Abstract
Purpose
This study examines the association between child maltreatment and adolescent smoking and the extent to which internalizing behavior problems mediate this hypothesized link.
Methods
Data from 522 youth at ages 12, 14, and 16 and their caregivers were obtained as part of a prospective, longitudinal study of child abuse and neglect (LONGSCAN). Official Child Protective Services (CPS) reports of maltreatment and self-reported abusive experiences were obtained at age 12. Internalizing behavior problems were reported by caregivers at age 14. Adolescents self-reported cigarette use at age 16.
Results
A significantly higher proportion of maltreated youth (19%) reported having smoked in the last 30 days compared to non-maltreated youth (7%). A history of child maltreatment predicted smoking at age 16. Maltreatment history was associated with internalizing problems at age 14, and internalizing problems were associated with smoking. Finally, internalizing behaviors partially mediated the link between child maltreatment by age 12 and adolescent smoking at age 16.
Conclusions
Internalizing problems are one mediating pathway by which adolescents with a history of child maltreatment may initiate smoking behavior during middle-adolescence. Given the elevated rate of smoking among maltreated adolescents, it is important to identify potential pathways to better guide prevention strategies. These finding suggest that youth with a history of maltreatment should be identified as a high-risk group, and that efforts to identify and address internalizing problems in this population may be an important area of intervention to reduce adolescent smoking.
Keywords: child maltreatment, adolescent smoking, internalizing problems, LONGSCAN
Introduction
Recent data from the 2009 Monitoring the Future survey suggest that 7% of 8th graders, 12% of 10th graders, and 20% of 12th graders smoked cigarettes in the 30 days prior to the survey [1]. Compared to non-smokers, adolescent smokers are more likely to have respiratory problems, asthma and allergy symptoms [2], [3], and [4]. Adolescent smoking is also associated with the use of alcohol and other drugs, as well as other health risk behaviors [5]. Studies assessing the behavioral consequences of youth smoking reveal significant links between adolescent smoking and frequent smoking in early adulthood, alcohol use problems or dependency in adulthood, physical health problems, sleep disturbances, academic difficulties, and mental health problems [6]. Cigarette use has significant long-term adverse health effects [7]. The US Department of Health and Human Services states that cigarette use is the leading cause of preventable death in the United States [8].
Several studies have assessed the role of demographic, environmental, and social factors in adolescent smoking [9]. With regard to demographic factors, current trends suggest approximately equal rates of cigarette use among male and female youth but a higher rate of use among White Non-Hispanic youth compared to African American or Hispanic youth [5], [10] and [11]. Environmental risk factors include low socioeconomic status, accessibility and price of tobacco products, and smoking by parents, siblings and peers [1], [5], and [9]. Social and individual risk factors include lack of parental involvement, low self-esteem, low academic achievement, lack of social skills to resist peer influences, perceptions of the number of peer and adult smokers, and trauma symptoms [5], [9], and [12]. Smoking behavior may also be influenced by portrayals of smoking in the media, tobacco marketing, and local smoking laws [13] and [14].
Studies have also demonstrated an association between child maltreatment and licit and illicit substance use [15], [16], and [17], yet few have specifically examined adolescent tobacco use apart from other substances. Studies that have examined the role of maltreatment in the onset and frequency of cigarette use have primarily focused on physical and/or sexual abuse, finding that these abuse types alone or in combination significantly increased the likelihood of smoking onset during adolescence [17], [18], [19], and [20].
