Abstract
Objectives. This study sought to estimate total health care costs for mild, moderate, and severe pediatric traumatic brain injury (TBI) and to compare individual- and population-level costs across levels of TBI severity.
Methods. Using 2007 to 2010 MarketScan Commercial Claims and Encounters data, we estimated total quarterly health care costs 1 year after TBI among enrollees (aged < 18 years). We compared costs across levels of TBI severity using generalized linear models.
Results. Mild TBI accounted for 96.6% of the 319 103 enrollees with TBI; moderate and severe TBI accounted for 1.7% and 1.6%, respectively. Adjusted individual health care costs for moderate and severe TBI were significantly higher than mild TBI in the year after injury (P < .01). At the population level, moderate and severe TBI costs were 88% and 75% less than mild TBI, respectively.
Conclusions. Individually, moderate and severe TBI initially generated costs that were markedly higher than those of mild TBI. At the population level, costs following mild TBI far exceeded those of more severe cases, a result of the extremely high population burden of mild TBI.
More than 600 000 children visit US emergency departments each year for traumatic brain injuries (TBIs).1 Several recent studies have described the costs associated with pediatric TBI2–7; however, many focused on acute inpatient treatment and used emergency department or hospital data only.2,3,5–7 These studies captured costs of moderate and severe TBIs, injuries that often involve poor verbal and motor responses, seizures, intracranial hypertension, and posttraumatic amnesia. Mild TBIs, such as concussions, may be evaluated solely in office settings and were not included in studies using emergency department or hospital data. Indeed, pediatric TBI cost analyses should include any rehabilitation, long-term care, and clinical evaluation for months after the injury, care that may be received in multiple clinical settings. Moderate and severe TBIs are associated with long-term physical and psychological impacts that require ongoing care, and recent research described disability from mild TBIs as well.8–11 Studies that estimated long-term costs years after injury were limited in geographic scope4 or population size.12
An analysis of the 1997 to 2000 Medical Expenditure Panel Survey (MEPS) estimated that total annual expenditures for services for nonhospitalized children with TBIs averaged $77.9 million in the United States, with per capita costs estimated at $1044.13 Although this study captured costs for mild and moderate TBIs that are often not reported in the scientific literature, the analysis was limited in MEPS by self-reported conditions.13
Given that mild TBI constitutes 75% of all TBIs in the United States,14 it is reasonable to expect that the population-level costs for mild TBI may exceed those of moderate or severe TBI, even though more severe injuries may cost considerably more per person. This would be important to payers who contemplate priorities for strategies to reduce costs after TBI. Moreover, although Medicaid patients are disproportionately affected by severe TBI, the diagnosis of mild TBI in particular may be more prevalent among commercially insured children.
The purpose of this study was to use a large, commercial claims database to provide a comprehensive estimate of total health care costs for pediatric TBI and to explore the differences between individual- and population-level costs for mild, moderate, and severe TBI.
METHODS
This retrospective observational cohort study of insured children with TBI used the MarketScan Commercial Claims and Encounters research database from Truven Health Analytics for the period starting January 1, 2007, and ending December 31, 2010. These data provide health services utilization information for more than 20 million US employees and dependents throughout the United States with health care coverage through privately insured, employer-sponsored health plans.15 Individuals are covered under a variety of fee-for-service, point-of-service, and capitated reimbursement schemes. Although these data make up a nonprobability convenience sample, nearly half of US health insurance plans contribute to these databases. Many large-scale, observational studies utilize MarketScan because it reflects real-world health care for a heterogeneous population of insured individuals.15,16
Records of enrollees younger than 18 years were included in this analysis if they included at least 1 TBI diagnosis for any inpatient or outpatient claim—termed the index TBI. TBI diagnoses followed the Centers for Disease Control and Prevention’s definition and included the following International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes: 800.0–801.9, 803.0–804.9, 850.0–854.1, 950.1–950.3, 959.01, and 995.55.1 Cases enrolled for less than 180 days before index TBI or cases with less than 12 months of enrollment after TBI were excluded. Variables were created to describe injury characteristics, all-cause health care costs, patient demographics, and comorbidities.
Measurement
Injury characteristics.
TBI severity was defined using the Abbreviated Injury Scale for the head and neck region (AIS-HN) and stratified severity into the following categories: mild (AIS-HN < 3), moderate (AIS-HN = 3), and severe (AIS-HN > 3). AIS-HN was estimated from the ICD Programs for Injury Categorization (ICDPIC), an ICD-9 mapping module for Stata (Stata Corp LP, College Station, TX).17 The ICD-based AIS-HN approach to categorizing injury severity has been employed previously.18,19 Diagnosis codes from the index TBI claims date and the 2 weeks thereafter were used to calculate the AIS-HN scores to avoid incorporating any subsequent injuries or conditions that arose independent of the index TBI. ICDPIC also generated maximum AIS and injury severity score estimates. We classified any enrollee with an index TBI claims date that coincided with hospital admission as being hospitalized for the index TBI. The presence of polytrauma was defined as AIS greater than 0 in any body region other than the head and neck. We categorized patients with an AIS of 3 or greater in the extremity region as experiencing a moderate to severe extremity injury.
