Abstract
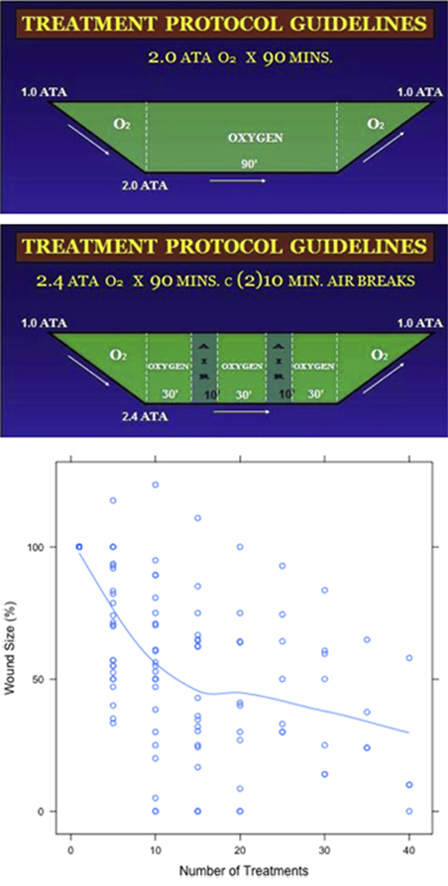
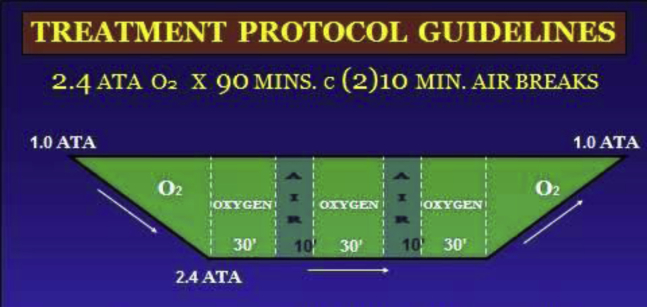
Hyperbaric Oxygen (HBO, HBO2) Therapy is a non-invasive therapy. It has been applied as adjuvant treatment in many medical conditions over the past 50 years. Different treatment protocols have been proven effective for specifically indicated conditions. To evaluate the clinical effectiveness of Hyperbaric Oxygen (HBO) Therapy as an adjunctive treatment for patients with complex wounds. In this prospective cohort study, 40 patients with complex wounds were included. All patients received HBO. HBO was delivered with 100% oxygen for 90 min at 2.0–2.4 ATA. Wound sizes were assessed by one wound surgeon before, during, and every 2 weeks for a total of 12 months after HBO. An analysis of demographic data, wound size and wound photography was performed. Over the 22-month period ending October 31, 2013, 40 patients (21 men and 19 women) with a mean age of 59.73 (range, 29–88) with complex wounds were included. All complex wounds studied were at least 6 months old. The mean wound size was 16.72 cm2 in diameter. Thirty-one patients with complex wounds healed after the completion of a series of HBO treatments (77.5%). Two orocutaneous fistulas were completely closed without further surgery. After 5 HBO treatments, the wound size reduced by 29.7% on average (p = 1.24 × 10−6). After 10 HBO treatments, the wound size statistically significantly reduced by an additional 16.9% (p = 0.0002). There were no complications in this study. Wound healing process was accelerated by HBO. Significant wound size reduction was noted after 5 HBO treatments. Because the biggest reduction in wound size occurred within the first 10 HBO treatments, it is important to conduct these first treatments without interruption. HBO is an effective and safe treatment modality for complex wounds.
Keywords: Hyperbaric oxygen therapy, Complex wound, Wound healing, Effectiveness
Graphical Abstract
Hyperbaric Oxygen (HBO) Therapy was delivered with 100% oxygen for 90 min at 2.0 to 2.4 ATA.
