Abstract
Objectives. We designed this study to examine differences in receipt of mental health treatment between low-income uninsured nonelderly adults with serious mental illness (SMI) who were eligible for Medicaid under the Affordable Care Act (ACA) and their existing Medicaid counterparts. Assessing these differences might estimate the impact of the Medicaid expansion efforts under the ACA on receipt of mental health treatment among uninsured nonelderly adults with SMI.
Methods. We examined data from 2000 persons aged 18 to 64 years who participated in the 2008 to 2013 National Survey on Drug Use and Health, had income below 138% of the federal poverty level, met SMI criteria, and either were uninsured (n = 1000) or had Medicaid-only coverage (n = 1000). We defined SMI according to the Alcohol, Drug Abuse, and Mental Health Administration Reorganization Act. We used descriptive analyses and logistic regression modeling.
Results. In the 28 states currently expanding Medicaid, the model-adjusted prevalence (MAP) of receiving mental health treatment among Medicaid-only enrollees with SMI (MAP = 71.3%; 95% confidence interval [CI] = 65.74%, 76.29%) was 30.1% greater than their uninsured counterparts (MAP = 54.8%; 95% CI = 48.16%, 61.33%). In the United States, the MAP of receiving mental health treatment among Medicaid-only enrollees with SMI (MAP = 70.4%; 95% CI = 65.67%, 74.70%) was 35.9% higher than their uninsured counterparts (MAP = 51.8%; 95% CI = 46.98%, 56.65%).
Conclusions. Estimated increases in receipt of mental health treatment because of enrolling in Medicaid among low-income uninsured adults with SMI might help inform planning and implementation efforts for the Medicaid expansion under the ACA.
In accordance with the Alcohol, Drug Abuse, and Mental Health Administration Reorganization Act of 1992, the Substance Abuse and Mental Health Services Administration defines serious mental illness (SMI) among adults as a mental disorder (excluding developmental and substance use disorders) that results in serious functional impairment that substantially interferes with or limits 1 or more major life activities.1–3 In 2012, among adults aged 18 years or older in the United States, approximately 4.1% (9.6 million) had SMI.1 Among these adults with SMI, 62.9% received mental health treatment in 2012.1 Adults with untreated SMI are at increased risk for diminished quality of life, co-occurring substance use disorders and medical conditions, hospitalization, involvement with criminal justice, shortened life expectancy, and suicide.4–7
SMI is also associated with poverty.8,9 Adults with SMI are often uninsured or enrolled in Medicaid.1,8 If they are uninsured, they may receive treatment through state and local government funding and the Community Mental Health Services Block Grant. Medicaid, which covers the remaining poor with SMI, is the largest source of financing for mental health treatment.3 Among adults with SMI who did not receive mental health treatment, but perceived a need for treatment in 2012, 70.7% reported that they could not afford the cost.10 The Patient Protection and Affordable Care Act (ACA) of 2010,11 which gives states the option of extending Medicaid coverage to uninsured adults younger than 65 years (nonelderly adults) whose family income is below 138% of the federal poverty level defined by the US Department of Health and Human Services12 (“low-income”), is expected to cover eligible low-income uninsured nonelderly adults with Medicaid.
Using the Kessler-6 (K6) distress scale1 and 2-item Patient Health Questionnaire, 1 study reported that approximately 0.9 million adult Medicaid enrollees with serious psychological distress or depression would also use mental health services under the ACA’s Medicaid expansion.13 However, that study has 3 major limitations. First, the 2 measures neither directly assessed the presence of a diagnosable mental disorder based on the criteria specified in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) nor captured functional impairment.14,15 Second, it controlled for census region and metropolitan statistical area, but did not consider the differences in Medicaid benefit packages across states that may influence Medicaid enrollment rates under the ACA’s Medicaid expansion.16 Third, that study did not adjust for the accessibility of mental health treatment at the county level and might overestimate the ACA impact. For example, 80% of US counties in 2008 were designated as Mental Health Professional Shortage Areas, and more than one third of counties did not have outpatient mental health facilities that accepted Medicaid.17
Importantly, 27 states (and the District of Columbia) are currently expanding Medicaid under the ACA.18 The potential changes for receipt of mental health treatment, once low-income uninsured adults with SMI are enrolled in Medicaid under the ACA, are unknown in these 28 states. Little is known about the potential changes in receipt of mental health treatment in the United States as a whole, if all of the states eventually move forward with Medicaid expansion. Understanding these changes will help inform planning and implementation efforts for the Medicaid expansion under the ACA and better meet mental health treatment needs among new Medicaid enrollees with SMI.
We examined differences in the receipt of mental health treatment between low-income uninsured nonelderly adults with SMI and their Medicaid counterparts in these 28 states and in United States as a whole, while adjusting for their sociodemographic factors, health status, perceived unmet need for mental health treatment, severity of mental illness, differences in Medicaid benefit packages across states, and accessibility of mental health treatment at the county level. We used the SMI definition according to the 1992 Alcohol, Drug, and Mental Health Administration Reorganization Act. This definition was used for distributing the Community Mental Health Services Block Grant and as one of the conditions determining Medicaid eligibility across states. Because SMI is often undiagnosed and untreated among low-income adults, we did not rely on existing mental health diagnoses that are conditional on health insurance or health care utilization.8,13,19 Using state and nationally representative survey data that assess SMI in the 28 states and the United States as a whole, we tested the following hypotheses: (1) in the 28 states (currently expanding Medicaid), the model-adjusted prevalence (MAP) of receiving mental health treatment in the past year among Medicaid-only enrollees with SMI was significantly greater than their uninsured counterparts; and (2) in the United States (if all states eventually move forward with Medicaid expansion), the MAP of receiving mental health treatment in the past year among Medicaid-only enrollees with SMI was significantly higher than their uninsured counterparts.
