Abstract
Objectives. We conducted a cluster randomized controlled study of a lay health worker (LHW) intervention to increase colorectal cancer (CRC) screening rates among Vietnamese Americans, who typically have lower rates than do non-Hispanic Whites.
Methods. We randomized 64 LHWs to 2 arms. Each LHW recruited 10 male or female participants who had never had CRC screening (fecal occult blood test, sigmoidoscopy, or colonoscopy). Intervention LHWs led 2 educational sessions on CRC screening. Control LHWs led 2 sessions on healthy eating and physical activity. The main outcome was self-reported receipt of any CRC screening at 6 months after the intervention. We conducted the study from 2008 to 2013 in Santa Clara County, California.
Results. A greater proportion of intervention participants (56%) than control participants (19%) reported receiving CRC screening (P < .001). When controlling for demographic characteristics, the intervention odds ratio was 5.45 (95% confidence interval = 3.02, 9.82). There was no difference in intervention effect by participant gender.
Conclusions. LHW outreach was effective in increasing CRC screening in Vietnamese Americans. Randomized controlled trials are needed to test the effectiveness of LHW outreach for other populations and other health outcomes.
Vietnamese Americans are a predominantly refugee and immigrant population with a distinct culture and language. Vietnamese Americans are the fourth largest Asian group in the United States,1 yet they have more socioeconomic and health disparities than do non-Hispanic Whites.2 Vietnamese Americans have higher rates of unemployment (10.6% vs 9.0%), receiving public assistance (1.8% vs 1.2%), and poverty (15.5% vs 10.7%) than do non-Hispanic Whites and have a lower mean number of years of education (11.8 years vs 13.6 years).2 One health care disparity is in colorectal cancer (CRC) screening, with the proportions ever screened by fecal occult blood test, sigmoidoscopy or colonoscopy, and any CRC screening test among Vietnamese Americans lower at 29.0%, 36.0%, and 52.0%, respectively, than those among non-Hispanic Whites at 58.0%, 57.0%, and 75.0%, respectively.3
Lay health workers (LHWs)—defined as “a member of the community who has received some training to promote health or to carry out some health care services, but is not a health care professional”4(p2)—in culturally appropriate community-based interventions can improve cancer screening behaviors in underserved, ethnic populations.4–6 In our previous work, LHW outreach increased breast and cervical cancer screening rates among Vietnamese American women.7,8 Two community-based cluster randomized trials in the African American and Latino communities did not increase CRC screening rates in these communities.9,10
A cluster randomized controlled trial, using churches as the units of randomization, compared the effectiveness of 2 intervention strategies to promote CRC prevention behaviors among African American members of rural churches. Campbell et al. used a 2 × 2 factorial design to compare a tailored print and video intervention, consisting of 4 individually tailored newsletters and targeted videotapes, with a lay health advisor intervention. Results showed that the rates of CRC screening tests did not differ among study groups at 1-year follow-up.9
A community-based cluster randomized trial without a control group compared 2 different intervention delivery methods for lay health educator–taught cancer screening classes. The Latina participants were randomly assigned to classes delivered either individually or in social support groups. Results showed that CRC screening and maintenance behaviors did not differ significantly between the 2 delivery methods. Because there was no control group, it was not possible to observe the effectiveness of any of the delivery methods.10
No community-based LHW interventions have been conducted targeting CRC screening in Vietnamese Americans. Consequently, we examined the effectiveness of a community-based LHW intervention on increasing self-reported CRC screening rates in Vietnamese American women and men and compared its effectiveness by gender. We hypothesized that (1) after intervention, the self-reported CRC screening rate would be higher among the intervention participants than the control participants, and (2) the intervention would be more effective in women than in men.
