Abstract
The term ‘habit’ is widely used to predict and explain behaviour. This paper examines use of the term in the context of health-related behaviour, and explores how the concept might be made more useful. A narrative review is presented, drawing on a scoping review of 136 empirical studies and 8 literature reviews undertaken to document usage of the term ‘habit’, and methods to measure it. A coherent definition of ‘habit’, and proposals for improved methods for studying it, were derived from findings. Definitions of ‘habit’ have varied in ways that are often implicit and not coherently linked with an underlying theory. A definition is proposed whereby habit is a process by which a stimulus generates an impulse to act as a result of a learned stimulus-response association. Habit-generated impulses may compete or combine with impulses and inhibitions arising from other sources, including conscious decision-making, to influence responses, and need not generate behaviour. Most research on habit is based on correlational studies using self-report measures. Adopting a coherent definition of ‘habit’, and a wider range of paradigms, designs and measures to study it, may accelerate progress in habit theory and application.
Keywords: habit, review, automaticity, behaviour change, study design
Habits are considered to play a fundamental role in generating behaviour (e.g., James, 1891; Triandis, 1977; Watson, 1913). Although used in everyday parlance to refer to frequent, persistent or customary behaviour, within health psychology ‘habit’ is defined as a phenomenon whereby behaviour is prompted automatically by situational cues, as a result of learned cue-behaviour associations (Wood & Neal, 2009). Habits form through repetition of behaviour in a specific context (Lally, van Jaarsveld, Potts, & Wardle, 2010). This reinforces a mental context-behaviour association, such that alternative options become less accessible in memory (Danner, Aarts, & de Vries, 2007, 2008), and the context acquires the potential to activate behaviour in the absence of awareness, conscious control, cognitive effort or deliberation (Bargh, 1994). Although habit has long been known to underpin behaviour (e.g., James, 1891; Watson, 1913), there has been a recent resurgence of interest in habit within health psychology (e.g., Gardner, de Bruijn, & Lally, 2011; Lally & Gardner, 2013; van t'Riet, Sijtsema, Dagevos, & de Bruijn, 2011).
Habit is hypothesised to have several characteristics that make it pertinent to understanding and changing health behaviour. Dual process models propose two parallel processing systems, analogous to two pathways to behaviour (Hofmann, Friese, & Wiers, 2008; Strack & Deutsch, 2004). Habit is depicted on an impulsive pathway, such that perception of cues activates low-level context-behaviour associations, which prompt behaviour rapidly and efficiently, with minimal forethought. Reasoned cognitions (e.g., intentions) are portrayed on a reflective pathway, whereby a cue initiates rule-based deliberation, which directs behaviour slowly and effortfully. Theory predicts that, in associated contexts, habit will consistently elicit behaviour and override counter-habitual intentions (Hall & Fong, 2007; Triandis, 1977). As habits form, action control is transferred to environmental stimuli, and reliance on attentional or motivational processes decreases (Lally, Wardle, & Gardner, 2011). Habits should thus persist even where conscious motivation wanes. This has led to calls for habit formation to be encouraged in interventions, to promote long-term maintenance (Rothman, Sheeran, & Wood, 2009).
The application of habit to the health domain has, however, proven controversial. Commentators have questioned whether health behaviours can be undertaken without conscious mediation (Ajzen, 2002; Maddux, 1997). Concerns have been raised around the coherence of the habit concept and popular measures of it (Gardner, Abraham, Lally, & de Bruijn, 2012; Sniehotta & Presseau, 2012). It would seem prudent, and timely, to evaluate the persuasiveness of evidence of the applicability of habit to health behaviour.
This paper examines the conceptual and methodological assumptions underpinning applications of habit to health behaviour. It is not a comprehensive literature summary, but is based on a scoping review conducted using systematic search and filter procedures. Evidence was identified via systematic searches of literature covering a 15-year period (1998–2013). Evidence was sorted into two strands: one to identify explicit definitions of habit from literature reviews (8 papers) and one to identify empirical research applying habit to health behaviours (136 studies; Supplemental Table 1). Details of evidence identification procedures are available as Supplemental Data.
The first two sections of this review explore the definitions of ‘habit’ and ‘habitual behaviour’, as extracted from extant evidence reviews. Next, the methods used in empirical applications of habit to health behaviour are assessed, in respective sections on habit measures, and the designs and analyses used to test theoretical predictions around habit and behaviour.
Conceptualising habit and habitual behaviour
What is a ‘habit’?
As an abstract and socially defined concept, there can be no objectively ‘correct’ or ‘incorrect’ definition of habit (West & Brown, 2013). Definitions must be judged according to their usefulness for predicting, explaining and changing behaviour. The lay definition of ‘habit’ as frequent, regular or persistent behaviour is unsatisfactory because it offers no explanatory mechanism for these characteristics, and is not discussed further.
Table 1 presents explicit definitions of habit cited within (eight) literature reviews. These definitions concur in describing elements of a process whereby behaviour is contextually cued, without conscious thought, via activation of a mental context-behaviour association learned through context-consistent performances. They differ in the location of ‘habit’ in this process. Five definitions portray ‘habit’ as behaviour generated by this process (Gardner et al., 2011, 2012; Nilsen, Bourne, & Verplanken, 2008; Nilsen, Roback, Broström, & Ellström, 2012; van t'Riet et al., 2011). One views habit as a tendency to engage in behaviour (Ouellette & Wood, 1998), and two as the automaticity of responses (Verplanken & Wood, 2006; Wood & Neal, 2009).
Table 1. Explicit psychological definitions of habit(s) in published evidence reviews.