METHODS
The only existing data source meeting all of our study criteria was the National Survey on Drug Use and Health (NSDUH). We first examined data from 3200 sampled persons ages 18 to 64 years who participated in the 2008 to 2013 NSDUH, who had family income less than 138% of federal poverty level (based on family income, size, composition [e.g., number of children], and respondent’s age),1,20 who met the criteria for having SMI in the past year, and who were either uninsured (n = 1400) or covered by Medicaid-only (n = 1800) at the time of survey interview.
NSDUH is conducted by the Substance Abuse and Mental Health Services Administration and provides nationally and state representative data on SMI among the civilian, noninstitutionalized population aged 18 years or older. Persons without a household address (e.g., homeless persons not in a shelter), active duty military personnel, and residents of institutional group quarters (e.g., hospitals, nursing homes, or prisons) are excluded from the survey.1,20 However, NSDUH covers homeless persons who lived in shelters at the time of survey interview and includes adults who were institutionalized sometime during the past year and were discharged from the institution at the time of survey interview. The Substance Abuse and Mental Health Services Administration requires that any description of overall sample sizes based on the restricted-use data files has to be rounded to the nearest 100 to minimize potential disclosure risk.
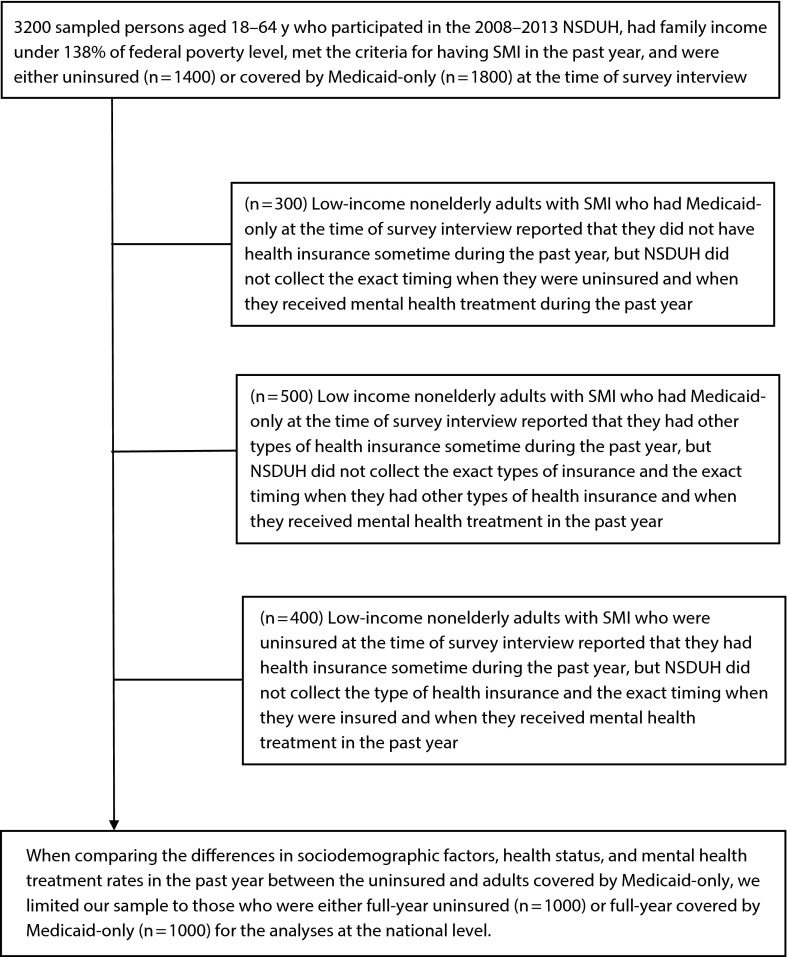
Because we examined potential changes in seeking mental health treatment because of switching from being uninsured to Medicaid under the ACA, and because issues related to continuous insurance coverage were common among the uninsured and unstably insured,21 we excluded certain respondents from the bivariate and multivariable analyses to reduce potential biases (Figure 1). If respondents reported having no health insurance at the time of survey interview and reported that it had been more than 1 year since they last had any kind of health insurance, they were considered as “full-year uninsured.” If respondents reported having Medicaid-only at the survey interview and reported having continuous insurance coverage over the past 12 months, they were considered as having “full-year Medicaid-only” coverage. We limited our sample to those who were either full-year uninsured (n = 1000) or full-year covered by Medicaid-only (n = 1000) for the analyses at the national level. For similar analyses related to the 28 states, we limited our sample to those who were either full-year uninsured (n = 500) or were full-year covered by Medicaid-only (n = 700).
FIGURE 1—
Flowchart showing the number of individuals excluded through each of the criteria and providing the corresponding rationale.