METHODS
A coalition of 19 organizations and 6 community members (representing county health departments, health maintenance organizations, immigrant resettlement service providers, health care providers, cancer survivors, and researchers) partnered with 4 community-based organizations (CBOs) to provide the LHW services and with 2 research institutions to carry out the research protocols. Coalition and community members participated in all phases of the research, including design, implementation, data analysis, interpretation, and dissemination.11,12
Study Design, Recruitment, and Randomization
We used a cluster randomized controlled trial design, with LHWs and their recruited participants randomized together to either the intervention or the control condition. The proportion of male and female LHWs was equal in both conditions. The sample size of 64 LHWs and 640 participants was powered to detect an effect size of a 20% difference between the intervention and control group in the proportion screened for CRC at posttest, assuming an intracluster correlation coefficient of 0.05, an attrition rate of 0.05, a recruitment of 10 participants per LHW, and an estimated 20% of the control group and 40% of the intervention group being screened at posttest. We determined the number of participants per LHW by our prior LHW studies.7,8
Four CBOs delivered the LHW services from February 2008 to February 2012 (each CBO participated for 16 months). Each CBO hired a LHW coordinator. After training by the research staff, each coordinator recruited 16 LHWs, with equal numbers of men and women, from the CBO’s client base or the coordinator’s social networks (family, friends, or referrals). Eligibility criteria for LHWs included (1) self-identifying as Vietnamese or Vietnamese American, (2) being aged 50 to 74 years, (3) understanding and speaking Vietnamese, and (4) living in and intending to stay in the study area (Santa Clara County, CA) for the next 12 months. Research staff randomized LHWs to either the intervention or control group in a 1-to-1 ratio and then informed LHWs of their randomization assignment.
Each LHW recruited 10 participants of the same gender from his or her own social network. Intervention group LHWs informed their participants that they would attend 2 educational sessions about CRC screening; control LHWs informed their participants that they would be educated about healthy eating and physical activity. Inclusion eligibility criteria for participants included
self-identifying as Vietnamese or Vietnamese American,
being aged 50 to 74 years,
understanding Vietnamese,
living in and intending to stay in the study area for the next 6 months, and
never having had CRC screening (fecal occult blood test, sigmoidoscopy, or colonoscopy).
An exclusion criterion was living in the same household as another study participant.
Theoretical Framework
The pathways framework13–19 and the diffusion of innovations theory20 provided the theoretical framework for the LHW intervention. According to the pathways framework, knowledge, attitudes, and beliefs are pathways to screening behavior.
The intervention LHWs delivered educational sessions, health educational materials, and follow-up support services to improve participants’ knowledge, attitudes, and beliefs about CRC screening. According to the diffusion of innovations theory, “innovators,” or “change agents,” who are respected by peers influence public opinion.20,21 The LHWs were the innovators, or change agents, because they asked participants to obtain a screening test that they had never had before.
Health Educational Materials and Formative Research