However, several limitations of this body of literature are worth noting. First, child maltreatment and age of smoking onset are often assessed retrospectively in an adult population and are thus subject to recall bias. Second, those studies that have examined this link in the teen population are primarily cross-sectional, which limits any temporal inferences. Third, we found only one study where neglect was included in the examination of maltreatment and smoking among adolescents [21]. Neglect and emotional abuse are notably absent from most investigations despite neglect being the most frequently reported type of maltreatment [22] and [23] and maltreatment types often co-occur [24]. For example, Hussey et al. [21] found significant associations between physical and supervisory neglect and adolescent smoking. Other studies have shown experiencing multiple types of maltreatment increases the risk of early smoking [19]. Limiting the assessment of childhood maltreatment and adolescent smoking to physical victimization may significantly undermine the complex role that maltreatment plays in the onset of smoking during adolescence. Finally, the majority of studies assessing the role of childhood maltreatment and adolescent smoking have primarily focused on bivariate associations and have not examined possible mediating pathways. Specifically, having a history of child maltreatment is associated with a host of negative consequences in adolescence including internalizing problems [25], [26], and [27] which in turn, have been associated with adolescent substance use [12] and [28]. It is possible that these factors are causally linked, yet this has not been explicitly examined to date.
Recent research suggests that internalizing problems, such as depression, may be a precursor to later tobacco use [29]. Several theories have been proposed to explain associations among smoking and internalizing problems, traumatic life events, stress, and negative affect including the self-medication model [30]. Generally these theories assert that drugs (e.g., nicotine) are used to regulate internalizing problems (e.g., mood, affect, stress) that may emerge following exposure to traumatic events. Despite the links between child maltreatment and smoking, and between internalizing problems and smoking, no study has examined whether internalizing problems may account for smoking in adolescents with a history of child maltreatment. Understanding potential mediating mechanisms can identify important intervention targets to reduce smoking in adolescents.
The purpose of the current prospective study was first to examine the link between a history of child maltreatment and adolescent smoking, and second to examine internalizing problems as a potential mediating pathway in this hypothesized link. We included neglect and emotional abuse in our assessment of child maltreatment rather than focusing on physical victimization alone. We hypothesized that internalizing problems, assessed at age 14, would mediate the link between maltreatment occurring prior to or at age 12 and adolescent self-reported smoking at age 16.
Methods
Study Sample
The present study uses data from the Longitudinal Studies of Child Abuse and Neglect (LONGSCAN), a prospective study of the antecedents and consequences of child maltreatment. LONGSCAN is a consortium of five sites, distributed across the United States (Northeast, South, Midwest, Northwest, and Southwest), and a Coordinating Center. All sites share common instruments and protocols for data collection, entry, and management. Site samples vary by maltreatment risk status and collectively include those (a) with substantiated maltreatment, (b) reported, but not substantiated, and (c) at high-risk for maltreatment due to medical or socio-demographic factors. The final baseline sample (N = 1354) comprised 65% of children reported to CPS by age 4, 20% at high-risk, but not reported, and 15% matched to maltreated children based on socio-demographic factors such as child age, ethnicity, family socioeconomic status, or medical problems [31]. Each site obtained Institutional Review Board approval. The primary caregiver at each interview provided informed consent for themselves and the youth to participate. The youth participants also provided assent.
LONGSCAN conducts face-to-face interviews with the study participants and/or their primary caregiver every two years, having begun when the children were approximately 4 years of age. Data for the current study were collected when the study participants were 12, 14, and 16 years of age. The youth and their primary caregivers participated in separate interviews using an Audio Computer Assisted Self-Administered Interview (A-CASI). A trained interviewer was present to facilitate the interviews, assist participants with any questions, and administer the few measures that were not self-administered. Data from the youth, caregiver, and reports to CPS were used for the current study.
Participants
The sample included 522 participants with complete data at ages 12, 14, and 16. Fifty-one percent of youths were female, a slight majority were African American (53%), followed by White (28%), mixed race (12%), and those of other race/ethnicity (7%). The median household income was between $25,000 and $29,999. The analysis sample did not differ from the baseline sample with regard to gender (χ2 (1, N = 1876) = 0.04, p >.05) or ethnicity (χ2 (1, N = 1876) = 1.10, p > .05). There were site differences (χ2 (4, N = 1876) = 21.69, p < .01); specifically, the Midwestern sample contributed significantly fewer participants to the analysis sample (13%) relative to the baseline representation (18%). The Northwest sample contributed more participants to the analysis sample (28%) relative to the baseline representation (19%). Chi-Square analyses revealed no demographic or maltreatment differences between the participants that were included from these sites and those who were not (p >.05).