Note. NSDUH = National Survey on Drug Use and Health; SMI = serious mental illness. Federal poverty level is defined by the US Department of Health and Human Services.12
To control for the impact of accessibility of mental health treatment on mental health treatment seeking, we used Federal Information Processing Standard state and county codes and linked the 2008 to 2013 NSDUH to the 2010 National Mental Health Services Survey data at the aggregated county level and linked to the 2011 Area Health Resources Files at the county level. The 2010 National Mental Health Services Survey is the most recent data set available on all known US public and private facilities providing mental health treatment to persons with mental illness.22 The 2011 Area Health Resources Files are the most recent files with earlier years of data, including health workforce data for every US county.23
Measures
Serious mental illness.
NSDUH defines SMI among adults aged 18 years or older as currently or at any time in the past year having had a mental disorder (excluding developmental disorders and substance use disorders) of sufficient duration to meet diagnostic criteria specified within the DSM-IV,24 that resulted in serious functional impairment substantially interfering with or limiting 1 or more major life activities. This SMI definition is consistent with the Alcohol, Drug Abuse, and Mental Health Administration Reorganization Act of 1992.
To generate estimates of SMI in the United States, the Substance Abuse and Mental Health Services Administration and the National Institute of Mental Health implemented the Mental Health Surveillance Study. In the Mental Health Surveillance Study, 5700 NSDUH sampled adults participated in a follow-up telephone interview by a trained mental health clinician using the Structured Clinical Interview for DSM-IV-TR Axis I Disorders. Using the data collected by the Mental Health Surveillance Study, a model was developed to predict SMI based on questions on psychological distress (past-year K6 scale), impairment (truncated version of the World Health Organization Disability Assessment Schedule), serious suicidal ideation, major depressive episode, and age.14,15 Then using this prediction model, past-year SMI status (yes/no) and the predicted probability of having SMI (a continuous score) were determined for each respondent in the NSDUH adult samples. We used the binary SMI variable to identify those with SMI and the continuous SMI variable to control for the severity of mental illness.
Data from the Mental Health Surveillance Study showed that this SMI prediction model had a sensitivity of 0.51 and a specificity of 0.98 in predicting SMI. Compared with the K6, which predicted SMI in an earlier study,25 this SMI model showed a higher sensitivity value and a similar specificity value, reduced the differences between clinical sample estimates and the model-based estimate, and improved the face validity (by including the functional impairment variable).26
Receipt of mental health treatment.
NSDUH asked all adult respondents to report the receipt of outpatient or inpatient mental health treatment or receipt of prescription medication for mental health problems in the past year.
Sociodemographic characteristics.
We examined age, gender, race/ethnicity, education status, marital status, employment status, metropolitan statistical area, and region. Because Medicaid benefit packages vary considerably across states, we also assessed “state” in our analyses to control for variations across states.
States currently expanding Medicaid.
We created a variable indicating whether the state where the respondent resides was expanding Medicaid (yes/no). States coded “yes” included Arizona, Arkansas, California, Colorado, Connecticut, Delaware, District of Columbia, Hawaii, Illinois, Iowa, Kentucky, Maryland, Massachusetts, Michigan, Minnesota, Nevada, New Jersey, New Hampshire, New Mexico, New York, North Dakota, Ohio, Oregon, Pennsylvania, Rhode Island, Vermont, Washington, and West Virginia.18
Health status.
NSDUH asked adult respondents if they were told by doctors or other health professionals that they had hypertension, heart disease, diabetes, stroke, asthma, and HIV/AIDS during their lifetime. NSDUH captured a respondent’s self-rated health and the number of past 12-month emergency room visits (for any reason). NSDUH assessed whether respondents had past 12-month substance use disorders (alcohol use disorders only, illicit drug use disorders, both alcohol use and illicit drug use disorders, or none) according to the DSM-IV criteria.24
Unmet need for mental health treatment.
NSDUH asked all respondents whether they perceived unmet needs for mental health treatment any time in the 12 months before the survey interview (yes/no).
Variables from the National Mental Health Services Survey as potential covariates.
Similar to a study17 that examined the number of outpatient mental health facilities that accept Medicaid in the county per 10 000 Medicaid enrollees, we assessed the number of facilities that accepted Medicaid per 10 000 county Medicaid enrollees and per 10 000 county residents for the following measures: the number of facilities that received the Community Mental Health Services Block Grant, the number of facilities that received state mental health agency funds, the number of facilities that received local government funds, the number of facilities that had designated programs for adults with SMI, and the number of facilities that offered cognitive or behavioral therapy.
Variables from the Area Health Resources Files as potential covariates.
We examined the following measures per 10 000 county residents: the number of persons at or under the federal poverty level, the number of federal-qualified health centers, the number of community mental health centers, the number of licensed psychologists, the number of office-based psychiatrists, the number of hospital-based psychiatrists, the number of general hospitals with psychiatry care, and the number of psychiatric hospitals.
Data Analysis
First, we used the Wald F test to compare differences in sociodemographic characteristics, health status, and unadjusted prevalence of receiving mental health treatment between uninsured low-income adults with SMI who were potentially eligible for Medicaid under the ACA and their Medicaid counterparts in the 28 states and in the United States as a whole. Statistical significance in each point difference was assessed at P < .05 using a 2-tailed test. The Bonferroni correction was applied in the multiple bivariate comparisons.