Wound Size by day-of-treatment: The relationship between initial wound size (%) and the wound size by days of treatment. Wound healing process was accelerated by HBO. HBO can be an effective and safe treatment modality for complex wounds.
Introduction
Hyperbaric Oxygen (HBO, HBO2) Therapy is a clinical treatment where patients breathe 100% oxygen in an enclosed hyperbaric oxygen chamber at a pressure greater than one atmosphere. Current information indicates that pressurization should be to 1.4 ATA or higher.1 HBO has been proven effective for many medical conditions. The Undersea and Hyperbaric Medicine Society (UHMS) has approved 14 medical indications.1 In addition, there are other conditions that may benefit from HBO. The therapeutic efficacy of HBO can be mainly explained by the simple physical relationships determining gas concentration, volume, and pressure. Breathing 100% oxygen at atmospheric pressures of up to 3 atm raises the arterial partial pressure of oxygen in the blood (PaO2) to more than 2000 mm Hg. This elevation leads to increased oxygen levels in the blood and tissue, control of infection, stimulated angiogenesis, increased collagen deposition, and reduced edema and inflammation.2–7 HBO has been promoted as an adjunctive treatment for complex wounds. Siriraj Hospital, Thailand currently uses HBO treatment for many indications, including complex wounds.8,9 Treatment of complex wounds represents a significant financial burden on the health care system. The purpose of this study is to evaluate the clinical effectiveness of the Hyperbaric Oxygen Therapy conducted at Siriraj HBO/wound care center as an adjunctive treatment for the patients with complex wounds. In practice the term of complex wounds tend to refer wounds with one or more complicating factors. The type of wounds considered complex are diabetic foot ulcers, leg ulcers, irradiated wounds, wound fistulas, ischemic wounds, refractory chronic wounds and wounds that have failed to heal within six months.
Research Design and Methods
Patient Population
Forty patients with complex wounds who were treated at Siriraj HBO/wound care center were eligible for enrollment between January 2012 and October 2013. Staff at Siriraj HBO/wound care center did the medical and nursing follow-up. Definition of complex wound is the term used more recently to group those well-known difficult wounds, either chronic or acute, that challenge medical and nursing teams. These complex wounds were defined as non-healing wounds in patients with either vascular problem, diabetes, irradiated wounds, osteoradionecrosis (ORN) and orocutaneous fistula. All complex wounds had not healed more than 6 months. All patients received standard wound care. The patients were collected prospectively to determine the effectiveness of HBO treatment. Exclusion criteria included patients who did not consent to HBO treatment, or patients with incomplete study data.
The study was approved by the Ethic Committee of Faculty of Medicine Siriraj Hospital, Mahidol University, Thailand.
Wound Diagnosis and Evaluation
To prevent treatment complications, an evaluation of patient health history and physical examination including a chest x-ray was performed before beginning hyperbaric treatments. Wound assessment using the ruler technique10 was taken and photographic records were created before the first session started and done after every 5 sessions of HBO treatments. In addition to the type of complex wound, information recorded included demographic data, wound size and days to heal. Each clinical assessment was evaluated by an experienced wound surgeon on each patient visit to the Siriraj HBO/wound care center. Protocol of HBO for each patient was recorded. Healing progression was assessed in term of time to healing. The percentage reduction in wound surface area after 5 sessions of HBO was used as an indicator of how the wound is responding to the treatment. The patients were seen every 2 weeks after the last HBO treatment for a total of 2 months, then every 2 months for 1 year.
HBO Treatment Protocols1
In the treatment of patients with diabetic wounds and peripheral arterial disease (PAD) received 90 min of 100% oxygen at a pressure equal to being beneath 33 feet of seawater (2.0 ATA) (Fig. 1). In the treatment of patients with irradiated wound, ORN and orocutaneous fistula, patients received 90 min of oxygen at a pressure of 2.4 ATA (45 feet of seawater). The oxygen was given in intervals of 30 min, with 10 min air breaks in between (Fig. 2). All patients were treated from Monday through Friday in the Sechrist Monoplace Hyperbaric Chambers model 2800.