Measures
Smoking
Smoking behavior was assessed at age 16 with a study-developed measure assessing tobacco, alcohol, and drug use [32] Youth self-reported whether they had ever smoked cigarettes, and if yes, how often in the last 30 days. For the current study, if the youth reported any use in the last 30 days, smoking was coded ‘1’, if not smoking was coded ‘0’.
Maltreatment History
The CDC defines child maltreatment as any abuse or neglect of a child under age 18 by a parent, caregiver or other person in a custodial role, including physical abuse, sexual abuse, emotional abuse, and neglect [22]. For the current study, child maltreatment is operationalized as any report to Child Protective Services (CPS) for physical abuse, sexual abuse, emotional abuse, or neglect and/or any adolescent self-reported physical abuse, sexual abuse, or emotional abuse. Thus, any official record or self-reported history of maltreatment between birth and age 12 was coded as affirmative for a history of child maltreatment. CPS case narratives were abstracted and coded using the Modified Maltreatment Classification System (MMCS) [33], which enables the standardization of maltreatment type regardless of definitional differences among agencies and across states. Because studies have demonstrated substantiated maltreatment is no better at predicting outcomes than alleged maltreatment [34] and [35], CPS allegations of maltreatment were used in the current study.
Three project-developed measures, Self-report of Physical Abuse, Self-report of Sexual Abuse, and Self-Report of Psychological Abuse [32] were administered at age 12 to assess possible lifetime experience of abuse. Each instrument contains stem questions addressing specific abuse experiences (e.g., “Has any adult ever kicked or punched you?” “Has someone touched your private parts or bottom in some way?” “Have any of your parents ever threatened to abandon or leave you forever?”). For the purposes of this study, 15 physical abuse, 11 sexual abuse, and 18 psychological abuse stem items were used to create a dichotomous indicator of any self-reported physical, sexual, or psychological abuse.
After examining the concordance between CPS records and youth self-report, Everson and colleagues [36] suggested that the inclusion of both sources of abuse history has the greatest accuracy, such that a positive endorsement from either source is sufficient for the participant to be classified as ‘abused’. If any maltreatment was indicated from CPS records or youth self-report, an affirmative code was assigned.
Internalizing Problems
Internalizing problems in the current study are defined as behavior indicative of anxiety, depression, somatic symptoms, or social withdrawal. The Child Behavior Checklist/4-18 (CBCL) [37] was used to assess internalizing behavior problems at age14. The CBCL includes 113 problem items. The Internalizing score is the sum of non-duplicate items from the Withdrawal, Anxious/Depressed, and Somatic problem scales. The CBCL has good psychometrics with regard to test-retest reliability, inter-rater agreement, and validity [37]. The raw scores were used for all analyses. Higher scores indicate greater internalizing problems.
Demographics and Other Control Variables
Demographic information on youth race/ethnicity and gender was obtained from the primary caregiver. Because adolescent smoking trends demonstrate disproportionately higher rates among Whites [3], race/ethnicity was coded as White (1) or non-White (0). Data on family income, assessed in $5,000 increments up to ≥ $50,000, were obtained from the primary caregiver at the age 16 interview.
In Home Smoking was assessed with the Risk Behavior of Family and Friends [32] measured at age 16. Youth were asked to indicate if they lived with anyone who smoked cigarettes. Responses were coded ‘1’ if yes and ‘0’ if no.
