Abstract
Objectives. We used electronic health record (EHR) data to determine rates and patient characteristics in offering cessation interventions (counseling, medications, or referral) and initiating quit attempts.
Methods. Ten community health centers in New York City contributed 30 months of de-identified patient data from their EHRs.
Results. Of 302 940 patients, 40% had smoking status recorded and only 34% of documented current smokers received an intervention. Women and younger patients were less likely to have their smoking status documented or to receive an intervention. Patients with comorbidities that are exacerbated by smoking were more likely to have status documented (82.2%) and to receive an intervention (52.1%), especially medication (10.8%). Medication, either alone (odds ratio [OR] = 1.9; 95% confidence interval [CI] = 1.5, 2.3) or combined with counseling (OR = 1.8; 95% CI = 1.5, 2.3), was associated with higher quit attempts compared with no intervention.
Conclusions. Data from EHRs demonstrated underdocumentation of smoking status and missed opportunities for cessation interventions. Use of data from EHRs can facilitate quality improvement efforts to increase screening and intervention delivery, with the potential to improve smoking cessation rates.
Smoking is the most preventable condition contributing to morbidity and mortality in the United States 1 and in New York City.2 Through combined efforts of public policy, taxation, and media campaigns, New York City has been able to reduce the rate of smoking over the past decade from 21% to 15%.3,4 However, more can be done. Research has demonstrated that providers’ advice can motivate patients to quit smoking.5,6 However, providers do not regularly document patients’ smoking status,7 thereby missing an opportunity to reduce smoking prevalence. Evidence shows that delivering both medication (nicotine replacement therapy or other prescription drugs) and counseling produces the highest rates of success in assisting smokers interested in quitting.8
The New York City Department of Health and Mental Hygiene has assisted community health centers (CHCs) and other providers in implementing health information technology and systems as a means to improve the delivery of clinical preventive services.9,10 Electronic health records (EHRs) can be useful to facilitate documentation of smoking status, which can increase smoking cessation interventions at primary care encounters,11 and may assist in the ultimate goal, getting patients to quit smoking. In addition, EHRs provide the opportunity to create patient registries,12 to track subpopulations, and to print lists of smokers so practices can schedule targeted visits, track whether patients receive interventions, facilitate documenting medication adherence,13 and track the success of various interventions if a standard definition of quit attempts is introduced. In addition, federal incentives have incorporated recording of smoking status with smoking cessation counseling delivery for smokers as a key metric for EHR adoption to demonstrate meaningful use,14 and market forces exerted by health plans and consumers continue to accelerate adoption15 of health information technology.
Studies have found that younger people, minorities,16 and Medicaid or uninsured smokers17 are less likely to receive smoking cessation interventions. The objective of this study was to use data extracted from the EHR to explore the patterns of patient characteristics (demographics, type of insurance, and comorbid conditions) associated with documentation of smoking status, the delivery of specific smoking cessation interventions, and quit attempts among smokers.
METHODS
Practices in this study were participants in a larger pilot program offering a modest financial incentive for increasing smoking cessation interventions, Health eQuits,18,19 a program implemented by the Primary Care Information Project (PCIP), a bureau of the New York City Department of Health and Mental Hygiene. We recruited CHCs from traditionally underserved neighborhoods with a higher prevalence of Medicaid insurance and patient smoking. To be eligible for Health eQuits, practices had to have been using an EHR system successfully for at least 1 year and had to be able to transmit aggregated EHR data to PCIP; PCIP identified 35 eligible health centers. Although 22 CHCs initially enrolled, only 19 were able to participate. All practices agreeing to participate in Health eQuits were to have adopted EHR software for at least 1 year with a system that typically had smoking cessation order sets, patient registry, and quality reporting capabilities and may also have included clinical decision support (point-of-care reminders).20 Of those 19 CHCs, 10 using eClinicalWorks software agreed to provide de-identified patient-level data to allow for further analysis.
Data Definitions
The de-identified data included information on patients aged 18 years or older, dates of office visits, medications, diagnoses, counseling, smoking status, and patient demographics (e.g., gender, age, race/ethnicity, and insurance status) from October 1, 2009, through March 31, 2012.
We derived smoking documentation from a structured data field in the EHR, the SmartForm (SF). Options for smoking status were “current smoker,” “former smoker,” or “nonsmoker” (a view is provided in Figure A, available as a supplement to the online version of this article at http://www.ajph.org). We defined a patient as a smoker if the SF indicated “current smoker” at any time during the study period. We defined a patient as a nonsmoker if the SF only indicated “nonsmoker” during the study period, and as a former smoker if the SF had “former smoker” but never “current smoker” during the study period. In addition, we defined subcategories based on the Centers for Medicare and Medicaid Services Meaningful Use incentives (every day smoker, some day smoker, unknown status).21 Number of cigarettes smoked per day was also recorded on a 1-to-5 scale (1: 1–5; 2: 6–10; 3: 11–20; 4: 21–30; 5: ≥ 31).