| Reference | Definition | Habit is… |
|---|---|---|
| Gardner et al. (2012, p. 1) | ‘behavioural patterns, based on learned context-behaviour associations, that are elicited automatically upon encountering associated contexts … acquired through context-dependent repetition’ | A type of behaviour |
| Gardner et al. (2011, p. 175) | ‘behavioural patterns learned through context-dependent repetition: repeated performance in unvarying settings reinforces context-behaviour associations such that, subsequently, encountering the context is sufficient to automatically cue the habitual response’ | A type of behaviour |
| Nilsen et al. (2008, p. 35) | ‘acquired behaviour patterns regularly followed until they become almost involuntary … Habits are cued relatively directly by the environment, with minimal amount of purposeful thinking and often without any sense of awareness’ | A type of behaviour |
| Nilsen et al. (2012, p. 1) | ‘behaviour that has been repeated until it has become more or less automatic, enacted without purposeful thinking, largely without any sense of awareness’ | A type of behaviour |
| Ouellette and Wood (1998, p. 55) | ‘tendencies to repeat responses given a stable supporting context … the cognitive processing that initiates and controls the response [is] automatic and can be performed quickly in parallel with other activities and with allocation of minimal focal attention’ | A tendency towards behaviour |
| van t'Riet et al (2011, p. 586) | ‘learned sequences of acts that have been reinforced in the past by rewarding experiences and that are triggered by the environment to produce behaviour largely outside of people's conscious awareness’ | A type of behaviour |
| Verplanken and Wood (2006, p. 91) | ‘A type of automaticity in responding that develops as people repeat actions in stable circumstances … habit formation involves the creation of associations in memory between actions and stable features of the circumstances in which they are performed. Recurring aspects of performance circumstances come to trigger habitual responses directly without input from people's intentions or decisions to act’ | A type of automaticity |
| Wood and Neal (2009, p. 580) | ‘A type of automaticity characterized by a rigid contextual cuing of behavior that does not depend on people's goals and intentions. Habits develop as people respond repeatedly in a stable context and thereby form direct associations in memory between that response and cues in the performance context’ | A type of automaticity |
Treating habit as a form of behaviour is incompatible with the portrayal of habit, within health behaviour models, as a determinant of action (e.g., Triandis, 1977). As Maddux (1997) noted, ‘to say that behavior that is an automatic response to situational cues is caused by habit is to say that a habit is caused by a habit … a habit cannot be both the behavior and the cause of the behavior’ (pp. 335–336). Viewing habit as a tendency towards behaviour is similarly problematic. Such a tendency must be inferred from and summarise occurrences of behaviour, so lacks explanatory value; stating that an individual tends to perform behaviour because they have a tendency to perform behaviour is truistic. Portraying habit as a form of automaticity avoids such problems by specifying habit as a cognitive mechanism independent of behaviour.
Six definitions depict habitual behaviour as directly or automatically triggered by associated cues (Gardner et al., 2011, 2012; Nilsen et al., 2008, 2012; Wood & Neal, 2009), so implying that the behavioural response is an inevitable outcome of cue encounters. Yet, empirical evidence suggests that contextually cued automatic behavioural responses can be consciously inhibited. Participants in one observational diary study reported some successes in inhibiting unwanted actions performed in stable contexts, through the spontaneous use of vigilant monitoring of cues and behaviour, or distraction (Quinn, Pascoe, Wood, & Neal, 2010). Planning alternative responses to habit cues has also been found to reduce engagement in self-reported habitual behaviours (Adriaanse et al., 2010). Behaviour may therefore not be a necessary consequence of encountering habit cues. Rather, habits can be inhibited – albeit sometimes with difficulty – given sufficient will-power and self-regulatory resources (Neal, Wood, & Drolet, 2013).
Logical inconsistencies between these definitions and theoretical and empirical evidence may be resolved by viewing habit as a process by which a stimulus automatically generates an impulse towards action, based on learned stimulus-response associations (see also West & Brown, 2013). This conceptualisation offers a coherent- and evidence-based explanatory mechanism for behaviour, and is novel in two respects. First, it represents habit as a process by which action is cued. This minimises conceptual and logical tensions that arise from portraying habit as behaviour, automaticity or any other single element of the wider process. It also incorporates the cue-dependence, automaticity and conditioned stimulus-response associations that characterise and distinguish habitual action from other forms of automatic behaviour (Gardner et al., 2012; Lally et al., 2010; Orbell & Verplanken, 2010; Wood & Neal, 2009). Second, depicting the ‘response’ to habit cues as an impulse allows for the possibility that habitual tendencies may, once activated, be overridden prior to translation into action. Impulses can be defined as high-level schematic representations of action which, if insufficiently opposed, trigger execution of action (e.g., Michie & West, 2013). A habitual impulse may be one of many momentary motivational forces competing to direct behaviour, so vying with various opposing forces favouring alternative actions or inhibition of the habitual response. PRIME Theory proposes that impulse generation is a low-level cognitive process that lies outside of awareness unless the impulse is frustrated, in which case it becomes consciously experienced as an urge to engage in behaviour (West & Brown, 2013). Thus, habitual behaviour may be experienced as directly cued where the impulse is unopposed, but inhibited where opposing forces are stronger.
What is a ‘habitual (health) behaviour’?
Habit has been applied to a variety of health behaviours, including dietary consumption (e.g., Adriaanse et al., 2010), physical activity (Rhodes & de Bruijn, 2010), alcohol consumption (Norman, 2011) and medication adherence (Bolman, Arwert, & Vollink, 2011). There is a disconnect between these relatively complex behaviours and the simple actions that have been the focus of investigation within other sub-disciplines of psychology. Early behaviourist studies of habit centred on behaviours such as pulling strings and lifting latches (Watson, 1913), and neuroscientists, for example, continue to investigate habit through observations of key presses, lever pushes and simple object-selection tasks (e.g., de Wit & Dickinson, 2009). The tacit assumption that the automatisation of simple actions can be transposed to complex health behaviours remains largely unquestioned (but see Maddux, 1997). Behaviourists have traditionally viewed complex habitual actions as concatenated sequences of simpler habitual actions (i.e., ‘composite habits’; Campbell, 1956), such that the cessation of each (habitual) action within a given sequence habitually activates the subsequent action until the sequence is completed. No study identified by the scoping review offers compelling evidence to suggest that the health actions to which habit has been applied are performed in rigid sequential order without conscious input. The notion that everyday health behaviours may be wholly rigidly automated and performed with little control, awareness or intention does not match the subjective experience of most health behaviours (Maddux, 1997).
Maddux (1997) proposed that, for complex health behaviours, habit be seen as a mechanism that cues conscious decision-making that in turn prompts behaviour, rather than regulating the procedural enactment of behaviour. This conceptualisation of ‘habitual behaviour’ as necessarily consciously mediated is incompatible with the definition of habit outlined here (and those in Table 1), and with empirical evidence demonstrating that action can be automatically cued without, or contrary to, conscious motivation (Neal, Wood, Wu, & Kurlander, 2011). A broader distinction between the (automatic) initiation and the (conscious) performance of behaviour, however, is concordant with the present definition. From this perspective, a ‘habitual’ bicycle commuter, for example, may automatically opt to use a bicycle rather than alternative transport (so automatically enacting the first behaviour in a superordinate ‘bicycle commuting’ sequence, such as putting on a cycle helmet), but negotiating the journey may require higher-level cognitive input. Conversely, a ‘habitual’ exerciser may consciously decide to visit the gym, but enact their subsequent pattern of exercises within the gym automatically, with little conscious thought. Indeed, the distinction between initiation and performance of behaviour implies three possible types of ‘habitual behaviour’, that is, those which are habitually initiated but consciously (non-habitually) performed (e.g., bicycle commuting); consciously initiated but habitually performed (e.g., exercising in the gym); or habitually initiated and habitually performed (e.g., eating unhealthy snacks).