Data Analysis
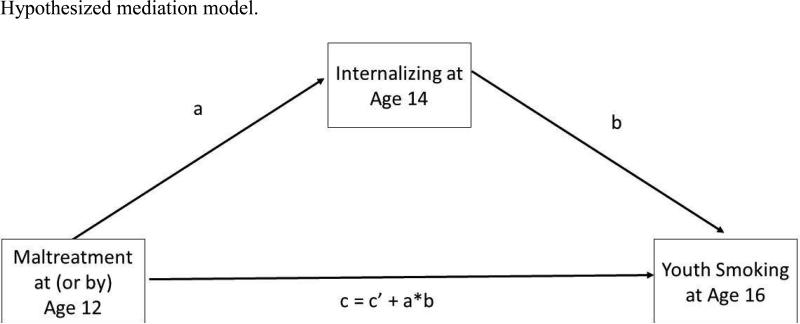
Mediation models are tests of the intervening process through which an independent variable affects an outcome. For mediation to occur, the independent variable must predict the outcome and the mediator; the mediator must predict the outcome, and the effect of the independent variable on the outcome must be significantly reduced once the mediator is added in the model [38] (Figure 1). A path analysis was used to test the mediation model. Path analysis, an extension of the regression model, is used to identify links among variables. Path analysis allows for the simultaneous testing of multiple relationships. Bias-corrected bootstrap (BCB) confidence intervals were used to test the significance of the total, direct, and indirect effect estimates using a bootstrap sample of 2000. Coefficients for the effect on youth smoking are reported as logit coefficients; the coefficients for internalizing problems are reported as linear regression coefficients. Analyses were conducted with Mplus software [39].
Figure 1.
Hypothesized mediation model.
Results
Eighty-one percent (n = 422) of participants had experienced one or more forms of maltreatment. Sixteen percent (n = 86) reported cigarette use in the last 30 days. The mean Internalizing raw score was 7.77 (SD = 7.52) corresponding to a T-score of 50.6 (SD=11.6); 24% of the sample scored in the borderline or clinical range for internalizing problems (T-score > 59). Chi-Square analyses indicated a relationship between smoking and any maltreatment, with significantly more maltreated youth engaged in smoking behavior at 16 (19%) compared to their non-maltreated counterparts (7%; [χ2 (1, N = 522) = 8.07, p < .01; OR=3.1]). Maltreated youth had significantly higher internalizing raw scores at age 14 (M = 8.5, SD =7.9) than non-maltreated youth (M = 4.6, SD =4.7; t =−6.4, p< .0001), with 27% of maltreated youth scoring in the borderline/clinical range compared to 10% of non-maltreated youth. Youth who endorsed smoking at age 16 had higher internalizing scores at age 14 (M =10.2, SD=8.1) than those who did not smoke (M =7.3, SD=7.3; t = −3.3, p<.01).
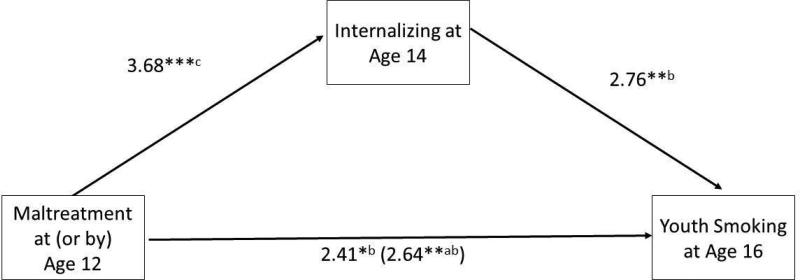
Formal model testing was conducted to determine (1) the effect of maltreatment on smoking (total effect), (2) the effect of maltreatment on internalizing problems (path a), (3) the effect of internalizing problems on smoking (path b), (4) the effect of maltreatment on smoking, controlling for internalizing problems (direct effect), and (5) the mediated effect or indirect effect (a*b) (Figure 1). Step 1 was conducted with logistic regression; steps 2 and 3 were conducted with a path analysis. In steps 1 and 3, study site, gender, race/ethnicity, income, and in-home smoking were included as control variables. In step 2, study site, gender, and race/ethnicity were included as control variables. Model fit was assessed with the root mean square error (RMSEA) and the weighted root mean residual (WRMR). RMSEA values below .5 and WRMR values below .9 are indicative of good model fit.
