Abstract
Since their introduction in clinical practice in the 1950's, Sulfonylureas (SUs) have remained the main-stay of pharmacotherapy in the management of type 2 diabetes. Despite their well-established benefits, their place in therapy is inappropriately being overshadowed by newer therapies. Many of the clinical issues associated with the use of SUs are agent-specific, and do not pertain to the class as such. Modern SUs (glimepiride, gliclazide MR) are backed by a large body of evidence, experience, and most importantly, outcome data, which supports their role in managing patients with diabetes. Person-centred care, i.e., careful choice of SU, appropriate dosage, timing of administration, and adequate patient counseling, will ensure that deserving patients are not deprived of the advantages of this well-established class of anti-diabetic agents. Considering their efficacy, safety, pleiotropic benefits, and low cost of therapy, SUs should be considered as recommended therapy for the treatment of diabetes in South Asia. This initiative by SAFES aims to encourage rational, safe and smart prescription of SUs, and includes appropriate medication counseling.
Keywords: Anti-hyperglycaemic agent, gliclazide, glimepiride, glipizide, safety, sulfonylurea, type 2 diabetes mellitus, vascular complications
EXECUTIVE SUMMARY
Sulfonylureas in the management of type 2 diabetes mellitus in South Asia – A consensus statement
An initiative of South Asian Federation of Endocrine Societies (SAFES)
Since their introduction in clinical practice in 1950's, Sulfonylureas (SUs) have remained the mainstay of pharmacotherapy in the management of type 2 diabetes mellitus (T2DM). Despite their well-established efficacy, safety and proven benefits, their clinical utility and place in therapy are inappropriately being overshadowed by newer therapies. Many of the clinical issues associated with the use of SUs are agent-specific and do not pertain to the class as such. A careful choice of SU, appropriate dosage, timing of administration, and adequate patient counseling, that is, person-centered care, will ensure that deserving patients are not deprived of the advantages of this well-established class of anti-diabetic agents. In addition, the modern SUs are backed by a large body of evidence experience and most importantly outcome data, which supports their role in managing patients with diabetes. Considering their efficacy, safety, pleiotropic benefits, and low cost of therapy, SUs should be considered as drugs/agents of choice for the treatment of diabetes in South Asia. This initiative by SAFES aims to encourage the rational, safe, and smart prescription of SUs and includes appropriate medication counseling by diabetes care professionals in South Asia.
A. Indications of Sulfonylureas
A1. SUs are an effective, safe, well tolerated, affordable, and convenient therapeutic option in the management of T2DM (Grade A; EL 1).
A2. SUs are effective second-line agents after metformin, in the management of T2DM. SU monotherapy as first-line may be considered in type 2 diabetes with metformin intolerance/contraindication and in patients with MODY (Grade A; EL 2).
A3. Modern SUs (Glimepiride and Gliclazide MR) should be initiated early in the course of T2DM, to achieve maximum glycemic benefits and obtain the benefits of metabolic memory (Grade A; EL 1).
A4. SU-containing dual or triple fixed dose combinations, if available, (with drugs that have complementary modes of action) reduce cost, offer convenience, and improve patient adherence (Grade B; EL 1).
B. Preferred Sulfonylureas
B1. Modern SUs (Glimepiride and Gliclazide MR) should be preferred over conventional SUs in view of the reduced mortality (all-cause and CV mortality), better CV outcomes (composite of acute myocardial infarction, stroke, and CV mortality), and renal protection (Grade A; EL 1).
B2. Modern SUs (Glimepiride and Gliclazide MR) should be preferred over conventional SUs in T2DM patients at increased risk of hypoglycemia (Grade A; EL 1).
B3. Modern SUs (Glimepiride and Gliclazide MR) should be the preferred choice of SU in overweight/obese T2DM patients (Grade A; EL 1).
B4. Modern SUs (Glimepiride and Gliclazide MR) should be preferred over conventional SUs in patients at increased risk of cardiovascular disease (CVD) or with CVD (Grade A; EL 2).
C. Sulfonylureas in co-morbid conditions
C1. Shorter acting drugs, especially those metabolized in the liver (glipizide), should be the preferred SU in patients with moderate/severe renal impairment. In mild/moderate renal impairment, gliclazide and glimepiride may also be used, preferably at lower doses (Grade A; EL 3).
C2. Reduction of dose and longer intervals between dose adjustments for SUs are recommended in patients with mild/moderate hepatic impairment (Grade B; EL 4).
C3. SUs with a lower risk of hypoglycemia such as gliclazide MR and glimepiride are recommended in elderly patients. Alternately, short-acting SUs, or SUs in low dose can be used (Grade B; EL 4).
C4. SUs are not indicated for use in children and adolescents, and should be avoided during pregnancy and lactation (Glibenclamide may be prescribed in pregnancy and lactation, if the person absolutely refuses to accept insulin, and if metformin is not tolerated/contraindicated) (Grade A; EL 1).
D. Sulfonylureas in Ramadan/Religious fasting
D1. SUs may be used during Ramadan, with appropriate counseling and dose modification. Modern SUs (Glimepiride and Gliclazide MR) are preferred as they confer a lower risk of hypoglycemia (Grade A; EL 3).
D2. Individuals on once daily SU should take their medications at Iftar (During Ramadan, Suhur is the meal taken before sunrise and Iftar is the one taken when the fast is broken after sunset). The dose may remain unchanged or reduced depending upon their pre-Ramadan glycemic status (Grade A; EL 4).
D3. Individuals on twice daily SUs, with higher doses in the morning and a smaller dose in the evening, may shift the higher morning dose to Iftar and the smaller evening dose, or its half, to Suhur (During Ramadan, Suhur is the meal taken before sunrise and Iftar is the one taken when the fast is broken after sunset). The Suhur dose may be reduced further if the control is adequate (Grade A; EL 4).
D4. Individuals with good control on conventional SUs do not require major changes in drug regimen, except for dose titration (Grade A; EL 4).
E. Practical tips for using Sulfonylureas
E1. Practice a “start low, step-up slow” approach, up-titrating gradually (Grade A; EL 4).
E2. SU titration should be based on glucose monitoring: (Grade A; EL 4).
Once in two weeks – for responders with no hypoglycemia
Once a week – for nonresponders with or without hypoglycemia.
E3. The timing of administration of SUs before the first and subsequent major meals of the day is important. The importance of adherence must be explained (Grade A; EL 4).
E4. Patients/family members should be educated on the need to carry diabetes identity cards, sick day management, and recognition and management of hypoglycemia, including de-escalation of SU doses, if required (Grade A; EL 4).
INTRODUCTION
The type 2 diabetes mellitus (T2DM) pandemic[1] is characterized by increasing complexity of management, raising concerns over safety and cost of therapy. Data from the National Disease and Therapeutic Index (NDTI) indicate that in USA, the number of diabetes medications per treated patient increased from 1.14 (95% CI, 1.06–1.22) in 1994 to 1.63 (1.54–1.72) in 2007, and the aggregate drug expenditure doubled from $6.7 billion in 2001 to $12.5 billion in 2007.[2] In India, the average number of antidiabetic drugs per prescription is 1.4, and the mean cost per 1 month prescription is INR 354.60 ± 305.72.[3,4] Globally, prescription patterns have changed in recent years with the introduction of newer classes of medications.[5,6,7] While, sulfonylureas (SUs) and human insulins were the mainstay of diabetes pharmacotherapy before 1995,[6] several new therapeutics are now available. Oral hypoglycaemic agents (OHAs) still dominate the prescribing pattern (57.0%) followed by insulin alone (14.0%) and insulin + OHAs (13.0%) in USA.[8] Similar trends are observed in South Asia, where majority of the population is treated with OHAs, either as monotherapy or in combination.[3,4,9] Uncertainty exists regarding the most commonly prescribed OHAs, with some studies reporting it to be SUs[9,10] and others, metformin.[4] Evidence from literature suggests that SUs account for up to 20% of newly initiated OHAs, either as monotherapy or in combination, for treatment of T2DM.[11]
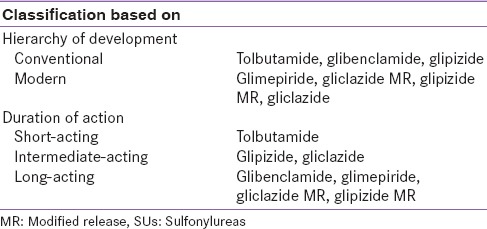
In order to avoid confusion with numerical generations of SUs, an attempt was made to classify them as conventional and modern SUs based on hierarchy of development. Another classification, based on duration of action (short, intermediate and long-acting) helped to define use in patients with specific clinical scenarios [Table 1]. The classifications in Table 1 will be used throughout the article to provide a clear picture of their place in diabetes management.
Table 1.
Classification of SUs
SITUATIONAL ASSESSMENT OF SULFONYLUREAS USED IN SOUTH ASIA
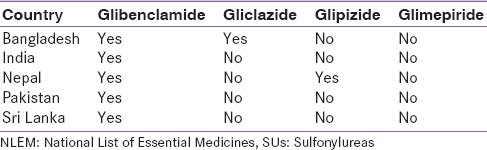
Both conventional and modern SUs remain the choice of OHA prescription in South Asia. Conventional SUs are listed alongside metformin, in the National List of Essential Medicines (NLEM) of these nations [Table 2]. According to NLEMs, glibenclamide (2.5 and 5.0 mg) is an essential SU in all the five countries (India, Pakistan, Nepal, Sri Lanka and Bangladesh).[12,13,14,15,16] Surprisingly none of the countries in the South Asian region have included glimepiride as an option for diabetes treatment in their NLEMs.[17] Bangladesh and Nepal are the only countries to have included newer generation SUs (gliclazide [80.0 mg] and glipizide [2.5, 5.0 mg], respectively), in their NLEMs. During 2014, general practitioners (GPs) from Pakistan had prescribed SUs more often than any other OHAs (including DPP-4 inhibitors).[18] Similarly in Sri Lanka, glibenclamide is the most commonly prescribed SU by GPs, while gliclazide prescription dominates the public sector. Interestingly, tolbutamide, one of the oldest SU, is still being prescribed in public hospitals of Sri Lanka as it is cheaper compared to other OHAs.[18] During 2014, SUs (as combination therapy) constituted the majority of OHAs market in India, with glimepiride combinations posting a growth higher than the market volume in drug class.[19] Recent studies from India and Pakistan report that SU/metformin are more efficacious than DPP-4inhibitors/metformin combinations.[20,21]
Table 2.
SUs listed under the NLEM for South Asian countries
SULFONYLUREAS IN DIABETES MANAGEMENT
An ideal anti-diabetic should confer glycaemic control, with lower risk of side effects, while providing inexpensive ease of use.[22] SUs are well-established glucose-lowering drugs, with insulinotropic action on pancreatic β-cells. Since the introduction of tolbutamide in 1956,[23] newer SUs have been developed, broadly classified based on their affinity to bind with sulfonylurea receptor (SUR) proteins.[24] The availability of modern SUs (glimepiride, glipizide, gliclazide MR and gliclazide modified release [MR]) with fewer side-effects and better efficacy[25] have contributed to their popularity.[26,27,28,29] Although the mechanism of action of SUs is well understood, their safety has been a matter of debate. Recent reviews and retrospective analyses suggest that SUs may cause hypoglycaemia and weight gain.[30,31] In addition, certain SUs are believed to accelerate β-cell apoptosis,[32] increase the risk of ischemic complications, and contribute to non-fatal cardiovascular (CV) outcomes and all-cause mortality.[33] The present consensus attempts to address their safety issues.
Systematic review of literature was conducted to provide the best possible evidence base for the use of SUs in the management of T2DM. Existing guidelines, meta-analyses, key morbidity-mortality trials, systematic reviews and most cited articles were reviewed, and recommendations relevant to South Asian scenario were framed. Where inadequate evidence was available, the panel relied on experience, judgment and consensus to make their recommendations. The current consensus is developed in accordance with the American Association of Clinical Endocrinologists/American College of Endocrinology (AACE/ACE) protocol for standardized production of clinical practice guidelines.[34] Recommendations were graded based on clinical importance and levels of evidence as described in Tables 3 and 4, respectively. The recommendations incorporate the objectivity of evidence-based medicine with the subjectivity of a complex clinical challenge. As individual patient circumstances and environments differ, management should be based on the best interest of the individual patient, in a manner appropriate for the local scenario, involving shared decision making by patient and clinician.
Table 3.
Evidence rating according to AACE protocol 2010
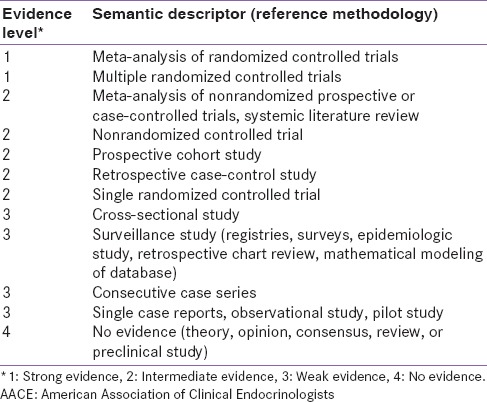
Table 4.