Second, we applied multivariable logistic regression modeling to assess the MAP and prevalence difference (predicted marginal proportions, using PREDMARG and PRED_EFF statements in SUDAAN27,28) in receiving mental health treatment (yes/no) between low-income uninsured nonelderly adults with SMI and their Medicaid counterparts in the 28 states and the United States. After controlling for potential confounding factors, the difference in model-adjusted predicted marginal proportions provided an estimated change in probability of receiving mental health treatment because of the change in health insurance status, from being full-year uninsured to full-year enrolling in Medicaid-only. We tested potential interaction effects, particularly the interaction effect between state and insurance status (Medicaid-only or uninsured), and found no significant interactions on any outcomes. Using the variance inflation factors, multicollinearity was assessed during multivariable modeling and was not identified in the final multivariable models. All of our analyses used SUDAAN software27 to account for the complex sample design and sampling weights of the NSDUH.
RESULTS
Table 1 shows that in the United States, compared with their Medicaid counterparts, low-income uninsured nonelderly adults with SMI were more likely to be men, employed full-time, and reside in the South, but were less likely to be disabled for work and reside in the Northeast. Compared with their uninsured counterparts, Medicaid adults with SMI were more likely to have more than 2 emergency room visits in the past year. The uninsured were more likely to have zero emergency room visits in the past year than their Medicaid counterparts. The results for the 28 states were similar to the national findings.
TABLE 1—
Demographic Characteristics and Health Status Among US Adults With Serious Mental Illness Who Were Uninsured or Covered by Medicaid-Only: National Survey on Drug Use and Health, 2008–2013
| Demographic Characteristics and Health Status | Full-Year Uninsured (n = 1000), Weighted % (SE) | Full-Year Medicaid-Only (n = 1000), Weighted % (SE) | P for Point Difference |
| Age, y | |||
| 18–25 | 15.5 (1.16) | 12.7 (0.97) | .057 |
| 26–49 | 63.5 (2.47) | 65.4 (2.64) | .601 |
| 50–64 | 21.0 (2.52) | 21.9 (2.63) | .795 |
| Gender: male | 42.7 (2.38) | 24.2 (2.34) | < .001a |
| Race/ethnicity | |||
| Non-Hispanic White | 62.4 (2.50) | 60.3 (2.58) | .562 |
| Non-Hispanic Black | 13.4 (1.72) | 19.6 (2.16) | .027 |
| Non-Hispanic Asian | 1.7 (0.62) | 1.1 (0.45) | .414 |
| Non-Hispanic multiple races | 1.2 (0.36) | 2.2 (0.51) | .125 |
| Non-Hispanic other | 1.1 (0.34) | 2.0 (0.50) | .153 |
| Hispanic | 20.2 (2.19) | 14.8 (1.88) | .068 |
| Education | |||
| < high school | 31.0 (2.13) | 35.4 (2.55) | .189 |
| High school graduate | 35.2 (2.30) | 35.4 (2.42) | .94 |
| Some college | 27.9 (2.23) | 25.6 (2.34) | .495 |
| College graduate | 6.0 (1.02) | 3.6 (0.82) | .07 |
| Employment status | |||
| Full-time | 20.1 (1.79) | 7.7 (1.19) | < .001a |
| Part-time | 17.8 (1.87) | 12.3 (1.66) | .026 |
| Disabled for work | 21.1 (2.12) | 52.3 (2.42) | < .001a |
| Unemployed | 23.1 (2.16) | 13.6 (1.81) | .008 |
| Other | 17.8 (1.86) | 14.1 (1.44) | .116 |
| Marital status: married (yes/no) | 25.8 (2.27) | 21.81 (2.29) | .209 |
| Metropolitan statistical area: yes | 77.5 (2.11) | 78.5 (1.84) | .7 |
| Region | |||
| Northeast | 4.6 (0.88) | 22.4 (2.01) | < .001a |
| Midwest | 20.1 (1.77) | 24.9 (2.21) | .084 |
| South | 52.4 (2.39) | 30.4 (2.44) | < .001a |
| West | 22.9 (2.18) | 22.2 (2.40) | .83 |
| Self-rated health | |||
| Excellent | 8.0 (1.31) | 3.9 (0.78) | .007 |
| Very good | 16.0 (1.65) | 15.7 (1.75) | .891 |
| Good | 31.4 (2.25) | 25.2 (2.04) | .042 |
| Fair/poor | 44.6 (2.42) | 55.3 (2.40) | .002 |
| Medical conditions | |||
| Hypertension | 25.2 (2.39) | 27.7 (2.19) | .438 |
| Heart disease | 4.2 (1.08) | 5.9 (1.21) | .26 |
| Stroke | 2.5 (0.90) | 1.9 (0.64) | .611 |
| Diabetes | 9.3 (1.59) | 12.5 (1.66) | .164 |
| Asthma | 18.8 (2.00) | 26.6 (2.20) | .008 |
| HIV/AIDS | 0.2 (0.15) | 0.7 (0.30) | .18 |
| Any of the above medical conditions | 42.9 (2.56) | 50.0 (2.47) | .047 |
| ≥ 3 of the above medical conditions | 3.2 (0.98) | 5.5 (1.26) | .108 |
| Past-year emergency room visits for any treatment | |||
| 0 | 45.7 (2.36) | 30.3 (2.31) | < .001a |
| 1 | 20.9 (1.96) | 20.8 (2.13) | .968 |
| 2 | 13.7 (1.54) | 16.4 (1.69) | .244 |
| ≥ 3 | 17.7 (1.79) | 30.1 (2.25) | < .001a |
| Substance use disorders | |||
| None | 67.5 (2.17) | 75.0 (2.04) | .01 |
| Illicit drug use disorders only | 6.6 (1.03) | 8.5 (1.34) | .273 |
| Alcohol use disorders only | 16.6 (1.73) | 10.1 (1.28) | .003 |
| Both illicit drug and alcohol use disorders | 9.3 (1.57) | 6.4 (1.13) | .123 |
Note. Substance Abuse and Mental Health Services Administration (SAMHSA) requires that any description of overall sample sizes based on the restricted-use data files has to be rounded to the nearest 100, which intends to minimize potential disclosure risk.
