Abstract
Aim:
The prevalence and associated risk factors of metabolic syndrome (MS) among adults over 18 years old in Jaffna district.
Materials and Methods:
It was community-based cross-sectional descriptive study. Multistage stratified cluster sampling technique was employed. An interviewer administered questionnaire was used to obtain the relevant information. Waist circumference (WC) and blood pressure (BP) measurements were recorded. Fasting plasma glucose (FPG), high-density lipoprotein (HDL), and triacylglycerols were analyzed by the enzymatic colorimetric assay using semi-automated analyzer (Teco Diagnostics TC-3300). International Diabetic Federation guideline for Asians was used to identify MS.
Results:
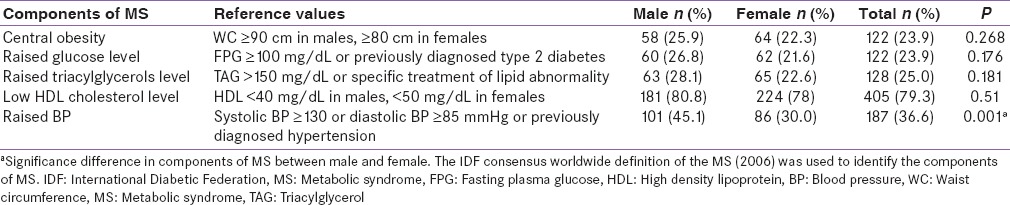
Sample response rate was 95.3% and of them, 43.8% (n = 224) was male. The prevalence of central obesity (WC for male ≥90 cm, female ≥80 cm) was 23.9%. Raised FPG (≥100 mg/dL, or previously diagnosed diabetes mellitus), hypertriacylglycerolemia (≥150 mg/dl), low level of HDL cholesterol (<40 mg/dL in males, <50 mg/dL in females), and raised BP (systolic BP ≥130 or diastolic BP ≥85 mmHg or previously diagnosed hypertension) were found in 23.9%, 25%, 79.3%, and 36.6% of the participants. The prevalence of MS was 15.8% (95% confidence interval [CI]: 12.8–19.3) and it was 17.4% in males and 14.6% in females. Participants living in the urban area had a higher prevalence of MS when compared with participants in a rural area (P = 0.015). Older age (P < 0.001) was a risk factor for development of MS. Smoking (P = 0.005) was a risk factor for the development of MS. Participants having sedentary, moderately active, and highly active lifestyle had the prevalence of MS 20.6% (95% CI: 13.2–29.7), 14.7% (95% CI: 10.6–19.5), and 14.7% (95% CI: 9.3–21.6), respectively (P = 0.247).
Conclusion:
Older age, urban living, and smoking carry a higher risk for development of MS among Jaffna Tamil community.
Keywords: Central obesity, fasting plasma glucose, high-density lipoprotein, hypertriacylglycerolemia, Jaffna, metabolic syndrome, Sri Lanka
INTRODUCTION
Metabolic syndrome (MS) is known as the clustering of several metabolic abnormalities; centrally distributed obesity, low level of high density lipoprotein (HDL) cholesterol, elevated triacylglycerols (TAGs), high blood pressure (BP), and hyperglycemia.[1] There is an increasing tendency of MS among people in the developing countries.[2] Identification of risk factors for the development of diabetes and cardiovascular diseases (CVDs) has consistently implicated four key components namely increased adiposity, disturbed glucose metabolism, dyslipidemia, and hypertension.[3] Identifying subjects with MS would help to prevent the increasing morbidity and mortality due to type 2 diabetes mellitus and CVD in Jaffna district, Sri Lanka. The prevalence of MS in Jaffna district has not been reported yet due to the inaccessibility of area during the three decades-long civil war. Therefore, this study was undertaken to determine the prevalence and factors associated with MS among adults in Jaffna district, Sri Lanka.