Recommendation grading according to the AACE protocol 2010
MECHANISM OF ACTION
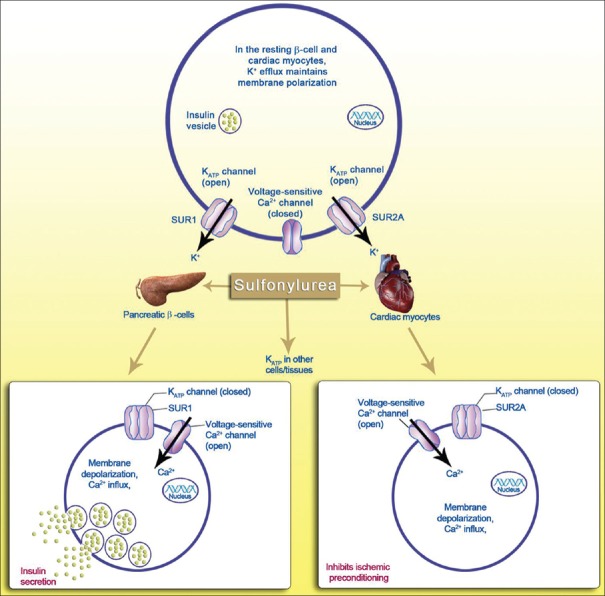
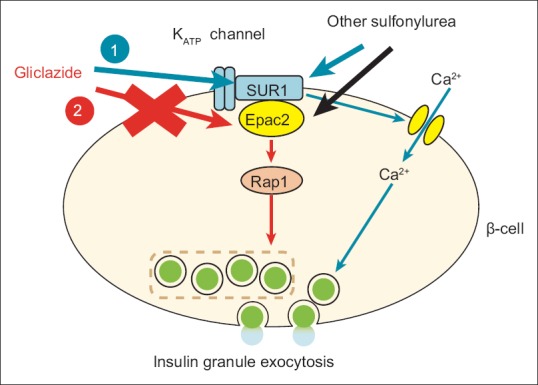
SUs are insulin secretagogues that stimulate endogenous insulin secretion by blocking adenosine triphosphate-sensitive potassium channels (KATP) on pancreatic β-cells, by binding to the SUR subunit present on the β-cell plasma membrane.[35] SUs bind to a common SUR unit on β-cells causing closure of the KATP channels and inhibition of K+ efflux, consequently depolarising the membrane and facilitating influx of Ca+2 ions. This in turn stimulates the exocytosis of insulin secretory vesicles [Figure 1].[35] Because insulin secretion is non-glucose-mediated, conventional SUs have been associated with a higher risk of hypoglycaemia.[36,37]
Figure 1.
Mechanism of action of sulfonylureas on pancreatic β-cells and cardiomyocytes (SUR: Sulfonylurea receptor; Adapted and modified from source: Gore MO, McGuire DK. Resolving drug effects from class effects among drugs for type 2 diabetes mellitus: More support for cardiovascular outcomes assessment. Euro Heart J 2011;32(15):1832-4)
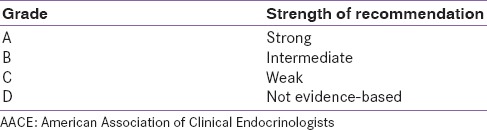
ALL SULFONYLUREAS ARE NOT THE SAME
SUs stimulate insulin secretion by blocking KATP channels in the pancreatic β-cell membrane, by binding to the SUR subunit of the channel.[38] KATP channels are also present in extrapancreatic tissues, but often contain different types of SUR subunit [Table 5]. Evidence suggests that the effect of SUs on these KATP channels in different tissues varies.[39] For instance, gliclazide and tolbutamide block SUR1 with higher affinity compared to SUR2 while glibenclamide and glimepiride block both receptors with similar affinity.[39,40] Reversibility also varies, with tolbutamide and gliclazide producing a reversible inhibition of Kir6.2/SUR1 and Kir6.2/SUR2 channels, whereas glibenclamide has a reversible effect on cardiac, but not β-cell, KATP channels.[40] Notably, SUs that inhibit SUR1 reversibly (tolbutamide and gliclazide) are smaller and possess fewer hydrophobic groups than SUs that are slowly reversible (glibenclamide and glimepiride).[38] These variations may be explained by considering the hetero-octameric complex of SUR1 KATP channels that contains two high-affinity binding sites, one for sulfonyl moiety and other for benzamido moiety.[41] The selectivity of SUR1 for the sulfonyl moiety is 100 to 1000 fold higher than SUR2.[42] While most SUs possess both sulfonyl and benzamido moieties [Figure 2] and interact with SUR1 and SUR2, short-chain molecules (gliclazide), with no benzamido moiety, bind only to the sulfonyl site. This in part explains the pancreas-selectivity of short chain SUs like gliclazide.[43]
Table 5.
SUR type present in different extrapancreatic tissues
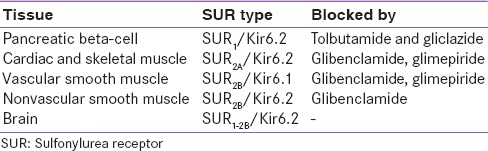
Figure 2.
Molecular structure of sulfonylureas
Glimepiride stimulates insulin secretion by binding to a specific 65-kDa protein site on the KATP channel of pancreatic β-cell and exerts allosteric inhibition of the SUR complex.[36,44] Further, compared to glibenclamide, glimepiride exhibits lower binding affinity (2- to 3-fold) for SUR as well as higher rate of association (2.5- to 3-fold) and dissociation (8- to 9-fold) from the receptor.[36,45] The distinct binding site and receptor interactions of glimepiride are believed to result in lower inhibition of KATP channel and hence, there is reduced risk of hypoglycaemia as compared to conventional SUs.[37,46] Moreover the ability of glimepiride to augment first and second phase insulin secretion in T2DM patients, indicate a possible relationship between good glycaemic control and acute improvement of regularity of the in vivo insulin release process.[47] Gliclazide is the only SU reported not bind to Epac2, a stimulating factor for insulin exocytosis. Consequently, gliclazide confers lower risk of hypoglycaemia [Figure 3].[30]
Figure 3.
Mechanism of action of gliclazide on pancreatic β-cells (SUR: Sulfonylurea receptor)
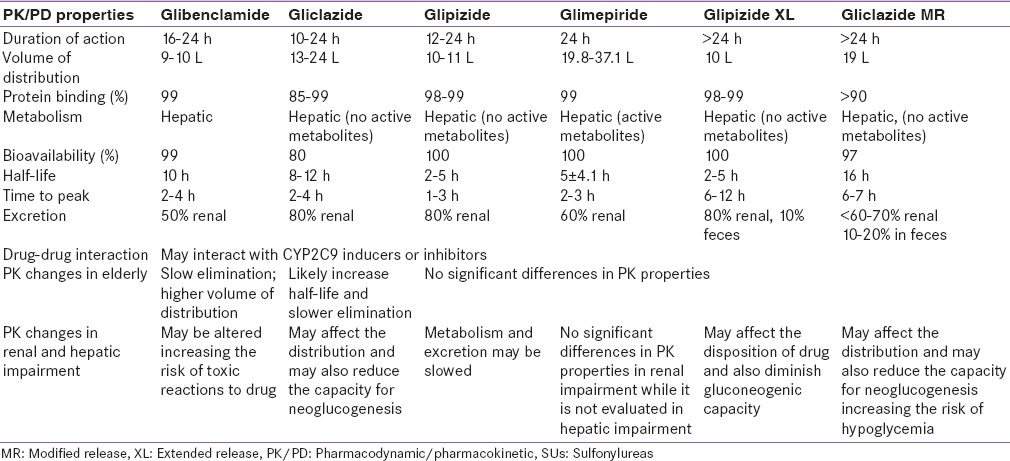
Variations in the pharmacodynamic/pharmacokinetic (PK/PD) profiles [Table 6] of individual SUs also explain the differences in anti-diabetic activity, hypoglycaemic risk, specificities to different tissue-specific SURs, effects on myocardial ischemic preconditioning, and insulin secretory effects.[48] In light of this, it may be wise to choose modern SUs that pose lower risk of hypoglycaemia and are cardiac friendly. However, lack of comparable data from clinical trials requires careful assessment of SUs with respect to patient-relevant endpoints.[49]
Table 6.
PK/PD profile of frequently prescribed SUs
GLYCEMIC EFFICACY
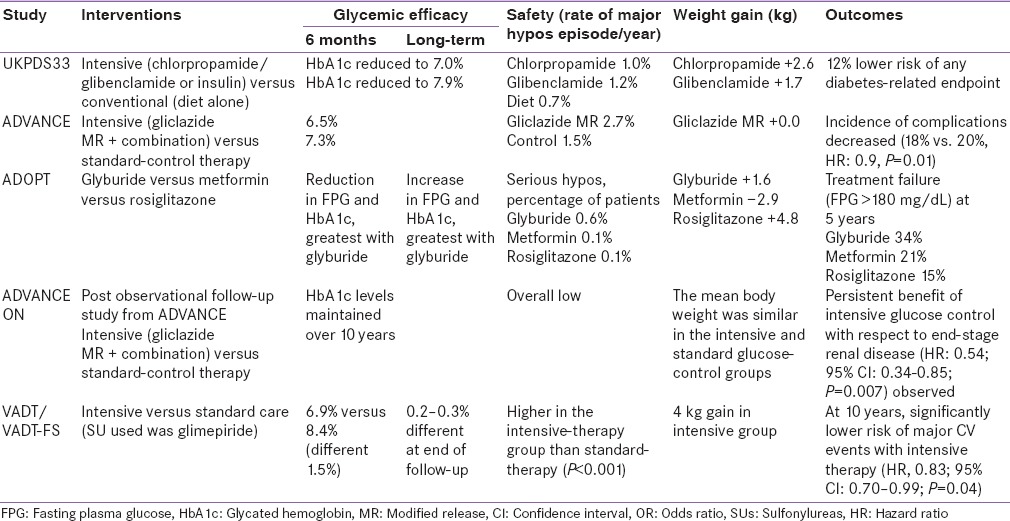
SUs have a robust evidence base for glycaemia lowering, both as monotherapy and in combination with other OHAs. In a recent systemic review and meta-analysis, SU monotherapy was found to lower glycated haemoglobin (HbA1c) by 1.51% more than placebo (95% CI, 1.25, 1.78).[25] Overall, in placebo comparator studies, treatment with SUs was found to reduce the fasting plasma glucose by 20–40 mg/dL and HbA1c by 1.0%–2.0%.[50,51] Several landmark trials including UKPDS, ADVANCE, ADOPT and VADT-FS showed that intensive glycaemic control with SU-based therapy (chlorpropamide, glibenclamide, glipizide in UKPDS; gliclazide MR in ADVANCE glibenclamide in ADOPT and glimepiride in VADT-FS) was associated with HbA1c reduction and improved long-term outcomes.[26,52,53,62] A meta-analysis of randomised clinical trials (RCTs) comparing the efficacy of metformin and glimepiride monotherapy, reported that glimepiride was as effective as metformin in achieving glycaemic control.[54]
In combination therapy with metformin,[55] rosiglitazone,[56] insulins[57] or DPP-4 inhibitor,[58] SUs provided better glycaemic control with relatively favourable safety profiles. A systemic review reported HbA1c reduction of 1.62% (95% CI: 1.0, 2.24) with SU + OHAs, and 0.46% (95% CI: 0.24, 0.69) with SU + insulin (with lowered insulin dose).[25] The DiaRegis registry that examined the impact of different treatment intensification options in T2DM patients following metformin failure, suggested that adding SU to metformin provides greater reductions in HbA1c than incretin therapy (–0.6% vs. –0.5%, P = 0.039) with no difference in the hypoglycaemic event rates.[59]
Efficacy in lowering micro-vascular and microvascular complications
Metformin, SUs and acarbose are the only OHAs with long term outcome data. An improved long-term outcome with SU based intensive therapy was evident from UKPDS and ADVANCE.[26,52] A 10 year follow-up of UKPDS suggested that intensive control with either insulin or SU was associated with relative reductions in risk for any diabetes-related end point (9%, P = 0.04) and microvascular disease (24%, P = 0.001), and risk reductions for myocardial infarction (15%, P = 0.01) and death from any cause (13%, P = 0.007).[60] In ADVANCE, a strategy of intensive glucose control (≤HbA1c 6.5%) with gliclazide MR yielded significant reductions in combined major macrovascular and microvascular events (18.1%, vs. 20.0% with standard control; hazard ratio, 0.90; 95% CI, 0.82 to 0.98; P = 0.01), as well as that of major microvascular events (9.4% vs. 10.9%; hazard ratio, 0.86; 95% CI, 0.77 to 0.97; P = 0.01) with no unfavourable cardiovascular outcomes.[52] In addition, a reduction of 10% in risk of serious diabetes complications, 21% in kidney disease, and 30% in macroalbuminuria development was observed in patients treated with intensive regimen.[52] Similar trends were observed in the ADVANCE ON Study where intensive target-driven, multifactorial approach with SU therapy, reduced the risk of microvascular complications (specifically end stage renal disease).[61] VADT-FS is the long term follow-up of the VADT (high risk diabetic patients treated with a multi-drug regimen using metformin, glimepiride, rosiglitazone and insulin; standard care vs intensive treatment). The 10 year results demonstrate that, compared to standard care, an intensive treatment results in a significant 17% relative reduction in major cardiovascular events, with no difference in mortality. This data provides evidence that a current multidrug glycemic treatment regimen (which includes glimepiride) can be associated with a significant reduction in major macrovascular events even among older patients who have had diabetes for many years.[62] The major outcomes of treatment with SUs in landmark trials have been presented in Table 7.