The distinction between behavioural initiation and performance is crude; after a complex behaviour sequence is initiated, performance to completion will require initiation of further lower-level actions, each of which may potentially be governed by independent habit processes. For bicycle commuters, for example, the movements required to ‘remove the bicycle from the shed’ may be activated by a ‘removing the bicycle from the shed’ habit, whereas ‘walking the bicycle to the road’ may be governed by a separate habit. The distinction is, however, useful from a practical perspective. It demands, for example, that habit formation intervention developers determine whether to target the automatic selection of a behavioural option (e.g., automatically opting to eat from a small plate so as to reduce portion size; Lally, Chipperfield, & Wardle, 2008) – possibly with the aim that, once initiated, disengagement from the behaviour (replacing it with a larger plate) will be unlikely – or to automate sequential activation of multiple behaviours within a higher-order sequence (e.g., performing rehabilitation exercises in a given order; Fleig et al., 2013). The latter may not be feasible for all behaviours; tentative evidence suggests complex sequences of actions may take longer to become habitual, and participants better adhere to habit formation attempts for simpler actions (Lally et al., 2010).
Habitual behaviour may be defined, broadly, as any action, or sequence of actions, that is controlled by habit. This allows for habit to be involved in initiation or performance of action, the former resonating more strongly with everyday experiences of complex behaviours (Maddux, 1997), and the latter reconnecting with historical treatments of ‘habitual behaviour’ as chunked automated sequences of lower-level actions (e.g., Graybiel, 2008; Watson, 1913). However, greater precision may be achieved by distinguishing between habitually initiated behaviour, which is instigated by a habitual impulse but may require cognitive input to be performed, and habitually performed behaviour, the execution of which is facilitated by the activation of one or more habits, regardless of whether consciously or non-consciously instigated. This distinction may be less important for simple behaviours for which initiation and performance cannot easily be separated, such as drinking water (e.g., Lally et al., 2010), but is pertinent to behaviours composed of multiple sub-actions, such as physical activity. Future work might use this distinction to specify more precisely the role(s) of habit in action.
Are existing methods for capturing ‘habit’ adequate?
Measuring habit
Progress in habit theory and application depends on reliable measures of the characteristics of habit: automatic impulse generation, impulses (or urges) to perform behaviour, cue-dependency, and an underlying stimulus-response association. Past behaviour has been used as a proxy for the potential for habit to regulate action (i.e., ‘habit strength’; Hull, 1943), but fails to distinguish between habit and non-habit processes (Ajzen, 2002). The scoping review identified four discrete habit measures.
Ouellette and Wood's (1998) ‘Behaviour Frequency × Context Stability’ (BFCS) measures, used in 16 studies (12% of all quantitative studies identified), assume that past behaviour reliably reflects habit in unvarying settings. Scores represent the multiplicative product of self-reported (past or typical) behaviour frequency (‘how often do you do X?’) and contextual covariation (‘when you do X, how often is cue Y present?’, with ‘cue Y’ typically specified as location, time, presence of others or mood; e.g., Ji & Wood, 2007). The Exercise Habit Survey (EHS), used in one study (1%; Tappe & Glanz, 2013), consists of 10 items addressing 4 factors: three contextual covariates of exercise behaviour (location, presence of others and time of day), and the rigidity of exercise sequences (e.g., ‘Every day that I exercised, I performed the same exercise(s)’). Both BFCS and EHS tap cue-dependency, but applications have been limited by a reliance on researcher-generated cues. It has been suggested that any environmental feature can cue habit given sufficient cue-behaviour pairings (Verplanken, 2005), and so BFCS measures may perhaps be enhanced by focusing on cues preliminarily elicited from participants (e.g., Judah, Gardner, & Aunger, 2013). Moreover, by focusing on cue stability, both BFCS and EHS assess the likelihood that habit has formed, not the automaticity with which habitual impulses are generated. Additionally, the BFCS implies a compensatory relationship between behaviour frequency and context stability, such that frequent enactment in varying settings is expected to have equivalent influence on habit strength as infrequent enactment in unvarying settings (B. Verplanken, personal communication, November 26, 2013). Empirical data are needed to explore the impact of variation in frequency and stability on the automaticity with which habitual behaviour proceeds.
One hundred and nineteen studies (88%) have used the Self-Report Habit Index (SRHI) (or abbreviations thereof), which is designed to capture automaticity (Verplanken & Orbell, 2003). Twelve items follow a stem (‘Behaviour X is something…’) and focus on three facets of automaticity – lack of awareness (‘…I do without thinking’), lack of control (‘…that would require effort not to do’) and mental efficiency (‘…I have no need to think about doing’) – behavioural frequency (‘…I do frequently’) and self-identity (‘…that's typically “me”’). The SRHI assumes that people can be aware, through reflection on the consequences of action, that they were unaware of initiating action at the time of performance (e.g., ‘I cannot recall lighting my cigarette, yet it is lit, so I must have lit it automatically’; Gardner et al., 2012; Sniehotta & Presseau, 2012).
SRHI applications have been criticised for neglecting cues (Sniehotta & Presseau, 2012). Any behaviour may be regulated by habit in one setting and deliberation in another, and so context-free estimates of the habitual nature of ‘behaviour X’ may conflate habitual and non-habitual performances. The SRHI can be adapted to incorporate contextual cues (e.g., ‘Behaviour X in Context Y is something I do automatically’; Sniehotta & Presseau, 2012). It is also unclear whether the SRHI captures habitual initiation or performance of action, though it may be easily modified to specify initiation rather than execution (e.g., ‘choosing to eat unhealthy snacks is something I do automatically’).
The SRHI also contains potentially conceptually redundant items. Identity is not a defining characteristic of habit (see e.g., Table 1). Although intended to capture the experience of repetitive action rather than to estimate frequency (Verplanken & Orbell, 2003), behavioural frequency SRHI items are likely to invite responses that covary closely with enactment frequency (e.g., Gardner et al., 2011). This is logically problematic: if habits are responses to cues, performance frequency will vary with the frequency with which cues are encountered. For example, for weekly cinema-goers with habits for eating popcorn in the cinema, the habitual popcorn impulse will be activated weekly, but monthly for monthly cinema-goers (Neal et al., 2011). The mechanism that underpins habitual action is automaticity; behaviour frequency is an antecedent, and consequence, of automaticity (Sniehotta & Presseau, 2012). The contribution of past performance to habit should be reflected in the automaticity with which the habitual impulse is activated.