Health care costs.
We calculated total costs using medical billing data from MarketScan. Total costs were defined as the total reimbursed amount delivered to facilities or health care services after the injury date and included inpatient admission, inpatient services, and outpatient services costs. Total costs constituted direct costs and did not include expenses indirectly related to the injury, such as missed time from work. Costs were not limited by diagnosis code or procedure received and were interpreted as all-cause health care costs. We aggregated costs in quarterly intervals after index TBI: 0 to 3 months, 4 to 6 months, 7 to 9 months, and 10 to 12 months. Any enrollee with negative cost observations (after aggregating) was excluded from analysis because it was not possible to ascertain whether these negative costs represented data entry errors or cost corrections for another month. For the subset of patients enrolled for 24 months after injury, we also explored total costs 0 to 12 and 13 to 24 months after injury.
Demographics and comorbidities.
The following demographic variables were calculated: age at index TBI, gender, geographic region, and rurality. We based geographic region and rurality on the primary beneficiary’s data. Geographic region was categorized as Northeast, North Central, South, West, and unknown. We classified enrollees located in metropolitan statistical areas as urban; rural enrollees were those not located in a metropolitan statistical area. Preexisting comorbidities were defined as the presence of ICD-9-CM diagnosis codes for 1 or more of the following conditions in the 180 days prior to index TBI: asthma, seizure, mental retardation, developmental disorders or delays, headaches, attention deficit and hyperactivity disorder, depression, anxiety, or fatigue (for ICD-9-CM codes see Table A, available as a supplement to the online version of this article at http://www.ajph.org). We selected these conditions as possible contributors to health care costs in pediatric patients; enrollees were coded as either having 1 or more comorbidities or not having any.
Statistical Analyses
We compared unadjusted mean total health care costs for patients across levels of TBI by using the t test for time intervals after index TBI. Generalized linear models (GLMs) were used to compare health care costs across levels of TBI severity. GLMs perform well and are often used in analyzing health care cost data, which are frequently skewed to the right and overdispersed.20–23 We used Box–Cox and modified Park tests to determine link and family specifications for GLMs.23,24 Regression models adjusted for the following demographic and injury characteristics that could influence costs: age at index TBI, gender, geographic region, rurality, evidence of polytrauma at the time of TBI, severe extremity injury at the time of TBI, and presence of any comorbidity. Model factors were evaluated for multicollinearity and removed if correlations exceeded 0.8. Models also adjusted for total health care costs in the 180 days before index TBI. Results were reported in terms of cost ratios (CRs). We analyzed data for all patients in the primary sample (enrolled for more than 12 months after index TBI) for the time intervals of 0 to 3, 4 to 6, 7 to 9, and 10 to 12 months. For the subgroup of patients enrolled for at least 24 months after injury, we analyzed costs for 0 to 12 and also 13 to 24 months.
To estimate the health care cost burden of pediatric TBI in this insured population, we calculated the sum of costs across each level of TBI severity for all patients. Unadjusted cost ratios were compared across levels of TBI severity. We used Stata MP version 13.1 for Macintosh for all analyses.
RESULTS
Between January 1, 2007, and December 31, 2010, the MarketScan Commercial Claims and Encounters research database included information for 22 876 839 covered individuals younger than 18 years. During this time period, we identified 614 105 unique individuals with at least 1 ICD-9-CM diagnosis code, indicating a TBI in the database. Among these, 586 866 were continuously enrolled for at least 180 days before diagnosis and did not have a diagnosis code for a TBI in the preceding 180 days. We excluded 267 763 enrollees from the study sample for 1 or more of the following criteria: enrollment for less than 12 months after index TBI claim (n = 259 322), death as a result of index TBI (n = 30), and geographic information not available (n = 8346). The final sample size for the primary analysis was 319 103 enrollees. For the subgroup analysis, we excluded persons enrolled for less than 24 months after index TBI for a sample size of 157 073 enrollees (Figure A, available as a supplement to the online version of this article at http://www.ajph.org).
The primary analysis sample comprised 308 174 (96.6%) children with mild TBI, 5579 (1.7%) with moderate TBI, and 5350 (1.6%) with severe TBI (Table 1). Individuals were most commonly male (62.4%) and located in the South (36.8%) and in urban areas (86.7%). Overall, 97.5% of children seen for index TBI were not admitted and were nearly all mild cases. Among moderate and severe TBI cases, 27.6% and 42.2% were admitted, respectively (Table 1). Whereas 45.0% had polytrauma, only 0.4% involved a severe extremity injury. In the subgroup analysis sample, 151 594 (96.5%) children had mild TBI, 2761 (1.8%) had moderate TBI, and 2718 (1.7%) had severe TBI (Table B, available as a supplement to the online version of this article at http://www.ajph.org). The subgroup sample reflected the primary sample for demographic and injury characteristics and health history.