Table 7.
Outcomes of treatment with SUs in landmark trials
Adverse effects
Adverse effects, other than hypoglycaemia and weight gain, with the use of SUs include symptomatic hyponatremia, alcohol-induced flushing or disulfiram-like effect, cholestatic jaundice, macular erythema, rash and, blood dyscrasias.[63,64] Conventional SUs may be associated with dizziness and headache,[65] hyponatremia, anaemia, leukopenia, and thrombocytopenia.[66]
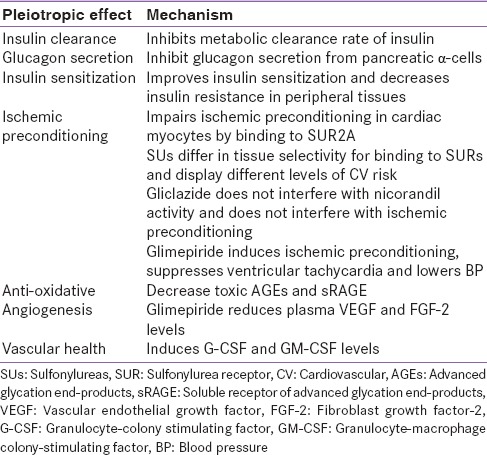
EXTRA-PANCREATIC EFFECTS
SUs (particularly glipizide) are known to reduce the hepatic uptake and metabolic clearance rate of insulin.[67] This effect is complemented by a decreased glucagon secretion from pancreatic α-cells.[68] In addition, modern SUs act as insulin-sensitizers, by increasing the expression of GLUT-4 (Glucose Transporter type-4) transporters and decreasing the insulin resistance in peripheral tissues.[69] Adding glimepiride to insulin therapy in patients with T2DM leads to a significant increase in high molecular weight adiponectin (P < 0.01), which in turn is inversely correlated to changes in HbA1c, contributing to improved glycaemic control, and lower insulin requirement.[70]
The cardiovascular effects of SUs are mediated through the inhibition of sarcolemmal and mitochondrial KATP channels on cardiac myocytes, and KATP channels on vascular smooth muscle cell.[71] This inhibition may lead to impairment of ischaemic pre-conditioning (IPC), a cardio-protective phenomenon. Glimepiride, however, was found not to impair IPC[72] while demonstrating anti-inflammatory and angiogenic activity in patients with T2DM.[73] Further, the ability of glimepiride to decrease toxic advanced glycation end products (AGEs) and soluble receptor for AGE (sRAGE), and increase colony-stimulating factors, suggests an anti-oxidative, pro-vascular effect.[73] Gliclazide exerts its extra-pancreatic effects by potentiating insulin mediated glucose uptake in muscles (+35%) to increase insulin sensitivity. These effects are consistent with a post-transcriptional action of gliclazide on GLUT-4 transporters. Gliclazide has also been shown to decrease hepatic glucose production, improving fasting glycaemia. Gliclazide exerts haemo-vascular and anti-oxidant effects, decreasing micro-thrombosis by partial inhibition of platelet aggregation/adhesion, increasing vascular endothelium fibrinolytic activity, and reducing plasma lipid peroxide and increases erythrocyte superoxide dismutase.[74] Glibenclamide is associated with worsening of blood pressure, due to insulin resistance and activation of the sympathetic system.[75] Table 8 summarizes these pleotropic effects and their mechanisms.
Table 8.
Pleotropic effects of different SUs
PLACE OF SULFONYLUREAS IN DIABETES MANAGEMENT RECOMMENDATIONS
SUs are the oldest class of OHAs recommended by current guidelines for treatment of T2DM.[76,77,78,79,80] The American Diabetes Association/European Association for the Study of Diabetes (ADA/EASD) position statement recommends use of SU as first line if metformin intolerant, as second-line after metformin, or as third-line when glycaemic goals are not achieved.[51] The Scottish Intercollegiate Guidelines Network (SIGN), the International Diabetes Federation (IDF) and National Institute for Health and Clinical Excellence (NICE) guidelines also recommend SUs as first- or second-line agents in patients who are not overweight, with intolerance or contraindications to metformin, and those requiring a rapid response due to hyperglycaemic symptoms.[76,79,80]
In addition, national guidelines from South Africa, China, Japan and Korea recommend the use of SUs as first- or second-line agents for the management of T2DM.[81,82,83,84] According to Japan Diabetes Society, SUs are to be considered early in the course of diabetes where patients present with considerable β-cell number and function.[82] The Indian Council of Medical Research (ICMR) guidelines for management of T2DM advocates the use of SU, either alone, or in combination with metformin,[85] and suggests not combining an SU with other SUs or meglitinide, as both have similar mechanism of action.
ISSUES WITH SULFONYLUREA TREATMENT
Although SUs have been the mainstay of pharmacologic management of T2DM, concern has been raised over their potential role in β-cell failure, blunting of IPC, weight gain, hypoglycaemia, and mortality risk. This section will focus on the concerns related to SUs usage. A thorough search of the literature pertaining to each of these issues was performed to frame evidence based recommendations.
β-cell apoptosis
As SUs act by stimulating insulin release from β-cells, there is concern regarding SU induced “β-cell exhaustion”. In UKPDS and ADOPT, majority of patients treated with glibenclamide experienced a loss of effective antidiabetic response after an initial excellent response (secondary failure).[26,30,53] In contrast, data from a systemic review of three RCTs reported lowest rates of secondary failure with gliclazide (7.0%) compared with glibenclamide (17.9%: P < 0.1) and glipizide (25.6%: P < 0.005) respectively.[86] In ADVANCE, compared to standard treatment group, greater proportion of patients in the intensive treatment group (gliclazide based regimen) achieved HbA1c <7.0% with reduced incidence of combined major macro- and microvascular events (HR, 0.90; 95% CI, 0.82 to 0.98; P = 0.01).[52] Gliclazide is therefore less likely to induce β-cell failure or secondary SU failure as compared to conventional SUs.[87]
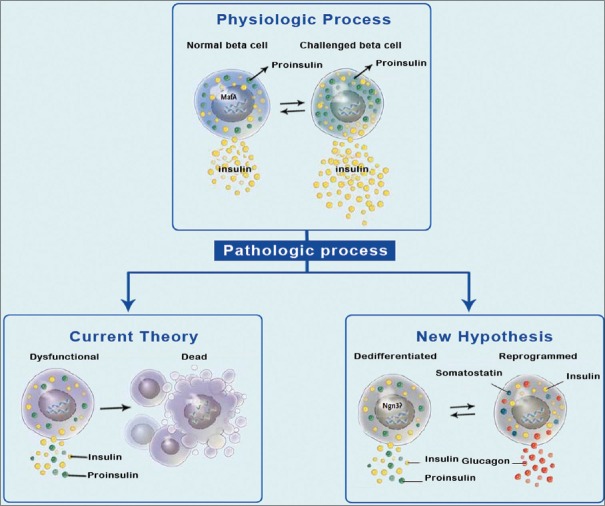
β-cell de-differentiation
Evidence suggests that β-cell de-differentiation, rather than cell death, is responsible for β-cell failure in T2DM.[88] According to Talchai et al., stressed β-cells undergo de-differentiation, where the expression of β-cell specific genes and enzymes that process pro-insulin to insulin is reduced [Figure 4]. De-differentiated β-cells reverted to progenitor-like cells expressing neurogenin3, Oct4, Nanog, and L-Myc, consequently expressing non β-cell hormones such as somatostatin and glucagon.[89,90] Thus β-cell de-differentiation may account for reduced β-cell mass and insulin secretion in patients with T2DM.
Figure 4.
De-differentiation of β-cell under stress
In addition, results of a 10 year observational study that investigated the effect of SUs on β-cell function (assessed by postprandial C-peptide) suggested that it was not long-term treatment with SUs (P = 0.894), but poor glycaemic control was associated with a decrease in β-cell function (P < 0.001).[91] Further, a study that evaluated the effects of exenatide, sitagliptin, and glimepiride on β-cell secretory capacity in early T2DM, indicated that it was glimepiride but not exenatide or sitagliptin, that enhanced β-cell secretory capacity (functional β-cell mass).[92] Current literature does not support the notion that SUs are harmful to β-cell mass or function; on the contrary, SUs appear to improve β-cell secretory capacity when used early in the course of T2DM.
Weight gain
SUs are linked to significant weight gain, a secondary effect also known to occur with insulin, thiazolidinediones, and glinides. The weight gain observed with SUs may be explained by their insulinotropic actions,[93,94] reduction of glycosuria and increased caloric intake to prevent/treat hypoglycaemia.[31] In UKPDS, patients on SU monotherapy gained more weight compared to dietary intervention (chlorpropamide: +2.6 kg, glibenclamide: +1.7 kg).[95] SU-induced weight gain stabilized after first 3 or 4 years while insulin treatment resulted in a progressive gain.[96] However, where SUs were used in combination with insulin, weight gain was minimal compared to insulin monotherapy (1.9 vs. 5.9 kg).[97] Glimepiride,[98] extended release (ER) glipizide[99] and gliclazide MR,[100] have reported weight neutrality at least for the first year. Once daily administration of glimepiride was associated with weight neutralizing/reducing effect over a period of 1.5 years.[101] Initial treatment of T2DM with glimepiride was associated with a significantly greater decrease in body weight/body mass index than with glibenclamide, (-2.04 ± 3.99 kg vs. -0.58 ± 3.65 kg, P < 0.001; -0.71 ± 1.38 kg/m2 vs. -0.20 ± 1.28 kg/m2, P < 0.001, respectively) while providing equivalent glycaemic control.[102] Five years follow-up of ADVANCE trial showed no weight gain in T2DM patients whose treatment included gliclazide MR.[61] Furthermore, in a recent double blind trial, gliclazide MR provided a weight reduction benefit similar to that of vildagliptin (-1.1 kg, in both groups).[103]
Hypoglycemia
Hypoglycaemia is the foremost clinical concern when intensifying anti-diabetic treatment. Individual SUs differ in their hypoglycaemic potential, mainly due to the duration and time of action, dose equivalence and affinity to SUR on β-cells.[48] SU-induced hypoglycaemia with or without the need of external assistance occurs in about 1 in every 100 persons per year.[104] In 10-year follow-up analysis of UKPDS, the annual incidence of at least one hypoglycaemic event was found to be less than half with SUs (17.7%) than those occurring with insulin (36.5%).[26,105] A recent review and meta-analysis showed that gliclazide-treated patients experienced lower rates of severe hypoglycaemia.[106] Glibenclamide has been reported to cause more hypoglycaemic episodes than glimepiride (150 vs. 105 episodes).[107] The GUIDE study demonstrated significantly lower rates of confirmed hypoglycaemia (BG <3 mmol/L) with gliclazide MR as compared to glimepiride (3.7% vs. 8.9%, P = 0.003). However, there were no episodes of severe hypoglycaemia/hypoglycaemia requiring external assistance in either arm.[100] A prospective, population-based, 4-year study reported that glimepiride was associated with fewer episodes of severe hypoglycaemia than glibenclamide in routine clinical use (0.86/1000 person-years vs. 5.6/1000 person-years, respectively).[46]
Cardiovascular safety
Concerns about the CV safety of SUs were raised initially in 1970s when the University Group Diabetes Program (UGDP) study found an increased association between tolbutamide use and risks of coronary artery events.[108] However, the UGDP suffers numerous flaws in the design, execution, analysis and interpretation of findings.[109,110] Further, the applicability of outcomes of the trial to our current multifactorial approach to reduce CV events is uncertain.[111] In fact, the UGDP findings prompted initiation of UKPDS, which found no detrimental effect of SUs on macrovascular complications or mortality in patients with T2DM.[26] This benefit persisted for up to 10 years in patients who had attained better glycaemic control.[60] Similar results were observed from 15 well designed long term (≥72-weeks) RCTs, including ADOPT, ADVANCE[52] and ADVANCE-ON,[61] where treatment with SUs was not found to be associated with an increase in CVD risk or mortality.[112]
Modern SUs (gliclazide MR and glimepiride) are associated with a lower risk of all-cause and CV-related mortality compared to conventional SUs in T2DM patients.[113,114,115] A recent case control study showed that the hazard of developing coronary artery disease (CAD) increased by 2.4-fold (P = 0.004) with glibenclamide; 2-fold (P = 0.099) with glipizide, while it decreased by 0.3-fold (P = 0.385) with glimepiride, and 0.4-fold (P = 0.192) with gliclazide.[116] A large cohort study (N = 11,141) demonstrated a trend towards an increased overall mortality risk with glibenclamide (hazard ratio [HR] 1.36 [95% CI 0.96–1.91]) or glipizide (1.39 [0.99–1.96]) vs. glimepiride.[71] Gliclazide MR, evaluated in a long duration trial (4.3 years follow-up), in diabetic patients co-treated with perindopril-indapamide combination, was associated with 15% reduction in major macro- and micro-vascular events (P = 0.002), 28% reduction in risk of all renal events (P = 0.0001) and 18% reduction in all-cause death (P = 0.04).[117]
ISCHEMIC PRECONDITIONING
Mocanu et al., using a murine model, demonstrated that glibenclamide inhibited mitochondrial KATP channels, impaired IPC and increased experimental infarct size, whereas glimepiride did not inhibit beneficial effects of mitochondrial KATP channel opening and showed no adverse effect on IPC or infarct size.[72] Moreover glimepiride was found to maintain myocardial preconditioning with fewer CV side effects as compared to glibenclamide (P = 0.01 vs. P = 0.34, respectively).[118] Similar results were observed in a recent nation-wide registry, where the risk of acute MI was significantly lower with modern SUs (gliclazide MR, glimepiride) compared to glibenclamide (2.7% vs. 7.5%; P = 0.019).[119] This finding further seems to confirm the beneficial effects of modern SUs in maintaining myocardial IPC. Although both glibenclamide and glimepiride have affinity for the SUR2 receptor, glimepiride appears to preserve myocardial preconditioning, a property not shared by glibenclamide.[27,72] Glimepiride was also reported to have a more rapid as well as longer duration of action; despite less stimulation of insulin secretion in comparison with glibenclamide.[120,121] Therefore, the effect of SUs on cardiac events depends on the molecule being used and the individual clinical setting of the individual case.[122]