Automaticity scales have been proposed. One measure, used in two studies (1%), is a six-item subscale of the Smoking Motivation Questionnaire (SMQ; Spielberger, 1986), and requires reflection on smoking automatically, without remembering lighting up, or when preoccupied with other tasks relate to lighting cigarettes. The domain specificity of the SMQ precludes its application to other behaviours. Automaticity-specific SRHI subscales have been more commonly employed. The most systematically developed is the ‘Self-Report Behavioural Automaticity Index’ [SRBAI, used in nine studies (7%)], which comprises four items shown to have content validity as automaticity indicators (Gardner et al., 2012). It is unclear whether the SRBAI remains sensitive to discrete facets of automaticity (mental efficiency, lack of awareness and control), but close observed SRHI–SRBAI convergence suggests participants do not distinguish between these. By not accounting for repetition history, the SRBAI may fail to discern habit from non-learned forms of automaticity. For behaviour prediction or habit tracking studies however, the SRBAI offers a more parsimonious and potentially conceptually clear alternative to the SRHI (Gardner et al., 2012).
Association tests, used in one study (1%; Danner, Aarts, Papies, & de Vries, 2011), are designed to assess the cue-behaviour associations that underpin behavioural habits. These operate on the basis that habitual responses are more mentally accessible than non-habit responses, so will be recognised more quickly and frequently in the presence of cues (e.g., Danner et al., 2008; Neal, Wood, Labrecque, & Lally, 2012). Repeated cue-dependent performance quickens responses to these tasks (Webb, Sheeran, & Luszczynska, 2009). Associative measures may be seen as a ‘gold standard’, in that they assess cue-response associations directly, bypassing the subjectivity of participant self-report. However, they require administration in controlled conditions, and prior knowledge of likely cues to habitual behaviour, making them unsuitable for the self-administered survey study designs that dominate the habit literature.
The habit process cannot be directly observed. Existing measures are necessarily imperfect, relying on inference from the conduciveness of conditions to habit formation and maintenance (Ouellette & Wood, 1998; Triandis, 1977) or observation of the characteristics and consequences of habitual responding (Danner et al., 2008; Spielberger, 1986; Tappe & Glanz, 2013; Verplanken & Orbell, 2003). The most theoretically valid measures use implicit association or response time tasks to directly assess cue-behaviour associations, but these are impractical in uncontrolled research settings. Consequently, self-report measures dominate. The accuracy of self-reports of behaviour, automaticity and cues is however questionable (Gardner & Tang, in press). This is problematic, given that predictive validity is used as a criterion for measurement accuracy (Gardner et al., 2012; Tappe & Glanz, 2013); a failure to detect habitual behaviour may indicate that behaviour is not habitual, or that the measure is insensitive to true habit. Similarly, temporal variations in habit scores could reflect habit strength fluctuations or an unstable and unreliable measure. Available self-report measures also fail to comprehensively capture habit: the BFCS and EHS measure cue-dependency but not automaticity, and the SRHI addresses automaticity but is rarely used to assess cue-dependency. Measures must tap the cue-dependency of the habit process (Orbell & Verplanken, 2010), and their sensitivity to automaticity might be assessed against associative tests. Self-report measures infer habit from reflections on behavioural performance (e.g., ‘behaviour X is something I do automatically’), but as argued above, habit need not prompt behaviour. Where habitual impulses are blocked, they can be consciously experienced as urges to enact the habitual response. Simple self-report measures of urges are available (Fidler, Shahab, & West, 2011) and might complement measures of automaticity and cue-dependence, as a proxy for the strength of the cue-response association that underpins habit.
Predicting habitual behaviour and behavioural habit
The majority of studies have investigated effects of habit on health behaviour (82 studies; 60% of all studies). These have tended to focus on ongoing habits and behaviour, testing two hypotheses (Triandis, 1977). First, habit strength will correlate positively with the likelihood of behavioural enactment. Second, habit will moderate the influence of conscious intentions on action, such that, as habit strength increases, the intention–behaviour relationship will diminish. Although derived from the Theory of Interpersonal Behaviour (TIB; Triandis, 1977), these hypotheses have mostly been tested within the framework of the Theory of Planned Behaviour (Ajzen, 1991). Figure 1 portrays these two effects (Paths A and B) within a generic social cognitive framework.
Figure 1. Hypothesised habit–behaviour relationships and the habit formation process.
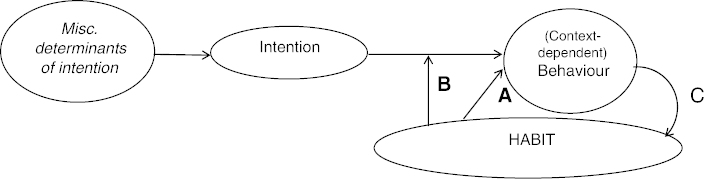
Note: Path A: Direct effect of habit strength on behaviour frequency (Triandis, 1977); Path B: Moderating impact of habit on the intention–behaviour relationship (Triandis, 1977); Path C: Effect of behavioural repetition on habit formation (Lally et al., 2010).
Twelve studies (9%) have sought to predict habit strength. Habit is defined by its acquisition through (context-dependent) repeated performance (Path C in Figure 1). A study of the formation of dietary and physical activity habits found variation in the speed with which habit strengthened, and the level at which it peaked, despite identical repetitions (Lally et al., 2010). Additional variables may strengthen habit by moderating the reinforcement value of each performance on the cue-response association. For example, the Associative Cybernetic Model proposes that rewarding outcomes of behaviour can hasten learning of cue-response relationships (de Wit & Dickinson, 2009). Repeated sequential presentation of context, behaviour and rewarding outcomes can imbue the context with the motivational properties of the reward, so that the context comes to signal both an opportunity and incentive to act. This should be expressed via an interaction between reward and repetition, such that repetition has a stronger impact on habit strength where behaviour is rewarded. Determinants of habit strength may thus be logically organised into four stages: those that aid intention formation; those that facilitate the translation of intention into action; those that aid continuation of a new behaviour and those that moderate the relationship between context-dependent repetition (CDR) and habit development (Lally & Gardner, 2013).
Predicting behaviour
Empirical tests have tended to support the two predicted effects of habit on action, but some results have been unexpected. Meta-analyses of SRHI applications have shown moderate-to-strong habit–behaviour correlations (Gardner et al., 2011), though coefficients are smaller when estimated using automaticity-specific SRHI measures (Gardner et al., 2012). Such modest effects concur with the proposition that, because impulses may be inhibited, habit need not prompt action. Moderation tests (conducted in 24 studies; see Supplemental Table 2) have tended to show intention to become less predictive of behaviour as habit strength increases, so that, where intention is weak and habit strong, behaviour corresponds with habit and not intention (18 studies, 75% of moderation tests; Gardner et al., 2011). Yet, four tests (17%) found no habit–intention interaction (e.g., Gardner et al., 2012), and three (13%) showed intention to be more predictive of behaviour at stronger levels of habit (de Bruijn, Rhodes, & van Osch, 2012; Gardner, de Bruijn, & Lally, 2012; Rhodes & de Bruijn, 2010). 1 It is unlikely that the direction of habit–intention interactions is behaviour-specific. Physical activity studies, for example, have produced mixed findings, with habits variously shown to weaken (seven studies), strengthen (two studies), or have no impact on intention–behaviour relations (two studies).