Source: SAMHSA, Center for Behavioral Health Statistics and Quality, NSDUH, 2008–2013.
Statistically significant even after the Bonferroni correction.
Unadjusted Prevalence of Receiving Mental Health Treatment
Table 2 shows that in the 28 states, 46.8% of low-income uninsured nonelderly adults with SMI received mental health treatment in the past year, whereas 76.0% of low-income nonelderly adults with SMI who were enrolled in Medicaid-only received mental health treatment in the past year. In the United States, among low-income uninsured nonelderly adults with SMI, 46.5% received mental health treatment in the past year. By contrast, among low-income nonelderly adults with SMI who were enrolled in Medicaid-only, 74.8% received mental health treatment in the past year.
TABLE 2—
Unadjusted Prevalence of Receiving Mental Health Treatment in the Past Year Among US Adults Aged 18–64 Years Who Had Serious Mental Illness and Were Either Uninsured or Covered by Medicaid-Only: National Survey on Drug Use and Health, 2008–2013
| Unadjusted Past-Year Mental Health Treatment Rates | Full-Year Uninsured, Weighted % (SE) | Full-Year Medicaid-Only, Weighted % (SE) | P for Point Difference |
| In the 28 statesa,b | |||
| Receipt of mental health treatment | 46.8 (3.47) | 76.0 (2.39) | < .001 |
| Receipt of outpatient mental health treatment | 27.3 (3.16) | 52.4 (2.91) | < .001 |
| Receipt of inpatient mental health treatment | 7.0 (1.90) | 16.6 (2.51) | .002 |
| Receipt of prescription medication for mental health problems | 39.4 (3.44) | 69.2 (2.71) | < .001 |
| In the United Statesa,c | |||
| Receipt of mental health treatment | 46.5 (2.39) | 74.8 (1.96) | < .001 |
| Receipt of outpatient mental health treatment | 26.0 (2.15) | 50.0 (2.52) | < .001 |
| Receipt of inpatient mental health treatment | 6.6 (1.22) | 14.9 (1.87) | < .001 |
| Receipt of prescription medication for mental health problems | 41.6 (2.38) | 69.7 (2.15) | < .001 |
Source: Substance Abuse and Mental Health Services Administration (SAMHSA), Center for Behavioral Health Statistics and Quality, NSDUH, 2008–2013.
SAMHSA requires that any description of overall sample sizes based on the restricted-use data files has to be rounded to the nearest 100, which intends to minimize potential disclosure risk.
The sample size was n = 500 for the full-year uninsured and n = 700 for those with full-year Medicaid-only.
The sample size was n = 1000 for the full-year uninsured and n = 1000 for those with full-year Medicaid-only.
Model-Adjusted Prevalence of Receiving Mental Health Treatment
Table 3 shows that in the 28 states, the MAP of receiving mental health treatment among full-year Medicaid-only enrollees with SMI in the past year (MAP = 71.3%) was 30.1% higher (P < .001) than their uninsured counterparts (MAP = 54.8%). The MAP of receiving outpatient mental health treatment among Medicaid enrollees with SMI (MAP = 47.4%) was 39.8% greater (P < .01) than their uninsured counterparts (MAP = 33.9%). The MAP of receiving inpatient mental health treatment among Medicaid enrollees with SMI did not significantly differ from their uninsured counterparts. The MAP of receiving psychotropic medications among Medicaid enrollees with SMI (MAP = 63.9%) was 33.1% higher (P = .001) than their uninsured counterparts (MAP = 48.0%).
TABLE 3—
Model-Adjusted Prevalence of Receiving Mental Health Treatment in the Past Year Among US Adults Aged 18–64 Years in the 28 States Who Had Serious Mental Illness and Were Either Uninsured or Covered by Medicaid-Only: National Survey on Drug Use and Health, 2008–2013
| Model-Adjusted Prevalence |
|||
| Outcome Variables | Full-Year Medicaid-Only, Predicted Marginal % (95% CI) | Full-Year Uninsured, Predicted Marginal % (95% CI) | Model-Adjusted Prevalence Difference (Full-Year Medicaid-only – Full-Year Uninsured), Predicted Marginal % (95% CI) |
| Receipt of mental health treatment | 71.3** (65.74, 76.29) | 54.8** (48.16, 61.33) | 16.5** (8.07, 24.93) |
| Receipt of outpatient mental health treatment | 47.4** (41.71, 53.26) | 33.9** (27.49, 40.99) | 13.5* (4.68, 22.32) |
| Receipt of inpatient mental health treatment | 14.4** (10.58, 19.33) | 9.9** (6.28, 15.32) | 4.5 (0.00, 10.38) |
| Receipt of prescription medication for mental health problems | 63.9** (57.90, 69.54) | 48.0** (41.29, 54.73) | 15.9** (6.88, 24.92) |
Note. CI = confidence interval. Substance Abuse and Mental Health Services Administration (SAMHSA) requires that any description of overall sample sizes based on the restricted-use data files has to be rounded to the nearest 100, which intends to minimize potential disclosure risk. Covariates in each of the 4 final multivariable models were age, gender, race/ethnicity, education, employment status, region, self-rated health, the number of emergency room visits, substance use disorders, severity of mental illness, perceived unmet need for mental health treatment, state variations (27 individual states and DC), and accessibility of mental health treatment per 10 000 county residents (the number of community mental health centers, the number of licensed psychologists, the number of office-based psychiatrists, and the number of psychiatric hospitals).