The logistic regression model demonstrated a significant association between maltreatment by age 12 and smoking at age 16 (total effect: β=2.64, p < .05). The path model provided a good fit for the data (R2 = .19, RMSEA = 0.00, WRMR = .06), and demonstrated significant associations between maltreatment and internalizing problems (path a: β=3.68,p < .01), and internalizing problems and smoking (path b: β=2.76,p < .01). The link between maltreatment and smoking remained significant after controlling for internalizing problems (direct effect: β=2.41,p < .05), but was diminished in strength (Figure 2). A test of the indirect effect (a*b) was significant (β=2.14,p < .05), demonstrating that internalizing problems partially mediate the effect of maltreatment on smoking (Table 1). After controlling for family income, exposure to someone in the home smoking, race/ethnicity, internalizing problems, study site, and gender, adolescents with a history of maltreatment are nearly two times as likely to smoke than their non-maltreated counterparts (OR=1.85). Every one point increase in the internalizing problems raw score was associated with a 3% increase in the odds of smoking (OR=1.02).
Figure 2.
*p ≤ .05, ** p ≤ .01, *** p ≤ .001
a Estimated total effect
b Controlling for study site, ethnicity, gender, family smoking at age 16, and family income at age 16
c Controlling for study site, ethnicity, and gender
Table 1.
Regression and Path coefficients assessing the mediating effect of internalizing problems between maltreatment and smoking.
| b | Std. b | 95% CI (BCB) | Adjusted Odds Ratio | |
|---|---|---|---|---|
| Maltreatment --> Internalizing1 | 2.35 | 3.68 | (0.99, 3.50) | - |
| Maltreatment --> Smoking2 (Total Effect) | .67 | 2.64 | (.25, 1.23) | 1.96 |
| Maltreatment --> Smoking2 (Direct Effect) | .61 | 2.41 | (.19, 1.19) | 1.85 |
| Maltreatment --> Smoking2 (Indirect Effect) | .06 | 2.14 | (.02, .12) | - |
| Internalizing --> Smoking | .025 | 2.76 | (.01, 0.04) | 1.02 |
Discussion
This study extends previous work by examining a potential pathway from child maltreatment to adolescent smoking in a prospective study of an at-risk sample. Findings from this study suggest that a history of child maltreatment by age 12 is significantly related to internalizing behaviors at age 14, which in turn are related to adolescent smoking at age 16. The effect of maltreatment on smoking was significantly reduced after accounting for internalizing problems. This suggests that internalizing problems resulting from a history of child maltreatment account significantly for adolescent smoking among maltreated adolescents.
These findings corroborate those of previous studies demonstrating an association between maltreatment and adolescent smoking [17], [18], and [21]. Overall, 16% percent of the 16-year old participants in this study reported smoking in the last 30-days, with 19% of the maltreated adolescents and 7% of the non-maltreated adolescents reported having smoked in the last 30 days. The rate for maltreated teens is considerably higher than the nationally reported 12% rate for 10th graders. This study further extends the examination of this link to include the effect of neglect as well as emotional abuse. Although studies have demonstrated a link between physical victimization and smoking, neglect and emotional abuse are notably absent from most investigations despite neglect being the most frequently reported type of maltreatment [22] and [23].
The finding that internalizing symptoms are related to smoking is also supported by prior studies [28], [30], and [40]. One longitudinal study found that childhood depressive symptoms predicted smoking in adolescence [29]. The authors speculate that there may be additional mechanisms associated with the development of depressive symptoms and cigarette use in adolescence. The results of this study suggest that child maltreatment may be one such precursor, whereby child maltreatment is predictive of internalizing problems, and internalizing problems predictive of teen smoking.