We recorded 3 types of cessation interventions: (1) medication (nicotine replacement therapy, varenicline, or bupropion), (2) counseling by a health care clinician on the benefits of quitting, or (3) referral to a state quit line, commonly referred to as “fax-to-quit.” The definition of counseling was left to the discretion of the provider, as long as an accepted procedure terminology code for smoking cessation counseling (99406 or 99407) was selected at any visit.
We grouped disease states or chronic conditions that are causally associated with smoking according to International Classification of Diseases, Ninth Revision codes22 (a complete list is available in Table A, available as a supplement to the online version of this article at http://www.ajph.org) into cardiovascular diseases: ischemic vascular disease, stroke, abdominal aortic aneurysm; respiratory diseases: chronic obstructive pulmonary disease, bronchitis, emphysema; cancers: lung, bladder, kidney, cervix, esophagus, stomach, pancreas, oral cavity, and acute myelogenous leukemia; osteoporosis; reproductive problems: infertility, premature birth, small for gestational age, stillbirths, and sudden infant death23; and cardiovascular disease risk factors: hypertension, diabetes mellitus, dyslipidemia, obesity, and physical inactivity.
For this analysis, at least 2 visit entries with SF completed were required to identify a quit attempt. We identified a quit attempt through a change in smoking status on the SF (i.e., when a patient’s smoking status on the SF changed from “current smoker” to “former smoker” as the last recorded status). For each patient, only 1 quit attempt could be recorded.
Analysis
We analyzed data in SAS version 9.2 (SAS Institute, Cary, NC). We generated simple descriptive statistics for each patient characteristic and identified by smoking status and type of cessation intervention (i.e., counseling, medication, or referral). We used the χ2 test to assess significance between groups by gender, age, race, types of insurance, and receipt of cessation interventions.
We used multivariable logistic regression to examine the effect of smoking cessation interventions on quit attempts, with control for effects by CHC, patient characteristics, types of insurance, and whether the patient was a heavy smoker. To take into account the possibility that younger women might have unique reproductive considerations as smokers, we included an interaction term for gender and age in the models; we also evaluated a possible interaction between the number of cigarettes per day and existence of comorbidities.
RESULTS
A total of 302 940 patient records were available for this study (Table 1). Overall, 40.1% (121 694) of patients had documentation as current smokers, former smokers, or nonsmokers. There were disparities among patients with and without a recorded smoking status. Whereas women represented 77.6% of the population, only 38.4% of women had smoking status documented within the SF. Similarly, patients aged 18 to 34 years and patients without insurance (self-pay) were 65.0% and 26.8% of the population, respectively, but only 39.4% and 36.7% of those were documented. By contrast, those with a comorbid condition represented 10.5% of the population but 82.2% had smoking status documented. Results by race were limited as 28% had missing values. Statistically significant differences were found for SF completion by all patient characteristics listed in Table 1.
TABLE 1—
Demographic Characteristics by Smoking Status: 10 New York City Community Health Centers, 2009–2012
| Variablea | No. (Overall %) | Not Documented, No. (%) or % | Documented, No. (%) or % | P | Current Smoker, No. (%) or % | Former Smoker, No. (%) or % | Nonsmoker, No. (%) or % | P |
| Total | 302 940 (100) | 181 246 (59.9) | 121 694 (40.1) | 35 057 (28.8) | 14 116 (11.6) | 72 521 (59.6) | ||
| Gender | ||||||||
| Male | 67 868 (22.4) | 53.5 | 46.5 | 49.2 | 15.0 | 35.8 | ||
| Female | 234 926 (77.6) | 61.6 | 38.4 | < .001 | 21.7 | 10.4 | 67.9 | < .001 |
| Age, y | ||||||||
| 18–34 | 193 643 (65.0) | 60.6 | 39.4 | 22.6 | 9.7 | 67.6 | ||
| 35–64 | 94 652 (31.8) | 56.3 | 43.7 | 41.1 | 13.8 | 45.1 | ||
| ≥ 65 | 9 867 (3.3) | 58.3 | 41.7 | < .001 | 19.8 | 23.7 | 56.5 | < .001 |
| Race/ethnicity | ||||||||
| American Indian | 902 (0.4) | 49.6 | 50.4 | 22.1 | 7.2 | 70.8 | ||
| Asian | 8 613 (3.7) | 49.0 | 51.0 | 18.6 | 12.4 | 69.0 | ||
| Black | 98 828 (39.2) | 46.5 | 53.5 | 31.7 | 10.6 | 57.7 | ||
| Hispanic | 3 245 (34.6) | 45.4 | 54.6 | 25.7 | 11.2 | 63.1 | ||
| Others | 54 161 (6.2) | 54.8 | 45.2 | 26.8 | 11.0 | 62.3 | ||
| White | 51 771 (16.0) | 48.6 | 51.4 | < .001 | 30.8 | 15.3 | 54.0 | < .001 |
| Insuranceb | ||||||||
| Commercial | 124 959 (41.3) | 45.9 | 54.1 | < .001 | 33.4 | 11.9 | 54.6 | < .001 |
