Abstract
Background:
Laparoscopic cholecystectomy (LC) has become the procedure of choice for management of symptomatic gallstone disease. At times, it is difficult and takes longer time or has to be converted to an open procedure. This study is undertaken to determine the predictive factors for difficult LC.
Aim:
The aim was to evaluate a scoring method to predict difficult LC preoperatively.
Materials and Methods:
There were 30 cases operated by a single experienced surgeon. There are total 15 score from history, clinical and sonological findings. Score up to 5 predicted easy, 6–10 difficult and >10 are very difficult.
Results:
Prediction came true in 76.4% for easy and 100% difficult cases; there were no cases with a score above 10. The factors like previous history of hospitalization (P - 0.004), clinically palpable gallbladder (GB) (P - 0.009), impacted GB stone (P - 0.001), pericholecystic collection (P - 0.04), and abdominal scar due to previous abdominal surgery (P - 0.009) were found statistically significant in predicting difficult LC.
Conclusion:
The proposed scoring system is reliable with a sensitivity of 76.47% and specificity of 100%.
KEYWORDS: Difficult, laparoscopic cholecystectomy, prediction, scoring
INTRODUCTION
Laparoscopic cholecystectomy (LC) has become the procedure of choice for management of symptomatic gallstone disease. Approximately, 2–15% of attempted LC has to be converted to an open procedure due to various difficulties faced while performing the procedure.[1] Various clinical and ultrasonological parameters that may help to predict the difficulty level preoperatively were analyzed in the present study. Such prediction done preoperatively may help the patient as well as the surgeon in being better prepared for the intra-operative challenges.
MATERIALS AND METHODS
The proposed study was conducted in the Department of General Surgery, Government Medical College, Amritsar. Thirty consecutive cases were taken and the scores were given based on history, clinical examination and sonological findings, 1-day prior to surgery. The scoring system used was of Randhawa and Pujahari[2] [Table 1]. The scores were added up to get a total score and the patients were divided into categories of risks based on the total score [Table 2].
Table 1.
Scoring system for clinical and ultrasonological parameters
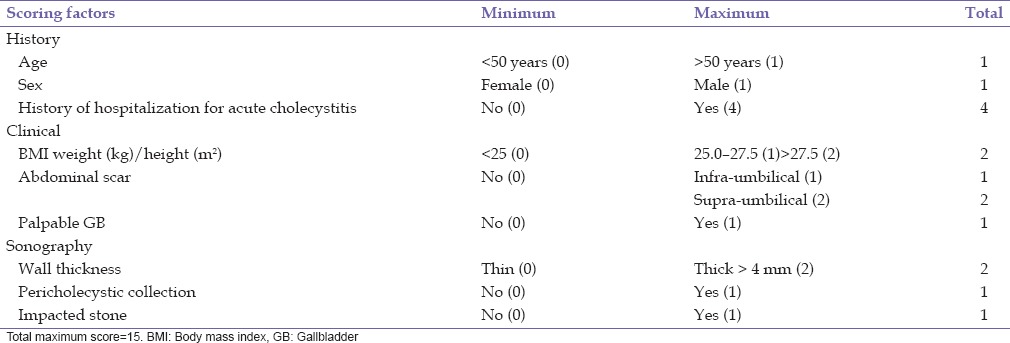
Table 2.
Preoperative risk based on the scoring system

The following operative parameters were recorded for all the patients undergoing LC:
Time taken for surgery
Bile/stone spillage
Injury to cystic duct or cystic artery
Conversion to open cholecystectomy.
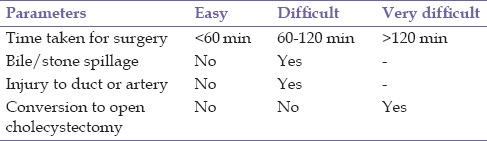
Based on these observations postoperative outcome of LC was grouped into easy, difficult and very difficult and evaluated [Table 3].
Table 3.
Scale for categorization of patients into easy, difficult and very difficult cases postoperatively
All cases were performed by a single surgeon using CO2 pneumoperitoneum with 12 mm Hg pressure and using standard two 5 mm and two 10 mm ports. The timing was noted from the first port site incision till the last ports closure.
