The study of health disparities and the five areas of scientific training, seen from a transdisciplinary approach set forth in the article by Golden et al.,1 is one of the recent excellent contributions to addressing comprehensively the effects of health hazards in cardiovascular diseases (CVDs), which the biomedical focus has not been able to solve. Certainly, the creation of a research center with a transdisciplinary approach, which will contribute to reducing health disparities that generate CVDs in any population group, is a strategy that we must promote and enrich with lessons learned in other countries. In the case of scientific training in México, we are also incorporating into this transdisciplinary perspective an ecosystemic approach developed in Canada.2 In this sense, besides the multidisciplinary focus, the role of the socially involved actors stands out, above all with a proactive role of the population, with strategic alliances developed between the civil society organizations and the health system. Considering these alliances, we emphasize, from a transdisciplinary perspective, the development of scientific evidences of health disparities that lead to cardiovascular problems along two very relevant lines3,4:
disparities in the economic burden to the health system, the patients, and society as a whole, and
the identification of the social determinants that allow us to determine whether hypertension is a cause or an effect of a social disparity.
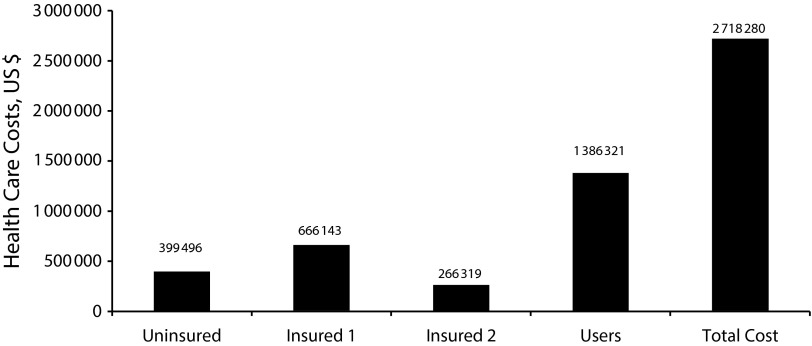
From the point of view of this transdisciplinary approach, we would like to highlight the importance of disparities in terms of catastrophic expenditures attributable to hypertension (> 30% of the family’s income) for patients and society as a whole. It is particularly important to point to the high economic cost to homes, when comparing with the cost to the state. Actually, as can be seen in Figure 1, health care costs for hypertension hit the pockets of patients and their families, so that of every US $100 spent on hypertension care in Mexico, US $52 come from patients’ pockets and US $48 from the health institutions.
FIGURE 1—
Health disparities in US $ from the economic burden of hypertension to providers and users in Mexico: 2013.
Note. Insured 1 = health providers to workers employed with companies; Insured 2 = health providers to workers employed with the state; Uninsured = health providers for nonsalaried workers.
Source. Arredondo et al.4
These evidences are particularly relevant because most of the out-of-pocket expense for care for this disease comes from homes belonging to the informal economy. Thus, a large number of patients with hypertension in Mexico do not have complete social protection for the disease or its complications and end up with out-of-pocket expenditures to cover more than half of the cost. This generates catastrophic expenditures, turning hypertension and its complications into an effect of a social disparity in the population that does not have complete social protection schemes for their health demands. But hypertension and its complications can also be a cause of social disparity, since families may be impoverished by the catastrophic health expenditure that is generated.
In this context and from a transdisciplinary approach, to decrease social disparities in health care costs for hypertension we propose, among other actions, the generation of a citizen observatory that, in alliance with the health systems, would monitor programs and resources for greater detection, promotion, and prevention of hypertension, and that would provide better control of complications in diagnosed cases and in patients undergoing treatment.
References
- 1.Golden SH, Ferketich A, Boyington J et al. Transdisciplinary cardiovascular and cancer health disparities training: experiences of the Centers for Population Health and Health Disparities. Am J Public Health. 2015;105(suppl 3):S395–S402. doi: 10.2105/AJPH.2014.302489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lebel J. Health: An Ecosystemic Approach. Ottawa, Ontario, Canada: International Development Research Centre; 2001. pp. 10–26. [Google Scholar]
- 3.Arredondo A, Zúñiga A. Epidemiological changes and financial consequences of hypertension in Latin America: implications for the health system and patients in Mexico. Cad Saúde. Cad Saude Publica. 2012;28(3):497–502. doi: 10.1590/s0102-311x2012000300010. [DOI] [PubMed] [Google Scholar]
- 4.Arredondo A, Aviles R, De Icaza E National Institute of Public Health. Costos de enfermedades crónicas en México. Cuernavaca, México: Informe Técnico de Memoria Metodológica; 2015. pp. 23–27. [Google Scholar]