Kenney et al. reported that 54.5% of 4134 children were inadequately hydrated, as defined by a single urine osmolality (Uosm) of 800 or greater milliosmoles per kilogram of water.1 This “dehydration” threshold was inferred from experimental data first described in 1965,2 with subsequent studies on US, Jewish, German, and Swedish children demonstrating mean values above this threshold.3 Despite the lack of necessary corroborative data on plasma indicators of dehydration, Kenney at al. and others have come to the surprising conclusion that a majority of the world’s children are dehydrated. Of great public health concern is the potential detrimental effects of dehydration on cognitive performance.1 However, the data are not convincing: in the cited Italian study, the intervention and control groups were not considered separately in statistical analyses (reference 7 in article),1 and the cited Israeli study found a significant difference in only 10% (1/10 total) of cognitive tests (number span) with a possible gender bias confounding the result (reference 6 in article).1
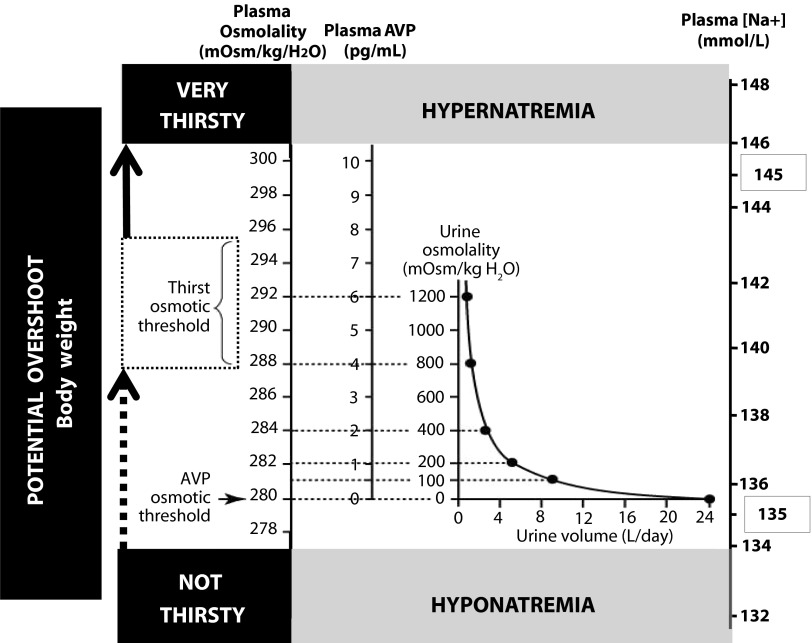
An alternative, physiology-based, interpretation of these data suggests that the majority of these children were in osmoregulatory balance, effectively conserving body water via osmotically appropriate arginine vasopressin (AVP) secretion and not dehydrated by clinically relevant, plasma-based, definitions.4 As shown in Figure 1, osmotically driven thirst stimulation occurs when plasma osmolality reaches a threshold of approximately 288 to 295 milliosmoles per kilogram of water, which corresponds to a Uosm of 800 to 1200 milliosmoles per kilogram of water and plasma sodium concentrations ([Na+]) within normal ranges. Although there is a high degree of individual variability in the osmotic thresholds for both thirst and AVP stimulation in humans, it is evident from the reported mean values that the children in the present study (except non-Hispanic Blacks) demonstrated Uosms below the average osmotic threshold for thirst stimulation—well within the normal physiological ranges for plasma AVP, osmolality, and [Na+]. Thus, the majority of children with a Uosm of 800 or more milliosmoles per kilogram of water were appropriately conserving fluids to maintain cellular hydration, although some at the very high ranges of Uosm may have met other standard criteria for dehydration. These well-known physiological relations serve to emphasize that measurement of urine osmolality, and particularly as a single measurement, cannot accurately predict body hydration status.
FIGURE 1—
Schematic representation of fluid homeostatic relationships between plasma osmolality, arginine vasopressin (AVP), and sodium concentration ([Na+]); urine osmolality and volume; osmotic thirst threshold; and clinically relevant natremia status.
Note. Normal plasma [Na+] is regulated between 135 and 145 mmol/L (normonatremia). Body weight is not a physiologically regulated variable, but is often used as a surrogate measure for fluid homeostasis.