The following study was approved by Institutional Ethical Committee with informed consent from participants.
Statistical analysis
All the data were filled in a printed format for further analysis by SPSS 17.0 Inc., IBM statistical system. Descriptive statistics of quantitative data was presented as mean and standard deviation. A univariate regression analysis was used to find the significant risk factors. Those found significant on univariate analysis were analyzed using multivariate linear regression model. Continuous normally distributed data were analyzed using Student's t-test. Proportions were compared by Chi-square test or Fischer exact test. For all comparisons, a probability of 5% was considered as significant.
RESULTS
Of the 30 patients included in the study, 6 patients were male (20%) and 24 were females (80%). The mean age group of the study was 39.47 ± 12.008 years with the minimum age being 18 years and the maximum being 64 years. The majority of patients were in the age group of ≤50 years (25 patients) and only 16.7% (five cases) were >50 years. Seventeen were scored easy (56.7%) and 13 (43.3%) were difficult and nil in very difficult group. There were 6 patients with body mass index (BMI) >27.5 kg/m2. The relation between the prediction of the difficulty level of the cases preoperatively and the actual outcome of the cases is shown in Table 4.
Table 4.
Correlation of preoperative score and the outcome
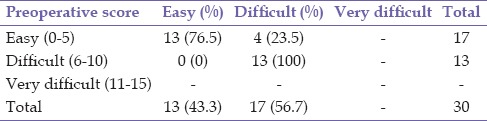
We observed a positive predictive value of 76.4% for our scoring system for cases predicted to be easy. For cases predicted to be difficult we registered a positive predictive value of 100% for the scoring system.
Postoperative outcome was correlated with the various factors included in the scoring system, and data analyzed to assess the significance of each factor [Table 5].
Table 5.
Univariate and multivariate analysis of preoperative outcome with risk factors
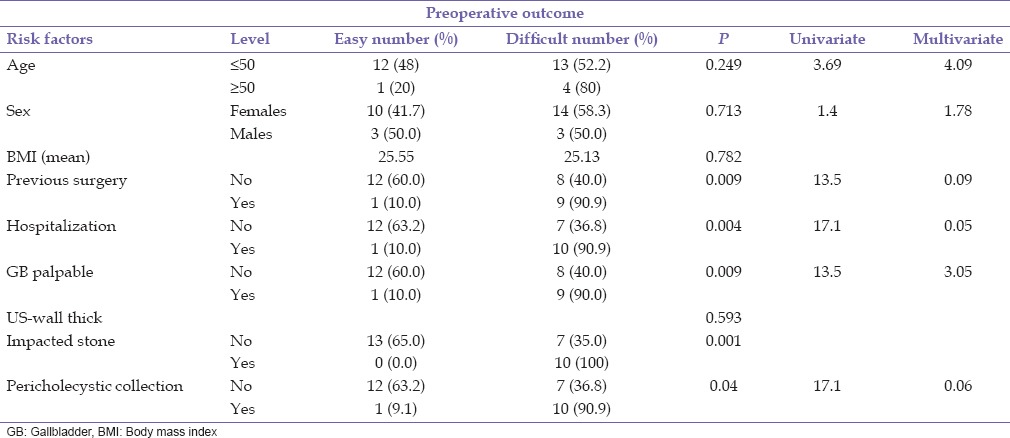
On univariate and multivariate analysis, the factors like previous history of hospitalization, clinically palpable gallbladder (GB), impacted GB stone, pericholecystic collection, and abdominal scar due to previous abdominal surgery were found statistically significant in predicting difficult LC with a receiver operating characteristic (ROC) curve is 0.873 with 95% confidence interval [Graph 1].
Graph 1.