We developed the educational materials “from scratch” as recommended by Achterberg22 to develop an appropriate communication mechanism, content, and illustration. We chose the flip-chart format as a teaching tool for LHWs to make presentations in small group educational sessions because it does not require LHWs to be proficient in technological devices. We developed the CRC screening flip chart in Vietnamese to connect directly to the target audience by using their vernacular, colloquial, and idiomatic expressions. A team of bilingual and bicultural staff and consultants drafted the content of the CRC flip chart to cover the colon in the body; what cancer is and specifically what CRC is; CRC risk factors, symptoms, prevention, and screening tests; the recommended age to begin; and where to get CRC screening.
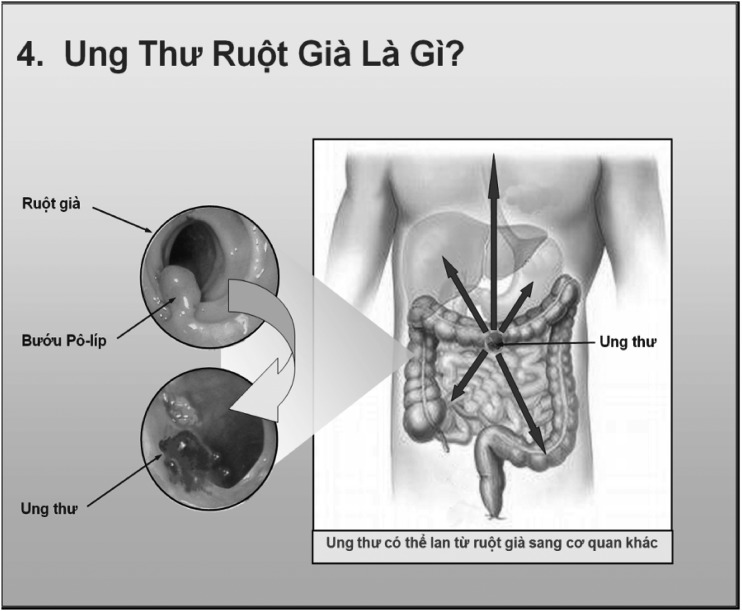
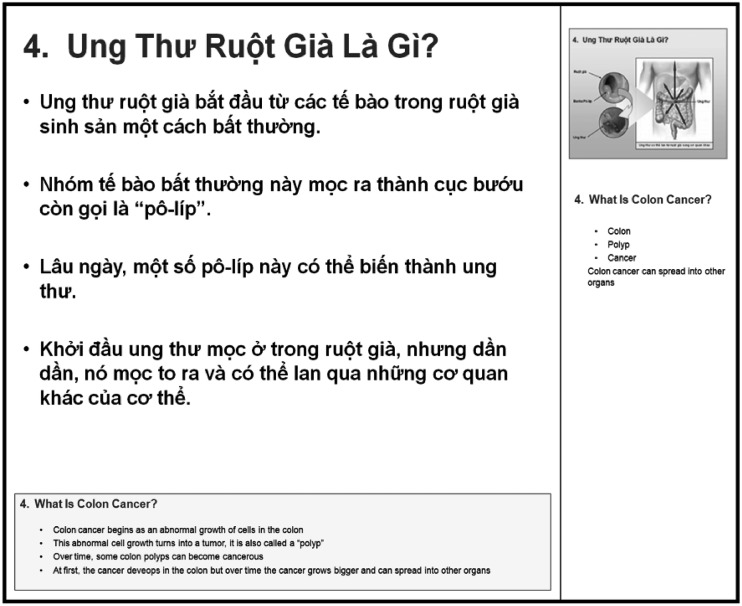
The CRC flip chart featured images of Vietnamese models obtaining CRC screening tests and other images to illustrate CRC screening recommendations. The flip chart was printed on 18- × 12-inch glossy heavy stock that was spiral bound and could to be set up in a tent format on a table for a small group to view. The front of each page, to be viewed by group participants, contained educational messages in Vietnamese, with graphics, photographs, and illustrations in full color to enhance the participants’ understanding of the presentation (Figure 1). The back, to be viewed by the LHWs, contained teaching points in Vietnamese and a small image of the front page with an English translation to aid the LHWs in delivering the presentation (Figure 2).
FIGURE 1—
Front page of the flip chart contains educational messages for participants to follow during the educational session presentation: Santa Clara County, CA, 2008–2013.
FIGURE 2—
Back page of the flip chart to be viewed by lay health workers, with teaching points to aid in delivering their presentations: Santa Clara County, CA, 2008–2013.
We conducted cognitive interviews of community members (not participants in the research) regarding the flip charts. Results of these cognitive interviews are reported separately.23 A bilingual and bicultural gastroenterologist reviewed the CRC flip chart for scientific accuracy. We used feedback and comments from the cognitive interview participants and the gastroenterologist to improve the prototype and make final adjustments to the flip chart. We then developed a CRC screening booklet with the same Vietnamese messages and images as on the front of the flip chart; the booklet contained the same messages in English at the bottom of each page. We also developed a healthy eating and physical activity flip chart and booklet for the control group using the same formative research process.
Lay Health Worker Intervention
LHW activities consisted of attending LHW training, recruiting participants, delivering 2 educational sessions, distributing health educational booklets, and providing follow-up support and navigation services to the participants. We paid each LHW $1200 to perform these functions. Over 2 days (for a total of 12 hours), the research staff and agency coordinator trained the LHWs in each study arm separately to prevent contamination. All LHWs were trained on recruitment of participants, outreach approaches and procedures, and organization and facilitation of educational sessions. The intervention LHWs were educated about CRC screening, whereas the control LHWs received information about healthy nutrition and physical activity. LHWs then practiced delivering their educational presentations using the flip charts. We gave LHWs a LHW reference manual covering their topics.
After the intervention LHWs recruited their 10 participants, they used the portable flip chart in the first educational group session to educate the participants about CRC screening and to recommend that they obtain it. At the end of the first session, the LHWs distributed the booklet. To permit the participants sufficient opportunity to obtain CRC screening, we allowed 2 to 3 months to pass between the first and the second educational sessions. In the second group session, the LHWs identified participants who had not followed the CRC screening recommendation, identified barriers to screening, and provided suggestions and support to overcome these barriers. Each session took 1 to 2 hours.