Figure 1.
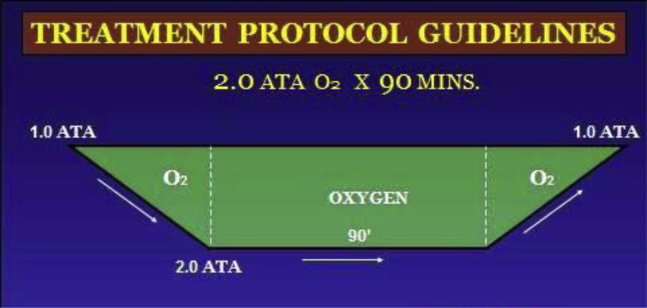
Treatment protocol for diabetic wound case.
Figure 2.
Treatment protocol for the patients with (1) irradiated wound, (2) ORN and (3) orocutaneous fistula.
Statistical Analysis
Wound size data was measured every 5 days. To compare the difference in wound size changes, the wound size in each patient was normalized to 100 percent using the wound size on day 1 (D1). Wound healing in 40 patients was recorded for at least 8 weeks after treatments or until the wound healed completely. Simple logistic regression was used to test for association of healing and covariates including age, sex, diabetes mellitus (DM), history of radiation therapy (RT), peripheral arterial disease (PAD). Statistically significant associations were considered for p-values <0.05.
To compare the effects of HBO treatment, the percent reduction in wound size measured every 5 days were compared with the previous measurement using paired T-test. Statistically significant reduction in wound size was considered for p-value <0.05. Statistical analyses were done in R version 3.0.211 and SPSS version 22.0.
Results
Forty patients, 21 male and 19 female, with complex wounds were included after informed consent and institutional ethics approval. They all received HBO treatment. Total treatments were 1087 sessions. The mean wound size was 16.72 cm2. Demographic data of the patients were illustrated in Table 1.
Table 1.
Demographic Data of the Patients.
| Characteristic | Patients (%) |
|---|---|
| Patient characteristic | |
|
40 |
|
21 (52.5) |
|
59.73 (29–88) |
| Treatment information | |
|
20 (50) |
|
20 (50) |
ATA, Atmosphere absolute pressure; fsw, feet of seawater.
HBO enhanced the wound healing process. All patients showed clinical continuous improvement under HBO. Thirty-one patients (77.5%) healed completely after HBO treatment. Two patients who were suffering from orocutaneous fistulas in the irradiated mandible were cured without further surgery. Nine complex wounds healed completely after staged surgery. Two cases of these were peripheral vascular disease (PAD) with diabetes mellitus (DM), seven cases were head and neck cancer with history of radiation therapy (RT).
We evaluated the factors that could affect wound healing – age, sex, diabetes mellitus, radiation therapy, peripheral arterial disease. Patients with history of radiation therapy were associated with 5 folds higher risk of having delayed wound healing (95% CI from 1.16 to 28.55, p = 0.032). Other covariates were not statistically significantly associated with complete wound healing.
After 5 HBO treatments, the wound size reduced by 29.7% on average (p = 1.24 × 10−6) from the initial wound size. After 10 HBO treatments, the wound size continued to statistically significantly reduce by an additional 16.9% (p = 0.0002) (Table 2). The reduction in wound size slowed down after 10 treatments to an additional 8.6% (p = 0.141). However, statistically significant wound size reduction effects could still be seen up to 20 treatments, which showed a wound size reduction by an additional 12.3% (p = 0.022). Treatment outcomes are shown in Fig. 3. All patients were followed up in the Siriraj HBO/wound care center at two weeks following the last HBO session until 2 months, then every 2 months for 1 year. There were no life-threatening complications.
Table 2.