All-cause mortality
Varying risk of non-fatal CV outcomes and all-cause mortality have been reported by recent retrospective SU studies,[123,124,125] indicating the lack of class effect. For instance, a meta-analysis evaluating all-cause mortality risk among SUs, reported the relative risk of death of each SU versus glibenclamide to be: 0.65 (95% credible interval: 0.53–0.79) for gliclazide, 0.83 (0.68–1.00) for glimepiride, 0.98 (0.80–1.19) for glipizide, 1.13 (0.90–1.42) for tolbutamide, and 1.34 (0.98–1.86) for chlorpropamide.[114] However, a retrospective study found no difference in overall mortality risk with glipizide versus glibenclamide (hazard ratio 1.04 [0.94–1.15]), versus glimepiride (1.05 [0.92–1.19]), or with glibenclamide versus. glimepiride (1.00 [0.89–1.14]) in patients with T2DM.[71]
Meta-analysis (14 trials) examining the patient-important outcomes of SUs versus metformin monotherapy found no significant difference in all-cause mortality (relative risk [RR] 0.98, 95% CI: 0.61 to 1.58) or CV mortality (RR 1.47, 95% CI: 0.54 to 4.01) in T2DM patients, but decreased risk of non-fatal macrovascular outcomes (RR: 0.67, 95% CI: 0.48 to 0.93).[29] Similar results were observed in a nation-wide study which demonstrated no significant difference between gliclazide and metformin for all-cause mortality in both patients without and with previous MI, [HR: 1.05; 95% CI:(0.94-1.16 and 0.90 (0.68-1.20) respectively].[126] Moreover, studies evaluating the risk of all-cause mortality in combinations of metformin with SUs was lower (OR 0.66, 95% CI: 0.58-0.75)[127] compared to combinations of metformin with insulin (33.7 vs. 22.7 per 1000 person years; adjusted hazard ratio (aHR), 1.44; 95% CI, 1.15-1.79; P = 0.001).[33]
ROLE OF SULFONYLUREAS IN DIABETES MANAGEMENT IN SOUTH ASIA
Affordability
Cost of medication is an important consideration, particularly in South Asia where a majority of patients are not covered under medical insurance[128] Documented efficacy/long term outcome improvement, extensive experience, and low cost have positioned SUs as the choice of OHA for the management of T2DM, particularly in resource limited countries.[129] SUs offer similar to superior glycaemic efficacy, and remain a reasonable and cost effective alternative[130] to newer agents.[131] Treatment with modern SUs is associated with a lower economic burden,[132,133] and fares better than other regimens in the cost for average glycaemic lowering.[128]
Adherence
Irrespective of the treatment regimen, poor adherence to medication is a common problem in T2DM. Adherence, defined as the extent to which patients take medications as prescribed,[134] depends on complexity of regimen, dose timing, need for self-monitoring, frequency of medication, associated side effects and cost of treatment.[135,136] Complexity of a regimen may be evaluated by considering the number of doses needed to lower glycaemic targets each day, and route of administration.[136] SUs have an oral route of administration (vs. injectable insulins and GLP-1 analogues) and once daily dosing schedule (vs. 1–2 daily for metformin and 3 times daily for alpha-glucosidase inhibitors and glinides).[128]
Fixed dose combinations
Over time, the glucose lowering efficacy of OHAs may diminish due to the progressive nature of diabetes. A combination of two or more drugs with complementary mechanism of action can help overcome multiple aetiologies of hyperglycaemia. Further, compared to two-pill therapy, fixed dose combinations (FDCs) are known to increase patient adherence.[137,138] The most widely used and recommended combination of OHAs with SUs include metformin[9] and thiazolidinediones.[139] An FDC of glimepiride/metformin (1/250mg twice daily) was associated with significant reduction in HbA1c (–1.2 vs. -0.8%, P < 0.0001), and FPG (–35.7 vs. -18.6 mg/dL, P < 0.0001) compared to metformin up-titration treatment.[140] Similarly, the FDC of pioglitazone/glimepiride (30 mg/3 mg and 15 mg/1 mg once daily) is well tolerated and found to significantly improve glycaemic control and lipid profiles in Japanese T2DM patients.[141] Therefore, using FDCs early in the course of natural history of disease progression, in optimal combinations and dosage may improve therapeutic outcomes in diabetes management.[142] Data from a prospective Indian multicentre study in urban primary care settings reported a significant reduction in HbA1c levels with FDC of gliclazide-metformin, with nearly 85% of patients achieving target FPG or HbA1c.[143]
SPECIAL SITUATIONS
Elderly
The elderly are at an increased risk of hypoglycaemia, due to declining renal and hepatic function, concurrent illnesses, poor caloric intake and poly-pharmacy.[30] Therefore, when prescribing SUs in elderly, one must exercise caution. It is suggested that use of either low dose[144] or short acting SUs is safe in this age group.[30,50]
Pregnancy and lactation
All SUs are listed as pregnancy Category C drugs and their use during pregnancy is suggested only if benefits outweigh the potential risk.[145,146,147] Studies using a single-cotyledon placental model have found minimal trans-placental transfer of glibenclamide; an observation that paved the way for further research on its role in the management of gestational diabetes mellitus.[148,149] However, contradicting results from other studies, together with lack of adequate data regarding its safety during the first trimester, and reports of increased neonatal morbidity, do not allow us to recommend SU as first line therapy in pregnancy.
Chlorpropamide and tolbutamide are known to enter breast milk while glibenclamide and glipizide are excreted in breast milk in negligible amounts. Because of their potential to cause hypoglycaemia in nursing infants, SUs are generally contraindicated in nursing mothers. If these drugs are required to be used in feeding mothers, monitoring of the breastfed infant for signs of hypoglycaemia is advisable.
Children and adolescents
There is no data supporting the use of SUs in children and adolescents (<18 years), and therefore SUs are not indicated in them. However, with increasing incidence of T2DM in paediatric and adolescent population, studies may be conducted to address the possible use of these agents in this age group. One 26-week, single-blind, active-controlled study, conducted in 285 paediatric subjects with T2DM, found that glimepiride was as effective as metformin in HbA1c reduction (–0.54%, P = 0.001 and –0.71%, P = 0.0002, respectively) with similar rates of hypoglycaemia (4.9% vs. 4.2%, respectively).[150]
Use of sulfonylureas during Ramadan
Fasting during the holy month of Ramadan has both spiritual and health benefits. In healthy subjects, fasting improves metabolic control, reduces weight and helps control hypertension. However in patients with diabetes it can induce hypoglycaemia and related complications. Ramadan fasting is acceptable for patients with well-controlled T2DM who are adherent to diet and drug intake.[151] In case of hypoglycaemia, Islam allows the patients to perform regular blood glucose monitoring and even break the fast in emergency. During Ramadan, patients should follow a highly individualized management plan[152] to avoid diabetes-related complications.
Modern SUs like gliclazide MR and glimepiride are relatively safe and effective for use during Ramadan.[153,154] South Asian guidelines recommend modern SUs (gliclazide MR and glimepiride) as effective and economical option during Ramadan fasting.[155] A study in well-controlled Asian T2DM patients showed that monotherapy with gliclazide MR in the evening can safely maintain glycaemic control with fewer hypoglycaemic episodes during the Ramadan fast.[154] Similar findings were observed with glimepiride.[153] Therefore, use of modern SUs such as gliclazide MR and glimepiride, supported by a clinician guided dosing schedule[103] is suggested in T2DM patients during Ramadan fast.[155] Practical considerations to be followed when observing fasting during Ramadan are summarised in Table 9.
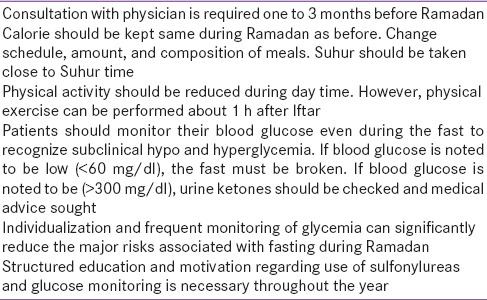
Table 9.
Practice points for persons with diabetes observing fast during Ramadan
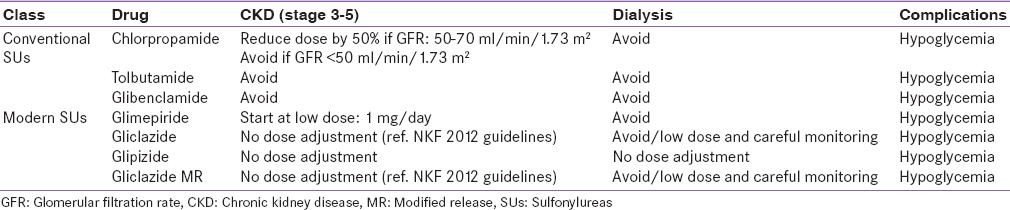
Renal impairment
Most SUs are metabolized in the liver and are excreted by the kidney.[156] Therefore in patients with renal impairment, an increased risk of hypoglycaemia is invariably seen.[30,155] The use of SUs in patients with chronic kidney disease (Stage 3) is associated with increased risk of hypoglycaemia and requires due consideration to dose adjustment. Use of long acting SUs such as glibenclamide should be contraindicated in renal failure as the active metabolites tend to accumulate, resulting in pronounced hypoglycaemia.[30,145,146,147] On the other hand, short acting SUs like glipizide and tolbutamide with inactive metabolities may be used with appropriate dose adjustments and monitoring, in moderate renal impairment (Stage 2 and 3).[157] Additionally, attention to hepatic status and potential drug interactions is particularly important when renal function deteriorates. Table 10 summarizes the usage of different SUs in renal impairment.
Table 10.
Use of different SUs in renal impairment
Hepatic impairment
Pharmacokinetic studies regarding the use of SUs in patients with hepatic insufficiency is lacking.[158] However, as most of the SUs are metabolized in liver, their use in patents with hepatic failure may pose challenges. In liver disease, inactivation of drugs is reduced, prolonging their half-life and consequently increasing the potential for hypoglycaemia. Moreover the extent of binding of SUs is dependent on the albumin concentration. Therefore in hypoalbuminemia, the amount of free drug available in plasma is enhanced resulting in frequent hypoglycaemia.[159] Hypoglycaemia is a major concern in patients with non-alcoholic steatohepatitis (NASH) when treated with SUs.[160] Further, alcohol induced enzyme degradation of SUs in patients with alcoholic liver disease may decrease clinical effectiveness of SUs. Moreover, patients with liver dysfunction experience depletion of glycogen storage, and lack of gluconeogenesis, predisposing them to hypoglycaemia.
TRANSLATING EVIDENCE INTO CLINICAL PRACTICE
Patient selection
Among many factors that are critical to the success of SU therapy, patient selection is paramount. Given that SUs act by stimulating β-cells, it is unlikely that patients without sufficient number of β-cells will respond to these medications. Therefore these agents may provide clinically meaningful outcomes in T2DM patients who still retain some β-cell function.[50,51] SUs should be preferred as initial therapy in patients with newly or previously diagnosed (<5 years) with functional β-cell mass, contraindication or intolerance to metformin, high HbA1c levels, suspected MODY, and willingness to follow a regular dietary and exercise plan [Table 11].[31] Since SUs may influence weight changes, they should be preferred in leaner subjects; however, glimepiride and gliclazide MR can be used in both obese and non-obese subjects. Patients with hepatic and/or renal impairment are not suitable candidates for SU therapy.[161] Similarly, SUs should be avoided in elderly, patients with long-standing diabetes and those with poor nutrition or who commonly miss meals, or have concomitant CVD.[30,50,162]
Table 11.
Place of SUs in diabetes therapy
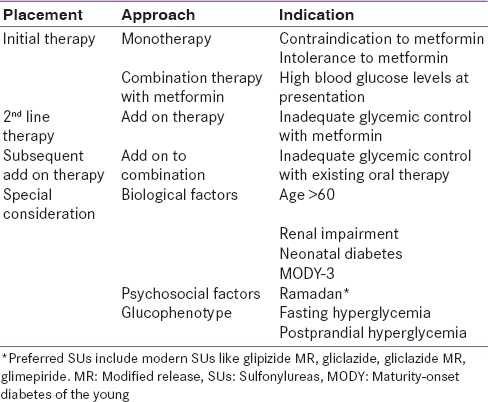
Drug selection
Clinical factors such as levels of fasting and post-prandial hyperglycaemia, comorbid hypertension, CVD, and hepatic or renal dysfunction determine the selection of one SU over the other. In patients with fasting hyperglycaemia twice daily SU in combination with metformin, while in those with post-prandial hyperglycaemia, short-acting SUs should be preferred.[50,145,146,147] For patients at higher risk of hypoglycaemia, gliclazide MR may be considered safe and effective. In the elderly and patients with hypertension or CVD or hepatic or renal dysfunction, glibenclamide is not preferred. If clinically indicated, glipizide can be used in patients with hepatic or renal dysfunction, and glimepiride or gliclazide in those with CVD [Table 11]. Combining two SUs with one other is not logical as they have similar mechanism of action. However, SUs may be combined with other OHAs such as biguanides, thiazolidinediones (with complementary mechanism of actions), and even with insulin.