TABLE 1—
Characteristics of Study Population With Follow-Up for at Least 12 Months After Injury: Sample of Patients, United States, January 1, 2007–December 31, 2010
| Demographic Characteristic | Mild TBI (n = 308 174) | Moderate TBI (n = 5 579) | Severe TBI (n = 5 350) | All TBI (n = 319 103) |
| Age, y | ||||
| < 5, no. (%) | 93 433 (30.3) | 1 154 (20.7) | 1 249 (23.3) | 95 836 (30.0) |
| 5–9, no. (%) | 61 123 (19.8) | 891 (16.0) | 985 (18.4) | 62 999 (19.7) |
| 10–14, no. (%) | 80 225 (26.0) | 1 538 (27.6) | 1 453 (27.2) | 83 216 (26.1) |
| 15–18, no. (%) | 73 393 (23.8) | 1 996 (35.8) | 1 663 (31.1) | 77 052 (24.2) |
| Mean (SD) | 9.0 (5.7) | 10.7 (5.5) | 10.1 (5.6) | 9.0 (5.7) |
| Gender, no. (%) | ||||
| Male | 191 851 (62.3) | 3 729 (66.8) | 3 450 (64.5) | 199 030 (62.4) |
| Female | 116 323 (37.8) | 1 850 (33.2) | 1 900 (35.5) | 120 073 (37.6) |
| Region, no. (%) | ||||
| Northeast | 54 423 (17.7) | 731 (13.1) | 704 (13.2) | 55 858 (17.5) |
| North Central | 83 008 (26.9) | 1 608 (28.8) | 1 426 (26.6) | 86 042 (27.0) |
| South | 112 727 (36.6) | 2 310 (41.4) | 2 294 (42.9) | 117 331 (36.8) |
| West | 58 016 (18.8) | 930 (16.7) | 926 (17.3) | 59 872 (18.8) |
| Rurality, no. (%) | ||||
| Urban | 267 867 (86.9) | 4 538 (81.3) | 4 380 (81.9) | 276 785 (86.7) |
| Rural | 40 307 (13.1) | 1 041 (18.7) | 970 (18.1) | 42 318 (13.3) |
| Injury characteristics | ||||
| Admitted to hospital for index TBI, no. (%) | ||||
| No | 303 973 (98.6) | 4 039 (72.4) | 3 095 (57.8) | 311 107 (97.5) |
| Yes | 4 201 (1.4) | 1 540 (27.6) | 2 255 (42.2) | 7 996 (2.5) |
| Polytrauma, no. (%) | ||||
| No | 171 715 (55.7) | 1 753 (31.4) | 2 057 (38.4) | 175 525 (55.0) |
| Yes | 136 459 (44.3) | 3 826 (68.6) | 3 293 (61.6) | 143 578 (45.0) |
| Severe extremity injury, no. (%) | ||||
| No | 307 242 (99.7) | 5 460 (97.9) | 5 206 (97.3) | 317 908 (99.6) |
| Yes | 932 (0.3) | 119 (2.1) | 144 (2.7) | 1 195 (0.4) |
| Health history | ||||
| Comorbidity diagnosis in prior 6 mo, no. (%) | ||||
| No | 262 428 (85.1) | 4 791 (85.9) | 4 542 (84.9) | 271 761 (85.2) |
| Yes | 45 746 (14.9) | 788 (14.1) | 808 (15.1) | 47 342 (14.8) |
| Total health care costs in prior 6 mo, $, median (IQR) | 335 (799) | 263 (772) | 275 (811) | 333 (799) |
| Patient-level medical costs, $, median (IQR) | ||||
| 0–3 mo | 1 004 (1 617) | 4 347 (9 853) | 7 265 (23 134) | 1 037 (1 715) |
| 4–6 mo | 114 (380) | 108 (427) | 153 (652) | 114 (384) |
| 7–9 mo | 107 (359) | 96 (377) | 114 (473) | 107 (361) |
| 10–12 mo | 106 (358) | 88 (335) | 106 (447) | 106 (359) |
| 0–12 mo | 1 868 (2 746) | 5 824 (11 438) | 9 214 (26 060) | 1 918 (2 920) |
| Population-level medical costs, $ | ||||
| 0–3 mo | 694 529 369 | 80 956 357 | 175 467 744 | 950 953 470 |
| 4–6 mo | 203 475 343 | 6 602 247 | 14 341 507 | 224 419 097 |
| 7–9 mo | 195 367 978 | 4 638 346 | 9 454 766 | 209 461 090 |
| 10–12 mo | 196 394 325 | 4 961 938 | 7 170 769 | 208 527 032 |
| 0–12 mo | 1 289 767 014 | 97 158 888 | 206 434 787 | 1 593 360 690 |
| Enrolled for at least 24 mo,a no. (%) | 151 594 (96.5) | 2 761 (1.8) | 2 718 (1.7) | 157 073 |
Note. IQR = interquartile range; TBI = traumatic brain injury. Exclusion criteria included the following: at least 12 months of enrollment, geographic information not available, and death caused by index.