After each session, the intervention LHWs made follow-up telephone calls or in-person visits to participants to remind them to obtain CRC screening, to provide referrals to low-cost or no-cost CRC screening options for those without health insurance coverage, to assist with making appointments, and sometimes to accompany participants to appointments. The control LHWs carried out the same number of educational sessions of equal length about healthy eating and physical activity, distributed a booklet, and made follow-up calls or visits to participants to remind them to follow recommendations on healthy eating and physical activity. We did not pay participants for intervention activities.
Measures
Before the first educational session, research staff conducted a pretest telephone survey of all participants to confirm their eligibility and to collect baseline data. Staff conducted a posttest telephone survey 6 months after the first educational session (and 3–4 months after the second session) to allow intervention group participants sufficient time and opportunity to follow the CRC screening recommendation.
The main outcome variable was participant report of ever having had a CRC screening test (screening status). Secondary outcome variables included knowledge (having heard of colon polyps and knowing the recommended age to begin CRC screening), attitudes (perceived susceptibility: worrying about getting colon cancer and ever having thought they might get colon cancer), and belief (believing colon cancer can be cured if found early).
Demographic variables included gender, age, education, income, marital status, years lived in the United States, English language proficiency, employment, self-perceived health status, health insurance, having a place for health care, and having a personal doctor (Table 1). We chose these demographic and secondary outcome variables because they have been found to be associated with screening for other types of cancer.8,19
TABLE 1—
Baseline Characteristics of Vietnamese American Participants by Study Arm: Santa Clara County, CA, 2008–2013
| Characteristics | Intervention Group, % (n = 320) | Control Group, % (n = 320) | Pa |
| Gender, womanb | 50.0 | 50.0 | ≥ .99 |
| Age, y | |||
| 50–64 | 67.8 | 75.0 | .18 |
| 65–74 | 32.2 | 25.0 | |
| Lived in US, y | |||
| ≤ 10 | 39.1 | 37.7 | .79 |
| > 10 | 60.9 | 62.3 | |
| English proficiency | |||
| Fluent or good | 8.4 | 4.4 | .09 |
| So-so | 19.7 | 24.8 | |
| Not very good or not at all | 71.9 | 70.9 | |
| Education | |||
| ≤ elementary school | 22.4 | 19.1 | .6 |
| Junior high or some high school | 22.1 | 17.9 | |
| High school graduate or general equivalency diploma | 20.2 | 22.9 | |
| Some college | 25.3 | 29.2 | |
| ≥ college graduate | 9.9 | 11.0 | |
| Employment | |||
| Employed | 26.9 | 27.2 | .95 |
| Unemployed, homemaker, student, retired, or disabled | 73.1 | 72.8 | |
| Marital status | |||
| Married or living with partner | 64.1 | 62.2 | .69 |
| Separated, widowed, divorced, or never married | 35.9 | 37.8 | |
| Health insurance | |||
| None | 30.9 | 29.4 | .3 |
| Indigent care from county | 10.9 | 16.3 | |
| Medicare or MediCal (Medicaid) | 42.8 | 41.3 | |
| Private | 15.3 | 13.1 | |
| Annual household income, $ | |||
| < 10 000 | 17.8 | 15.3 | .14 |
| 10 000–19 999 | 20.3 | 24.1 | |
| 20 000–39 999 | 10.9 | 16.3 | |
| > 40 000 | 12.5 | 9.7 | |
| Don’t know or refused | 38.4 | 34.7 | |
| Self-perceived health status | |||
| Excellent, very good, or good | 49.7 | 38.4 | .02 |
| Fair, poor, or don’t know | 50.3 | 61.6 | |
| Had a particular place for health care | 61.3 | 55.9 | .22 |
| Had a personal doctor | 71.2 | 69.1 | .64 |
| Personal doctor was Vietnamesec | 90.8 | 92.8 | .46 |
P values are from generalized estimating equation models that account for clustering of participants by lay health workers.
Equal numbers of men and women by design.
Among those who had a personal doctor.
Statistical Analysis
From 2012 to 2013, we analyzed the pre- and posttest survey data using SAS version 9.3 (SAS Institute, Inc., Cary, NC). We used generalized estimating equation models in all analyses to account for participant clustering by LHW and correlated data between pre- and posttest on the same individual. In particular, we used bivariate generalized estimating equation models to assess the similarity between the study arms in participants’ demographic characteristics and to compare the study arms regarding the main outcome (screening status at posttest) and regarding the pre–post change (difference between pretest and posttest) in secondary outcome variables.