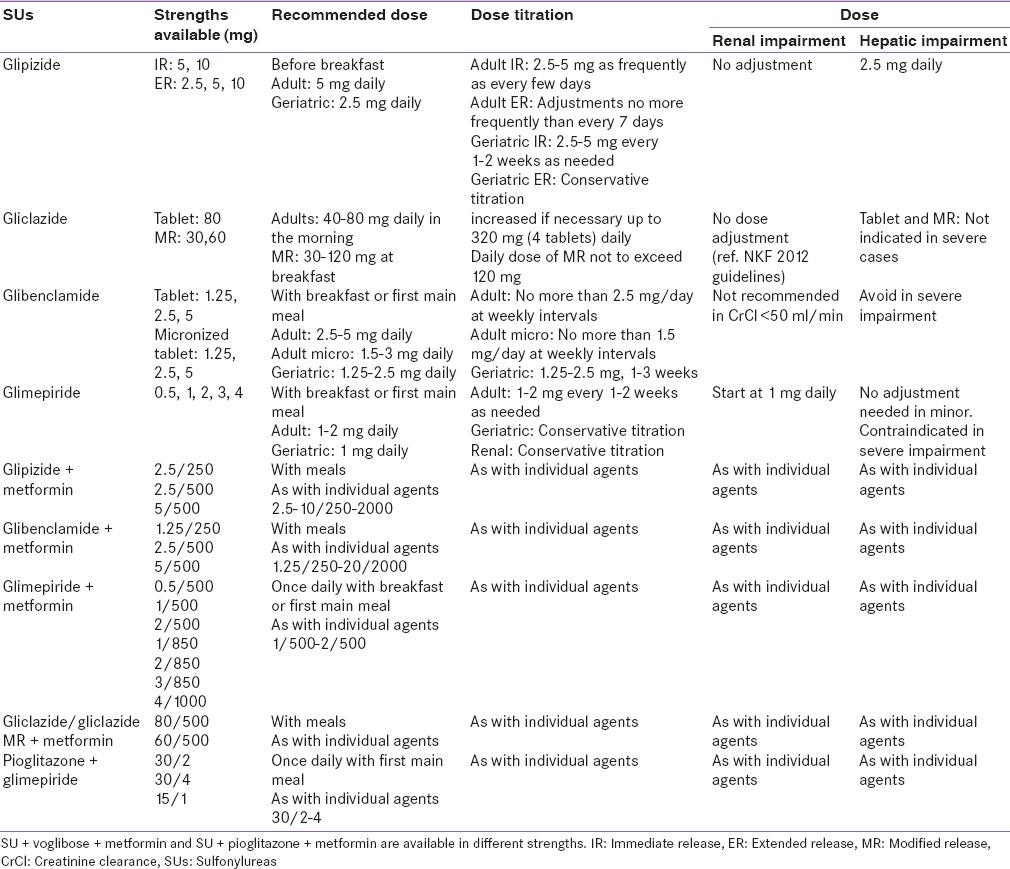
Dosage selection
In patients with T2DM who are uncontrolled on metformin, a low initial dose may be started and titrated every 1-2 weeks, based on self-monitoring of blood glucose until maximal benefit is achieved.[30] Long-term therapy should be continued as long as the drug maintains euglycaemia, without causing hypoglycaemia.[30] MR formulations of SUs may be used when further dose reduction is required.[131] It is recommended to reduce the dose of SU when DPP-4 inhibitors are initiated, especially in the elderly and/or patients with renal insufficiency. When appropriate glycaemic control is not achieved after initiation of DPP-4 inhibitors, consider increasing the dose of SUs. However when hypoglycaemic episodes are confirmed, reduction of dose should be considered.[162] Table 12 summarises strengths, time of administration and recommended dosages of available SUs either individually or in FDCs.
Table 12.
Strengths and timing of administration of various SUs
Patient empowerment
Diabetes being a progressive disease requires constant self-management on day-to-day basis. The need for patient education and participation is more evident with the growing complexity of management. Patients should be encouraged and supported to become active partners in decision-making process, to set realistic goals, select appropriate management strategies, enhance adherence and improve treatment outcomes. Patients and their families should be educated on safe use of SUs, while providing information on the signs and symptoms of hypoglycaemia, self-down titration of doses in case of hypoglycaemia, and the importance of regular and healthy lifestyle. Scored tablets may be used to facilitate down titration of doses in case of suspected hypoglycaemia. Training on hypoglycaemia awareness can increase adherence to prescribed SU regimen.[144] Self-monitoring of blood glucose (SMBG) is another important tool that aids in improving glycaemic control. Frequent SMBG is recommended in patients at increased risk of hypoglycaemia, particularly elderly and patients with renal or hepatic impairment.
Physician empowerment
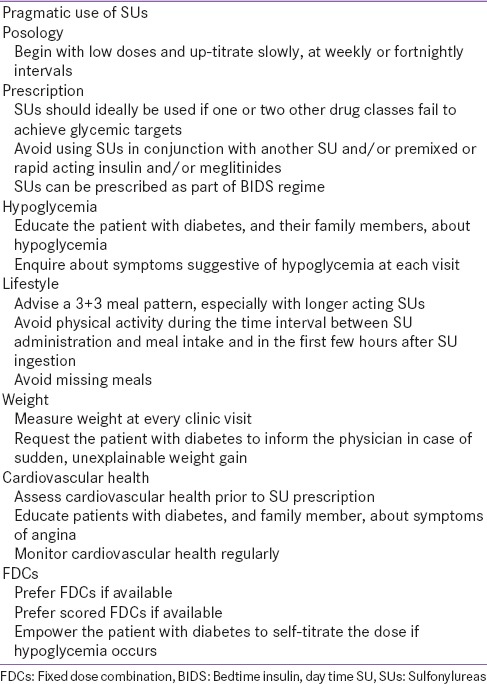
Physicians should adopt a patient-centred approach when prescribing SUs for management of diabetes. Physicians should carefully consider clinical profile of the patient and implement strategies that will not only help to minimize patient's concerns over SU treatment, but also empower them for self-management. Physicians play an important role in selecting the “right drug (SU in this case) in right dose at right time to right patient”. It is important that SUs are initiated at low doses and gradually titrated until glycaemic targets are achieved. Clinical judgement is required when titrating SU dose. This is particularly crucial in patients with renal or hepatic impairment. At each visit physicians should enquire about symptoms suggestive of hypoglycaemia and adjust doses accordingly when risks outweigh glycaemic benefits. Pragmatic use of SUs based on various patient-related characteristics has been described in Table 13.[143]
Table 13.
Practical considerations for the use of SUs
CONCLUSIONS
SUs are the main stream of pharmacotherapy in the management of patients with T2DM. Their well-established glycaemic efficacy, safety and tolerability support their use as an integral part of diabetes treatment. Given the fact that many of the clinical concerns associated with the use of SUs are agent-specific, and do not pertain to the class as such, a careful choice of specific SU should be considered beneficial. Considering better glycaemic efficacy, long-term outcomes and low medication cost, SUs, should be continued to be used as a front-line agent in the treatment algorithm of T2DM, particularly in South Asia. Proper patient selection, choice of drug and dose, patient education and empowerment, and physician training will help ensure effective and safe use of this important class of drugs.
Financial support and sponsorship
Sanofi India.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors acknowledge Sanofi INDIA for supporting this initiative with an academic grant and M. Vimal Kumar Varma, Ph.D. from Jeevan Scientific Technology Limited (Hyderabad, India) for editorial assistance in the development of this manuscript.
REFERENCES
- 1.International Diabetes Federation. Key Findings. 2014. [Last accessed on 2015 Mar 25]. Available from: http://www.idf.org/diabetesatlas/update-2014 .
- 2.Alexander GC, Sehgal NL, Moloney RM, Stafford RS. National trends in treatment of type 2 diabetes mellitus, 1994-2007. Arch Intern Med. 2008;168:2088–94. doi: 10.1001/archinte.168.19.2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kannan, Arshad, Senthil K. A study on drug utilization of oral hypoglycemic agents in type-2 diabetic patients. Asian J Pharm Clin Res. 2011;5:60–4. [Google Scholar]
- 4.Acharya KG, Shah KN, Solanki ND, Rana DA. Evaluation of antidiabetic prescriptions, cost and adherence to treatment guidelines: A prospective, cross-sectional study at a tertiary care teaching hospital. J Basic Clin Pharm. 2013;4:82–7. doi: 10.4103/0976-0105.121653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wysowski DK, Armstrong G, Governale L. Rapid increase in the use of oral antidiabetic drugs in the United States, 1990-2001. Diabetes Care. 2003;26:1852–5. doi: 10.2337/diacare.26.6.1852. [DOI] [PubMed] [Google Scholar]
- 6.Grant RW, Pirraglia PA, Meigs JB, Singer DE. Trends in complexity of diabetes care in the United States from 1991 to 2000. Arch Intern Med. 2004;164:1134–9. doi: 10.1001/archinte.164.10.1134. [DOI] [PubMed] [Google Scholar]
- 7.Cohen FJ, Neslusan CA, Conklin JE, Song X. Recent antihyperglycemic prescribing trends for US privately insured patients with type 2 diabetes. Diabetes Care. 2003;26:1847–51. doi: 10.2337/diacare.26.6.1847. [DOI] [PubMed] [Google Scholar]
- 8.Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2008. Centers for Disease Control and Prevention. National Diabetes Fact Sheet: General Information and National Estimates on Diabetes in the United States, 2007. [Google Scholar]
- 9.Agarwal AA, Jadhav PR, Deshmukh YA. Prescribing pattern and efficacy of anti-diabetic drugs in maintaining optimal glycemic levels in diabetic patients. J Basic Clin Pharm. 2014;5:79–83. doi: 10.4103/0976-0105.139731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahmed QS, Sayedda K, Dharmender G, Ahmad AN. Prescribing patterns of Antidiabetic medications in a tertiary care teaching hospital, Bareilly, UP, India. J Pharm Sci Innov. 2013;2:41–6. [Google Scholar]
- 11.Desai NR, Shrank WH, Fischer MA, Avorn J, Liberman JN, Schneeweiss S, et al. Patterns of medication initiation in newly diagnosed diabetes mellitus: Quality and cost implications. Am J Med. 2012;125(302):1–7. doi: 10.1016/j.amjmed.2011.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Essential Medicine List of Bangladesh. Ministry of Health and Family Welfare. 2008. [Last accessed on 2015 Mar 25]. Available from: http://www.who.int/selection_medicines/country_lists/bgd_eml_2008.pdf .
- 13.National List of Essential Medicines of India. 2011. [Last accessed on 2015 Mar 25]. Available from: http://www.mohfw.nic.in/WriteReadData/l892s/7364497513National%20List%20of%20Essential%20Medicine,%202011.pdf .
- 14.National List of Essential Medicines of Nepal. 2011. [Last accessed on 2015 Mar 25]. Available from: http://www.searo.who.int/entity/medicines/neml_nep_2011_govtwebsite_ok.pdf .
- 15.National Essential Medicine List of Pakistan. Ministry of Health. Government of Pakistan. [Last accessed on 2015 Mar 25]. Available from: http://www.apps.who.int/medicinedocs/documents/s17119e/s17119e.pdf .
- 16.National List of Essential Medicines Sri Lanka. 2009. [Last accessed on 2015 Mar 25]. Available from: http://www.apps.who.int/medicinedocs/documents/s16730e/s16730e.pdf .
- 17.Kalra S, Gupta Y, Saboo B. Essential drugs in diabetes: South and South East Asian perspective. J Soc Health Diabetes. 2015;3:4–6. [Google Scholar]
- 18.IMS Health. 2014. [Last accessed on 2015 Apr 01]. Available from: http://www.imshealth.com/portal/site/imshealth .
- 19.IMS TSA. 2014. [Last accessed on 2015 Apr 01]. Available from: http://www.imsbrogancapabilities.com/en/healthcare-tsa.html .