Source: SAMHSA, Center for Behavioral Health Statistics and Quality, National Survey on Drug Use and Health, 2008–2013.
*P < .01; **P ≤ .001.
Table 4 shows that in the United States, the MAP of receiving mental health treatment among full-year Medicaid-only enrollees with SMI in the past year (MAP = 70.4%) was 35.9% higher (P < .001) than their uninsured counterparts (MAP = 51.8%). The MAP of receiving outpatient mental health treatment among Medicaid enrollees with SMI (MAP = 45.4%) was 52.3% higher (P < .001) than their uninsured counterparts (MAP = 29.8%). The MAP of receiving inpatient mental health treatment among Medicaid enrollees with SMI did not significantly differ from their uninsured counterparts. The MAP of receiving psychotropic medications among Medicaid enrollees with SMI (MAP = 65.3%) was 39.5% higher (P = .001) than their uninsured counterparts (MAP = 46.8%).
TABLE 4—
Model-Adjusted Prevalence of Receiving Mental Health Treatment in the Past Year Among US Adults Aged 18–64 Years Who Had Serious Mental Illness and Were Either Uninsured or Covered by Medicaid-Only: National Survey on Drug Use and Health, 2008–2013
| Model-Adjusted Prevalence |
|||
| Outcome Variables | Full-Year Medicaid-Only, Predicted Marginal % (95% CI) | Full-Year Uninsured, Predicted Marginal % (95% CI) | Model-Adjusted Prevalence Difference (Full-Year Medicaid-Only – Full-Year Uninsured), Predicted Marginal % (95% CI) |
| Receipt of mental health treatment | 70.4** (65.67, 74.70) | 51.8** (46.98, 56.65) | 18.6** (11.74, 25.46) |
| Receipt of outpatient mental health treatment | 45.4** (40.62, 50.35) | 29.8** (25.34, 34.81) | 15.6** (8.94, 22.26) |
| Receipt of inpatient mental health treatment | 16.0** (12.95, 19.67) | 13.3** (10.05, 17.27) | 2.7 (0.00, 8.09) |
| Receipt of prescription medication for mental health problems | 65.3** (60.32, 69.92) | 46.8** (42.06, 51.64) | 18.5** (11.64, 25.36) |
Note. CI = confidence interval. Substance Abuse and Mental Health Services Administration (SAMHSA) requires that any description of overall sample sizes based on the restricted-use data files has to be rounded to the nearest 100, which intends to minimize potential disclosure risk. Covariates in each of the 4 final multivariable models were age, gender, race/ethnicity, education, employment status, region, self-rated health, the number of emergency room visits, substance use disorders, severity of mental illness, perceived unmet need for mental health treatment, state variations (50 individual states and DC), and accessibility of mental health treatment per 10 000 county residents (the number of community mental health centers, the number of licensed psychologists, the number of office-based psychiatrists, and the number of psychiatric hospitals).
Source: SAMHSA, Center for Behavioral Health Statistics and Quality, National Survey on Drug Use and Health, 2008–2013.
**P ≤ .001.
DISCUSSION
To our knowledge, ours is the first study that examined differences in the prevalence of receiving mental health treatment between low-income uninsured nonelderly adults with SMI who are eligible for Medicaid under the ACA and their existing Medicaid counterparts. Using state and nationally representative survey data, we assessed these differences in the 28 states currently expanding Medicaid and in the United States as a whole, if all states eventually move forward with Medicaid expansion. Importantly, because the SMI prediction model based on the NSDUH data had a high value of specificity (0.98), the large majority of the included cases met the SMI criteria.
Our results showed evidence that supported the 2 hypotheses that we proposed in this study. Under the ACA, Medicaid expansion efforts might significantly increase the prevalence of receiving mental health treatment among new Medicaid enrollees with SMI in the 28 states that are currently expanding Medicaid. Also, if all states eventually move forward with Medicaid expansion, the expansion efforts might also significantly increase the prevalence of receiving mental health treatment among this population in the United States.
It was critical to control for the differences in Medicaid benefit packages across states, accessibility of mental health treatment, and other potential confounding factors when we assessed the impact of Medicaid expansion efforts under the ACA. For example, we showed that the unadjusted prevalence of receiving mental health treatment in the past year was 62.4% higher among low-income nonelderly adults with SMI who were enrolled in Medicaid than among their uninsured counterparts in the 28 states. However, after adjusting for potential confounding factors, our results revealed that the prevalence of receiving mental health treatment among low-income uninsured nonelderly adults with SMI might increase 30.1% in the 28 states that are currently expanding Medicaid.