| Medicaid | 125 852 (41.5) | 43.0 | 57.0 | < .001 | 34.0 | 11.2 | 54.8 | < .001 |
| Medicare | 8 438 (2.8) | 41.9 | 58.1 | < .001 | 35.9 | 19.6 | 44.5 | < .001 |
| Self-pay | 81 175 (26.8) | 63.3 | 36.7 | < .001 | 30.4 | 12.1 | 57.6 | < .001 |
| Others | 60 (0.0) | 38.3 | 61.7 | < .001 | 27.0 | 16.2 | 56.8 | .68 |
| Comorbidityc | ||||||||
| Cardiovascular | 1 353 (0.5) | 12.9 | 87.1 | < .001 | 46.6 | 18.1 | 35.3 | < .001 |
| Respiratory | 1 114 (0.4) | 12.2 | 87.8 | < .001 | 74.9 | 17.4 | 7.8 | < .001 |
| Osteoporosis | 1 967 (0.7) | 7.5 | 92.5 | < .001 | 24.3 | 14.0 | 61.7 | < .001 |
| Cardiovascular disease risks | 30 587 (10.1) | 18.0 | 82.0 | < .001 | 38.8 | 16.4 | 44.7 | < .001 |
| No comorbidity | 271 192 (89.5) | 64.7 | 35.3 | < .001 | 26.0 | 10.3 | 63.7 | < .001 |
| Any comorbidity | 31 748 (10.5) | 17.9 | 82.2 | < .001 | 39.1 | 16.3 | 44.6 | < .001 |
The “overall” column represents column percentages by demographic category. For example, under the “Gender” category, the rows for male and female demographics add to 100% of the category. Data in columns 3, 4, 6, 7, and 8 represent row percentages. For example, current plus former plus nonsmoker add up to 100% for men.
More than 1 insurance type is possible for each patient.
More than 1 condition is possible for each patient.
Of the patients with a recorded smoking status, 28.8% were identified as current smokers, 11.6% as former smokers, and 59.6% as nonsmokers (Table 1). Among the demographic categories, the following groups of patients made up a higher proportion of current smokers than former smokers or nonsmokers: men (49.2% vs 15.0% and 35.8%, respectively), patients with cardiovascular conditions (46.6% vs 18.1% and 35.3%, respectively), and patients with respiratory conditions (74.9% vs 17.4% and 7.8%, respectively). Only 44.6% of patients with any comorbid condition were nonsmokers, compared with 63.7% of patients with no comorbidity (Table 1).
Of the current smokers, 65.7% did not receive any cessation interventions (Table 2), 19.2% received counseling only, 13.3% received medication with or without counseling, and 1.8% were referred to the state quit line. More men who were classified as current smokers (46.9%) received any cessation intervention than did women (24.3%), more patients aged 35 to 64 years (45.8%) received an intervention than did other age groups (18–34 years: 22.7%; ≥ 65 years: 41.3%), and 50.0% of patients with Medicare insurance received an intervention. More than 50% of patients with smoking-related comorbidities or risk factors for cardiovascular diseases received an intervention, with the exception of patients with osteoporosis. Male smokers, those aged 35 to 64 years, those with Medicare insurance, and smokers with comorbidities (except osteoporosis) were most likely to receive medication, with or without counseling. We observed no differences according to interaction terms by age.
TABLE 2—
Demographic Characteristics of Smokers by Smoking Cessation Intervention Type (Row %): 10 New York City Community Health Centers, 2009–2012
| Variable | No Intervention, No. (%) or % | Counseling Only, No. (%) or % | Medication Only, No. (%) or % | Both, No. (%) or % | Fax-to-Quit, No. (%) or % | Total, No. (%) or No. | P |
| Total | 23 018 (65.7) | 6725 (19.2) | 1934 (5.5) | 2748 (7.8) | 632 (1.8) | 35 057 (100) | |
| Gender | |||||||
| Male | 53.1 | 25.5 | 6.8 | 12.8 | 1.7 | 15 535 | |
| Female | 75.7 | 14.1 | 4.5 | 3.9 | 1.9 | 19 518 | < .001 |
| Age, y | |||||||
| 18–34 | 77.3 | 15.2 | 2.7 | 3.5 | 1.3 | 17 246 | |
| 35–64 | 54.2 | 23.1 | 8.2 | 12.2 | 2.3 | 16 994 | |
| ≥ 65 | 58.7 | 21.5 | 8.3 | 8.1 | 3.4 | 816 | < .001 |
| Race/ethnicity | |||||||
| American Indian | 72.1 | 17.4 | 4.7 | 4.7 | 1.2 | 86 | |
| Asian | 77.7 | 16.6 | 2.3 | 2.7 | 0.7 | 771 | |
| Black | 60.1 | 21.2 | 6.5 | 9.8 | 2.5 | 14 511 | |
| Hispanic | 69.5 | 16.8 | 5.9 | 6.3 | 1.6 | 10 562 | |
| Others | 69.0 | 15.7 | 6.5 | 6.7 | 2.0 | 1 621 | |
| White | 66.3 | 20.3 | 3.9 | 8.6 | 0.8 | 5 515 | < .001 |
| Insurancea | |||||||
| Commercial | 68.9 | 15.7 | 6.6 | 6.4 | 2.4 | 16 984 | < .001 |
| Medicaid | 61.5 | 20.0 | 6.8 | 9.6 | 2.1 | 24 434 | < .001 |
| Medicare | 50.0 | 25.9 | 9.4 | 12.5 | 2.2 | 1 759 | < .001 |
| Self-pay | 62.6 | 21.6 | 4.5 | 10.2 | 1.2 | 9 016 | < .001 |
| Others | 70.0 | 10.0 | 10.0 | 0.0 | 10.0 | 10 | .254 |
| Comorbidityb | |||||||
| Cardiovascular | 39.9 | 26.6 | 12.8 | 17.9 | 2.9 | 549 | < .001 |
| Respiratory | 28.4 | 23.9 | 17.2 | 26.9 | 3.6 | 732 | < .001 |
| Osteoporosis | 62.9 | 16.3 | 10.6 | 7.9 | 2.3 | 442 | < .001 |
| Cardiovascular disease risk | 47.8 | 23.3 | 10.8 | 15.3 | 2.9 | 9 734 | < .001 |
| No comorbidity | 73.0 | 17.6 | 3.4 | 4.7 | 1.4 | 24 860 | < .001 |
| Any comorbidity | 47.9 | 23.2 | 10.8 | 15.4 | 2.9 | 10 197 | < .001 |
More than 1 insurance type is possible for each patient.