Source. Adapted from Verbalis JG. Disorders of body water homeostasis. Best Pract Res Clin Endocrinol Metab. 2003;17(4):471–503.
The proposed health benefits of drinking fluids beyond regulatory need is unsubstantiated by scientific evidence,5 including a panel of experts assembled by the Institute of Medicine.6 And although the recommendation to drink more water seems harmless enough, the threat of drinking beyond thirst carries the risk of serious medical consequences from low blood [Na+] (dilutional hyponatremia), especially during exercise, and has resulted in the deaths of two high school athletes in the past year.7 Thus, we urge public health professionals to critically examine the physiological evidence underlying the use of a Uosm threshold of 800 milliosmoles per kilogram of water for “dehydration” before enacting policies encouraging children to drink beyond their thirst. The potential dangers may outweigh any perceived cognitive or health benefit, with the approximately 33% intake of sugar-sweetened beverages perhaps the more serious detriment to health.
Acknowledgments
The EAH (Exercise-Associated Hyponatremia) Panel members also include Mitchell H. Rosner, MD, University of Virginia Health System, Charlottesville; Sandra Fowkes-Godek, PhD, West Chester University, West Chester, PA; Jonathan P. Dugas, PhD, The Vitality Group, Chicago, IL; Martin D. Hoffman, MD, Veterans Affairs Northern California Health Care System and University of California Davis, Sacramento; Douglas P. Lewis, MD, Via Christi Hospitals Wichita, Inc, Wichita, KS; Ronald J. Maughan, PhD, Loughborough University, Leicestershire, UK; Kevin C. Miller, PhD, Central Michigan University, Mount Pleasant; Scott J. Montain, PhD, US Army Research Institute of Environmental Medicine, Natick, MA; Nancy J. Rehrer, PhD, University of Otago, Dunedin, New Zealand; William O. Roberts, MD, University of Minnesota, Minneapolis; Ian R. Rogers, MBBS, St John of God Murdoch Hospital and University of Notre Dame, Perth, Western Australia; Arthur J. Siegel, MD, Harvard Medical School, Boston, MA; Kristin J. Stuempfle, PhD, Gettysburg College, Gettysburg, PA. James M. Winger, MD, Loyola University Chicago Stritch School of Medicine, Chicago. Joseph G. Verbalis, MD, Georgetown University Medical Center, Washington, DC.
References
- 1.Kenney EL, Long MW, Cradock AL, Gortmaker SL. Prevalence of inadequate hydration among US children and disparities by gender and race/ethnicity: National Health and Nutrition Examination Survey, 2009–2012. Am J Public Health. 2015 doi: 10.2105/AJPH.2015.302572. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Katz AI, Massry S, Agmon J, Toor M. Concentration and dilution of urine in permanent inhabitants of hot regions. Isr J Med Sci. 1965;1(5):968–978. [PubMed] [Google Scholar]
- 3.Stookey JD, Brass B, Holliday A, Arieff A. What is the cell hydration status of healthy children in the USA? Preliminary data on urine osmolality and water intake. Public Health Nutr. 2012;15(11):2148–2156. doi: 10.1017/S1368980011003648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mange K, Matsuura D, Cizman B et al. Language guiding therapy: the case of dehydration versus volume depletion. Ann Intern Med. 1997;127(9):848–853. doi: 10.7326/0003-4819-127-9-199711010-00020. [DOI] [PubMed] [Google Scholar]
- 5.Valtin H. “Drink at least eight glasses of water a day.” Really? Is there scientific evidence for “8 x 8”? Am J Physiol Regul Integr Comp Physiol. 2002;283(5):R993–R1004. doi: 10.1152/ajpregu.00365.2002. [DOI] [PubMed] [Google Scholar]
- 6.Institute of Medicine of the National Academies. Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. Washington, DC: The National Academies Press; 2004. [Google Scholar]
- 7.Hew-Butler T, Rosner MH, Fowkes-Godek S et al. Statement of the Third International Exercise-Associated Hyponatremia Consensus Development Conference, Carlsbad, CA, 2015. Clin J Sport Med. 2015;25(4):303–320. doi: 10.1097/JSM.0000000000000221. [DOI] [PubMed] [Google Scholar]