The 28 states are sharing the costs with the federal government through the ACA’s Medicaid expansion to improve the Medicaid mental health treatment infrastructure. Our multivariable results revealed that, compared with being uninsured, the impact of being enrolled in Medicaid on receipt of mental health treatment would be similar between the 28 states and the rest of the states that are not currently expanding Medicaid. Therefore, the rest of the states might gain similar prevalence of receiving mental health treatment if they eventually expand their Medicaid programs under the ACA. However, they might be reluctant to expand Medicaid because of the potential cost sharing that may occur later on.29,30
Limitations
Our study had several imitations. First, the ACA excludes undocumented aliens from enrolling in Medicaid. NSDUH collected the status of being born in the United States, but did not collect the status of lawful resident aliens or lawful permanent residents. We repeated the multivariable analyses only among low-income nonelderly adults who had past-year SMI and were born in the United States, and we had similar results. Second, NSDUH did not sample adults who were living in institutions at the time of the survey interview. Therefore, our results could only be generalized to community-dwelling adults. Third, our analyses did not adjust for all demand–supply issues related to mental health service utilization. For example, because of unavailable county-level data, we did not consider serious situations such as staff shortages and long waiting lines for mental health patients among mental health facilities accepting Medicaid.17,31,32 We also could not control for Medicaid acceptance rates of private therapists or physicians providing mental health treatment because of unavailable county-level data. At least 2 studies suggested that low Medicaid acceptance rates of psychiatrists might pose a barrier to mental health treatment access.33,34 Policies need to be implemented to ensure that the increased demand stemming from the Medicaid expansion under the ACA will not exacerbate the demand–supply gaps in mental health treatment.
Low-income uninsured nonelderly adults with SMI who are eligible for Medicaid face additional barriers to Medicaid enrollment and mental health treatment. One study revealed that populations with higher perceived treatment need and better awareness of coverage options are more likely to enroll in Medicaid.35 Among low-income uninsured adults with SMI in the 28 states, 31.5% neither received mental health treatment nor perceived unmet treatment need in the past year (additional analysis, data not shown). They were less likely to seek and receive mental health treatment even if they were enrolled in Medicaid. Therefore, programs with effective outreach and screening for SMI are particularly needed by low-income uninsured adults who do not perceive unmet need for mental health treatment. These programs often require additional resources and might have potential budgetary implications on state and federal governments.
Conclusions
In summary, our results might still overestimate the increases in receipt of mental health treatment under the ACA’s Medicaid expansion. However, these timely results might help inform planning and implementation efforts for the Medicaid expansion under the ACA to meet mental health treatment needs among low-income adults with SMI. More studies are needed to examine detailed demand–supply gaps in mental health treatment and mental health treatment patterns among low-income nonelderly adults with SMI in Medicaid expansion states and in the rest of the states over time.
Acknowledgments
We would like to thank Neil Russell, PhD, Peter Delany, PhD, and Ryan Mutter, PhD, of the Substance Abuse and Mental Health Services Administration and William Eaton, PhD, of the Johns Hopkins Bloomberg School of Public Health for their helpful comments.
Human Participant Protection
The data collection protocol of the National Survey on Drug Use and Health was approved by the institutional review board at RTI International.
References
- 1.Substance Abuse and Mental Health Services Administration. Results From the 2012 National Survey on Drug Use and Health: Mental Health Findings. NSDUH Series H-47; HHS Publication No. SMA 13-4805. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [Google Scholar]
- 2.Kessler RC, Berglund PA, Bruce ML et al. The prevalence and correlates of untreated serious mental illness. Health Serv Res. 2001;36(6 pt 1):987–1007. [PMC free article] [PubMed] [Google Scholar]
- 3.Wang PS, Demler O, Kessler RC. Adequacy of treatment for serious mental illness in the United States. Am J Public Health. 2002;92(1):92–98. doi: 10.2105/ajph.92.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McAlpine DD, Mechanic D. Utilization of specialty mental health care among persons with severe mental illness: the roles of demographics, need, insurance, and risk. Health Serv Res. 2000;35(1 pt 2):277–292. [PMC free article] [PubMed] [Google Scholar]
- 5.New Freedom Commission on Mental Health. Achieving the Promise: Transforming Mental Health Care in America. Final Report. DHHS Publication SMA-03-3832. Rockville, MD: US Department of Health and Human Services; 2003. [Google Scholar]
- 6.Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis. 2006;3(2):A42. [PMC free article] [PubMed] [Google Scholar]
- 7.Newcomer JW, Hennekens CH. Severe mental illness and risk of cardiovascular diseases. JAMA. 2007;298(15):1794–1796. doi: 10.1001/jama.298.15.1794. [DOI] [PubMed] [Google Scholar]
- 8.Vick B, Jones K, Mitra S. Poverty and severe psychiatric disorder in the US: evidence from the Medical Expenditure Panel Survey. J Ment Health Policy Econ. 2012;15(2):83–96. [PubMed] [Google Scholar]
- 9.Hudson CG. Socioeconomic status and mental illness: tests of the social causation and selection hypotheses. Am J Orthopsychiatry. 2005;75(1):3–8. doi: 10.1037/0002-9432.75.1.3. [DOI] [PubMed] [Google Scholar]
- 10. Substance Abuse and Mental Health Services Administration. Results From the 2012 National Survey on Drug Use and Health: Mental Health Detailed Tables. Available at: http://www.samhsa.gov/data/NSDUH/2k12MH_FindingsandDetTables/MHDT/NSDUH-MHDetTabsSect1peTabs2012.htm#Tab1.45B. Accessed February 26, 2014.
- 11. The Centers for Medicare & Medicaid Services. Affordable Care Act. Available at: http://www.medicaid.gov/affordablecareact/affordable-care-act.html. Accessed January 12, 2015.
- 12. The Centers for Medicare & Medicaid Services. Eligibility. Available at: http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Eligibility/Eligibility.html. Accessed January 12, 2015.