Inconsistent study findings may arise from limitations inherent to the designs and analyses used to predict habitual action. Interaction tests have mostly been based on measures of congruent intentions, habits and behaviour (e.g., intentions to snack, snacking habits, snacking frequency; 21 studies [88%]), with habit–intention conflict inferred from projected behaviour patterns where intention is weak and habit strong. Such estimates can lack ecological validity, because habits and intentions tend to correlate positively and strongly (e.g., de Bruijn et al., 2012; van Bree et al., 2013). This is unsurprising: habits form through repetition of intentional actions (Lally & Gardner, 2013), and so, in the absence of intervention, habit and intentions should concur. Automatic action can proceed in the absence of conscious intention, but habitual actions need not be performed without, or contrary to, intention (Bargh, 1994). Additionally, intentions are always measured in relation to a single behavioural option (‘to what extent do you intend to do X?’). A weak intention to perform a behaviour (e.g., eat unhealthy snacks) need not, however, reflect a strong intention to perform an alternative (eat healthy snacks) or inhibit the focal behaviour (avoid eating unhealthy snacks). The distinction between the absence of a habit-congruent intention (not intending to do a habitual behaviour), and the presence of a counter-habitual intention (intending not to do a habitual behaviour), is important for action regulation. In one experimental study, participants who formed an intention to perform a counter-habitual action were able to consciously suppress their habitual responses and act in line with their intentions, contrary to TIB predictions (Danner et al., 2011). It has also been suggested that, where habits concur with intentions, habits can effectively facilitate the translation of intention into action (Neal et al., 2013). Habitual actions tend to persist even when self-regulatory resources are depleted, and so habits can shield pursuit of an intended (and habitual) behaviour from derailment which might otherwise occur when the will-power required to act on intention is diminished (Neal et al., 2013). More precise estimation of intention–habit conflict requires identification of situations or samples in which intentions are expected to shift, or have shifted, away from established habits. Only two studies (8%) have explored whether counter-intentional habits moderate intention–behaviour relationships, and neither found a habit–intention interaction (Gardner et al., 2012; Murtagh, Rowe, Elliott, McMinn, & Nelson, 2012).
Seventy-four behaviour prediction studies (90% of such studies) have used context-free habit measures, which may obscure true habit–behaviour relationships. Identification of habitual action requires specification of cues in both habit and behaviour measures, to differentiate between performances conditional upon associated contexts, and unconditional performances (Sniehotta, 2009). Conditional behaviour measures are most urgently demanded where contextual cues are rarely encountered, or where behaviour occurs non-habitually in other contexts (Sniehotta, 2009). In such situations, frequency is unlikely to reflect habit. This may add noise to habit–behaviour correlations. The timing of questionnaire administration may affect associations between habit, intention and behaviour (e.g., Schwarzer, 2014). Intentions may change or be forgotten between measurement and encountering action opportunities (e.g., Sheeran & Abraham, 2003). This may weaken observed intention–behaviour relationships, independently of habit. Real-time data collection methods are available that capture cognitions more proximal to the moment of action (Jones & Johnston, 2011).
Theory has also been inadequately tested at the individual level. Most (80; 98%) studies have exclusively modelled between-person variation in habit, based on aggregates of individuals' habit scores. Yet, habitual action is inherently idiosyncratic, based on personally acquired behavioural responses to personally meaningful cues. Within-person effects cannot be reliably interpreted from aggregations of processes that differ between people (Jaccard, 2012; Molenaar, 2004). Studies of between-person differences cannot reveal, for example, whether an individual is more likely to act in line with habits or counter-habitual intentions. Habit requires study as an intra-individual phenomenon (Conroy, Maher, Elavsky, Hyde, & Doerksen, 2013; Lally et al., 2010). More appropriate methods are available. For example, observational single-case designs can capture habit development, or the impact of habit on behaviour, within the individual by capturing multiple in-situ observations from one person over time (Lally et al., 2010). Similarly, N-of-1 trials can evaluate the impact of experimental manipulations versus control treatments as administered to one individual over several time points (Hobbs, Dixon, Johnston, & Howie, 2013). Multilevel modelling also facilitates individual-level analyses by estimating within-person variation while controlling for between-person variance (Conroy et al., 2013; Johnston & Johnson, 2013).
Predicting habit
Eleven (quantitative) studies have sought to predict or model habit strength (Supplemental Table 3). A distinction must be drawn between studies of the habit formation process, and observational studies of ongoing habits. Only formation studies, which focus on participants undergoing natural or purposive interventions to create new habits, are available (Fleig et al., 2013; Judah et al., 2013; Lally et al., 2010). Most (8; 73%) studies have sought to predict ongoing habits, by investigating determinants of habit over and above behavioural repetition, or moderators of the repetition–habit strength relationship. For example, one cross-sectional study examined the effect of self-determination on the relationship between past behaviour (as a proxy for behavioural repetition) and habit strength (Gardner & Lally, 2013). Studies of ongoing habits may obscure the temporal nature of relationships between context-dependent behavioural repetition and habit formation. In the formative stages, motivation prompts behavioural repetition, which in turn strengthens habit, and as habit develops, it acquires the potential to cue further repetition (Lally et al., 2010, 2011). Any given sample may consist of participants forming habits, for whom repetition should shape habit (Path C in Figure 1), and those with established habits, for whom habit should prompt repetition (Path A). Group-level aggregations of behaviour–habit correlation coefficients potentially conflate causal repetition-habit and habit-repetition effects, thereby overestimating the true size of either effect in isolation and precluding reliable interpretation of causality (Weinstein, 2007). This problem is not reliably circumvented by prospective designs in which baseline measures of behavioural repetition and additional factors are used to predict habit at a later point. After habit strength peaks, repetition has little impact on habit (Lally et al., 2010); habit should prompt behaviour, not vice versa. In the absence of intervention, habit strength and behaviour frequency should be stable over time (Verplanken & Orbell, 2003). ‘Predictive’ effects of behaviour frequency on later habit scores may reflect the impact of a stable habit on an ongoing behaviour, rather than a causal behaviour–habit effect (Weinstein, 2007).
Studies of ongoing habits have also been limited by a focus on between-person differences in habit strength. The between-person habit strength distribution in a given sample may not reflect the asymptotic distribution of within-person scores as habit forms (Lally et al., 2010). Between-person variance in habit may reflect variation in the level at which habit has peaked, or, for those engaged in formation attempts, the speed with which habit has developed. Correlational studies of between-participant differences give limited insight into the habit formation process.