To test hypothesis 1, we created a logistic regression generalized estimating equation model of the main outcome as a function of study arm (intervention group vs control group) to control for demographic characteristics and LHW agency. To test hypothesis 2—that participant gender moderated the intervention—we added an interaction term between gender and study arm to the model regarding screening status.24
RESULTS
Of 894 potential participants recruited by the LHWs, the study enrolled 640, yielding a participation rate of 71.6%. Reasons for exclusion were could not be contacted by telephone, duplicated names, or lived in the same household as another participant (87); refused before eligibility could be determined (1); did not meet inclusion criteria (147); and refused after eligibility determination (19). The major reason for ineligibility (95% of ineligible participants) was that the potential participant had already had CRC screening. At posttest, 8 participants could not be recontacted (moved, died, or no contact after at least 7 attempts), and 5 refused, yielding a high retention rate of 98%.
Table 1 shows that demographic characteristics did not differ significantly between study arms except that intervention participants were more likely to rate their health as “excellent, very good, or good” than were controls. As shown in Table 2, the intervention group was significantly more likely than were controls to report having had CRC screening at posttest (56% vs 19%; P < .001). From pre- to posttest, the intervention group had significantly greater increases than did controls in the proportion who had heard of colon polyps, who knew the recommended age to begin CRC screening, and who believed that colon cancer can be cured if found early. From pre- to posttest, the intervention group showed a nonsignificant decrease in the proportion who worried about getting colon cancer, whereas the control group had a significant increase, and the pre–post change between the study arms was statistically significant.
TABLE 2—
Colorectal Cancer Screening Behavior, Knowledge, Perceived Susceptibility Attitudes, and Beliefs of Vietnamese American Participants by Study Arm: Santa Clara County, CA, 2008–2013
| Intervention Group (n = 316) |
Control Group (n = 311) |
||||||
| Outcome | Before Test, % | After Test, % | Differencea | Before Test, % | After Test, % | Differencea | Intervention Minus Control Differenceb |
| Reports ever having had CRC screening | 0 | 56 | NA | 0 | 19 | NA | 37*** |
| Knowledge | |||||||
| Has heard of colon polyps | 26 | 94 | 68*** | 27 | 46 | 19*** | 49*** |
| Knows age to begin CRC screening | 42 | 91 | 49*** | 39 | 60 | 21*** | 28*** |
| Perceived susceptibility attitudes | |||||||
| Worries about getting colon cancer | 45 | 42 | −3 | 42 | 53 | 11** | −14** |
| Ever thought might get colon cancer | 28 | 54 | 26*** | 28 | 47 | 19*** | 7 |
| Believes colon cancer can be cured if found early | 86 | 99 | 13*** | 90 | 95 | 5* | 8** |
Note. CRC = colorectal cancer; NA = not analyzed. P values are from generalized estimating equation models that account for clustering of participants by lay health workers.
P value for difference between pre- and posttest.
P value for difference between study arms with respect to posttest (self-reported behavior) and pre–post change (all other outcomes).
*P < .05; **P < .01; ***P < .001.
In a multivariable model for the factors associated with CRC screening adjusted for LHW agency and participant demographic characteristics, the LHW intervention was effective (odds ratio [OR] = 5.45; 95% confidence interval [CI] = 3.02, 9.82) and no adjusted variables were significant. That is, the odds of participants in the intervention group having CRC screening were more than 5 times that of control group participants, thus confirming hypothesis 1. After we added an interaction term between participant gender and study arm to the model, the intervention was effective in both women (OR = 7.15; 95% CI = 3.11, 16.4) and men (OR = 4.09; 95% CI = 1.76, 9.48). However, the size of the effect did not differ significantly by gender (P = .36). Therefore, participant gender was not a moderator of the intervention, and hypothesis 2 was not confirmed.