More than 1 condition is possible for each patient.
A total of 1191 quit attempts were documented in this data set (3.4% of current smokers). Compared with no smoking cessation intervention, the quit attempt rate for smokers with a documented receipt of medication only was highest (odds ratio [OR] = 1.9; 95% confidence interval [CI] = 1.5, 2.3), followed by both medication and counseling (OR = 1.8; 95% CI = 1.5, 2.3; Table 3). There was no difference for patients who received a fax-to-quit intervention (OR = 1.2; 95% CI = 0.8, 1.8) or counseling only (OR = 0.9; 95% CI = 0.8, 1.1). However, including the number of visits or number of SFs completed in the model reduced the effect of treatment on the quit rate (data not shown). Female (OR = 2.2; 95% CI = 1.7, 2.8) and older smokers (aged 35–64 years: OR = 1.8; 95% CI = 1.4, 2.2; aged ≥ 65 years: OR = 3.0; 95% CI = 1.9, 4.7) were more likely to have documented quit attempts. The interaction between age and gender was significant (OR = 0.5; 95% CI = 0.4, 0.7; and OR = 0.4; 95% CI = 0.2, 0.8), indicating that younger women (aged 18–34 years) and older men (aged ≥ 35 years) were more likely to have documented quit attempts.
TABLE 3—
Odds Ratio of Quit Attempts by Intervention Type and Patient Characteristics: 10 New York City Community Health Centers, 2009–2012
| Variable | OR (95% CI) |
| Intervention for smokers | |
| Counseling only | 0.9 (0.8, 1.1) |
| Medication only | 1.9 (1.5, 2.3) |
| Both | 1.8 (1.5, 2.3) |
| Fax-to-quit | 1.2 (0.8, 1.8) |
| No intervention (Ref) | 1.0 |
| Gender | |
| Female | 2.2 (1.7, 2.8) |
| Male (Ref) | 1.0 |
| Age group | |
| 18–34 (Ref) | 1.0 |
| 35–65 | 1.8 (1.4, 2.2) |
| ≥ 65 | 3.0 (1.9, 4.7) |
| Gender × age | |
| Female: 35–64 y | 0.5 (0.4, 0.7) |
| Female: ≥ 65 y | 0.4 (0.2, 0.8) |
| Daily smokers | |
| Yes | 0.6 (0.5, 0.7) |
| Missing | 0.7 (0.5, 1.0) |
| No (Ref) | 1.0 |
| Number of cigarettes | |
| 1–5 (Ref) | 1.0 |
| 6–10 | 0.7 (0.6, 0.8) |
| 11–20 | 0.5 (0.4, 0.7) |
| 21–30 | 0.4 (0.3, 0.6) |
| ≥ 31 | 0.4 (0.2, 0.7) |
| Missing | 0.9 (0.6, 1.4) |
| Insurancea | |
| Commercial | 1.9 (1.6, 2.2) |
| Self-pay | 1.5 (1.2, 1.9) |
| Medicaid | 1.5 (1.3, 1.8) |
| Medicare | 1.5 (1.1, 1.9) |
| Community health center | |
| A | 0.4 (0.3, 0.6) |
| B | 1.3 (1.0, 1.6) |
| C | 0.7 (0.5, 1.2) |
| D | 1.4 (1.0, 1.8) |
| E (Ref) | 1.0 |
| F | 0.8 (0.6, 1.2) |
| G | 0.8 (0.6, 1.0) |
| H | 1.5 (1.0, 2.2) |
| I | 1.1 (0.8, 1.5) |
| J | 1.9 (1.4, 2.5) |
Note. CI = confidence interval; OR = odds ratio. The sample size was n = 1191.
Reference for each insurance type is group without that insurance type.