Observing causal influences on habit strength requires a focus on longitudinal habit changes within individuals undergoing habit formation attempts (e.g., Lally et al., 2010), or the use of experimental methods to manipulate habit formation (e.g., Webb et al., 2009). Such studies are rare. Formation studies may be most ecologically valid in depicting processes of habit change, but are costly and time-consuming, as they demand an effective behaviour change intervention to initiate and maintain a formation attempt, and multiple long-term follow-up measures to record progress (e.g., Judah et al., 2013). Studies of ongoing habits can play an important but limited role as pilot studies, to identify hypotheses warranting further investigation (Weinstein, 2007).
Habit and behavioural change interventions
Habit theory yields important implications for behaviour change interventions: forming ‘good’ habits should maintain intervention impact over time, and unwanted habitual health-risk behaviours (‘bad habits’) might be resistant to change via deliberative pathways (Rothman et al., 2009; Verplanken & Wood, 2006). Only 21 behavioural intervention studies (15% of all studies; Supplemental Table 4) have incorporated habit in any capacity, and thirteen (62%) of these entered habit only as a potential covariate, mediator or moderator of effects on behaviour. Only eight (38%) interventions have explicitly been designed to change habits.
Habit formation may be used as an intervention outcome, or a behaviour change technique based on CDR (Michie et al., 2013). Seven (purposive) interventions have used habit formation in either capacity. Of these, four used formation as an outcome and a technique, to change dietary consumption and physical activity. Carels et al. (in press) found a habit-based diet and activity intervention to have greater impact on weight loss at six-month follow-up than a non-habit treatment, based on addressing relationships with food, body dissatisfaction and weight bias. Relative to a no-treatment control condition, habit-based interventions evaluated by Lally et al. (2008) and McGowan et al. (2013) yielded greater automaticity and behaviour gains at 8-week follow-up, and in both instances, automaticity change correlated positively with behaviour change indicators. Lally et al. (2008) also observed weight losses in the intervention group at 32-week follow-up. Wind, Kremers, Thijs, and Brug (2005) found that an intervention promoting brushing teeth daily at regular time points increased brushing at one-year follow-up, yet failed to modify habit strength.
One retrospective observational study focused on students' responses to a natural habit disruption intervention (moving university; Wood, Tam, & Guerrero Witt, 2005). Reduced engagement in previously habitual behaviours (watching TV and physical activity) was observed where the usual contexts for performance of those behaviours were deemed to be significantly different across the two universities.
Habit change interventions offer opportunities to test causal links between conscious motivation, habit and behaviour that cannot be reliably inferred from studies of ongoing habits (Weinstein, 2007). The few available intervention studies have demonstrated relationships between habit and gains in health-promoting behaviour (Lally et al., 2008; McGowan et al., 2013), and habit disruption and decreased engagement in unhealthy behaviours (Wood et al., 2005). However, key hypotheses remain untested. Habit formation interventions have been compared with unmatched active treatments, or no treatment, making it difficult to identify whether CDR advice is the ‘active ingredient’ of habit formation interventions. It is possible that simple advice to repeat a chosen behaviour may be more novel or easier to follow than non-CDR advice, so changing behaviour via deliberation, rather than habit. Comparisons of automaticity and behaviour changes in CDR-based interventions with matched non-CDR treatments are required to estimate the unique contribution of CDR advice to habit formation. Longer follow-ups are also required to test assumptions about the sustainability of habits over time.
Habit may inform behaviour change intervention design and evaluation in several respects. No intervention trial has yet used habit strength to identify intervention recipients, or to tailor intervention techniques (Michie & Prestwich, 2010). Such trials would inform theory by testing the assumption that self-regulatory strategies are more effective than intention change in disrupting habitual unhealthy behaviour (Verplanken & Wood, 2006). Formation and disruption studies tend to require investment of considerable time and financial resources to track habit change over time. Using intervention trials for theory testing purposes may maximise returns on this investment.
Discussion
Towards a new research agenda
Habit may be most coherently defined as a cognitive-motivational process, conceptually distinct from behaviour. The distinction between habit and behaviour is not new (e.g., Verplanken & Orbell, 2003), but its implications have not been fully considered. Habits are cue-contingent, such that the habit-generated impulse will not be activated when the cue is not encountered (Orbell & Verplanken, 2010). It is therefore possible for ‘habitual’ behaviours to be automatic yet infrequent. These might be thought of as ‘implicit habits’, whereby stored cue-response associations retain the potential to activate action impulses, but have not done so for some time because cues have not been encountered. ‘Implicit habits’ have important implications for predicting and changing behaviour. Discontinuation of cue exposure has been suggested as a method to disrupt habitual behaviour (Verplanken, Walker, Davis, & Jurasek, 2008), but may fail to yield lasting behaviour changes because returning to previous contexts after the intervention period may activate implicit habits. This offers one explanation as to why behavioural interventions typically yield short-term gains, which erode as old behaviours re-emerge (e.g., Jeffery et al., 1990). The habit–behaviour separation invokes a further distinction between the extinction of behaviour, and the unlearning, or overwriting, of cue-response associations (Bouton, 2000). It is possible that interventions designed to ‘break habits’ may discontinue habitually regulated behaviours yet fail to disrupt the underlying cue-response association, making spontaneous recovery of unwanted implicit habits a possibility. No empirical investigations of changes in habit following habit disruption interventions were found; the sole study to have observed people with strong habits following context disruption focused on behaviour, not habit, change (Wood et al., 2005). The habit behaviour distinction may not be important where cue exposure is permanently discontinued, such as when moving house (Verplanken et al., 2008). Empirical research is needed to investigate whether, when settings are only temporarily disrupted, habit recovery undermines long-term behaviour change, and the impact of discontinued cue exposure on habit strength.
The portrayal of habit as an impulse-generating process achieves consistency with theory and empirical evidence by recognising that habits may be inhibited (Quinn et al., 2010; Strack & Deutsch, 2004). The Reflective–Impulsive Model proposes that the impulsive processing system (which generates habitual behaviour) is constantly active, but reflective system activity depends on cognitive capacity (Strack & Deutsch, 2004). Thus, while the reflective system will be disengaged and impulses will regulate behaviour by default where cognitive capacity is diminished (Neal et al., 2013; Strack & Deutsch, 2004), impulsive behavioural tendencies can be inhibited where sufficient cognitive resources are available. Indeed, mindful in-situ self-monitoring of behaviour and contexts can block unwanted actions (Quinn et al., 2010). Self-control is cognitively effortful, and draws on finite resources that deplete through exertion, so reducing capacity for further self-regulation (Hagger, Wood, Stiff, & Chatzisarantis, 2009). Self-regulation depletion thus prevents inhibition of unwanted habits (Neal et al., 2013). Self-regulatory resources may however be mobilised by the formation of strong intentions (Fleig et al., 2013), and so counter-habitual intention formation may inhibit unwanted habitual actions (Danner et al., 2011). This qualifies predictions that intention modification will have little impact on habitual behaviour (Triandis, 1977), and suggests that self-regulatory skills training may be a valuable addition to interventions aimed at modifying habits via reflective motivation change. Further experimental research might establish the most effective methods for inhibiting habitual behaviour and disrupting cue-response associations.