MATERIALS AND METHODS
This was a community-based cross-sectional descriptive study among adults (above 18 years). A multistage stratified cluster sampling was used to obtain a sample that represents the adult population of the Jaffna district. Totally, calculated the sample size was 544. The first stage of sampling the population in the Jaffna district was stratified into urban and rural sectors. The 32 clusters were allocated by probability proportion to the size of the population in each sector. Considering the proportion of the population, 7 and 25 clusters were selected from the urban and rural sectors, respectively. Seventeen individuals were included in a cluster, so that the required sample size of 544 was scattered in 32 clusters. An updated list of households was available with the Grama Niladhari officer. A household was randomly selected from this list in each of the clusters. In the field, the randomly selected house was located and visited as the first house. Next house to be visited was the one closest to the right side of the front door of the first house. This procedure was repeated until the required number of respondents was interviewed in each cluster. In every house visited, all eligible males and females above 18 years were listed on the summary form. The person to be interviewed was selected randomly using lottery method. This ensured that the sex ratio of the study population.
Ethical clearance was obtained from the Ethical Review Committee, Faculty of Medicine, University of Jaffna. Written consent was obtained from individual participants.
An interviewer administrated questionnaire was employed to collect relevant information. The age was categorized as 18–34, 35–49, 50–64, and ≥65 years. Physical activity level was classified into three categories namely insufficiently active (no activity is reported/some activity is reported but not enough to meet categories of sufficiently active or highly active), sufficiently active (≥600 metabolic equivalent of task (MET)-min/week) and highly active (≥3,000 MET-min/week) using the International physical activity questionnaire, which was translated into Tamil and pretested in the preliminary study. Waist circumference was taken by positioning the nonelastic measuring tape midway between the lower rib margin and the iliac crest, at the end of a normal expiration to the nearest 0.5 cm. BP was measured in the seated position after the participants had rested for at least 5 min. The measurement was taken using the supported left arm at the heart level, using sphygmomanometer. Two recordings were taken, and the average was used for analysis. In the event of variation of over 20 mmHg between recordings, a third reading was taken, and the average of the last two recordings was used. Fasting plasma glucose (FPG), HDL cholesterol, and triacylglycerols were analyzed by the enzymatic colorimetric assay using the semi-automated analyzer (Teco Diagnostics TC-3300). The Chi-square test and simple linear regression were performed on data using the SPSS version 16 statistical package (SPSS South Asia Pvt Ltd., Kacharakanahalli). The probability level was set as P < 0.05.
RESULTS
The sample response rate was 95.3% and among the subjects, 43.8% (n = 224) was male. Prevalence of central obesity was 23.9%. In the study population, 23.9%, 25%, and 79.3% of the participants had raised FPG, raised triglycerides, and low HDL cholesterol levels [Table 1]. The prevalence of MS was 15.8% (n = 81, 95% confidence interval [CI]: 12.8–19.3) and it was 17.4% (95% CI: 12.7–23.0) among males and 14.6% (95% CI: 10.8–19.3) among females. However, gender was not significantly associated with MS (P = 0.394). In this study, 14.2% of the participants selected from the rural area had MS; whereas 19.6% of the participants selected from the urban area had MS. Females living in the urban area had a higher prevalence of MS than those living in the rural area (23.7% vs. 12.3%). A similar observation was also made among males (18.1% vs. 15.5%). In females, there was statistically significant association between the sector and MS (P = 0.007).
Table 1.
Components of MS in the study population stratified by gender
Association between the sector and MS was marginally significant in the model unadjusted for the gender (P = 0.059). Therefore, gender seemed to be confounding the effect of the sector on MS. Mean age of the selected participants was 45.6 (±14.4) years, whereas the mean age of participants with MS was 55.6 (±13.2) years. Prevalence of MS was 6.0%, 8.0%, 21.1%, and 47.3% in the age groups of 18–34, 35–49, 50–64, and above 65 years, respectively. Older age was a risk for developing MS among the Jaffna population (P < 0.0001). Participants within different age groups had a statistically significant relationship in developing MS both in males (P = 0.045) and females (P < 0.001). There was a statistically significant positive linear relationship between the categories of age and the MS in the total population (R2 = 91.9%), in males (R2 = 80.4%) and in females (R2 = 95.2%).