DISCUSSION
We made a few key findings. First, in this cluster randomized controlled trial, LHW outreach was effective in increasing self-reported CRC screening rates in Vietnamese American men and women. A previous quasiexperimental design study by our group of investigators found that a media-led intervention also increased CRC screening rates in Vietnamese Americans. The intervention effect size of 37 percentage points was large and clinically significant. The magnitude of the intervention effect–adjusted OR of 5.45 is similar to that in other randomized controlled trials aimed at increasing CRC screening in Asian Americans using clinic-based or professional-delivered approaches.25–27 Large effect sizes have been found in other community-based randomized controlled trials using LHWs among Vietnamese Americans for breast cancer screening (OR = 3.62) and cervical cancer screening (OR = 2.02).7,8 Thus, our study adds to the growing evidence that cancer screening can be increased significantly among Asian Americans when educational interventions are delivered in culturally appropriate ways and that LHW outreach can achieve similar effect sizes to those achieved by interventions delivered by CBO staff or health professionals.26,27
Second, to our knowledge, this is the first community-based cluster randomized controlled trial showing that LHW outreach is effective in increasing CRC screening in any ethnic group. Two previous community-based cluster randomized trials in the African American and Latino communities did not increase CRC screening rates in these communities.9,10
Third, the LHW intervention was effective in both women and men. Although our study was powered to detect an intervention effect in each gender, we did not find a significant difference in the intervention effect by gender. Most LHW intervention studies to promote cancer screening have been conducted in women.6–8,17,18,28–30 The few CRC community-based randomized controlled trials that included both men and women were delivered by CBO staff or health professionals.26,27 The result of our analysis supports the idea that community-based LHW outreach can work not only among women but also among men.
Why might this LHW intervention have worked? Social networks provided the existing relationships, trust, and social and cultural norms among the network members for LHWs to rely on for influencing the participants to obtain CRC screening. LHWs served as innovators, or change agents, to introduce a new behavior, namely, CRC screening. Shared common characteristics, such as language, culture, age group, and geographical residential area, between the participants and LHWs were the connectors for the LHWs to influence the participants’ behavior.
Follow-up services through telephone calls and visits to remind the participants to get CRC screening reinforced the efforts made at the educational sessions. Navigation services, such as providing referrals to low-cost or no-cost CRC screening, making appointments, and accompanying participants to appointments, are practical supports enabling participants to overcome barriers to obtain screening. These factors and services may have contributed to the intervention’s effectiveness. However, we did not assess how these individual factors influenced the intervention outcomes, and future research should examine the mechanisms through which such LHW outreach components increase cancer screening.
There are several limitations to this study. First, the study results may not be generalized to all Vietnamese Americans in the United States, because the study area was only a single urban area with a high concentration of Vietnamese Americans.
Second, there was the potential for contamination between the intervention and control group. For example, intervention members may have shared CRC screening information with control members during interactions in the community outside the educational sessions. However, if any such contamination occurred, it would have reduced only the intervention effect size.
Third, testing–observer (Hawthorne) effects (here, the effects of repeating the same question in the pre- and posttest surveys) may have affected respondents’ answers in the posttest survey. However, testing–observer effects would influence participants in both study arms.
Fourth, there is a potential selection bias. Although the LHWs were randomized to study arms, the participants were informed of the topic of the educational sessions at recruitment and thus were not blinded. It is possible that intervention LHWs would be more likely to choose potential participants who were willing to get CRC screening and, similarly, that control LHWs would be more likely to pick potential participants who were more willing to eat more servings of fruits and vegetables and to be more physically active.
However, both the intervention and control participants started out at baseline with low levels of knowledge of CRC screening and had never had CRC screening because this was one of the study enrollment eligibility criteria. In fact, the LHWs reported that finding participants who met this “no prior CRC screening” criterion was their greatest challenge in recruitment. Having had CRC screening was the major reason for ineligibility for participants’ enrollment in the study (95% of ineligible participants). Furthermore, the intervention and control groups were very comparable in demographic characteristics as well as in knowledge, attitudes, and belief at the pretest survey. However, there may still be some unmeasured bias. This limitation could be avoided by informing the LHWs of their randomization status and training them on the subject of the educational session only after they recruited their participants.
Fifth, the intervention group might have been susceptible to social desirability bias. We did not validate screening status with medical records review but relied solely on self-report in both arms. Therefore, the proportion screened may be an overestimate of true screening rates.
Strengths of this study include the high participation and retention rates and the formative research processes. In addition, the study contributes significantly to the LHW literature because it is a cluster randomized controlled trial including both women and men. Although our previous LHW studies concerned breast and cervical cancer in women,7,8 this study shows that LHW outreach is effective for promoting CRC screening as well and that it works well for Vietnamese American men as well as women.