Exclusion criteria included those listed in note above; however, enrollment was restricted to those with at least 24 months of enrollment. These values represent the subgroup analysis sample.
Individual-Level Costs
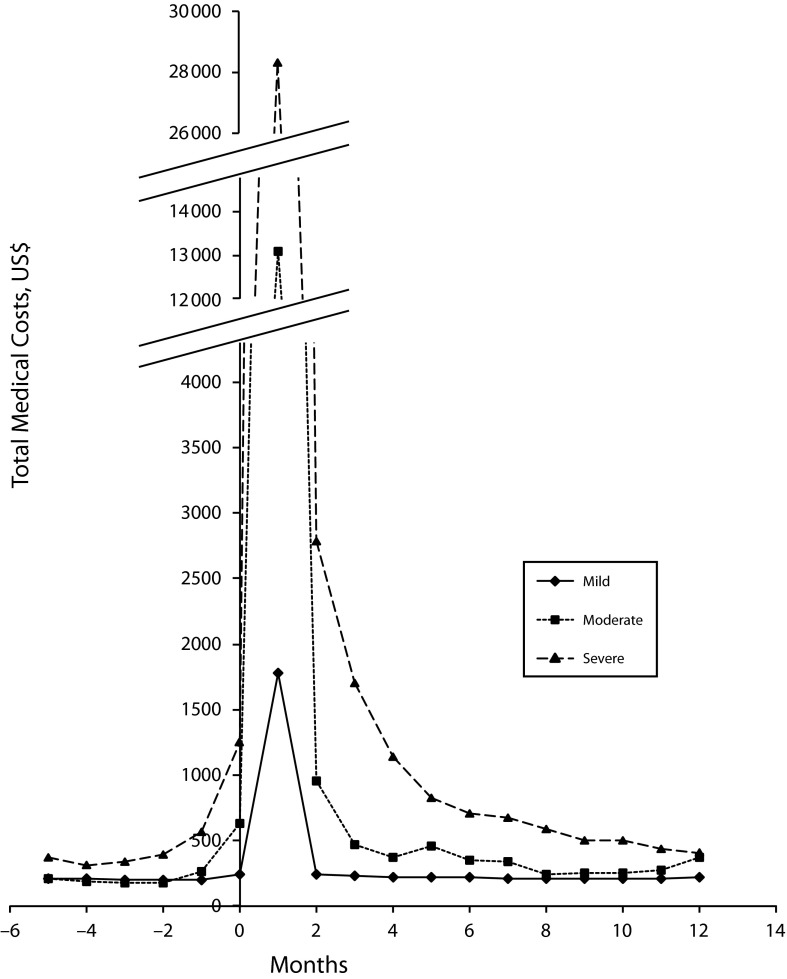
Across levels of severity, the median total health care costs in the 6 months before injury ranged from $263 to $335 (Table 1) in the primary sample. In the 3 months after injury, the median individual-level costs were $1004 for mild TBI, $4347 for moderate TBI, and $7265 for severe TBI cases; in subsequent time intervals, costs did not increase as much with severity (Table 1). By 12 months, health care costs were similar to preinjury costs (Figure 1). In the subgroup sample, increasing costs with worsening severity were observed in the first 12 months after injury but not in the second year after injury (see supplemental material available online).
FIGURE 1—
Unadjusted monthly total health care costs for patients diagnosed with traumatic brain injury: Sample of Patients, United States, January 1, 2007–December 31, 2010.
Note. Line graph shows mean costs for pediatric patients with mild, moderate, and severe traumatic brain injury (TBI) for 6 months before and 12 months after injury. The sample size was n = 319 103.
Log link and gamma family were GLM specifications for cost models supported by Box–Cox and modified Park tests. Multicollinearity was not observed for confounders in the adjusted models. Unadjusted GLM models showed that total costs 3 months after injury were 6 and 15 times higher among patients with moderate and severe TBI, respectively, compared with mild TBI (moderate TBI: CR = 6.44; 95% confidence interval [CI] = 5.79, 7.17 and severe TBI: CR = 14.55; 95% CI = 13.05, 16.23). Subsequent time intervals showed similar patterns of increasing costs with worsening severity (Table 2). However, this pattern was attenuated after adjusting for demographic and injury characteristics and health history (Table 2). Compared with mild TBI cases, adjusted total health care costs for moderate TBI cases were 5 times higher in the first 3 months after injury and 2 times higher in the 4 to 6 months after injury (CR = 4.91; 95% CI = 4.53, 5.32 and CR = 1.80; 95% CI = 1.53, 2.11 for each time interval, respectively); significant differences in costs between mild and moderate cases continued in subsequent time intervals. Adjusted total health care costs for severe TBI cases were significantly higher than those for mild TBI cases across all time periods (Table 2). Adjusted total health care costs for children with severe TBI were 11 times the costs of mild TBI cases in the first 3 months after injury (CR = 11.07; 95% CI = 10.19, 12.03). For the subgroup analysis, moderate and severe TBI cases had significantly higher adjusted total health care costs than mild TBI in the 2 years after injury, and differences were sustained in the second year after injury (Table 2).