- 20.Srivastava S, Saxena GN, Keshwani P, Gupta R. Comparing the efficacy and safety profile of sitagliptin versus glimepiride in patients of type 2 diabetes mellitus inadequately controlled with metformin alone. J Assoc Physicians India. 2012;60:27–30. [PubMed] [Google Scholar]
- 21.Abrar A, Khan S, Rehman MU, Jan T, Faisal M. Safety and efficacy of sitagliptin compared with glimepiride in patients with type 2 diabetes mellitus inadequately controlled with metformin monotherapy. Gomal J Med Sci. 2013;11:3–7. [Google Scholar]
- 22.Philippe J, Raccah D. Treating type 2 diabetes: How safe are current therapeutic agents? Int J Clin Pract. 2009;63:321–32. doi: 10.1111/j.1742-1241.2008.01980.x. [DOI] [PubMed] [Google Scholar]
- 23.Seltzer HS. Efficacy and safety of oral hypoglycemic agents. Annu Rev Med. 1980;31:261–72. doi: 10.1146/annurev.me.31.020180.001401. [DOI] [PubMed] [Google Scholar]
- 24.Aguilar-Bryan L, Nichols CG, Wechsler SW, Clement JP, 4th, Boyd AE, 3rd, González G, et al. Cloning of the beta cell high-affinity sulfonylurea receptor: A regulator of insulin secretion. Science. 1995;268:423–6. doi: 10.1126/science.7716547. [DOI] [PubMed] [Google Scholar]
- 25.Hirst JA, Farmer AJ, Dyar A, Lung TW, Stevens RJ. Estimating the effect of sulfonylurea on HbA1c in diabetes: A systematic review and meta-analysis. Diabetologia. 2013;56:973–84. doi: 10.1007/s00125-013-2856-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352:837–53. [PubMed] [Google Scholar]
- 27.Basit A, Riaz M, Fawwad A. Glimepiride: Evidence-based facts, trends, and observations (GIFTS). [corrected] Vasc Health Risk Manag. 2012;8:463–72. doi: 10.2147/HIV.S33194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Canaglifozin (Invokana) for type 2 diabetes. Med Lett Drugs Ther. 2013;55:37–9. [PubMed] [Google Scholar]
- 29.Hemmingsen B, Schroll JB, Wetterslev J, Gluud C, Vaag A, Sonne DP, et al. Sulfonylurea versus metformin monotherapy in patients with type 2 diabetes: A Cochrane systematic review and meta-analysis of randomized clinical trials and trial sequential analysis. CMAJ Open. 2014;2:E162–75. doi: 10.9778/cmajo.20130073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thulé PM, Umpierrez G. Sulfonylureas: A new look at old therapy. Curr Diab Rep. 2014:14–473. doi: 10.1007/s11892-014-0473-5. [DOI] [PubMed] [Google Scholar]
- 31.Sehra D, Sehra S, Sehra ST. Sulfonylureas: Do we need to introspect safety again? Expert Opin Drug Saf. 2011;10:851–61. doi: 10.1517/14740338.2011.583234. [DOI] [PubMed] [Google Scholar]
- 32.Maedler K, Carr RD, Bosco D, Zuellig RA, Berney T, Donath MY. Sulfonylurea induced beta-cell apoptosis in cultured human islets. J Clin Endocrinol Metab. 2005;90:501–6. doi: 10.1210/jc.2004-0699. [DOI] [PubMed] [Google Scholar]
- 33.Roumie CL, Greevy RA, Grijalva CG, Hung AM, Liu X, Murff HJ, et al. Association between intensification of metformin treatment with insulin vs sulfonylureas and cardiovascular events and all-cause mortality among patients with diabetes. JAMA. 2014;311:2288–96. doi: 10.1001/jama.2014.4312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Handelsman Y, Mechanick JI, Blonde L, Grunberger G, Bloomgarden ZT, Bray GA, et al. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for developing a diabetes mellitus comprehensive care plan. Endocr Pract. 2011;17(Suppl 2):1–53. doi: 10.4158/ep.17.s2.1. [DOI] [PubMed] [Google Scholar]
- 35.Kramer W, Müller G, Geisen K. Characterization of the molecular mode of action of the sulfonylurea, glimepiride, at beta-cells. Horm Metab Res. 1996;28:464–8. doi: 10.1055/s-2007-979838. [DOI] [PubMed] [Google Scholar]
- 36.Briscoe VJ, Griffith ML, Davis SN. The role of glimepiride in the treatment of type 2 diabetes mellitus. Expert Opin Drug Metab Toxicol. 2010;6:225–35. doi: 10.1517/17425250903512955. [DOI] [PubMed] [Google Scholar]
- 37.Davis SN. The role of glimepiride in the effective management of Type 2 diabetes. J Diabetes Complications. 2004;18:367–76. doi: 10.1016/j.jdiacomp.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 38.Gribble FM, Reimann F. Differential selectivity of insulin secretagogues: Mechanisms, clinical implications, and drug interactions. J Diabetes Complications. 2003;17(2 Suppl):11–5. doi: 10.1016/s1056-8727(02)00272-6. [DOI] [PubMed] [Google Scholar]
- 39.Ashcroft FM, Gribble FM. Tissue-specific effects of sulfonylureas: Lessons from studies of cloned K (ATP) channels. J Diabetes Complications. 2000;14:192–6. doi: 10.1016/s1056-8727(00)00081-7. [DOI] [PubMed] [Google Scholar]
- 40.Gribble FM, Ashcroft FM. Sulfonylurea sensitivity of adenosine triphosphate-sensitive potassium channels from beta cells and extrapancreatic tissues. Metabolism. 2000;49(10)(Suppl 2):3–6. [PubMed] [Google Scholar]
- 41.Song DK, Ashcroft FM. Glimepiride block of cloned beta-cell, cardiac and smooth muscle K (ATP) channels. Br J Pharmacol. 2001;133:193–9. doi: 10.1038/sj.bjp.0704062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vila-Carriles WH, Zhao G, Bryan J. Defining a binding pocket for sulfonylureas in ATP-sensitive potassium channels. FASEB J. 2007;21:18–25. doi: 10.1096/fj.06-6730hyp. [DOI] [PubMed] [Google Scholar]
- 43.Winkler M, Stephan D, Bieger S, Kühner P, Wolff F, Quast U. Testing the bipartite model of the sulfonylurea receptor binding site: Binding of A-, B-, and A+B-site ligands. J Pharmacol Exp Ther. 2007;322:701–8. doi: 10.1124/jpet.107.123224. [DOI] [PubMed] [Google Scholar]
- 44.Kramer W, Müller G, Girbig F, Gutjahr U, Kowalewski S, Hartz D, et al. Differential interaction of glimepiride and glibenclamide with the beta-cell sulfonylurea receptor. II. Photoaffinity labeling of a 65 kDa protein by [3H] glimepiride. Biochim Biophys Acta. 1994;1191:278–90. doi: 10.1016/0005-2736(94)90178-3. [DOI] [PubMed] [Google Scholar]
- 45.Müller G, Hartz D, Pünter J, Okonomopulos R, Kramer W. Differential interaction of glimepiride and glibenclamide with the beta-cell sulfonylurea receptor. I. Binding characteristics. Biochim Biophys Acta. 1994;1191:267–77. doi: 10.1016/0005-2736(94)90177-5. [DOI] [PubMed] [Google Scholar]
- 46.Holstein A, Plaschke A, Egberts EH. Lower incidence of severe hypoglycaemia in patients with type 2 diabetes treated with glimepiride versus glibenclamide. Diabetes Metab Res Rev. 2001;17:467–73. doi: 10.1002/dmrr.235. [DOI] [PubMed] [Google Scholar]
- 47.Korytkowski M, Thomas A, Reid L, Tedesco MB, Gooding WE, Gerich J. Glimepiride improves both first and second phases of insulin secretion in type 2 diabetes. Diabetes Care. 2002;25:1607–11. doi: 10.2337/diacare.25.9.1607. [DOI] [PubMed] [Google Scholar]
- 48.Proks P, Reimann F, Green N, Gribble F, Ashcroft F. Sulfonylurea stimulation of insulin secretion. Diabetes. 2002;51(Suppl 3):S368–76. doi: 10.2337/diabetes.51.2007.s368. [DOI] [PubMed] [Google Scholar]
- 49.Pfeiffer AF, Klein HH. The treatment of type 2 diabetes. Dtsch Arztebl Int. 2014;111:69–81. doi: 10.3238/arztebl.2014.0069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nyenwe EA, Jerkins TW, Umpierrez GE, Kitabchi AE. Management of type 2 diabetes: Evolving strategies for the treatment of patients with type 2 diabetes. Metabolism. 2011;60:1–23. doi: 10.1016/j.metabol.2010.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, et al. Management of hyperglycemia in type 2 diabetes: A patient-centered approach: Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetes Care. 2012;35:1364–79. doi: 10.2337/dc12-0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.ADVANCE Collaborative Group. Patel A, MacMahon S, Chalmers J, Neal B, Billot L, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560–72. doi: 10.1056/NEJMoa0802987. [DOI] [PubMed] [Google Scholar]
- 53.Kahn SE, Haffner SM, Heise MA, Herman WH, Holman RR, Jones NP, et al. Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. N Engl J Med. 2006;355:2427–43. doi: 10.1056/NEJMoa066224. [DOI] [PubMed] [Google Scholar]
- 54.Zhu H, Zhu S, Zhang X, Guo Y, Shi Y, Chen Z, et al. Comparative efficacy of glimepiride and metformin in monotherapy of type 2 diabetes mellitus: Meta-analysis of randomized controlled trials. Diabetol Metab Syndr. 2013:5–70. doi: 10.1186/1758-5996-5-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Charpentier G, Fleury F, Kabir M, Vaur L, Halimi S. Improved glycaemic control by addition of glimepiride to metformin monotherapy in type 2 diabetic patients. Diabet Med. 2001;18:828–34. doi: 10.1046/j.1464-5491.2001.00582.x. [DOI] [PubMed] [Google Scholar]
- 56.McCluskey D, Touger MS, Melis R, Schleusener DS, McCluskey D. Results of a randomized, double-blind, placebo-controlled study administering glimepiride to patients with type 2 diabetes mellitus inadequately controlled with rosiglitazone monotherapy. Clin Ther. 2004;26:1783–90. doi: 10.1016/j.clinthera.2004.11018. [DOI] [PubMed] [Google Scholar]
- 57.Fritsche A, Schweitzer MA, Häring HU. Glimepiride combined with morning insulin glargine, bedtime neutral protamine hagedorn insulin, or bedtime insulin glargine in patients with type 2 diabetes. A randomized, controlled trial. Ann Intern Med. 2003;138:952–9. doi: 10.7326/0003-4819-138-12-200306170-00006. [DOI] [PubMed] [Google Scholar]
- 58.Hermansen K, Kipnes M, Luo E, Fanurik D, Khatami H, Stein P, et al. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor, sitagliptin, in patients with type 2 diabetes mellitus inadequately controlled on glimepiride alone or on glimepiride and metformin. Diabetes Obes Metab. 2007;9:733–45. doi: 10.1111/j.1463-1326.2007.00744.x. [DOI] [PubMed] [Google Scholar]
- 59.Gitt AK, Bramlage P, Binz C, Schneider S, Krekler M, Tschoepe D. Outcome of sulfonylurea and insulin versus incretin-based treatment in type 2 diabetes patients uncontrolled on prior metformin mono therapy: Results of Dia Regis. J Am Coll Cardiol. 2014;63(12 Suppl):A1336. [Google Scholar]
- 60.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577–89. doi: 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]
- 61.Zoungas S, Chalmers J, Neal B, Billot L, Li Q, Hirakawa Y, et al. Follow-up of blood-pressure lowering and glucose control in type 2 diabetes. N Engl J Med. 2014;371:1392–406. doi: 10.1056/NEJMoa1407963. [DOI] [PubMed] [Google Scholar]
- 62.Hayward RA, Reaven PD, Wiitala WL, Bahn GD, Reda DJ, Ge L, et al. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;372:2197–206. doi: 10.1056/NEJMoa1414266. [DOI] [PubMed] [Google Scholar]
- 63.Darlow BA. Symptomatic hyponatraemia associated with tolbutamide therapy. Postgrad Med J. 1977;53:223–4. doi: 10.1136/pgmj.53.618.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Harris EL. Adverse reactions to oral antidiabetic agents. Br Med J. 1971;3:29–30. doi: 10.1136/bmj.3.5765.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Campbell RK. Glimepiride: Role of a new sulfonylurea in the treatment of type 2 diabetes mellitus. Ann Pharmacother. 1998;32:1044–52. doi: 10.1345/aph.17360. [DOI] [PubMed] [Google Scholar]
- 66.Gajos G, Pilacinski S, Zozulinska-Ziólkiewicz D. Controversies in diabetes in 2013 – A brief update. Adv Clin Exp Med. 2013;22:777–84. [PubMed] [Google Scholar]
- 67.Barzilai N, Groop PH, Groop L, DeFronzo RA. A novel mechanism of glipizide sulfonylurea action: Decreased metabolic clearance rate of insulin. Acta Diabetol. 1995;32:273–8. doi: 10.1007/BF00576262. [DOI] [PubMed] [Google Scholar]
- 68.Landstedt-Hallin L, Adamson U, Lins PE. Oral glibenclamide suppresses glucagon secretion during insulin-induced hypoglycemia in patients with type 2 diabetes. J Clin Endocrinol Metab. 1999;84:3140–5. doi: 10.1210/jcem.84.9.6002. [DOI] [PubMed] [Google Scholar]
- 69.Mori RC, Hirabara SM, Hirata AE, Okamoto MM, Machado UF. Glimepiride as insulin sensitizer: Increased liver and muscle responses to insulin. Diabetes Obes Metab. 2008;10:596–600. doi: 10.1111/j.1463-1326.2008.00870.x. [DOI] [PubMed] [Google Scholar]
- 70.Li CJ, Zhang JY, Yu DM, Zhang QM. Adding glimepiride to current insulin therapy increases high-molecular weight adiponectin levels to improve glycemic control in poorly controlled type 2 diabetes. Diabetol Metab Syndr. 2014;6:41. doi: 10.1186/1758-5996-6-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pantalone KM, Kattan MW, Yu C, Wells BJ, Arrigain S, Jain A, et al. The risk of overall mortality in patients with type 2 diabetes receiving glipizide, glyburide, or glimepiride monotherapy: A retrospective analysis. Diabetes Care. 2010;33:1224–9. doi: 10.2337/dc10-0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mocanu MM, Maddock HL, Baxter GF, Lawrence CL, Standen NB, Yellon DM. Glimepiride, a novel sulfonylurea, does not abolish myocardial protection afforded by either ischemic preconditioning or diazoxide. Circulation. 2001;103:3111–6. doi: 10.1161/01.cir.103.25.3111. [DOI] [PubMed] [Google Scholar]
- 73.Nakamura I, Oyama J, Komoda H, Shiraki A, Sakamoto Y, Taguchi I, et al. Possible effects of glimepiride beyond glycemic control in patients with type 2 diabetes: A preliminary report. Cardiovasc Diabetol. 2014:13–15. doi: 10.1186/1475-2840-13-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Diamicron MR (Gliclazide) Product Monograph. [Last accessed on 2015 Apr 01]. Available from: http://www.servier.ca/sites/default/files/webform/Products/EN-DIAMICRON-MR-PI.pdf .