Wound Size Reduction: Comparison of the Wound Size Between Each 5 Visits. The Wound Size Reduction was Calculated as a Proportion of Wound Size Reduced From the Previous Visit.
| HBO (sessions) | Difference | p-Value |
|---|---|---|
| 1–5 | −29.659 | <0.001 |
| 5–10 | −16.907 | <0.001 |
| 10–15 | −8.565 | 0.141 |
| 15–20 | −12.304 | 0.022 |
| 20–25 | −5.647 | 0.224 |
| 25–30 | −9.669 | 0.012 |
| 30–35 | 3.205 | 0.591 |
| 35–40 | −18.104 | 0.073 |
Figure 3.
Wound size by day-of-treatment: The relationship between initial wound size (%) and the wound size by days of treatment.
Discussion
Hyperbaric oxygen (HBO, HBO2) is a primary and adjunctive therapy for medical conditions. In the early 1960s, HBO was widely used in a variety of medical indications.1 Numerous studies have revealed the efficacy of HBO. It also has been shown to be an effective method for treating complex wounds. Complex wounds are challenging to manage, with many associated problems. The main problems include having to deal with underlying diseases such as diabetes, vascular problems, history of radiation therapy, low oxygen and wound infection. In a previous study, Pecoraro et al12 discovered that periwound measurement of transcutaneous oxygen tension (TcPO2) was significantly associated with the initial rate of tissue repair. They found that patients with low periwound TcPO2 (<20 mm Hg) was associated with a 39 folds increased risk of early healing failure. The study by Fife et al13 concluded that baseline air TcPO2 identified degree of tissue hypoxia and related to wound failure rate. Lack of oxygen can lead to chronic wounds. HBO increases oxygenation of tissues and supports wound healing. Clinical outcome seems to improve after HBO treatments, even though traditional wound treatments had been unsuccessful.
Osteoradionecrosis (ORN) is one type of complex wound. It is a complication of the use of radiation therapy. Clinical manifestations of ORN may include orocutaneous fistula, which is difficult to treat and requires staged surgery. David et al14 concluded that using HBO as an adjunctive treatment of ORN was beneficial. The study also showed that HBO was an effective adjunctive method for treating this problem. Two patients with orocutaneous fistula closed completely under HBO. Our patients benefited from this treatment because no further surgery was needed.
Specific HBO treatment protocols depend on the patient's specific medical condition. In this study, the authors came to two important conclusions. First, significant wound size reduction was noted after 5 HBO treatments. Secondly, in addition to finishing the prescribed number of sessions, uninterrupted completion of the first 10 HBO treatments is very important.
Unfortunately, this study lacks a control group for comparison with patients with complex wounds that did not receive HBO treatments. Wound measurements can monitor changes in wound size, help predict wound healing and evaluate the effectiveness of the treatment. However, the literature states that ruler-based methods provide a crude wound measurement that potentially overestimates wound area by twenty five percent.10 HBO has been promoted as an adjunctive treatment for complex wounds. Data is used to indicate the effectiveness of hyperbaric oxygen to reduce amputation rate and promote wound healing.15–22 In addition to HBO, proper wound care is essential.23 HBO is safe and well tolerated. There are few side effects, and most are mild and reversible. Severe consequences can occur in rare cases.24–29
Conclusion
Hyperbaric oxygen therapy has a role in modern medical practice. In most cases, it is safe and severe side effects are rare. There are many indications for HBO treatment. The results suggest that HBO has been shown to be an effective method for treating complex wounds. It significantly improved wound healing. However, HBO does not replace quality wound care. HBO should be used in addition to, but not as a replacement of aggressive wound treatment.
Acknowledgments
The authors thank Jim Sheffield of International ATMO, Nix Wound Care & Hyperbaric Medical Center, San Antonio, Texas for his input and the Hyperbaric staffs of the Siriraj Hyperbaric Medical Center/Wound Care Center for helping to conduct the study.
Footnotes
Disclosure: None of the authors have any disclosures to make.