This review highlighted important knowledge gaps around the role of habit in health behaviour. Fundamental theoretical predictions that, in unchanging contexts, habits will remain stable over time, consistently prompt behaviour, and override conscious deliberative tendencies (Triandis, 1977; Verplanken & Wood, 2006), have not been adequately tested. Little empirical attention has been paid to the sustainability of habits over time. One study found that gains in dental flossing automaticity partially eroded six months after cessation of a habit formation procedure (Judah et al., 2013). The potential for habit decay is underexplored. Other knowledge gaps exist because methodological problems have constrained theory-testing. For example, tests of habit–intention interactions have focused on concordant habits and intentions, which reveal little about the influence of ‘bad’ habits on the translation of ‘good’ intentions into action. Studies of counter-intentional habits and intentions are needed. Additionally, studies have relied heavily on observational and correlational designs to test causal relationships, typically among pre-existing behaviours and habits. Experimental designs, intervention trials, and longitudinal observational studies of habit formation or disruption offer valuable opportunities to establish causality and so may be used to apply, test and refine habit theory (e.g., Head & Noar, 2014; Michie & Prestwich, 2010; Rhodes, 2014).
This review focused solely on health-related habits, neglecting theoretical and empirical evidence from other epistemological strands of psychology. Nonetheless, it is important to assess the extent to which evidence derived from other sub-disciplines applies to health behaviour. Decades of research have consistently shown that learned stimulus-response associations can direct human action (e.g., Graybiel, 2008; James, 1891; Watson, 1913). Yet, the most compelling studies have been based on the automatisation of simple actions, such as pulling levers (Watson, 1913). It is important to consider the role(s) that habit may play in the broad behavioural categories of interest to health psychologists, such as dietary consumption, physical activity, or drinking alcohol. Further work is required to document more convincingly the relevance of habit to health behaviour.
Acknowledgements
The author thanks Phillippa Lally, Bas Verplanken and Robert West for invaluable comments on earlier draft of the manuscript. Thanks too to Gaby Judah, Phillippa Lally, Susan Michie and Robert West for stimulating conversations that led to the generation of ideas expressed in this paper.
Note
One study (Rhodes & de Bruijn, 2010) found habit to weaken intention–behaviour relationships for moderate physical activity but to strengthen intention–behaviour relations for vigorous physical activity, and so is counted twice in this and subsequent lists.
Supplemental data
Supplemental data for this article can be accessed here: http://dx.doi.org/10.1080/17437199.2013.876238.
References
- Adriaanse M. A., Oettingen B., Gollwitzer P. M., Hennes E. P., de Ridder D. T. D., de Wit J. B. F. When planning is not enough: Fighting unhealthy snacking habits by mental contrasting with implementation intentions (MCII) European Journal of Social Psychology. 2010:1277–1293. doi: 10.1002/ejsp.730. [DOI] [Google Scholar]
- Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991:179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- Ajzen I. Residual effects of past on later behavior: Habituation and reasoned action perspectives. Personality and Social Psychology Review. 2002:107–122. doi: 10.1207/S15327957PSPR0602_02. [DOI] [Google Scholar]
- Bargh J. A. The four horsemen of automaticity: Awareness, intention, efficiency, and control in social cognition. In: Wyer R. S., Srull T. K., editors. Handbook of social cognition. Hillsdale, NJ: Lawrence Erlbaum; 1994. pp. 1–40. [Google Scholar]
- Bolman C., Arwert T. G., Vollink T. Adherence to prophylactic asthma medication: Habit strength and cognitions. Heart & Lung. 2011:63–75. doi: 10.1016/j.hrtlng.2010.02.003. [DOI] [PubMed] [Google Scholar]
- Bouton M. E. A learning theory perspective on lapse, relapse, and the maintenance of behavior change. Health Psychology. 2000;(Suppl l):S57–S63. doi: 10.1037/0278-6133.19.Suppl1.57. [DOI] [PubMed] [Google Scholar]
- Campbell D. T. Enhancement of contrast as composite habit. The Journal of Abnormal and Social Psychology. 1956:350–355. doi: 10.1037/h0041013. [DOI] [PubMed] [Google Scholar]
- Carels R. A., Burmeister J. M., Koball A., Oehlhof M. W., Hinman N., LeRoy M., et al. Amanda G. A randomized trial comparing two approaches to weight loss: Differences in weight loss maintenance. Journal of Health Psychology. doi: 10.1177/1359105312470156. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy D. E., Maher J. P., Elavsky S., Hyde A. L., Doerksen S. E. Sedentary behavior as a daily process regulated by habits and intentions. Health Psychology. 2013:1149–1157. doi: 10.1037/a0031629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danner U. N., Aarts H., de Vries N. K. Habit formation and multiple means to goal attainment: Repeated retrieval of target means causes inhibited access to competitors. Personality and Social Psychology Bulletin. 2007:1367–1379. doi: 10.1177/0146167207303948. [DOI] [PubMed] [Google Scholar]
- Danner U. N., Aarts H., de Vries N. K. Habit vs. intention in the prediction of future behaviour: The role of frequency, context stability and mental accessibility of past behaviour. British Journal of Social Psychology. 2008:245–265. doi: 10.1348/014466607X230876. [DOI] [PubMed] [Google Scholar]
- Danner U. N., Aarts H., Papies E. K., de Vries N. K. Paving the path for habit change: Cognitive shielding of intentions against habit intrusion. British Journal of Health Psychology. 2011:189–200. doi: 10.1348/2044-8287.002005. [DOI] [PubMed] [Google Scholar]
- de Bruijn G. J., Rhodes R. E., van Osch L. Does action planning moderate the intention-habit interaction in the exercise domain? A three-way interaction analysis investigation. Journal of Behavioral Medicine. 2012:509–519. doi: 10.1007/s10865-011-9380-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit S., Dickinson A. Associative theories of goal-directed behaviour: A case for animal-human translational models. Psychological Research. 2009:463–476. doi: 10.1007/s00426-009-0230-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fidler J. A., Shahab L., West R. Strength of urges to smoke as a measure of severity of cigarette dependence: Comparison with the Fagerstrom Test for nicotine dependence and its components. Addiction. 2011:631–638. doi: 10.1111/j.1360-0443.2010.03226.x. [DOI] [PubMed] [Google Scholar]