- 13.Garfield RL, Zuvekas SH, Lave JR, Donohue JM. The impact of national health care reform on adults with severe mental disorders. Am J Psychiatry. 2011;168(5):486–494. doi: 10.1176/appi.ajp.2010.10060792. [DOI] [PubMed] [Google Scholar]
- 14.Kott P, Hedden S, Aldworth J A revised strategy for estimating the prevalence of mental illness. Available at: http://www.samhsa.gov/data/2k12/NSDUHrevisedMImethods2012/NSDUHrevisedMImethods2012.pdf. Accessed April 2, 2014.
- 15.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. The NSDUH Report: Revised Estimates of Mental Illness from the National Survey on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [PubMed] [Google Scholar]
- 16.Saloner B, Sabik L, Sommers BD. Pinching the poor? Medicaid cost sharing under the ACA. N Engl J Med. 2014;370(13):1177–1180. doi: 10.1056/NEJMp1316370. [DOI] [PubMed] [Google Scholar]
- 17.Cummings JR, Wen H, Ko M, Druss BG. Geography and the Medicaid mental health care infrastructure: implications for health care reform. JAMA Psychiatry. 2013;70(10):1084–1090. doi: 10.1001/jamapsychiatry.2013.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. State Reforum. Map: where states stand on Medicaid expansion decisions. Available at: https://www.statereforum.org/Medicaid-Expansion-Decisions-Map?gclid=CLPUl93H-MACFeRj7AodvEYA3w. Accessed September 23, 2014.
- 19.Devoe JE, Gold R, McIntire P, Puro J, Chauvie S, Gallia CA. Electronic health records vs. Medicaid claims: completeness of diabetes preventive care data in community health centers. Ann Fam Med. 2011;9(4):351–358. doi: 10.1370/afm.1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Substance Abuse and Mental Health Services Administration. 2011 National Survey on Drug Use and Health: Imputation Report. Imputation for the NSDUH Income Variables. Available at: http://www.samhsa.gov/data/2k12/NSDUH2011MRB/NSDUHmrbImputation2011.pdf. Accessed April 2, 2014.
- 21.Schoen C, DesRoches C. Uninsured and unstably insured: the importance of continuous insurance coverage. Health Serv Res. 2000;35(1 pt 2):187–206. [PMC free article] [PubMed] [Google Scholar]
- 22. Substance Abuse and Mental Health Services Administration. National Mental Health Services Survey: 2010 Data on Mental Health Treatment Facilities. Available at: http://www.samhsa.gov/data/DASIS/NMHSS2010_Web.pdf. Accessed on May 7, 2014.
- 23. Health Resources and Services Administration. Area Health Resources Files. Available at: http://ahrf.hrsa.gov. Accessed on May 7, 2014.
- 24.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 25.Kessler RC, Barker PR, Colpe LJ et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 26. Gfroerer J. Estimating Mental Illness in the United States: SAMHSA’s Methodology. Briefing to the National Institute of Mental Health. November 18, 2013.
- 27. Shah B, Barnwell B, Bieler G. SUDAAN User’s Manual. Version 9.1 Research Triangle Park, NC: Research Triangle Institute; 2005.
- 28.Bieler GS, Brown GG, Williams RL, Brogan DL. Estimating model-adjusted risks, risk differences, and risk ratio from complex survey data. Am J Epidemiol. 2010;171(5):618–623. doi: 10.1093/aje/kwp440. [DOI] [PubMed] [Google Scholar]
- 29.Blumenthal D, Collins SR. Health care coverage under the Affordable Care Act—a progress report. N Engl J Med. 2014;371(3):275–281. doi: 10.1056/NEJMhpr1405667. [DOI] [PubMed] [Google Scholar]
- 30. The Council of Economic Advisors, Executive Office of the President of the United States. Missed opportunities: the consequences of state decisions not to expand Medicaid. Available at: http://www.whitehouse.gov//sites/default/files/docs/missed_opportunities_medicaid_0.pdf. Accessed July 5, 2014.
- 31.Cunningham P, McKenzie K, Taylor EF. The struggle to provide community-based care to low-income people with serious mental illness. Health Aff (Millwood) 2006;25(3):694–705. doi: 10.1377/hlthaff.25.3.694. [DOI] [PubMed] [Google Scholar]
- 32.Bishop TF, Press MJ, Keyhani S, Pincus HA. Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry. 2014;71(2):176–181. doi: 10.1001/jamapsychiatry.2013.2862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cunningham PJ, O’Malley AS. Do reimbursement delays discourage Medicaid participation by physicians? Health Aff (Millwood) 2009;28(1):w17–w28. doi: 10.1377/hlthaff.28.1.w17. [DOI] [PubMed] [Google Scholar]
- 34.Thomas KC, Ellis AR, Konrad TR, Holzer CE, Morrissey JP. County-level estimates of mental health professional shortage in the United States. Psychiatr Serv. 2009;60(10):1323–1328. doi: 10.1176/ps.2009.60.10.1323. [DOI] [PubMed] [Google Scholar]
- 35.Dhingra SS, Zack MM, Strine TW, Druss BG, Simoes E. Change in health insurance coverage in Massachusetts and other New England states by perceived health status: potential impact of health reform. Am J Public Health. 2013;103(6):e107–e114. doi: 10.2105/AJPH.2012.300997. [DOI] [PMC free article] [PubMed] [Google Scholar]