The robustness of the LHW intervention effect on 3 different cancer screening recommendations and for both genders suggests that LHW outreach might be productively disseminated to other geographic areas with large concentrations of Vietnamese Americans and potentially to other disease and risk factor outcomes. The literature on the effectiveness of LHW outreach on CRC screening in other ethnicities is mixed.25,29–31 More randomized controlled trials are needed to test the effectiveness of LHW outreach for other populations and other health outcomes.
Acknowledgments
This research was supported by the National Cancer Institute (grant R01 CA 132660).
This research was presented in part at the American Association for Cancer Research Conference on the Science of Cancer Health Disparities in Racial/Ethnic Minorities and the Medically Underserved; October 27–30, 2012; San Diego, CA.
We thank the Vietnamese Reach for Health Coalition, community-based organization and research institution partners, and community members for participating in all phases of the study.
Human Participant Protection
The institutional review boards of the Cancer Prevention Institute of California and the University of California, San Francisco approved the research protocol.
References
- 1.Hoeffel EM, Rastogi S, Kim MO, Shahid H. The Asian population. 2010. Available at: http://www.census.gov/prod/cen2010/briefs/c2010br-11.pdf. Accessed April 14, 2014.
- 2.Logan JR, Zhang W. Separate but equal: Asian nationalities in the US. 2013. Available at: http://www.s4.brown.edu/us2010/Data/Report/report06112013.pdf. Accessed April 14, 2014.
- 3.Wong ST, Gildengorin G, Nguyen T, Mock J. Disparities in colorectal cancer screening rates among Asian Americans and non-Latino Whites. Cancer. 2005;104(12 suppl):2940–2947. doi: 10.1002/cncr.21521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lewin S, Munabi-Babigumira S, Glenton C et al. Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Syst Rev. 2010;(3) doi: 10.1002/14651858.CD004015.pub3. CD004015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lipp A. Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases: a review synopsis. Public Health Nurs. 2011;28(3):243–245. doi: 10.1111/j.1525-1446.2011.00950.x. [DOI] [PubMed] [Google Scholar]
- 6.Hou SI, Sealy DA, Kabiru CW. Closing the disparity gap: cancer screening interventions among Asians—a systematic literature review. Asian Pac J Cancer Prev. 2011;12(11):3133–3139. [PubMed] [Google Scholar]
- 7.Mock J, McPhee SJ, Nguyen T et al. Effective lay health worker outreach and media-based education for promoting cervical cancer screening among Vietnamese American women. Am J Public Health. 2007;97(9):1693–1700. doi: 10.2105/AJPH.2006.086470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nguyen TT, Le G, Nguyen T et al. Breast cancer screening among Vietnamese Americans: a randomized controlled trial of lay health worker outreach. Am J Prev Med. 2009;37(4):306–313. doi: 10.1016/j.amepre.2009.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Campbell MK, James A, Hudson MA et al. Improving multiple behaviors for colorectal cancer prevention among African American church members. Health Psychol. 2004;23(5):492–502. doi: 10.1037/0278-6133.23.5.492. [DOI] [PubMed] [Google Scholar]
- 10.Larkey LK, Herman PM, Roe DJ et al. A cancer screening intervention for underserved Latina women by lay educators. J Womens Health (Larchmt) 2012;21(5):557–566. doi: 10.1089/jwh.2011.3087. [DOI] [PubMed] [Google Scholar]
- 11.Israel BA, Schulz AJ, Parker EA, Becker AB, Allen AJ, III, Guzman JR. Critical issues in developing and following CBPR principles. In: Minkler M, Wallerstein N, editors. Community-Based Participatory Research for Health: From Process to Outcome. 2nd ed. San Francisco, CA: Jossey-Bass; 2008. pp. 53–76. [Google Scholar]
- 12.Viswanathan M, Ammerman A, Eng E et al. Community-based participatory research: assessing the evidence. Evid Rep Technol Assess (Summ) 2004;(99):1–8. [PMC free article] [PubMed] [Google Scholar]
- 13.Walsh JM, McPhee SJ. A systems model of clinical preventive care: an analysis of factors influencing patient and physician. Health Educ Q. 1992;19(2):157–175. doi: 10.1177/109019819201900202. [DOI] [PubMed] [Google Scholar]