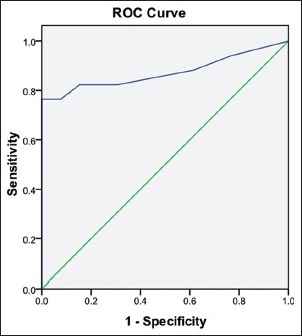
Receiver operating characteristic curve and its area under curve for predicting the operative outcome based on preoperative scores
DISCUSSION
Laparoscopic cholecystectomy is one of the most commonly performed surgeries world over and is undergoing regular amendments with growing technology in order to make it safer, cosmetically acceptable, and cost effective.
Age is a risk factor for difficult GB surgery.[3] In our series, the majority of patients were in the age group of ≤50 years (25 patients) and only 16.7% (five cases) were >50 years. However, in our study we found no significant correlation between age and the difficult level of surgery. This could be because of the small sample size of the study population and also there was an unequal distribution of the patients into different age group with only five cases in >50 years age group with clustering of cases in ≤50 years age group.
In studies done worldwide, male sex has been described to be associated with difficult LC.[4] In the present study, there were 6 males and 24 females. Of 6 males, 2 were predicted to have a difficult surgery. Postsurgery 50.0% males (3 out of 6) turned out to have a difficult procedure. In our study, there was no statistically significant difference in the total time taken for the procedure between the two sexes. Small study group and an unequal distribution of patients on the basis of sex could have altered the results in our series.
Clinically palpable GB was found to be predictor of difficult LC.[2] Palpable GB could be due to a distended GB, mucocele GB, thick-walled, or due to the adhesions between the GB and the omentum. In our study, only 10 patients had clinically palpable GB and out of them 90% (9 out of 10) turned out to have a difficult procedure postsurgery. There are less number of studies supporting clinically palpable GB as a predictor of difficult LC. This is one of the unique features of this study and found strongly significant.
There is a linear correlation between previous history of hospitalization[5] due to acute attacks of cholecystitis and the difficulty level of LC. Each attack of cholecystitis increases the GB wall thickness and the GB becomes scarred and fibrosed. It further increases the adhesions at the Calot's triangle and between GB and fossa. In our study, we found strongly significant correlation between previous history of hospitalization and difficult LC. Such a strong prediction may be possible due to higher scoring given to previous history of hospitalization (score = 4) in our study.
While performing LC, stone impacted at the neck of GB poses some technical problems, because of distension of GB, as is with thick GB wall. It is difficult to grasp the GB neck to allow adequate retraction to perform dissection at the Calot's triangle.[6] It was found to be a statistically significant factor in predicting the difficulty of the procedure in our study. 33.3% patients (10 out of 30) in our series had GB stone impacted at the neck of GB and turned out to be difficult.
Obese patients may have a difficult laparoscopic surgery due to various factors.[7] Port placement in obese patient takes longer time due to the thick abdominal wall. Dissection at the Calot's triangle is also technically difficult due to the obscure anatomy because of excessive intraperitoneal fat and difficulty in the manipulation of instruments through an excessively thick abdominal wall. In our study, we found no correlation between BMI and difficult level of surgery. Surgical expertise of the operating surgeon could be one of the reasons for this discrepancy; as such increased BMI is not a technical problem.
Pericholecystic collection was found to be a predictor of difficult LC.[8] Postoperatively we found 90.9% of these patients (10 out of 11) having difficulty in LC. Hence, we found a strong correlation between pericholecystic collection and difficult LC. Upper abdominal scars (indicators of previous upper abdominal surgeries) may cause the formation of intraperitoneal adhesions that may lead to increased probability of injury and bleeding while placement of umbilical port.[9] It was found to be statistically significant factor in our study.
Increased GB wall thickness is associated with difficult dissection of the GB from its bed.[10] Presence of a thick GB wall may make grasping and manipulation of GB difficult. This makes the dissection at the Calot's triangle and the GB bed to be difficult and limits the extent of anatomical definition. In our study, we found no significant correlation between the GB wall thickness and the difficulty level of surgery. Better randomization of the patients into the two groups and a larger sample size would have allowed us to extrapolate the results into the general population.