The authors have no financial conflict of interest to declare in this study.
References
- 1.Gesell L.B., editor. Hyperbaric Oxygen Therapy Indications. The Hyperbaric Oxygen Therapy Committee Report. 12th ed. Undersea and Hyperbaric Medical Society; Durham: 2008. [Google Scholar]
- 2.Faglia E., Favales F., Aldeghi A. Adjunctive systemic hyperbaric oxygen therapy in treatment of severe prevalently ischemic diabetic foot ulcer: a randomized study. Diabetes Care. 1996 Dec;19(12):1338–1343. doi: 10.2337/diacare.19.12.1338. [DOI] [PubMed] [Google Scholar]
- 3.Brown G.L., Thomson P.D., Mader J.T., Hilton J.G., Browne M.E., Wells C.H. Effects of hyperbaric oxygen upon S. aureus, Ps. aeruginosa and C. albicans. Aviat Space Environ Med. 1979;50:717–720. [PubMed] [Google Scholar]
- 4.Marx R.E., Ehler W.J., Tayapongsak P., Pierce L.W. Relationship of oxygen dose to angiogenesis induction in irradiated tissue. Am J Surg. 1990;160:519–524. doi: 10.1016/s0002-9610(05)81019-0. [DOI] [PubMed] [Google Scholar]
- 5.Brismar K., Lind F., Kratz G. Dose-dependent hyperbaric oxygen stimulation of human fibroblast proliferation. Wound Repair Regen. 1997;5:147–150. doi: 10.1046/j.1524-475X.1997.50206.x. [DOI] [PubMed] [Google Scholar]
- 6.Mandell G.L. Bacteriacidal activity of aerobic and anaerobic polymorphonuclear leukocytes. Infect Immun. 1974;9(2):337–341. doi: 10.1128/iai.9.2.337-341.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reng J.J., Hussan M.Z., Constant J., Hunt T.K. Angiogenesis in wound healing. J Surg Pathol. 1998;3:1–7. [Google Scholar]
- 8.Despatis M., Shapera L., Parslow N., Woo K. Complex wounds. WCC. 2008;6(2):24–25. [Google Scholar]
- 9.Ferreira M.C., Tuma P., Jr., Carvalho V.F., Kamamoto F. Complex wounds. Clinics. 2006;61(6):571–578. doi: 10.1590/s1807-59322006000600014. [DOI] [PubMed] [Google Scholar]
- 10.Gethin G. The importance of continuous wound measuring. Wounds UK. 2006;2(2):60–68. [Google Scholar]
- 11.R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2013. R: A Language and Environment for Statistical Computing.http://www.R-project.org/ [Google Scholar]
- 12.Pecoraro R.E., Ahroni J.H., Boyko E.J., Stensel V.L. Chronology and determinants of tissue repair in diabetic lower-extremity ulcers. Diabetes. 1991;40:1305–1313. doi: 10.2337/diab.40.10.1305. [DOI] [PubMed] [Google Scholar]
- 13.Fife C.F., Buyukcakir C., Otto G.H. The predictive value of transcutaneous oxygen tension measurement in diabetic lower extremity ulcers treated with hyperbaric oxygen therapy: a retrospective analysis of 1144 patients. Wound Repair Regen. 2002;10:198–207. doi: 10.1046/j.1524-475x.2002.10402.x. [DOI] [PubMed] [Google Scholar]
- 14.David L.A., Sandor G.K., Evans A.W., Brown D.H. Hyperbaric oxygen therapy and mandibular osteoradionecrosis: a retrospective study and analysis of treatment outcomes. J Can Dent Assoc. 2001;67:384. [PubMed] [Google Scholar]
- 15.Barnes R.C. Point: hyperbaric oxygen is beneficial for diabetic foot wounds. Clin Infect Dis. 2006;43(2):188–192. doi: 10.1086/505207. [DOI] [PubMed] [Google Scholar]