Daily smokers were less likely to have documented quit attempts (OR = 0.6; 95% CI = 0.5, 0.7) and the number of cigarettes was inversely associated with documented attempts to quit. We found no interaction between number of cigarettes and comorbidities. Nicotine replacement represented 81% of prescribed medications, varenicline 17%, and bupropion 2%.
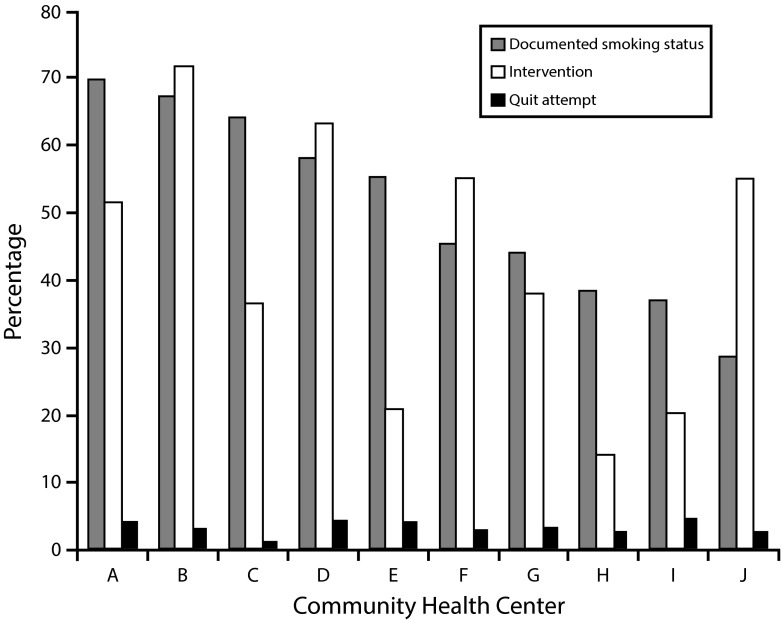
There was a wide variation of documentation and intervention by CHC (Figure 1). Consistently across CHCs, we observed very few quit attempts in comparison with the total population of smokers that could or did receive a cessation intervention.
FIGURE 1—
Documentation of smoking status and intervention by community health center: 10 New York City community health centers, 2009–2012.
Note. Documentation of smoking status, smoking cessation intervention and quit attempt by community health center (CHC) varied widely. Bar graphs show proportion of population per CHC that were documented, identified as current smokers, given a cessation intervention, and attempted quit. For example, for CHC “A,” 78% of their patients had smoking status documented, nearly 46% were current smokers, 33% received an intervention (or 71% intervention rate with smokers), and fewer than 5% attempted to quit.
DISCUSSION
We used EHR data from more than 300 000 patients and identified screening for smoking and cessation intervention disparities among patients according to demographic patterns. Women, younger patients, and the uninsured were less likely to have smoking status recorded and women and younger patients were less likely to be offered an intervention. By contrast, patients with a diagnosis of chronic illness or comorbid condition exacerbated by smoking were more likely to have smoking status documented and interventions offered.
To use data collected from EHRs for quality improvement, we need to accept that there are limitations to such data sources. Documentation of patients’ smoking status, history, or interventions in unstructured note sections would not be captured in this data set. In earlier research, PCIP found that only 53% of patients with smoking status recorded in the EHR were captured in the SF, with the remainder of smokers listed in unstructured sections.24 Thus, EHR-derived measures can undercount practice performance in quality improvement activities. Quit rates based on EHR data are not standardized and generally have not been reported.11 In our analysis, quit rates were calculated conservatively, based on documentation of smoking status during an office visit, but patients may not have mentioned a change in smoking status during a visit. Our data may underestimate the number of smokers or interventions in this population.
On the other hand, the quit rate in this sample is much lower than those reported in a national survey25 for several possible reasons: (1) episodic data may not capture as many occurrences with a relapsing condition; (2) quit attempts per se were not predefined within the EHR and, unlike other quality improvement targets, there is no standard definition currently in use; (3) for patients who were identified as having a smoking status change, the documentation does not represent an actual quit rate; and (4) the study did not identify quit attempts with a cotinine measurement to confirm smoking abstinence.26 Still, the quit attempt data reported here captures patient characteristics and provides insight useful in reporting the smoking cessation program results.
Although there are many published reports of organizations using EHRs to improve smoking cessation efforts,11,27,28 our program is unique because we targeted a more challenging population—Medicaid patients at unaffiliated EHR-enabled centers in underserved urban neighborhoods. In addition, our patient-level results identify disparities for women and younger patients, differing from earlier smoking cessation reports.16,17,29,30 Our results do not mirror other reports in the literature in relation to racial or insurance disparities,16,17 but agree with earlier findings that patients with comorbid conditions were more likely to have smoking status recorded and counseling provided.29–31
In this study population, proportionately fewer former smokers were recorded in comparison with current smokers, whereas reports in the literature25 and a community survey report relatively equal or greater proportion of former and current smokers.4 This bias is somewhat expected as the study focuses on 10 CHCs and this health care setting typically serves primarily Medicaid patients who have reported higher percentage of smokers. In addition, as these centers recently adopted EHR software, documentation of current smokers over former smokers or nonsmokers may have taken precedence to ensure transition of key patient medical problems, diagnoses, and vital information from paper to electronic records.24 Nevertheless, there is ample opportunity to prescribe medications or offer counseling; not doing so translates into missed opportunities for increased quit attempts.