- 14.Hiatt R, Pasick RJ, Perez-Stable EJ et al. Pathways to early cancer detection in the multiethnic population of the San Francisco Bay Area. Health Educ Q. 1996;23(suppl):S10–S27. [Google Scholar]
- 15.Bird JA, Otero-Sabogal R, Ha NT, McPhee SJ. Tailoring lay health worker interventions for diverse cultures: lessons learned from the Vietnamese and Latina communities. Health Educ Q. 1996;23(suppl):S105–S122. [Google Scholar]
- 16.McPhee SJ, Bird JA, Ha NT, Jenkins CN, Fordham D, Le B. Pathways to early cancer detection for Vietnamese women: Suc khoe la vang! (Health is gold!) Health Educ Q. 1996;23(suppl):S60–S75. [Google Scholar]
- 17.Bird JA, McPhee SJ, Ha NT, Le B, Davis T, Jenkins CN. Opening pathways to cancer screening for Vietnamese-American women: lay health workers hold a key. Prev Med. 1998;27(6):821–829. doi: 10.1006/pmed.1998.0365. [DOI] [PubMed] [Google Scholar]
- 18.Lam TK, McPhee SJ, Mock J et al. Encouraging Vietnamese-American women to obtain Pap tests through lay health worker outreach and media education. J Gen Intern Med. 2003;18(7):516–524. doi: 10.1046/j.1525-1497.2003.21043.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nguyen BH, McPhee SJ, Stewart SL, Doan HT. Effectiveness of a controlled trial to promote colorectal cancer screening in Vietnamese Americans. Am J Public Health. 2010;100(5):870–876. doi: 10.2105/AJPH.2009.166231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rogers EM. Diffusion of Innovations. 5th ed. New York, NY: Free Press; 2003. [Google Scholar]
- 21.Glasgow RE, Marcus AC, Bull SS, Wilson KM. Disseminating effective cancer screening interventions. Cancer. 2004;101(5 suppl):1239–1250. doi: 10.1002/cncr.20509. [DOI] [PubMed] [Google Scholar]
- 22.Achterberg CL. Qualitative research: what do we know about teaching good nutritional habits? J Nutr. 1994;124(9 suppl):1808S–1812S. doi: 10.1093/jn/124.suppl_9.1808S. [DOI] [PubMed] [Google Scholar]
- 23.Nguyen BH, Nguyen CP, McPhee SJ, Stewart SL, Bui-Tong N, Nguyen TT. Cognitive interviews of Vietnamese Americans on healthy eating and physical activity health educational materials. Ecol Food Nutr. 2015 doi: 10.1080/03670244.2015.1015119. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 24.Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 25.Tu SP, Taylor V, Yasui Y et al. Promoting culturally appropriate colorectal cancer screening through a health educator: a randomized controlled trial. Cancer. 2006;107(5):959–966. doi: 10.1002/cncr.22091. [DOI] [PubMed] [Google Scholar]
- 26.Walsh JM, Salazar R, Nguyen TT et al. Healthy Colon, Healthy Life: a novel colorectal cancer screening intervention. Am J Prev Med. 2010;39(1):1–14. doi: 10.1016/j.amepre.2010.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maxwell AE, Bastani R, Danao LL, Antonio C, Garcia GM, Crespi CM. Results of a community-based randomized trial to increase colorectal cancer screening among Filipino Americans. Am J Public Health. 2010;100(11):2228–2234. doi: 10.2105/AJPH.2009.176230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wells KJ, Luque JS, Miladinovic B et al. Do community health worker interventions improve rates of screening mammography in the United States? A systemic review. Cancer Epidemiol Biomarkers Prev. 2011;20(8):1580–1598. doi: 10.1158/1055-9965.EPI-11-0276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jandorf L, Gutierrez Y, Lopez J, Christie J, Itzkowitz SH. Use of a patient navigator to increase colorectal cancer screening in an urban neighborhood health clinic. J Urban Health. 2005;82(2):216–224. doi: 10.1093/jurban/jti046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Viswanathan M, Kraschnewski JL, Nishikawa B et al. Outcomes of community health worker interventions. Evid Rep Technol Assess (Full Rep) 2009;(181):1–144. A1–A2, B1–B14, passim. [PMC free article] [PubMed] [Google Scholar]
- 31.Viswanathan M, Kraschnewski JL, Nishikawa B et al. Outcomes and cost of community health worker interventions: a systematic review. Med Care. 2010;48(9):792–808. doi: 10.1097/MLR.0b013e3181e35b51. [DOI] [PubMed] [Google Scholar]