The current study supports and builds on previous findings of the association between maltreatment and adolescent smoking and offers several methodological and conceptual contributions. First, this study examined a potential mediating pathway in the link between maltreatment and smoking. Findings demonstrate that internalizing problems partially explained the link between maltreatment and smoking. Second, child maltreatment, internalizing problems, and subsequent smoking were all assessed prospectively reducing the possibility of recall bias and better establishing the temporal order of these associations leading to greater confidence when inferring pathways. That is, prior child maltreatment was assessed at age 12, internalizing behaviors assessed two years later at age 14, and smoking behavior assessed four years later at age 16. Third, possible shared method variance was avoided by the use of multiple sources of data, including CPS records, youth reports, and caregiver reports.
Some limitations of the current study are worth noting. First, there may be other important mediators that were not assessed in the current study that either alone or in conjunction with internalizing problems may more fully explain the link between maltreatment and smoking. Also factors such as gender or race/ethnicity may moderate potential mediated relationships and should be examined in future research. Second, maltreatment may not have ceased prior to age 12. Thus there may be ongoing maltreatment that influenced the association of maltreatment and smoking. Third, other potential factors such as severity of maltreatment, duration, and combinations of abuse types were not examined in this first study. It is possible that examining mediation effects among these factors as well as specific subtypes of maltreatment may subsequently illuminate differential patterns of mediation among youth with different types of maltreatment experiences. Fourth, smoking prior to age 16 was not controlled for in the current analyses. Finally, the current sample includes maltreated and/or high-risk youth participating in a longitudinal study, potentially limiting generalizability to an at-risk, study population.
Despite these limitations, our findings suggest that internalizing problems are one mediating pathway by which child maltreatment is associated with smoking behavior. Considering the high rate of tobacco use among abused and neglected youth and the likelihood of long-term dependence in early users, maltreated adolescents are particularly at risk for significant long-term health consequences as a result of early and chronic use of tobacco. Intervention efforts targeting internalizing problems, especially in maltreated youth, may have the potential, in part, to prevent the early initiation of tobacco use.
Acknowledgments
Funding: This work was supported by grants from the National Center on Child Abuse and Neglect, the Children's Bureau, Office of Child Abuse and Neglect Administration on Children, Youth, and Families; and the National Institute for Child Health and Human Development (NICHD) National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Johnston LD, O'Malley PM, Bachman JG, et al. More good news on teen smoking: Rates at or near record lows. University of Michigan News Service; Ann Arbor, MI.: 2008. [February 10, 2009]. Available at: http://www.monitoringthefuture.org. [Google Scholar]
- 2.Burr ML, Anderson HR, Austin JB, et al. Respiratory symptoms and home environments in children: A national survey. Thorax. 1999;54:27–32. doi: 10.1136/thx.54.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Henderson AJ. The effects of tobacco smoke exposure on respiratory health in school-aged children. Paediatr Respir Rev. 2008;9:21–28. doi: 10.1016/j.prrv.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 4.Smoking and the Young. Royal College of Physicians of London; London: 1992. Working Party on Smoking and the Young. [Google Scholar]
- 5.Centers for Disease Control Smoking and Tobacco Use. [March 1, 2009];Fact Sheet: Youth and tobacco use: Current estimates. 2006 Available at http://www.cdc.gov/tobacco/data_statistics/fact_sheets/youth_data/tobacco_use/index.htm.
- 6.Mathers M, Toumbourou RF, Catalano RF, et al. Consequences of youth tobacco use: A review of prospective behavioural studies. Addiction. 2006;101:948–958. doi: 10.1111/j.1360-0443.2006.01438.x. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control Smoking and Tobacco Use. [February 9, 2009];Fact Sheet: Health effects of cigarette smoking. 2008 Available at: http://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/health_effects.htm.