The prevalence of MS was 29.1% and 14.3% among the smokers and the nonsmokers, respectively. Smoking was found to be a risk factor for the development of MS (P = 0.007). There was no statistically significant difference in the prevalence of MS (21.1%, 95% CI: 11.9–33.7) among the alcohol consumers and (15.1%, 95% CI: 11.9–18.8) among the nonalcohol consumers (P = 0.213). Participants having sedentary, moderately active, and highly active lifestyle had the prevalence of MS 20.6% (95% CI: 13.2–29.7), 14.7% (95% CI: 10.6–19.5), and 14.7% (95% CI: 9.3–21.6), respectively (P = 0.247).
DISCUSSION
In the study population, the prevalence of MS was 15.8% (95% CI: 12.8–19.3). There was no gender difference. In the rest of population in Sri Lanka, crude prevalence of MS was 27.1% (95% CI: 25.8–28.5), and age-adjusted prevalence was 24.3% (95% CI: 23.0–25.6). The prevalence in males and females was 18.4 and 28.3%, respectively.[4] These differences could be due to different cultural practices prevailing in the Jaffna and rest of the country. Misra and Shrivastava suggested that cultural and social restrictions on outdoor physical activity in women in South Asian countries might be an important reason for increasing obesity and the MS.[5]
Prevalence estimate for MS, in the present study, was more or less similar to Korea (19.5%), Singapore (17.7%), China (16.3%), and Taiwan (13.9%); and higher than that of Japanese (7.8%), and lower than nationwide study in Malaysia (37.1%), USA (39%), and Greece (43.4%).[3] A study conducted in urban areas of Karachi and Pakistan showed a high prevalence of MS, 34.8 and 49%, respectively. According to the International Diabetic Federation definition and modified National Cholesterol Education Program, Adult Treatment Panel III criteria, respectively.[6] In a recent community-based study from eastern India, estimated the prevalence of MS was 31.4% and it was a much higher among the females (48.2%) than the males (16.3%).[7]
In this study, 14.2% of subjects from a rural area and 19.6% of the subjects from the urban area had MS. Females living in the urban area had a higher proportion of MS than those living in the rural area (23.7% vs. 12.3%). A similar observation was also made among males (18.1% vs. 15.5%). Katulanda et al. observed a similar distribution in other regions of the country.[4] MS was more prevalent among urban dwellers in India too.[3] Surveys in large cities in different parts of the country suggest that about one-third of the urban population in large cities in India had MS.[8] The underlying reasons are obvious, urbanization which exposes people to a number of challenges, imbalanced diets, physical inactivity, long working hours, and other urban stress making them vulnerable to noncommunicable diseases.[5]
According to the present study, MS was more prevalent to be among the people who are more than 50 years. This is compatible with the findings of the previous study which was done in other parts of Sri Lanka.[4] Old age was identified as a risk factor for the development of MS in the study population (P < 0.0001) and also there was a statistically significant positive linear relationship between the categories of age and the MS in the total population (R2 = 91.9%), in males (R2 = 80.4%) and in females (R2 = 95.2%). The adipose deposition could be increased with aging. It may lead to insulin resistance and higher LDL-cholesterol, triacylglycerols, blood glucose, and BP. Geriatric changes in the body systems may invariably contribute to this association.
The prevalence of MS was 29.1% and 14.3% among the smokers and the nonsmokers, respectively. Smoking is a risk factor for the development of MS (P = 0.007). It is inconsistent with findings of many studies in which cigarette smoking was identified as independent risk factor for MS.[9,10,11] In view of smoking could accelerate visceral fat accumulation and promote obesity-related disorders. Nicotine, carbon monoxide, and other metabolites from smoking also play an important role in insulin resistance. Indeed, several studies in the past have shown that nicotine leads to insulin resistance, has an antiestrogenic effect and increases the level of stress hormones like cortisol.[11,12] This different observation could be due to the small sample size in each group of the frequency of smoking in the present study.