Patterns of interventions with documented smokers differ from reports in the literature. The fax-to-quit option, which provides a standardized curriculum for counseling at state centers proven effective in other programs32 was infrequently used and was not associated with quit attempts. A Morbidity and Mortality Weekly Report highlighted the use of cessation medications more often than counseling and attributes over-the-counter availability as a facilitator.25 However, the current results show that counseling was more likely to be offered than other interventions and this may be attributable to the practice preference of clinicians in the CHC setting or changes in 2011 Medicaid benefits to reimburse for counseling. Rates of counseling intervention also varied widely across the centers and this may be a reflection of differences in clinician comfort with counseling on smoking cessation, as counseling was not standardized.33
Similar to reports in the literature, cessation intervention activities were more prevalent when patients had comorbidities that are exacerbated by smoking.29–31 Consistent with published reports,8,34 with a combination of medication and counseling, more quit attempts were observed in this data set than either alone, and medication was more effective than counseling. However, these published reports also indicated that counseling alone may be effective, at least among patients expressing an interest in quitting; our data did not show an effect of counseling alone on quit attempts. Future initiatives may need to incorporate patient interest and focus on consistency in counseling techniques to be able to observe a positive effect of counseling alone.
Limitations
Several limitations of the study results are presented here. Counseling was not standardized for providers. Data used in this study had to be derived from structured fields within the EHRs. Because of technical issues with EHR software connecting to facsimile servers, the data collected for the fax-to-quit referral rate may be underreported or underdocumented. Furthermore, the data cannot determine whether the patient or the provider initiated requests for a cessation intervention, or the effect that may have had on quit attempts. Multiple quit attempts per patient were not determined, making underestimation of total quit attempts possible. The higher rate of quit attempts in younger women may have been related to family planning considerations, but capturing such data was beyond the scope of this project.
Previous publications addressing smoking cessation have suggested that system-level changes making tobacco screening and referral routine are needed to improve smoking cessation interventions in the United States.35,36 With the increasing availability of EHRs, information technology can be harnessed to increase screening patients for tobacco use as well as to improve the delivery of smoking cessation interventions within a continuous quality improvement process. Although it is never too late to quit, mortality is reduced and health benefits are optimized when the youngest smokers quit.37 Ending age and gender disparities by identifying opportunities for improved clinical prevention can be more immediate because data are now available electronically. Clinicians could use reports on their patients to identify systematic changes to their practice to better deliver intervention. Increasing to 50% intervention could dramatically increase the number of smokers to attempt to quit.
These findings suggest areas to target when one is designing interventions with CHCs. A focus on documenting smoking status at every visit continues to be a necessary first step in smoking cessation interventions; all smokers, not just those with comorbidities, should receive medical attention. Providers need to take the initiative to discuss smoking cessation, rather than wait for patients to make requests. To improve the association between counseling and quit attempts, future programs could incorporate a standardized patient counseling script or protocol as well as encourage providers to print a summary of the counseling to share with each patient after each counseling session.
Examples of EHR applications that were available within the PCIP and could be included by other centers include using decision support reminders (e.g., refer all smokers to cessation programs),38 emphasizing the effectiveness of medication,28 creating order sets, providing quality measure feedback27 (e.g., reviewing summary reports on number of patients with smoking status documented and smokers that received a cessation intervention), creating registries within the EHRs12 (e.g., generating lists of patients who have gone from “current smoker” to “former smoker”), and employing a panel manager to conduct outreach to smokers for additional office visits or phone calls or e-mails to encourage patients to quit.39
As documentation of smoking status continues to be the first step in smoking cessation efforts, centers that use EHRs may consider spreading the smoking assessment and intervention across the health care team, rather than leaving it all on the shoulders of clinicians, by assigning ancillary staff responsibility for tracking smoking status at every visit.7,27 Practices could implement policies, such as offering effective smoking cessation interventions to each smoker as part of every medical encounter, and in multispecialty centers, integrating screening and interventions as routine work flow across disciplines, including dentists, pharmacists, and nurses.40 Quality improvement programs could prioritize preventive services for the most advanced cases.
More advanced use of health information technology in the future may allow clinicians to obtain feedback from text searches, locating smoking status documentation in other than structured data field locations; to obtain pharmacy claims as a method to track smoking cessation medication adherence13; and to use the personal health record to connect smokers directly with support for quitting, similar to earlier mobile phone application attempts.41
Conclusions
In summary, data from EHRs at 10 CHCs demonstrated underdocumentation of smoking status and missed opportunities for cessation interventions. Interventions were disproportionately low for women and younger smokers. Medication, with or without counseling, was associated with higher quit attempt rates compared with no intervention. Using data from EHRs can facilitate future quality improvement efforts to increase smoking cessation interventions.
Acknowledgments
This study was funded by a Centers for Disease Control and Prevention Communities Putting Prevention to Work grant.