Adhesions are the important cause for difficulty encountered in LC and these cannot be assessed on routine ultrasonography (USG) done for cholelithiasis. One more factor is the presence of anatomical variation, making the identification of structures a demanding task.[11] These anatomical variations are usually not diagnosed on routine USG done for cholelithiasis. And finally another important factor that plays a role in the time requirement for the procedure is the surgical expertise of the operating surgeon.[12]
CONCLUSION
Clinically palpable GB, impacted GB stone, pericholecystic collection, previous history of hospitalization due to acute cholecystitis and abdominal scar due to previous abdominal surgery were found statistically significant to predict difficult LC. There was no significant correlation between age and the difficult level of surgery. The preoperative scoring is statistically and clinically a good test for predicting the operative outcome in LC (area under ROC = 0). Sample size is small but the predictors of difficult LC correlated well with previous studies. Further randomized prospective trial with large sample size needed to validate the scoring system.
Footnotes
Source of Support: Nil
Conflicts of Interest: None declared.
REFERENCES
- 1.Alponat A, Kum CK, Koh BC, Rajnakova A, Goh PM. Predictive factors for conversion of laparoscopic cholecystectomy. World J Surg. 1997;21:629–33. doi: 10.1007/pl00012288. [DOI] [PubMed] [Google Scholar]
- 2.Randhawa JS, Pujahari AK. Preoperative prediction of difficult lap chole: A scoring method. Indian J Surg. 2009;71:198–201. doi: 10.1007/s12262-009-0055-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Simopoulos C, Botaitis S, Polychronidis A, Tripsianis G, Karayiannakis AJ. Risk factors for conversion of laparoscopic cholecystectomy to open cholecystectomy. Surg Endosc. 2005;19:905–9. doi: 10.1007/s00464-004-2197-0. [DOI] [PubMed] [Google Scholar]
- 4.O’Leary DP, Myers E, Waldron D, Coffey JC. Beware the contracted gallbladder – Ultrasonic predictors of conversion. Surgeon. 2013;11:187–90. doi: 10.1016/j.surge.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 5.Rattner DW, Ferguson C, Warshaw AL. Factors associated with successful laparoscopic cholecystectomy for acute cholecystitis. Ann Surg. 1993;217:233–6. doi: 10.1097/00000658-199303000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lal P, Agarwal PN, Malik VK, Chakravarti AL. A difficult laparoscopic cholecystectomy that requires conversion to open procedure can be predicted by preoperative ultrasonography. JSLS. 2002;6:59–63. [PMC free article] [PubMed] [Google Scholar]
- 7.Rosen M, Brody F, Ponsky J. Predictive factors for conversion of laparoscopic cholecystectomy. Am J Surg. 2002;184:254–8. doi: 10.1016/s0002-9610(02)00934-0. [DOI] [PubMed] [Google Scholar]
- 8.Dhanke PS, Vgane SP. Factors predicting difficult laparoscopic cholecystectomy: A single-institution experience. Int J Stud Res. 2014;4:3–7. [Google Scholar]
- 9.Botaitis S, Pitiakoudis M, Perente S, Tripsianis G, Polychronidis A, Simopoulos C. Laparoscopic cholecystectomy in acute cholecystitis: An analysis of the risk factors. S Afr J Surg. 2012;50:62. doi: 10.7196/sajs.1284. 64, 68. [DOI] [PubMed] [Google Scholar]
- 10.Fried GM, Barkun JS, Sigman HH, Joseph L, Clas D, Garzon J, et al. Factors determining conversion to laparotomy in patients undergoing laparoscopic cholecystectomy. Am J Surg. 1994;167:35–9. doi: 10.1016/0002-9610(94)90051-5. [DOI] [PubMed] [Google Scholar]
- 11.Meshikhes AW, al-Dhurais S, Bhatia D, al-Khatir N. Laparoscopic cholecystectomy: The Dammam Central Hospital experience. Int Surg. 1995;80:102–4. [PubMed] [Google Scholar]
- 12.Takegami K, Kawaguchi Y, Nakayama H, Kubota Y, Nagawa H. Preoperative grading system for predicting operative conditions in laparoscopic cholecystectomy. Surg Today. 2004;34:331–6. doi: 10.1007/s00595-003-2714-0. [DOI] [PubMed] [Google Scholar]