The prevalence of MS was 21.1% among the alcohol consumers and 15.1% among the participants who did not consume alcohol. Heavy alcohol consumption was associated with an increased risk of the MS by influencing its components.[13] In contrast to the present study, in another study, males who never consumed alcohol had the highest prevalence of MS (12.3%).[4] Participants with sedentary lifestyle had the highest prevalence of MS (20.6%) than moderately active (14.7%) and highly active (14.7%) participants. Sedentary lifestyle compounded with the change in the nutritional pattern in Jaffna population makes them more vulnerable to noncommunicable diseases. Regular exercise could increase energy expenditure and achieve weight loss and increase insulin sensitivity. Exercise could reduce BP, increase HDL cholesterol, and lower triacylglycerols levels. However, determinants of physical inactivity in South Asians have not yet been systematically studied.[5]
CONCLUSION
Older age, urban living, and smoking carry a higher risk for development of MS among Jaffna Tamil community.
Financial support and sponsorship
National Research Council (NRC), Sri Lanka, grant no: 13-122.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This research was supported by the National Research Council (NRC), Sri Lanka, grant no: 13-122. Authors wished to thank NRC for granting the fund.
REFERENCES
- 1.Zimmet P, Alberti KG, Serrano Ríos M. A new international diabetes federation worldwide definition of the metabolic syndrome: The rationale and the results. Rev Esp Cardiol. 2005;58:1371–6. [PubMed] [Google Scholar]
- 2.Mohan V, Deepa M. The metabolic syndrome in developing countries. Diabetes Metab Syndr. 2006;51:15–7. [Google Scholar]
- 3.Pandit K, Goswami S, Ghosh S, Mukhopadhyay P, Chowdhury S. Metabolic syndrome in South Asians. Indian J Endocrinol Metab. 2012;16:44–55. doi: 10.4103/2230-8210.91187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Katulanda P, Ranasinghe P, Jayawardana R, Sheriff R, Matthews DR. Metabolic syndrome among Sri Lankan adults: Prevalence, patterns and correlates. Diabetol Metab Syndr. 2012:4–24. doi: 10.1186/1758-5996-4-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Misra A, Shrivastava U. Obesity and dyslipidemia in South Asians. Nutrients. 2013;5:2708–33. doi: 10.3390/nu5072708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hydrie MZ, Shera AS, Fawwad A, Basit A, Hussain A. Prevalence of metabolic syndrome in urban Pakistan (Karachi): Comparison of newly proposed international diabetes federation and modified adult treatment panel III criteria. Metab Syndr Relat Disord. 2009;7:119–24. doi: 10.1089/met.2008.0055. [DOI] [PubMed] [Google Scholar]
- 7.Das M, Pal S, Ghosh A. Association of metabolic syndrome with obesity measures, metabolic profiles, and intake of dietary fatty acids in people of Asian Indian origin. J Cardiovasc Dis Res. 2010;1:130–5. doi: 10.4103/0975-3583.70911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Misra A, Khurana L. Obesity and the metabolic syndrome in developing countries. J Clin Endocrinol Metab. 2008;93(11 Suppl 1):S9–30. doi: 10.1210/jc.2008-1595. [DOI] [PubMed] [Google Scholar]
- 9.Takeuchi T, Nakao M, Nomura K, Yano E. Association of metabolic syndrome with smoking and alcohol intake in Japanese men. Nicotine Tobacco Research. Oxf J. 2009;11:1093–8. doi: 10.1093/ntr/ntp106. [DOI] [PubMed] [Google Scholar]
- 10.Sun K, Liu J, Ning G. Active smoking and risk of metabolic syndrome: A meta-analysis of prospective studies. PLoS One. 2012;7 doi: 10.1371/journal.pone.0047791. e47791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chiolero A, Faeh D, Paccaud F, Cornuz J. Consequences of smoking for body weight, body fat distribution, and insulin resistance. Am J Clin Nutr. 2008;87:801–9. doi: 10.1093/ajcn/87.4.801. [DOI] [PubMed] [Google Scholar]
- 12.Cena H, Tesone A, Niniano R, Cerveri I, Roggi C, Turconi G. Prevalence rate of metabolic syndrome in a group of light and heavy smokers. Diabetol Metab Syndr. 2013:5–28. doi: 10.1186/1758-5996-5-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baik I, Shin C. Prospective study of alcohol consumption and metabolic syndrome. Am J Clin Nutr. 2008;87:1455–63. doi: 10.1093/ajcn/87.5.1455. [DOI] [PubMed] [Google Scholar]