- 8.US Department of Health & Human Services . Healthy People 2010: understanding and improving health. 2nd Ed. US Dept of Health & Human Services; Washington DC: 2000. [February 9, 2009]. Available at: http://www.health.gov/healthypeople. [Google Scholar]
- 9.Schepis TS, Rao U. Epidemiology and etiology of adolescent smoking. Current Opinion in Pediatrics. 2005;17:607–612. doi: 10.1097/01.mop.0000176442.49743.31. [DOI] [PubMed] [Google Scholar]
- 10.Burns DM, Johnson LD. Overview of recent changes in adolescent smoking behavior. [February 10, 2009];Tobacco Control Monographs. 2001 14:1–8. Available at http://cancercontrol.cancer.gov/tcrb/monographs/14/index.html. [Google Scholar]
- 11.Faulkner DL, Merritt RK. Race and cigarette smoking among United States Adolescents: The role of lifestyle behaviors and demographic factors. Pediatrics. 1998;101:E.4. doi: 10.1542/peds.101.2.e4. [DOI] [PubMed] [Google Scholar]
- 12.Roberts ME, Fuemmeler BF, McClernon JF, et al. Association between trauma exposure and smoking in a population-based sample of young adults. J of Adolesc Health. 2008;42:266–274. doi: 10.1016/j.jadohealth.2007.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dalton MA, Beach ML, Adachi-Mejia AM, et al. Early exposure to movie smoking predicts established smoking by older teens and young adults. Pediatrics. 2009;123:e551–e558. doi: 10.1542/peds.2008-2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Botello-Harbaum MT, Haynie DL, Iannotti RJ, et al. Tobacco control policy and adolescent cigarette smoking status in the United States. Nicotine Tob Res. 2009;11:875–885. doi: 10.1093/ntr/ntp081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hamburger ME, Leeb RT, Swahn MH. Childhood maltreatment and early alcohol use among high-risk adolescents. J Stud Alcohol and Drug. 2008;69:291–295. doi: 10.15288/jsad.2008.69.291. [DOI] [PubMed] [Google Scholar]
- 16.Ireland TO, Smith CA, Thornberry TP. Developmental issues in the impact of child maltreatment on delinquency and drug use. Criminology. 2002;40:359–399. [Google Scholar]
- 17.Moran PB, Vuchinich S, Hall NK. Associations between types of maltreatment and substance use during adolescence. Child Abuse Negl. 2004;28:565–574. doi: 10.1016/j.chiabu.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 18.Anda RF, Croft JB, Felitti VJ, et al. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA. 1999;282:1652–1658. doi: 10.1001/jama.282.17.1652. [DOI] [PubMed] [Google Scholar]
- 19.Jun H, Rich-Edwards JW, Boynton-Jarrett R, et al. Child abuse and smoking among young women: The importance of severity, accumulation, and timing. J Adolesc Health. 2008;43:55–63. doi: 10.1016/j.jadohealth.2007.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nichols HB, Harlow BL. Childhood abuse and risk of smoking onset. J Epidemiol Community Health. 2004;58:402–406. doi: 10.1136/jech.2003.008870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hussey JM, Chang JJ, Kotch JB. Child maltreatment in the United States: Prevalence, risk factors, and adolescent health consequences. Pediatric. 2006;118:933–942. doi: 10.1542/peds.2005-2452. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control. Child maltreatment [February 19, 2009];Facts at a Glance. 2008 Available at http://www.cdc.gov/ViolencePrevention/pdf/CM-DataSheet-a.pdf.