- 16.Faglia E., Favales F., Aldeghi A. Change in major amputation rate in a center dedicated to diabetic foot care during the 1980s: prognostic determinants for major amputation. J Diabetes Complications. 1998;12(2):96–102. doi: 10.1016/s1056-8727(97)98004-1. [DOI] [PubMed] [Google Scholar]
- 17.Escobar S.J., Slade J.B., Jr., Hunt T.K., Cianci P. Adjuvant hyperbaric oxygen therapy (HBO2) for treatment of necrotizing fasciitis reduces mortality and amputation rate. Undersea Hyperb Med. 2005;32(6):437–443. [PubMed] [Google Scholar]
- 18.Ong M. Hyperbaric oxygen therapy in the management of diabetic lower limb wounds. Singapore Med J. 2008;49(2):105–109. [PubMed] [Google Scholar]
- 19.Kaya A., Aydin F., Altay T., Karapinar L., Ozturk H., Karakuzu C. Can major amputation rates be decreased in diabetic foot ulcers with hyperbaric oxygen therapy? Int Orthop. 2009;33(2):441–446. doi: 10.1007/s00264-008-0623-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Angelucci D.D. ModernMedicine Network. Dermatology Times; 2010. Hyperbaric Oxygen Therapy Reduces Amputation Risk in Chronic Wounds.http://dermatologytimes.modernmedicine.com/dermatology-times/news/modernmedicine/modern-medicine-feature-articles/hyperbaric-oxygen-therapy-red [cited 2013 Nov 16]. Available from: [Google Scholar]
- 21.Marx R.E. A new concept in the treatment of osteoradionecrosis. J Oral Maxillofac Surg. 1983;41(6):351–357. doi: 10.1016/s0278-2391(83)80005-6. [DOI] [PubMed] [Google Scholar]
- 22.Hart G.B., Mainous E.G. The treatment of radiation necrosis with hyperbaric oxygen (OHP) Cancer. 1976;37(6):2580–2585. doi: 10.1002/1097-0142(197606)37:6<2580::aid-cncr2820370603>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 23.Opasanon S., Muangman P., Namviriyachote N. Clinical effectiveness of alginate silver dressing in outpatient management of partial-thickness burns. Int Wound J. 2010;7(6):467–471. doi: 10.1111/j.1742-481X.2010.00718.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kindall E.P. Contraindications and side effects to hyperbaric oxygen treatment. In: Kindall E.P., Whelan H.T., editors. Hyperbaric Medicine Practice. 3rd ed. Best Publishing; Flagstaff, AZ: 2008. pp. 273–288. [Google Scholar]
- 25.Plafki C., Peters P., Almeling M. Complications and side effects of hyperbaric oxygen therapy. Aviat Space Environ Med. 2000;71:119–124. [PubMed] [Google Scholar]
- 26.Clements K.S., Vrabec J.T., Mader J.T. Complications of tympanostomy tubes inserted for facilitation of hyperbaric oxygen therapy. Arch Otolaryngol Head Neck Surg. 1998;124:278. doi: 10.1001/archotol.124.3.278. [DOI] [PubMed] [Google Scholar]
- 27.Tibbles P.M., Edelsberg J.S. Hyperbaric-oxygen therapy. N Engl J Med. 1996;334(25):1642. doi: 10.1056/NEJM199606203342506. [DOI] [PubMed] [Google Scholar]
- 28.Leach R.M., Rees P.J., Wilmshurst P. Hyperbaric oxygen therapy. BMJ. 1998;317(7166):1140–1143. doi: 10.1136/bmj.317.7166.1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Davis J.C., Dunn J.M., Heimbach R.D. Hyperbaric medicine: patient selection, treatment procedures, and side effects. In: Davis J.C., Hunt T.K., editors. Problem Wounds: The Role of Oxygen. Elsevier Science; New York: 1988. pp. 233–235. [Google Scholar]