TABLE 2—
Regression Analysis Comparing Patient-Level Medical Costs Across Levels of Severity: Sample of Patients, United States, January 1, 2007–December 31, 2010
| Unadjusted Analysis, CR (95% CI) |
Adjusted Analysis, CR (95% CI) |
|||
| Sample | Moderate TBI | Severe TBI | Moderate TBI | Severe TBI |
| Primary analysis,a mo | ||||
| 0–3 | 6.44 (5.79, 7.17) | 14.55 (13.05, 16.23) | 4.91 (4.53, 5.32) | 11.07 (10.19, 12.03) |
| 4–6 | 1.79 (1.42, 2.26) | 4.06 (3.21, 5.14) | 1.80 (1.53, 2.11) | 3.84 (3.26, 4.52) |
| 7–9 | 1.31 (1.07, 1.61) | 2.79 (2.27, 3.43) | 1.30 (1.10, 1.54) | 2.37 (1.99, 2.82) |
| 10–12 | 1.40 (1.13, 1.73) | 2.10 (1.69, 2.61) | 1.33 (1.12, 1.60) | 1.84 (1.54, 2.21) |
| Subgroup analysis,b mo | ||||
| 0–12 | 3.84 (3.31, 4.44) | 8.55 (7.38, 9.91) | 3.53 (3.27, 3.82) | 7.70 (7.10, 8.33) |
| 13–24 | 1.29 (1.08, 1.54) | 2.04 (1.70, 2.43) | 1.22 (1.05, 1.42) | 1.95 (1.67, 2.27) |
Note. CI = confidence interval; CR = cost ratio; TBI = traumatic brain injury. CRs compare the costs to the reference group (mild TBI) in each category. Adjusted regression analysis included the following covariates: age, gender, region, rurality, polytrauma, severe extremity injury, comorbidity diagnosis in the preceding 6 months, and total medical costs in the 6 months before index TBI. Separate models were conducted for each follow-up interval.
Exclusion criteria included the following: at least 12 months of enrollment, geographic region, and nonnegative costs at each time interval (n = 319 103).
Exclusion criteria include those listed in footnote a; however, enrollment was restricted to those with at least 24 months of enrollment (n = 157 073).
Population-Level Costs
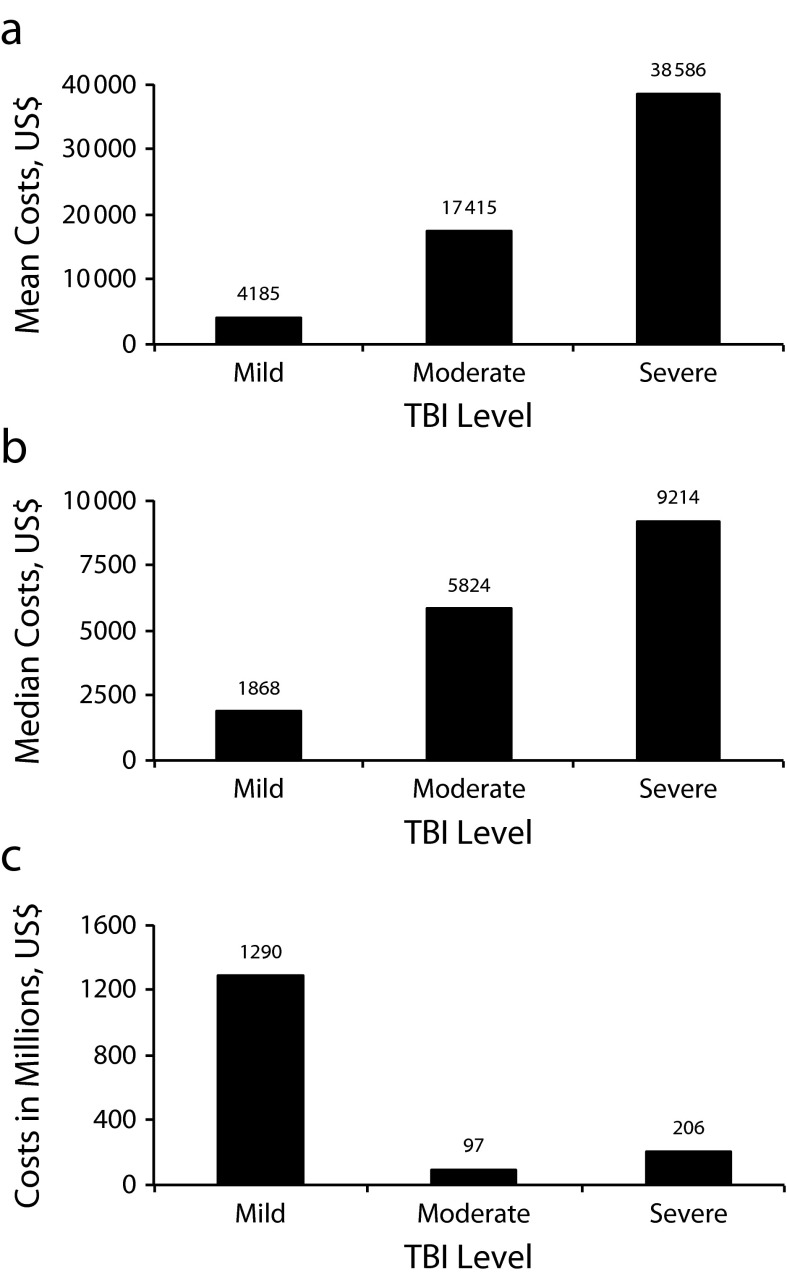
Total population-level costs for mild TBI were estimated at $695 million in the first 3 months after injury (Table 1). Comparatively, moderate and severe TBI costs were lower: $81 million and $175 million, respectively. To contrast the magnitude of difference between individual- and population-level costs, we compared total population costs using simple ratios of costs across levels of TBI severity. At the population level in all cases in the main analysis, based on 3-month total unadjusted health care costs reported in Table 1, moderate TBI costs were 88% less than mild TBI costs, and severe TBI costs were 75% less (moderate TBI: CR = 0.12; severe TBI: CR = 0.25; Figure 2).