- 75.Yosefy C, Magen E, Kiselevich A, Priluk R, London D, Volchek L, et al. Rosiglitazone improves, while Glibenclamide worsens blood pressure control in treated hypertensive diabetic and dyslipidemic subjects via modulation of insulin resistance and sympathetic activity. J Cardiovasc Pharmacol. 2004;44:215–22. doi: 10.1097/00005344-200408000-00011. [DOI] [PubMed] [Google Scholar]
- 76.Global Guideline for Type 2 Diabetes. IDF. 2012. [Last accessed on 2015 Mar 25]. Available from: http://www.idf.org/sites/default/files/IDF-Guideline-for-Type-2-Diabetes-pdf .
- 77.Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, et al. Management of hyperglycemia in type 2 diabetes, 2015: A patient-centered approach: Update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38:140–9. doi: 10.2337/dc14-2441. [DOI] [PubMed] [Google Scholar]
- 78.Garber AJ, Abrahamson MJ, Barzilay JI, Blonde L, Bloomgarden ZT, Bush MA, et al. American Association of Clinical Endocrinologists’ comprehensive diabetes management algorithm 2013 statement-Executive summary. Endocr Pract. 2013;19:536–57. doi: 10.4158/EP13176.CS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.NICE Clinical Guideline 87. Type 2 Diabetes: The Management of Type 2 Diabetes. NICE. 2009. [Last accessed on 2015 Mar 25]. Available from: http://www.nice.org.uk/guidance/ta203/resources/nice-recommends-liraglutide-for-type-2-diabetes-mellitus4 .
- 80.SIGN. Management of Diabetes. A National Clinical Guideline. SIGN. 2010. [Last accessed on 2015 Mar 25]. Available from: http://www.sign.ac.uk/pdf/sign116.pdf .
- 81.Amod A, Ascott-Evans BH, Berg GI, Blom DJ, Brown SL, Carrihill MM, et al. The 2012 SEMDSA guideline for the management of type 2 diabetes (revised). The 2012 SEMDSA treatment algorithm for type 2 diabetes. J Endocrinol Metab Diabetes S Afr. 2012;17(Suppl 1):S36–40. [Google Scholar]
- 82.Japan Diabetes Society. Treatment Guideline for Diabetes; 2012-2013. [Last accessed on 2015 Mar 25]. Available from: http://www.jds.or.jp/modules/en/index.php?content_id=44 .
- 83.Chinese Diabetes Society. China Guideline for type 2 Diabetes. Chin J Diabetes. 2010;2(Suppl 2):1–56. [Google Scholar]
- 84.Ko SH, Kim SR, Kim DJ, Oh SJ, Lee HJ, Shim KH, et al. 2011 clinical practice guidelines for type 2 diabetes in Korea. Diabetes Metab J. 2011;35:431–6. doi: 10.4093/dmj.2011.35.5.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.ICMR 2005. [Last accessed on 2015 Apr 03]. Available from: http://www.icmr.nic.in/guidelines_diabetes/section7.pdf .
- 86.Harrower AD. Comparison of efficacy, secondary failure rate, and complications of sulfonylureas. J Diabetes Complications. 1994;8:201–3. doi: 10.1016/1056-8727(94)90044-2. [DOI] [PubMed] [Google Scholar]
- 87.Satoh J, Takahashi K, Takizawa Y, Ishihara H, Hirai M, Katagiri H, et al. Secondary sulfonylurea failure: Comparison of period until insulin treatment between diabetic patients treated with gliclazide and glibenclamide. Diabetes Res Clin Pract. 2005;70:291–7. doi: 10.1016/j.diabres.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 88.Dor Y, Glaser B. β-cell dedifferentiation and type 2 diabetes. N Engl J Med. 2013;368:572–3. doi: 10.1056/NEJMcibr1214034. [DOI] [PubMed] [Google Scholar]
- 89.Talchai C, Xuan S, Lin HV, Sussel L, Accili D. Pancreatic ß cell dedifferentiation as a mechanism of diabetic ß cell failure. Cell. 2012;150:1223–34. doi: 10.1016/j.cell.2012.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kitamura T. The role of FOXO1 in ß-cell failure and type 2 diabetes mellitus. Nat Rev Endocrinol. 2013;9:615–23. doi: 10.1038/nrendo.2013.157. [DOI] [PubMed] [Google Scholar]
- 91.Nybäck-Nakell A, Bergström J, Adamson U, Lins PE, Landstedt-Hallin L. Decreasing postprandial C-peptide levels over time are not associated with long-term use of sulphonylurea: An observational study. Diabetes Metab. 2010;36:375–80. doi: 10.1016/j.diabet.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 92.Gudipaty L, Rosenfeld NK, Fuller CS, Gallop R, Schutta MH, Rickels MR. Effect of exenatide, sitagliptin, or glimepiride on ß-cell secretory capacity in early type 2 diabetes. Diabetes Care. 2014;37:2451–8. doi: 10.2337/dc14-0398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Krentz A, Sinclair A. Do sulfonylureas still have a role in type 2 diabetes? Curr Issues. 2011;22:32–6. [Google Scholar]
- 94.Nathan DM, Buse JB, Davidson MB, Heine RJ, Holman RR, Sherwin R, et al. Management of hyperglycemia in type 2 diabetes: A consensus algorithm for the initiation and adjustment of therapy: A consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2006;29:1963–72. doi: 10.2337/dc06-9912. [DOI] [PubMed] [Google Scholar]
- 95.Turner R. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–53. [PubMed] [Google Scholar]
- 96.Turner R, Cull C, Holman R. United Kingdom Prospective Diabetes Study 17: A 9-year update of a randomized, controlled trial on the effect of improved metabolic control on complications in non-insulin-dependent diabetes mellitus. Ann Intern Med. 1996;124(1 Pt 2):136–45. doi: 10.7326/0003-4819-124-1_part_2-199601011-00011. [DOI] [PubMed] [Google Scholar]
- 97.Olsson PO, Lindström T. Combination-therapy with bedtime nph insulin and sulphonylureas gives similar glycaemic control but lower weight gain than insulin twice daily in patients with type 2 diabetes. Diabetes Metab. 2002;28(4 Pt 1):272–7. [PubMed] [Google Scholar]
- 98.Bugos C, Austin M, Atherton T, Viereck C. Long-term treatment of type 2 diabetes mellitus with glimepiride is weight neutral: A meta-analysis. Diabetes Res Clin Pract. 2000:50–S47. [Google Scholar]
- 99.Johnston PS, Lebovitz HE, Coniff RF, Simonson DC, Raskin P, Munera CL. Advantages of alpha-glucosidase inhibition as monotherapy in elderly type 2 diabetic patients. J Clin Endocrinol Metab. 1998;83:1515–22. doi: 10.1210/jcem.83.5.4824. [DOI] [PubMed] [Google Scholar]
- 100.Schernthaner G, Grimaldi A, Di Mario U, Drzewoski J, Kempler P, Kvapil M, et al. GUIDE study: Double-blind comparison of once-daily gliclazide MR and glimepiride in type 2 diabetic patients. Eur J Clin Invest. 2004;34:535–42. doi: 10.1111/j.1365-2362.2004.01381.x. [DOI] [PubMed] [Google Scholar]
- 101.Weitgasser R, Lechleitner M, Luger A, Klingler A. Effects of glimepiride on HbA (1c) and body weight in Type 2 diabetes: Results of a 1.5-year follow-up study. Diabetes Res Clin Pract. 2003;61:13–9. doi: 10.1016/s0168-8227(02)00254-1. [DOI] [PubMed] [Google Scholar]
- 102.Martin S, Kolb H, Beuth J, van Leendert R, Schneider B, Scherbaum WA. Change in patients' body weight after 12 months of treatment with glimepiride or glibenclamide in Type 2 diabetes: A multicentre retrospective cohort study. Diabetologia. 2003;46:1611–7. doi: 10.1007/s00125-003-1238-x. [DOI] [PubMed] [Google Scholar]
- 103.Hassanein M, Abdallah K, Schweizer A. A double-blind, randomized trial, including frequent patient-physician contacts and Ramadan-focused advice, assessing vildagliptin and gliclazide in patients with type 2 diabetes fasting during Ramadan: The STEADFAST study. Vasc Health Risk Manag. 2014;10:319–26. doi: 10.2147/VHRM.S64038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Leese GP, Wang J, Broomhall J, Kelly P, Marsden A, Morrison W, et al. Frequency of severe hypoglycemia requiring emergency treatment in type 1 and type 2 diabetes: A population-based study of health service resource use. Diabetes Care. 2003;26:1176–80. doi: 10.2337/diacare.26.4.1176. [DOI] [PubMed] [Google Scholar]
- 105.United Kingdom Prospective Diabetes Study 24: A 6-year, randomized, controlled trial comparing sulfonylurea, insulin, and metformin therapy in patients with newly diagnosed type 2 diabetes that could not be controlled with diet therapy. United Kingdom Prospective Diabetes Study Group. Ann Intern Med. 1998;128:165–75. doi: 10.7326/0003-4819-128-3-199802010-00001. [DOI] [PubMed] [Google Scholar]
- 106.Landman GW, de Bock GH, van Hateren KJ, van Dijk PR, Groenier KH, Gans RO, et al. Safety and efficacy of gliclazide as treatment for type 2 diabetes: A systematic review and meta-analysis of randomized trials. PLoS One. 2014;9 doi: 10.1371/journal.pone.0082880. e82880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Draeger KE, Wernicke-Panten K, Lomp HJ, Schüler E, Rosskamp R. Long-term treatment of type 2 diabetic patients with the new oral antidiabetic agent glimepiride (Amaryl): A double-blind comparison with glibenclamide. Horm Metab Res. 1996;28:419–25. doi: 10.1055/s-2007-979830. [DOI] [PubMed] [Google Scholar]
- 108.Feinglos MN, Bethel MA. Therapy of type 2 diabetes, cardiovascular death, and the UGDP. Am Heart J. 1999;138(5 Pt 1):S346–52. doi: 10.1016/s0002-8703(99)70034-7. [DOI] [PubMed] [Google Scholar]
- 109.Seltzer HS. A summary of criticisms of the findings and conclusions of the University Group Diabetes Program (UGDP) Diabetes. 1972;21:976–9. doi: 10.2337/diab.21.9.976. [DOI] [PubMed] [Google Scholar]
- 110.Kilo C, Miller JP, Williamson JR. The Achilles heel of the University Group Diabetes Program. JAMA. 1980;243:450–7. [PubMed] [Google Scholar]
- 111.Rydén L, Standl E, Bartnik M, Van den Berghe G, Betteridge J, de Boer MJ, et al. Guidelines on diabetes, pre-diabetes, and cardiovascular diseases: Executive summary. The Task Force on Diabetes and Cardiovascular Diseases of the European Society of Cardiology (ESC) and of the European Association for the Study of Diabetes (EASD) Eur Heart J. 2007;28:88–136. doi: 10.1093/eurheartj/ehl260. [DOI] [PubMed] [Google Scholar]
- 112.Rosenstock J, Marx N, Kahn SE, Zinman B, Kastelein JJ, Lachin JM, et al. Cardiovascular outcome trials in type 2 diabetes and the sulphonylurea controversy: Rationale for the active-comparator CAROLINA trial. Diab Vasc Dis Res. 2013;10:289–301. doi: 10.1177/1479164112475102. [DOI] [PubMed] [Google Scholar]
- 113.Selvin E, Bolen S, Yeh HC, Wiley C, Wilson LM, Marinopoulos SS, et al. Cardiovascular outcomes in trials of oral diabetes medications: A systematic review. Arch Intern Med. 2008;168:2070–80. doi: 10.1001/archinte.168.19.2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Simpson SH, Lee J, Choi S, Vandermeer B, Abdelmoneim AS, Featherstone TR. Mortality risk among sulfonylureas: A systematic review and network meta-analysis. Lancet Diabetes Endocrinol. 2015;3:43–51. doi: 10.1016/S2213-8587(14)70213-X. [DOI] [PubMed] [Google Scholar]
- 115.Monami M, Genovese S, Mannucci E. Cardiovascular safety of sulfonylureas: A meta-analysis of randomized clinical trials. Diabetes Obes Metab. 2013;15:938–53. doi: 10.1111/dom.12116. [DOI] [PubMed] [Google Scholar]
