shorten the time of patients staying in the PED and avoid any delay in their transfer to ICU might reduce the mortality.
In summary, our data from the PED of a tertiary hospital in south China show that one-third of patients died of fatal acute diseases, with pneumonia being the first leading causes of death, and the rest of the patients died on arrival or of end-stage malignant diseases. Our data emphasize the importance of prevention of birth deficits via reducing the deaths of infants and children, which calls for more efforts from multiple aspects, including those from government agencies. We also have realized some limitations in this study. Due to their extreme grief in emotion, some parents and families of DOA patients were either unable or unwilling to talk with us about their children’s death. This made it difficult for us to get detailed information unless the paper records could be found, not even to suggest an autopsy. Hence, for approximately one-third of the patients who died, we were unable to identify the underlying cause of death or concomitant problems. Additionally, we did not review the cases of patients who survived from cardiac arrest in the PED and therefore we did not attempt to draw any conclusion about the survival rate. Collectively, our study will be helpful for understanding the mortality of patients in PEDs in China and other developing countries.
Footnotes
Funding: None.
Ethical approval: The study was approved by the Institutional Research and Ethics Committee in the medical center.
Conflicts of interest: The authors declare no conflict of interest.
Contributors: Zhu CP proposed the study. All authors contributed to the design and interpretation of the study, and approved the final manuscript.
REFERENCES
- 1.Pei YV, Xiao F. Emergency medicine in China: present and future. World J Emerg Med. 2011;2:245–252. doi: 10.5847/wjem.j.1920-8642.2011.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kissoon N, Goldman RD. Pediatric emergency medicine: a world of potential. CJEM. 2007;9:453–458. doi: 10.1017/s1481803500015499. [DOI] [PubMed] [Google Scholar]
- 3.Committee on Pediatric Emergency Medicine. Overcrowding crisis in our nation’s emergency departments: is our safety net unraveling? Pediatrics. 2004;114:878–888. doi: 10.1542/peds.2004-1287. [DOI] [PubMed] [Google Scholar]
- 4.Mínguez Masó S, Supervía A, Campodarve I. Characteristics of deaths in a hospital emergency department. Emergencias. 2008;20:113–116. [Google Scholar]
- 5.Ugare GU, Ndifon W, Bassey IA, Oyo-Ita AE, Egba RN, Asuquo M, et al. Epidemiology of death in the emergency department of a tertiary health centre south-south of Nigeria. Afr Health Sci. 2012;12:530–537. doi: 10.4314/ahs.v12i4.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robison JA, Ahmad ZP, Nosek CA, Durand C, Namathanga A, Milazi R, et al. Decreased pediatric hospital mortality after an intervention to improve emergency care in Lilongwe, Malawi. Pediatrics. 2012;130:e676–e682. doi: 10.1542/peds.2012-0026. [DOI] [PubMed] [Google Scholar]
- 7.Ayrton J, Attwood D, Kuron Lado D. A retrospective analysis of mortality distribution in Juba Teaching Hospital, Southern Sudan. South Sudan Med J. 2009;2 http://www.Southsudanmedicaljournal.com/archive/2009-02/untitledresource.html . [Google Scholar]
- 8.Maniktala A, Pruitt C, Poirier M. Deaths in a non-trauma center pediatric emergency department: a ten-year experience. Internet J Emerg Med. 2002. p. 1. http://ispub.com/IJEM/1/2/12268 .
- 9.Murray CJ, Laakso T, Shibuya K, Hill K, Lopez AD. Can we achieve Millennium Development Goal 4? New analysis of country trends and forecasts of under-5 mortality to 2015. Lancet. 2007;370:1040–1054. doi: 10.1016/S0140-6736(07)61478-0. [DOI] [PubMed] [Google Scholar]
- 10.Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? Lancet. 2003;361:2226–2234. doi: 10.1016/S0140-6736(03)13779-8. [DOI] [PubMed] [Google Scholar]
- 11.Walkera DM, Tolentinob VR, Teacha SJ. Trends and challenges in international pediatric emergency medicine. Curr Opin Pediatr. 2007;19:247–252. doi: 10.1097/MOP.0b013e32812908b8. [DOI] [PubMed] [Google Scholar]
- 12.Maclennan C, von Xylander S, Weber MW. Improving the quality of emergency care for children in developing countries. Bull World Health Organ. 2006;84:258. doi: 10.2471/blt.06.030379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guo SW. China: the maternal and infant health care law. [Published April 16, 2012]; doi: 10.1002/9780470015902.a0005201.pub2. [Google Scholar]
- 14.Liu YL. Development of the rural health insurance system in China. Health Policy Plan. 2004;19:159–165. doi: 10.1093/heapol/czh019. [DOI] [PubMed] [Google Scholar]
- 15.Hou XY, FitzGerald G. Introduction of emergency medicine in China. Emerg Med Australas. 2008;20:363–369. doi: 10.1111/j.1742-6723.2008.01108.x. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization National Health Account database. World Bank Group website. [Accessed September 10, 2011]. http://data.worldbank.org/indicator/SH.XPD.OOPC.ZS .
- 17.Chiu HS, Chung CH. Risk management in emergency department. Hong Kong J Emerg Med. 2000;7:96–103. [Google Scholar]
- 18.World Health Organization. Geneva, Switzerland: World Health Organization; 2006. Perinatal and Neonatal Mortality for the Year 2000: Country, Regional and Global Estimates. [Google Scholar]
- 19.Dib HH, Pan X, Zhang H. Evaluation of the new rural cooperative medical system in China: is it working or not? Int J Equity Health. 2008;7:17. doi: 10.1186/1475-9276-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu Y, Hsiao WC, Eggleston K. Equity in health and health care: the Chinese experience. Soc Sci Med. 1999;49:1349–1356. doi: 10.1016/s0277-9536(99)00207-5. [DOI] [PubMed] [Google Scholar]
- 21.Pison G, Trape JF, Lefebvre M, Enel C. Rapid decline in child mortality in a rural area of Senegal. Int J Epidemiol. 1993;22:72–80. doi: 10.1093/ije/22.1.72. [DOI] [PubMed] [Google Scholar]
- 22.Greenwood BM, Bradley AK, Byass P, Greenwood AM, Menon A, Snow RW, et al. Evaluation of a primary health care programme in the Gambia. II. Its impact on mortality and morbidity in young children. J Trop Med Hyg. 1990;93:8. [PubMed] [Google Scholar]
- 23.Chalfin DB, Trzeciak S, Likourazos A, Baumann BM, Dellinger RP DELAY-ED Study Group. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–1483. doi: 10.1097/01.CCM.0000266585.74905.5A. [DOI] [PubMed] [Google Scholar]