Human Participant Protection
The institutional review board of the New York City Department of Health and Mental Hygiene approved this study, and waived patient informed consent (institutional review board number 10-086).
References
- 1.Farley TA, Dalal MA, Mostashari F, Frieden TR. Deaths preventable in the US by improvements in use of clinical preventive services. Am J Prev Med. 2010;38(6):600–609. doi: 10.1016/j.amepre.2010.02.016. [DOI] [PubMed] [Google Scholar]
- 2. NYC Quits. Available at: https://a816-nycquits.nyc.gov/pages/why.aspx. Accessed December 11, 2013.
- 3. New York City Department of Health and Mental Hygiene. Community Health Survey 2002. Available at: https://a816-healthpsi.nyc.gov/SASStoredProcess/guest?_PROGRAM=%2FEpiQuery%2FCHS%2FchsX&year=2002&strat1=none&strat2=none&qtype=univar&var=rsmoke3&crude=no. Accessed June 25, 2013.
- 4. New York City Department of Health and Mental Hygiene. Community Health Survey 2011. Available at: https://a816-healthpsi.nyc.gov/SASStoredProcess/guest?_PROGRAM=%2FEpiQuery%2FCHS%2FchsX&year=2011&strat1=none&strat2=none&qtype=univar&var=rsmoke3&crude=no. Accessed June 25, 2013.
- 5.Kreuter MW, Chheda SG, Bull FC. How does physician advice influence patient behavior? Evidence for a priming effect. Arch Fam Med. 2000;9(5):426–433. doi: 10.1001/archfami.9.5.426. [DOI] [PubMed] [Google Scholar]
- 6.Bao Y, Duan N, Fox SA. Is some provider advice on smoking cessation better than no advice? An instrumental variable analysis of the 2001 National Health Interview Survey. Health Serv Res. 2006;41(6):2114–2135. doi: 10.1111/j.1475-6773.2006.00592.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCullough A, Fisher M, Goldstein AO, Kramer KD, Ripley-Moffitt C. Smoking as a vital sign: prompts to ask and assess increase cessation counseling. J Am Board Fam Med. 2009;22(6):625–632. doi: 10.3122/jabfm.2009.06.080211. [DOI] [PubMed] [Google Scholar]
- 8.Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff. A clinical practice guideline for treating tobacco use and dependence: 2008 update. A US Public Health Service Report. Am J Prev Med. 2008;35(2):158–176. doi: 10.1016/j.amepre.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frieden TR, Mostashari F. Health care as if health mattered. JAMA. 2008;299(8):950–952. doi: 10.1001/jama.299.8.950. [DOI] [PubMed] [Google Scholar]
- 10.Mostashari F, Tripathi M, Kendall M. A tale of two large community electronic health record extension projects. Health Aff (Millwood) 2009;28(2):345–356. doi: 10.1377/hlthaff.28.2.345. [DOI] [PubMed] [Google Scholar]
- 11.Boyle R, Solberg L, Fiore M. Use of electronic health records to support smoking cessation. Cochrane Database Syst Rev. 2011;12:CD008743. doi: 10.1002/14651858.CD008743.pub2. [DOI] [PubMed] [Google Scholar]
- 12.Wright A, McGlinchey EA, Poon EG, Jenter CA, Bates DW, Simon SR. Ability to generate patient registries among practices with and without electronic health records. J Med Internet Res. 2009;11:e31. doi: 10.2196/jmir.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenbaum L, Shrank WH. Taking our medicine—improving adherence in the accountability era. N Engl J Med. 2013;369(8):694–695. doi: 10.1056/NEJMp1307084. [DOI] [PubMed] [Google Scholar]
- 14. 2014 Clinical quality measures (CQMs) adult recommended core measures. Available at: http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/2014_CQM_AdultRecommend_CoreSetTable.pdf. Accessed October 15, 2014.
- 15. Deloitte Center for Health Solutions. Physician adoption of health information technology: implications for medical practice leaders and business partners. Available at: http://www2.deloitte.com/content/dam/Deloitte/us/Documents/life-sciences-health-care/us-lshc-physician-adoption-10012014.pdf. Accessed October 15, 2014.
- 16.Browning KK, Ferketich AK, Salsberry PJ, Wewers ME. Socioeconomic disparity in provider-delivered assistance to quit smoking. Nicotine Tob Res. 2008;10(1):55–61. doi: 10.1080/14622200701704905. [DOI] [PubMed] [Google Scholar]
- 17.Parnes B, Main DS, Hocomb S, Pace W. Tobacco cessation counseling among underserved patients: a report from CaReNet. J Fam Pract. 2002;51(1):65–69. [PubMed] [Google Scholar]
- 18.Duquaine D, Farley S, Sacks R, Mandel Ricci J, Silfen S, Shih S. Implementing a quality improvement program with electronic health records: New York City’s Health eQuits. Am J Med Qual. 2014 doi: 10.1177/1062860613520406. Epub ahead of print March 6, 2014. [DOI] [PubMed] [Google Scholar]
- 19.Silfen SL, Farley SM, Shih S et al. Increases in smoking cessation interventions in 19 community health centers following a practice feedback and improvement initiative using electronic health records—New York City, 2010–2012. MMWR Morb Mortal Wkly Rep. 2014;63(41):921–924. [PMC free article] [PubMed] [Google Scholar]
- 20.Amirfar S, Taverna J, Anane S, Singer J. Developing public health clinical decision support systems (CDSS) for the outpatient community in New York City: our experience. BMC Public Health. 2011;11:753. doi: 10.1186/1471-2458-11-753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Eligible professional meaningful use core measures. Measure 9 of 134. Stage 1. May 2014. Available at: http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/downloads/9_Record_Smoking_Status.pdf. Accessed September 24, 2014.