- 116.Sadikot SM, Mogensen CE. Risk of coronary artery disease associated with initial sulphonylurea treatment of patients with type 2 diabetes: A matched case-control study. Diabetes Res Clin Pract. 2008;82:391–5. doi: 10.1016/j.diabres.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 117.Zoungas S, de Galan BE, Ninomiya T, Grobbee D, Hamet P, Heller S, et al. Combined effects of routine blood pressure lowering and intensive glucose control on macrovascular and microvascular outcomes in patients with type 2 diabetes: New results from the ADVANCE trial. Diabetes Care. 2009;32:2068–74. doi: 10.2337/dc09-0959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Klepzig H, Kober G, Matter C, Luus H, Schneider H, Boedeker KH, et al. Sulfonylureas and ischaemic preconditioning; a double-blind, placebo-controlled evaluation of glimepiride and glibenclamide. Eur Heart J. 1999;20:439–46. doi: 10.1053/euhj.1998.1242. [DOI] [PubMed] [Google Scholar]
- 119.Zeller M, Danchin N, Simon D, Vahanian A, Lorgis L, Cottin Y, et al. Impact of type of preadmission sulfonylureas on mortality and cardiovascular outcomes in diabetic patients with acute myocardial infarction. J Clin Endocrinol Metab. 2010;95:4993–5002. doi: 10.1210/jc.2010-0449. [DOI] [PubMed] [Google Scholar]
- 120.Geisen K. Special pharmacology of the new sulfonylurea glimepiride. Arzneimittelforschung. 1988;38:1120–30. [PubMed] [Google Scholar]
- 121.Raptis SA, Hatziagelaki E, Dimitriadis G, Draeger KE, Pfeiffer C, Raptis AE. Comparative effects of glimepiride and glibenclamide on blood glucose, C-peptide and insulin concentrations in the fasting and postprandial state in normal man. Exp Clin Endocrinol Diabetes. 1999;107:350–5. doi: 10.1055/s-0029-1212125. [DOI] [PubMed] [Google Scholar]
- 122.Kar P, Holt RI. The effect of sulphonylureas on the microvascular and macrovascular complications of diabetes. Cardiovasc Drugs Ther. 2008;22:207–13. doi: 10.1007/s10557-008-6090-2. [DOI] [PubMed] [Google Scholar]
- 123.Roumie CL, Hung AM, Greevy RA, Grijalva CG, Liu X, Murff HJ, et al. Comparative effectiveness of sulfonylurea and metformin monotherapy on cardiovascular events in type 2 diabetes mellitus: A cohort study. Ann Intern Med. 2012;157:601–10. doi: 10.7326/0003-4819-157-9-201211060-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Pantalone KM, Kattan MW, Yu C, Wells BJ, Arrigain S, Jain A, et al. Increase in overall mortality risk in patients with type 2 diabetes receiving glipizide, glyburide or glimepiride monotherapy versus metformin: A retrospective analysis. Diabetes Obes Metab. 2012;14:803–9. doi: 10.1111/j.1463-1326.2012.01604.x. [DOI] [PubMed] [Google Scholar]
- 125.Tzoulaki I, Molokhia M, Curcin V, Little MP, Millett CJ, Ng A, et al. Risk of cardiovascular disease and all cause mortality among patients with type 2 diabetes prescribed oral antidiabetes drugs: Retrospective cohort study using UK general practice research database. BMJ. 2009:339–b4731. doi: 10.1136/bmj.b4731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Schramm TK, Gislason GH, Vaag A, Rasmussen JN, Folke F, Hansen ML, et al. Mortality and cardiovascular risk associated with different insulin secretagogues compared with metformin in type 2 diabetes, with or without a previous myocardial infarction: A nationwide study. Eur Heart J. 2011;32:1900–8. doi: 10.1093/eurheartj/ehr077. [DOI] [PubMed] [Google Scholar]
- 127.Johnson JA, Majumdar SR, Simpson SH, Toth EL. Decreased mortality associated with the use of metformin compared with sulfonylurea monotherapy in type 2 diabetes. Diabetes Care. 2002;25:2244–8. doi: 10.2337/diacare.25.12.2244. [DOI] [PubMed] [Google Scholar]
- 128.White JR, Campbell RK. Medications for the Treatment of Diabetes. Montvale NJ: American Diabetes Association/Thomson Reuters; 2008. Overview of medications used to treat type 2 diabetes; pp. 5–15. [Google Scholar]
- 129.Makkar BM, Gupta D, Gainda A. API Medicine. Ch. 87. Mumbai: Jaypee Brothers; 2013. Clinical Trials to Clinical Practice: Role of Sulfonylureas in Todayf's Practice; pp. 393–8. [Google Scholar]
- 130.Bolen S, Feldman L, Vassy J, Wilson L, Yeh HC, Marinopoulos S, et al. Systematic review: Comparative effectiveness and safety of oral medications for type 2 diabetes mellitus. Ann Intern Med. 2007;147:386–99. doi: 10.7326/0003-4819-147-6-200709180-00178. [DOI] [PubMed] [Google Scholar]
- 131.Naidoo P, Rambiritch V, Butkow N, Saman S. Optimal utilisation of sulphonylureas in resource-constrained settings. Cardiovasc J Afr. 2014;25:83–5. doi: 10.5830/CVJA-2014-007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kabadi UM. Cost-effective management of hyperglycemia in patients with type 2 diabetes using oral agents. Manag Care. 2004;13:48–9. 53-6, 58-9. [PubMed] [Google Scholar]
- 133.Zhang Y, McCoy RG, Mason JE, Smith SA, Shah ND, Denton BT. Second-line agents for glycemic control for type 2 diabetes: Are newer agents better? Diabetes Care. 2014;37:1338–45. doi: 10.2337/dc13-1901. [DOI] [PubMed] [Google Scholar]
- 134.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 135.Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23:1296–310. doi: 10.1016/s0149-2918(01)80109-0. [DOI] [PubMed] [Google Scholar]
- 136.Meece J. Improving medication adherence among patients with type 2 diabetes. J Pharm Pract. 2014;27:187–94. doi: 10.1177/0897190013513803. [DOI] [PubMed] [Google Scholar]
- 137.Pan F, Chernew ME, Fendrick AM. Impact of fixed-dose combination drugs on adherence to prescription medications. J Gen Intern Med. 2008;23:611–4. doi: 10.1007/s11606-008-0544-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Treatment adherence: Can fixed-dose combinations help? Lancet Diabetes Endocrinol. 2015:3–91. doi: 10.1016/S2213-8587(15)70011-2. [DOI] [PubMed] [Google Scholar]
- 139.Thayer S, Arondekar B, Harley C, Darkow TE. Adherence to a fixed-dose combination of rosiglitazone/glimepiride in subjects switching from monotherapy or dual therapy with a thiazolidinedione and/or a sulfonylurea. Ann Pharmacother. 2010;44:791–9. doi: 10.1345/aph.1M426. [DOI] [PubMed] [Google Scholar]
- 140.Kim HS, Kim DM, Cha BS, Park TS, Kim KA, Kim DL, et al. Efficacy of glimepiride/metformin fixed-dose combination vs metformin uptitration in type 2 diabetic patients inadequately controlled on low-dose metformin monotherapy: A randomized, open label, parallel group, multicenter study in Korea. J Diabetes Investig. 2014;5:701–8. doi: 10.1111/jdi.12201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Hiroi S, Sugiura K, Matsuno K, Hirayama M, Kuriyama K, Kaku K, et al. A multicenter, phase III evaluation of the efficacy and safety of a new fixed-dose pioglitazone/glimepiride combination tablet in Japanese patients with type 2 diabetes. Diabetes Technol Ther. 2013;15:158–65. doi: 10.1089/dia.2012.0246. [DOI] [PubMed] [Google Scholar]
- 142.Kalra S. Aggressive treatment in newly diagnosed diabetes with fixed dose combinations. [Last accessed on 2015 Apr 01];API Med Update. 2012 22:249–53. Available from: http://www.apiindia.org/pdf/medicine_update_2012/diabetology_04.pdf . [Google Scholar]
- 143.Pareek A, Chandurkar N, Zawar S, Agrawal N. Evaluation of efficacy and tolerability of gliclazide and metformin combination: A multicentric study in patients with type 2 diabetes mellitus uncontrolled on monotherapy with sulfonylurea or metformin. Am J Ther. 2010;17:559–65. doi: 10.1097/MJT.0b013e3181c6c0f9. [DOI] [PubMed] [Google Scholar]
- 144.Kalra S, Gupta Y. Sulfonylureas. J Pak Med Assoc. 2015;65:101–4. [PubMed] [Google Scholar]
- 145.Glyade: Gliclazide Tablets: Label Information of TGA. [Last accessed on 2015 Mar 25]. Available from: http://www.medicines.org.au/files/afpglyad.pdf .
- 146.Diabeta: Glyburide Tablets. Label Information of FDA. [Last accessed on 2015 Mar 25]. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/017532Orig1s034lbl.pdf .
- 147.Amaryl: Glimepiride Tablets. Label Information of FDA. [Last accessed on 2015 Mar 25]. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/020496s027lbl.pdf .
- 148.Langer O, Conway DL, Berkus MD, Xenakis EM, Gonzales O. A comparison of glyburide and insulin in women with gestational diabetes mellitus. N Engl J Med. 2000;343:1134–8. doi: 10.1056/NEJM200010193431601. [DOI] [PubMed] [Google Scholar]
- 149.Bertini AM, Silva JC, Taborda W, Becker F, Lemos Bebber FR, Zucco Viesi JM, et al. Perinatal outcomes and the use of oral hypoglycemic agents. J Perinat Med. 2005;33:519–23. doi: 10.1515/JPM.2005.092. [DOI] [PubMed] [Google Scholar]
- 150.Gottschalk M, Danne T, Vlajnic A, Cara JF. Glimepiride versus metformin as monotherapy in pediatric patients with type 2 diabetes: A randomized, single-blind comparative study. Diabetes Care. 2007;30:790–4. doi: 10.2337/dc06-1554. [DOI] [PubMed] [Google Scholar]
- 151.Benaji B, Mounib N, Roky R, Aadil N, Houti IE, Moussamih S, et al. Diabetes and Ramadan: Review of the literature. Diabetes Res Clin Pract. 2006;73:117–25. doi: 10.1016/j.diabres.2005.10.028. [DOI] [PubMed] [Google Scholar]
- 152.Fariduddin M, Mahtab H, Latif ZA, Siddiqui NI. Practical management of diabetes during Ramadan fasting. Mymensingh Med J. 2011;20:541–6. [PubMed] [Google Scholar]
- 153.Glimepiride in Ramadan (GLIRA) Study Group. The efficacy and safety of glimepiride in the management of type 2 diabetes in Muslim patients during Ramadan. Diabetes Care. 2005;28:421–2. doi: 10.2337/diacare.28.2.421. [DOI] [PubMed] [Google Scholar]
- 154.Zargar AH, Siraj M, Jawa AA, Hasan M, Mahtab H. Maintenance of glycaemic control with the evening administration of a long acting sulphonylurea in male type 2 diabetic patients undertaking the Ramadan fast. Int J Clin Pract. 2010;64:1090–4. doi: 10.1111/j.1742-1241.2009.02262.x. [DOI] [PubMed] [Google Scholar]
- 155.Bashir MI, Pathan MF, Raza SA, Ahmad J, Khan AK, Ishtiaq O, et al. Role of oral hypoglycemic agents in the management of type 2 diabetes mellitus during Ramadan. Indian J Endocrinol Metab. 2012;16:503–7. doi: 10.4103/2230-8210.97994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Rendell M. The role of sulphonylureas in the management of type 2 diabetes mellitus. Drugs. 2004;64:1339–58. doi: 10.2165/00003495-200464120-00006. [DOI] [PubMed] [Google Scholar]
- 157.Glucotrol: Glipizide Tablets. Label Information of FDA. [Last accessed on 2015 Mar 25]. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/017783s025lbl.pdf .
- 158.Scheen AJ. Pharmacokinetic and toxicological considerations for the treatment of diabetes in patients with liver disease. Expert Opin Drug Metab Toxicol. 2014;10:839–57. doi: 10.1517/17425255.2014.902444. [DOI] [PubMed] [Google Scholar]
- 159.Wosilait WD. An analysis of the effect of hypoalbuminemia on the amount of free drug in plasma for drugs bound at two sets of sites. Res Commun Chem Pathol Pharmacol. 1974;9:681–8. [PubMed] [Google Scholar]
- 160.Khan R, Foster GR, Chowdhury TA. Managing diabetes in patients with chronic liver disease. Postgrad Med. 2012;124:130–7. doi: 10.3810/pgm.2012.07.2574. [DOI] [PubMed] [Google Scholar]
- 161.Campbell I. Sulfonylureas and hypoglycemia. Diabet Hypoglycemia. 2009;2:3–10. [Google Scholar]
- 162.Yabe D, Seino Y. Dipeptidyl peptidase-4 inhibitors and sulfonylureas for type 2 diabetes: Friend or foe? J Diabetes Investig. 2014;5:475–7. doi: 10.1111/jdi.12229. [DOI] [PMC free article] [PubMed] [Google Scholar]