FIGURE 2—
All-cause health care costs for the 12 months after pediatric traumatic brain injury across levels of severity by (a) mean patient-level costs, (b) median patient-level costs, and (c) population-level costs: Sample of Patients, United States, January 1, 2007–December 31, 2010.
Note. TBI = traumatic brain injury. The sample size was n = 319 103.
DISCUSSION
This study compared overall health care costs for pediatric patients with TBI across levels of severity and time since injury. Our study is unique in that it described health care costs from both inpatient and outpatient settings, allowing us to capture the full spectrum of pediatric TBI from mild to severe cases. We derived costs for all-cause health care utilization after injury, including care related to TBI sequelae that might not have been attributed to the TBI in the medical billing system, such as mental health care.
We found that patients with moderate and severe TBI initially generated per capita costs that were markedly higher than mild TBI after injury. These comparisons, however, were on the individual level; at the population level, the health care costs after mild TBI far exceeded those of moderate and severe TBI, as shown in Figure 2. This was simply a product of the extremely high population burden of mild TBI, which constituted 96.6% of all pediatric TBI cases that occurred in this population of commercially insured children from 2007 to 2010.
The results of this study align with research that has examined the high population burden of pediatric mild TBI. A population-based cohort study of children with TBI found that the proportion of children with disabilities 12 months after injury was significantly lower among those with mild TBI compared with moderate or severe TBI. However, the high incidence of mild TBI contributed greatly to the overall disability from TBI at the population level.25 The implications of our findings suggest that mild TBI prevention strategies are particularly important and that all mild TBI cannot be thought of as a low-cost, temporary problem with little or no long-term sequelae. It is possible that follow-up for mild TBI is needed, with strategies for screening for the reasons that led to long-term costs in this group. Future studies should examine reasons and patterns for postinjury visits after mild, moderate, and severe TBI, which can then inform postinjury health care practice in mild TBI.
Past research on the costs of pediatric TBI has principally utilized hospital charge data, such as the Healthcare Cost and Utilization Project Kids’ Inpatient Database.5,7 Few studies have addressed overall health care costs beyond the inpatient or emergency department setting. An analysis of MEPS data estimated the average per capita annual expenditure for mild and moderate TBI at $1044 (year 2000 US$), which approximates our 0- to 12-month median individual-level medical costs ($1868; Table 1) after accounting for inflation.26 Using commercial claims and Medicaid data, Peterson et al. assessed 1209 patients with inflicted TBIs (which are likely predominantly severe TBI).27 Compared with matched controls, inflicted TBI was associated with significantly greater medical service use and higher inpatient, outpatient, drug, and total costs for multiple years after the diagnosis. The estimated total medical cost attributable to inflicted TBI in the 4 years after diagnosis was $47 952 (95% CI = $40 219, $55 685) per patient with inflicted TBI (year 2012 US$) and differed for commercially insured ($38 231; 95% CI = $29 898, $46 564) and Medicaid ($56 691; 95% CI = $4290, $69 092) patients.27
In their population-based cohort study, Leibson et al. examined all-cause medical costs after TBI among residents (all ages) in 1 Minnesota county.4 Their findings supported ours: mild and symptomatic TBI (termed “probable” and “possible,” respectively) constituted most TBI cases and population-level costs. They concluded that preventing these injuries may result in substantially reduced medical costs.4 Further underscoring the high population-level costs of mild TBI in children, Miller et al. reported on disability-adjusted life years (DALYs) among children aged 0 to 4 years and showed that the annual DALY burden several years after mild inflicted TBI exceeded the DALY burden of a severe burn.28
Limitations
This study had several limitations. We relied on administrative data, which, although extensive in some regards, lacked clinical detail that medical records could have provided. We were therefore unable to classify TBI severity using traditional clinical indicators, as outlined in definitions such as those provided by the American Congress of Rehabilitation Medicine.29,30 It is possible that, because of the use of ICD-9–derived AIS-HN scores to determine severity, some misclassification by TBI severity may have occurred. Given the scope of this study, which described costs of care for more than 600 000 children with TBI, it would not be feasible to evaluate detailed clinical records. Because of the administrative nature of this data source, we could not control for patient-level factors known to influence health care utilization, such as pain and functioning. Although we controlled for several injury-related characteristics, including polytrauma and extremity injuries, it is possible that residual confounding by unmeasured characteristics might have occurred. Also, it is possible that a child may have experienced a second TBI during our study’s follow-up period, which we would be unable to distinguish from care related to the index TBI. The MarketScan data available for this study summarized health care expenditures from 2007 to 2010, which may be slightly dated. Costs in this study only referred to direct health care costs and did not capture indirect costs, such as time missed from work or transportation expenses. It is possible that severe TBI cases may have greater indirect costs than mild or moderate TBI cases. However, this study’s strength was its ability to capture out-of-pocket, copay, and covered costs across all clinical settings. Finally, we did not examine costs by mechanism of injury and did not have data available for analyzing DALY burden.