- 23.Child Maltreatment . U.S. Government Printing Office. US Department of Health & Human Services, Administration on Children, Youth and Families; Washington, DC: 2006. [February 20, 2009]. 2008 Available at: http://www.acf.hhs.gov/programs/cb/pubs/cm06/index.htm. [Google Scholar]
- 24.Finklehor D, Ormrod H, Turner H, et al. The victimization of children and youth: A comprehensive national survey. Child Maltreat. 2005;10:5–25. doi: 10.1177/1077559504271287. [DOI] [PubMed] [Google Scholar]
- 25.Fletcher JM. Child maltreatment and adolescent and young adult depression. Soc Sci Med. 2008;68:799–806. doi: 10.1016/j.socscimed.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 26.Lansford JE, Dodge KA, Pettit GS, et al. A 12-year prospective study of the long-term effects of early child physical maltreatment on psychological, behavioral, and academic problems in adolescence. Arch Pediatr Adolesc Med. 2002;156:824–30. doi: 10.1001/archpedi.156.8.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Toth SL, Manly JT, Cicchetti D. Child maltreatment and vulnerability to depression. Dev Psychopathol. 1992;4:97–112. [Google Scholar]
- 28.Dierker LC, Vesel F, Sledjeski EM, et al. Testing the dual pathway hypothesis to substance use in adolescence and young adulthood. Drug Alcohol Depend. 2007;87:83–93. doi: 10.1016/j.drugalcdep.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 29.Prinstein MJ, La Greca AM. Childhood depressive symptoms and adolescent cigarette use: A six-year longitudinal study controlling for peer correlates. Health Psychol. 2009;28(3):283–291. doi: 10.1037/a0013949. [DOI] [PubMed] [Google Scholar]
- 30.Kassel JD, Stroud LR, Paronis CA. Smoking, stress, and negative affect: Correlation, causation, and context across stages of smoking. Psychol Bull. 2003;129:270–304. doi: 10.1037/0033-2909.129.2.270. [DOI] [PubMed] [Google Scholar]
- 31.Runyan DK, Curtis PA, Hunter WM, et al. LONGSCAN: A consortium for longitudinal studies of maltreatment and the life course of children. Aggress Violent Behav. 1998;3:275–285. [Google Scholar]
- 32.Knight ED, Smith JS, Martin L, et al. Measures for Assessment of Functioning and Outcomes in Longitudinal Research on Child Abuse Volume 3: Early Adolescence (Ages 12-14) 2008 Available at: http://www.iprc.unc.edu/longscan/pages/measures/Ages12to14/index.html.
- 33.English DJ, the LONGSCAN Investigators Modified Maltreatment Classification System (MMCS) 1997 http://www.iprc.unc.edu/longscan/pages/mmcs/LONGSCAN%20MMCS%20Coding.pdf.
- 34.Hussey JM, Marshall JM, English DJ, et al. Defining maltreatment according to substantiation: distinction without a difference? Child Abuse Negl. 2005;29(5):479–92. doi: 10.1016/j.chiabu.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 35.Kohl PL, Jonson-Reid M, Drake B. Time to leave substantiation behind: findings from a national probability study. Child maltreat. 2009;14:17–26. doi: 10.1177/1077559508326030. [DOI] [PubMed] [Google Scholar]
- 36.Everson MD, Smith JB, Hussey JM, et al. Concordance between adolescent reports of childhood abuse and Child Protective Service determinations in an at-risk sample of young adolescents. Child Maltreat. 2008;13:14–26. doi: 10.1177/1077559507307837. [DOI] [PubMed] [Google Scholar]
- 37.Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 Profile. University of Vermont, Department of Psychiatry; Burlington, VT: 1991. [Google Scholar]
- 38.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychology research. Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 39.Muthén LK Muthén, BO. Mplus User's Guide. Fifth Edition Muthén & Muthén; Los Angeles, CA: 2008. [Google Scholar]
- 40.Crone MR, Reijneveld SA. The association of behavioural and emotional problems with tobacco use in adolescence. Addictive Behavior. 2007;8:1692–1698. doi: 10.1016/j.addbeh.2006.11.006. [DOI] [PubMed] [Google Scholar]