- 22.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980. [Google Scholar]
- 23. Health effects of cigarette smoking. Available at: http://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/#children. Accessed March 13, 2013.
- 24.Parsons A, McCullough C, Wang J, Shih S. Validity of electronic health record-derived quality measurement for performance monitoring. J Am Med Inform Assoc. 2012;19(4):604–609. doi: 10.1136/amiajnl-2011-000557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention. Quitting smoking among adults—United States, 2001–2010. MMWR Morb Mortal Wkly Rep. 2011;60(44):1513–1519. [PubMed] [Google Scholar]
- 26.Volpp KG, Troxel AB, Pauly MV et al. A randomized controlled trial of financial incentives for smoking cessation. N Engl J Med. 2009;360(7):699–709. doi: 10.1056/NEJMsa0806819. [DOI] [PubMed] [Google Scholar]
- 27.Land TG, Rigotti NA, Levy DE, Schilling T, Warner D, Li W. The effect of systematic clinical interventions with cigarette smokers on quit status and the rates of smoking-related primary care office visits. PLoS ONE. 2012;7:e41649. doi: 10.1371/journal.pone.0041649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mathias JS, Didwania AK, Baker DW. Impact of an electronic alert and order set on smoking cessation medication prescription. Nicotine Tob Res. 2012;14(6):674–681. doi: 10.1093/ntr/ntr265. [DOI] [PubMed] [Google Scholar]
- 29.Ferketich AK, Khan Y, Wewers ME. Are physicians asking about tobacco use and assisting with cessation? Results from the 2001–2004 National Ambulatory Medical Care Survey (NAMCS) Prev Med. 2006;43(6):472–476. doi: 10.1016/j.ypmed.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 30.Taggar JS, Coleman T, Lewis S, Szatkowski L. The impact of the Quality and Outcomes Framework (QOF) on the recording of smoking targets in primary care medical records: cross-sectional analyses from The Health Improvement Network (THIN) database. BMC Public Health. 2012;12:329. doi: 10.1186/1471-2458-12-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoel AW, Nolan BW, Goodney PP et al. Variation in smoking cessation after vascular operations. J Vasc Surg. 2013;57(5):1338–1344. doi: 10.1016/j.jvs.2012.10.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Warner DD, Land TG, Rodgers AB, Keithly L. Integrating tobacco cessation quitlines into health care: Massachusetts, 2002–2011. Prev Chronic Dis. 2012;9:E133. doi: 10.5888/pcd9.110343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schroeder SA. How clinicians can help smokers to quit. JAMA. 2012;308(15):1586–1587. doi: 10.1001/jama.2012.13858. [DOI] [PubMed] [Google Scholar]
- 34.Rigotti NA. Strategies to help a smoker who is struggling to quit. JAMA. 2012;308(15):1573–1580. doi: 10.1001/jama.2012.13043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Thorndike AN, Regan S, Rigotti NA. The treatment of smoking by US physicians during ambulatory visits: 1994–2003. Am J Public Health. 2007;97(10):1878–1883. doi: 10.2105/AJPH.2006.092577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bernstein SL, Yu S, Post LA, Dziura J, Rigotti NA. Undertreatment of tobacco use relative to other chronic conditions. Am J Public Health. 2013;103(8):e59–e65. doi: 10.2105/AJPH.2012.301112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jha P, Ramasundarahettige C, Landsman V et al. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368(4):341–350. doi: 10.1056/NEJMsa1211128. [DOI] [PubMed] [Google Scholar]
- 38.Asch DA, Muller RW, Volpp KG. Conflicts and compromises in not hiring smokers. N Engl J Med. 2013;368(15):1371–1373. doi: 10.1056/NEJMp1303632. [DOI] [PubMed] [Google Scholar]
- 39.Savarimuthu SM, Jensen AE, Schoenthaler A et al. Developing a toolkit for panel management: improving hypertension and smoking cessation outcomes in primary care at the VA. BMC Fam Pract. 2013;14:176. doi: 10.1186/1471-2296-14-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Multi-disciplinary approach to increase smoking cessation interventions. Million Hearts Progress Note. Available at: http://millionhearts.hhs.gov/docs/SS_ny.pdf. Accessed April 29, 2014.
- 41.Whittaker R, Maddison R, McRobbie H et al. A multimedia mobile phone–based youth smoking cessation intervention: findings from content development and piloting studies. J Med Internet Res. 2008;10(5):e49. doi: 10.2196/jmir.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]