Conclusions
This was the first study to our knowledge to provide data on all-cause health care costs after pediatric TBI in a large, commercially insured population across the spectrum of TBI severity. We found that the population burden of costs in the year after TBI was primarily attributable to mild TBI. Although the long-term costs of severe TBI were significant at the individual level, the high population costs of mild cases suggested that mild TBI prevention strategies are particularly important.
Acknowledgments
The study was supported by funding from the National Institute of Neurologic Disorders and Stroke (grant R01 NS072308-03 to M. S. V.) and the HIPRC.
The authors thank Ali Rowhani-Rahbar for his valuable input on the analysis and methodology and Billy Kreuter for his assistance in acquiring and managing the data for this study.
Note. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Human Participant Protection
Data for this study were de-identified and do not directly involve human participants; therefore, this study was exempt from review by the University of Washington institutional review board.
References
- 1.Faul M, Xu L, Wald M, Coronado V. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations and Deaths 2002–2006. Atlanta, GA: Centers for Disease Control and Prevention; 2010. [Google Scholar]
- 2.Hu J, Ugiliweneza B, Meyer K, Lad S, Boakye M. Trend and geographic analysis for traumatic brain injury mortality and cost based on MarketScan database. J Neurotrauma. 2013;30(20):1755–1761. doi: 10.1089/neu.2013.2857. [DOI] [PubMed] [Google Scholar]
- 3.Jaffe KM, Massagli TL, Martin KM, Rivara JB, Fay GC, Polissar NL. Pediatric traumatic brain injury: acute and rehabilitation costs. Arch Phys Med Rehabil. 1993;74(7):681–686. doi: 10.1016/0003-9993(93)90024-5. [DOI] [PubMed] [Google Scholar]
- 4.Leibson CL, Brown AW, Hall Long K, et al. Medical care costs associated with traumatic brain injury over the full spectrum of disease: a controlled population-based study. J Neurotrauma. 2012;29(11):2038–2049. doi: 10.1089/neu.2010.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schneier AJ, Shields BJ, Hostetler SG, Xiang H, Smith GA. Incidence of pediatric traumatic brain injury and associated hospital resource utilization in the United States. Pediatrics. 2006;118(2):483–492. doi: 10.1542/peds.2005-2588. [DOI] [PubMed] [Google Scholar]
- 6.Schootman M, Buchman TG, Lewis LM. National estimates of hospitalization charges for the acute care of traumatic brain injuries. Brain Inj. 2003;17(11):983–990. doi: 10.1080/0269905031000110427. [DOI] [PubMed] [Google Scholar]
- 7.Shi J, Xiang H, Wheeler K, et al. Costs, mortality likelihood and outcomes of hospitalized US children with traumatic brain injuries. Brain Inj. 2009;23(7–8):602–611. doi: 10.1080/02699050903014907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O’Connor SS, Zatzick DF, Wang J, et al. Association between posttraumatic stress, depression, and functional impairments in adolescents 24 months after traumatic brain injury. J Trauma Stress. 2012;25(3):264–271. doi: 10.1002/jts.21704. [DOI] [PubMed] [Google Scholar]
- 9.Nampiaparampil DE. Prevalence of chronic pain after traumatic brain injury: a systematic review. JAMA. 2008;300(6):711–719. doi: 10.1001/jama.300.6.711. [DOI] [PubMed] [Google Scholar]
- 10.Ponsford J, Cameron P, Fitzgerald M, Grant M, Mikocka-Walus A. Long-term outcomes after uncomplicated mild traumatic brain injury: a comparison with trauma controls. J Neurotrauma. 2011;28(6):937–946. doi: 10.1089/neu.2010.1516. [DOI] [PubMed] [Google Scholar]
- 11.Blume HK, Vavilala MS, Jaffe KM, et al. Headache after pediatric traumatic brain injury: a cohort study. Pediatrics. 2012;129(1):e31–e39. doi: 10.1542/peds.2011-1742. [DOI] [PubMed] [Google Scholar]
- 12.Rockhill CM, Fann JR, Fan MY, Hollingworth W, Katon WJ. Healthcare costs associated with mild traumatic brain injury and psychological distress in children and adolescents. Brain Inj. 2010;24(9):1051–1060. doi: 10.3109/02699052.2010.494586. [DOI] [PubMed] [Google Scholar]
- 13.Brener I, Harman JS, Kelleher KJ, Yeates KO. Medical costs of mild to moderate traumatic brain injury in children. J Head Trauma Rehabil. 2004;19(5):405–412. doi: 10.1097/00001199-200409000-00005. [DOI] [PubMed] [Google Scholar]
- 14.National Center for Injury Prevention and Control. Report to Congress on Mild Traumatic Brain Injury in the United States: Steps to Prevent a Serious Public Health Problem. Atlanta, GA: Centers for Disease Control and Prevention; 2003. [Google Scholar]
- 15.Hansen L, Chang S. Health research data for the real world: the MarketScan databases. Available at: http://truvenhealth.com/portals/0/assets/PH_11238_0612_TEMP_MarketScan_WP_FINAL.pdf. Accessed January 22, 2014.
- 16.Truven Health Analytics. MarketScan studies: abbreviated bibliography. Available at: http://sites.truvenhealth.com/bibliography/2014TruvenHealthMarketScanBibliography.pdf. Accessed January 22, 2014.
- 17.Clark DE, Osler TM, Hahn DR. ICDPIC: Stata module to provide methods for translating International Classification of Diseases (Ninth Revision) diagnosis codes into standard injury categories and/or scores. Available at: http://econpapers.repec.org/software/bocbocode/s457028.htm. Accessed December 2, 2014.
- 18.Sánchez AI, Krafty RT, Weiss HB, Rubiano AM, Peitzman AB, Puyana JC. Trends in survival and early functional outcomes from hospitalized severe adult traumatic brain injuries, Pennsylvania, 1998 to 2007. J Head Trauma Rehabil. 2012;27(2):159–169. doi: 10.1097/HTR.0b013e3182074c41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greene NH, Kernic MA, Vavilala MS, Rivara FP. Validation of ICDPIC software injury severity scores using a large regional trauma registry. Inj Prev. 2015 doi: 10.1136/injuryprev-2014-041524. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 20.Blough DK, Madden CW, Hornbrook MC. Modeling risk using generalized linear models. J Health Econ. 1999;18(2):153–171. doi: 10.1016/s0167-6296(98)00032-0. [DOI] [PubMed] [Google Scholar]
- 21.Bombardier CH, Fann JR, Temkin NR, Esselman PC, Barber J, Dikmen SS. Rates of major depressive disorder and clinical outcomes following traumatic brain injury. JAMA. 2010;303(19):1938–1945. doi: 10.1001/jama.2010.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Diehr P, Yanez D, Ash A, Hornbrook M, Lin DY. Methods for analyzing health care utilization and costs. Annu Rev Public Health. 1999;20:125–144. doi: 10.1146/annurev.publhealth.20.1.125. [DOI] [PubMed] [Google Scholar]
- 23.Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. J Health Econ. 2005;24(3):465–488. doi: 10.1016/j.jhealeco.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 24.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20(4):461–494. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- 25.Rivara FP, Koepsell TD, Wang J, et al. Incidence of disability among children 12 months after traumatic brain injury. Am J Public Health. 2012;102(11):2074–2079. doi: 10.2105/AJPH.2012.300696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.US Bureau of Labor Statistics. Consumer price index inflation calculator. Available at: http://www.bls.gov/data/inflation_calculator.htm. Accessed April 22, 2015.
- 27.Peterson C, Xu L, Florence C, et al. The medical cost of abusive head trauma in the United States. Pediatrics. 2014;134(1):91–99. doi: 10.1542/peds.2014-0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miller TR, Steinbeigle R, Wicks A, Lawrence BA, Barr M, Barr RG. Disability-adjusted life-year burden of abusive head trauma at ages 0–4. Pediatrics. 2014;134(6):e1545–e1550. doi: 10.1542/peds.2014-1385. [DOI] [PubMed] [Google Scholar]
- 29.Menon DK, Schwab K, Wright DW, Maas AI. Position statement: definition of traumatic brain injury. Arch Phys Med Rehabil. 2010;91(11):1637–1640. doi: 10.1016/j.apmr.2010.05.017. [DOI] [PubMed] [Google Scholar]
- 30.Kay T, Harrington DE, Adams R, et al. Definition of mild traumatic brain injury. J Head Trauma Rehabil. 1993;8(3):86–87. [Google Scholar]