- Fleig L., Pomp S., Parschau L., Barz M., Lange D., Schwarzer R., Lippke S. From intentions via planning and behavior to physical exercise habits. Psychology of Sport and Exercise. 2013:632–639. doi: 10.1016/j.psychsport.2013.03.006. [DOI] [Google Scholar]
- Gardner B., Abraham C., Lally P., de Bruijn G. J. Towards parsimony in habit measurement: Testing the convergent and predictive validity of an automaticity subscale of the self-report habit index. International Journal of Behavioral Nutrition and Physical Activity. 2012:102. doi: 10.1186/1479-5868-9-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner B., de Bruijn G. J., Lally P. A systematic review and meta-analysis of applications of the self-report habit index to nutrition and physical activity behaviours. Annals of Behavioral Medicine. 2011:174–187. doi: 10.1007/s12160-011-9282-0. [DOI] [PubMed] [Google Scholar]
- Gardner B., de Bruijn G. J., Lally P. Habit, identity, and repetitive action: A prospective study of binge-drinking in UK students. British Journal of Health Psychology. 2012:565–581. doi: 10.1111/j.2044-8287.2011.02056.x. [DOI] [PubMed] [Google Scholar]
- Gardner B., Lally P. Does intrinsic motivation strengthen physical activity habit? Modeling relationships between self-determination, past behaviour and habit strength. Journal of Behavioral Medicine. 2013:488–497. doi: 10.1007/s10865-012-9442-0. [DOI] [PubMed] [Google Scholar]
- Gardner B., Tang V. Reflecting on non-reflective action: An exploratory think-aloud study of self-report habit measures. British Journal of Health Psychology. doi: 10.1111/bjhp.12060. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graybiel A. M. Habits, rituals, and the evaluative brain. Annual Review of Neuroscience. 2008:358–387. doi: 10.1146/annurev.neuro.29.051605.112851. [DOI] [PubMed] [Google Scholar]
- Hagger M. S., Wood C., Stiff C., Chatzisarantis N. L. D. The strength model of self-regulation failure and health-related behaviour. Health Psychology Review. 2009:208–238. doi: 10.1080/17437190903414387. [DOI] [Google Scholar]
- Hall P. T., Fong G. T. Temporal self-regulation theory: A model for individual health behavior. Health Psychology Review. 2007:6–52. doi: 10.1080/17437190701492437. [DOI] [Google Scholar]
- Head K. J., Noar S. M. Facilitating progress in health behaviour theory development and modification: The reasoned action approach as a case study. Health Psychology Review. 2014:34–52. doi: 10.1080/17437199.2013.778165. [DOI] [PubMed] [Google Scholar]
- Hobbs N., Dixon D., Johnston M., Howie K. Can the theory of planned behaviour predict the physical activity behaviour of individuals. Psychology & Health. 2013:234–249. doi: 10.1080/08870446.2012.716838. [DOI] [PubMed] [Google Scholar]
- Hofmann W., Friese M., Wiers R. W. Impulsive versus reflective influences on health behavior: A theoretical framework and empirical review. Health Psychology Review. 2008:111–137. doi: 10.1080/17437190802617668. [DOI] [Google Scholar]
- Hull C. L. Principles of behavior: An introduction to behavior theory. New York, NY: Appleton-Century-Crofts; 1943. [Google Scholar]
- Jaccard J. The reasoned action model: Directions for future research. The Annals of the American Academy of Political and Social Science. 2012:58–80. doi: 10.1177/0002716211426097. [DOI] [Google Scholar]
- James W. The principles of psychology. London: Macmillan; 1891. [Google Scholar]
- Jeffery R. W., Drewnowski A., Epstein L. H., Stunkard A. J., Wilson G. T., Wing R. R. Long-term maintenance of weight loss: Current status. Health Psychology. 1990;(Suppl 1):S5–S16. doi: 10.1037/0278-6133.19.suppl1.5. [DOI] [PubMed] [Google Scholar]
- Ji M. F., Wood W. Purchase and consumption habits: Not necessarily what you intend. Journal of Consumer Psychology. 2007:261–276. doi: 10.1016/S1057-7408(07)70037-2. [DOI] [Google Scholar]
- Johnston D. W., Johnson M. Useful theories should apply to individuals. British Journal of Health Psychology. 2013:469–473. doi: 10.1111/bjhp.12049. [DOI] [PubMed] [Google Scholar]
- Jones M. C., Johnston D. Understanding phenomena in the real world: The case for real time data collection. Journal of Health Services Research and Policy. 2011:172–176. doi: 10.1258/jhsrp.2010.010016. [DOI] [PubMed] [Google Scholar]
- Judah G., Gardner B., Aunger R. Forming a flossing habit: An exploratory study of the psychological determinants of habit formation. British Journal of Health Psychology. 2013:338–353. doi: 10.1111/j.2044-8287.2012.02086.x. [DOI] [PubMed] [Google Scholar]
- Lally P., Chipperfield A., Wardle J. Healthy habits: Efficacy of simple advice on weight control based on a habit-formation model. International Journal of Obesity. 2008:700–707. doi: 10.1038/sj.ijo.0803771. [DOI] [PubMed] [Google Scholar]
- Lally P., Gardner B. Promoting habit formation. Health Psychology Review. 2013;(Suppl 1):S137–S158. doi: 10.1080/17437199.2011.603640. [DOI] [Google Scholar]
- Lally P., van Jaarsveld C. H. M., Potts H. W. W., Wardle J. How are habits formed: Modelling habit formation in the real world. European Journal of Social Psychology. 2010:998–1009. doi: 10.1002/ejsp.674. [DOI] [Google Scholar]
- Lally P., Wardle J., Gardner B. Experiences of habit formation: A qualitative study. Psychology, Health & Medicine. 2011:484–489. doi: 10.1080/13548506.2011.555774. [DOI] [PubMed] [Google Scholar]
- Maddux J. E. Habit, health and happiness. Journal of Sport & Exercise Psychology. 1997:331–346. [Google Scholar]
- McGowan L., Cooke L. J., Gardner B., Beeken R., Croker H., Wardle J. Healthy feeding habits: Efficacy results from a cluster-randomized, controlled exploratory trial of a novel, habit-based intervention with parents. American Journal of Clinical Nutrition. 2013:769–777. doi: 10.3945/ajcn.112.052159. [DOI] [PubMed] [Google Scholar]
- Michie S., Prestwich A. Are interventions theory-based? Development of a theory coding scheme. Health Psychology. 2010:1–8. doi: 10.1037/a0016939. [DOI] [PubMed] [Google Scholar]
- Michie S., Richardson M., Johnston M., Abraham C., Francis J., Hardeman W., et al. Wood C. E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine. 2013:81–95. doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- Michie S., West R. Behaviour change theory and evidence: A presentation to Government. Health Psychology Review. 2013:1–22. doi: 10.1080/17437199.2011.649445. [DOI] [Google Scholar]
- Molenaar P. C. M. A manifesto on psychology as an idiographic science: Bringing the person back into scientific psychology, this time forever. Measurement: Interdisciplinary Research and Perspectives. 2004:201–218. doi: 10.1207/s15366359mea0204_1. [DOI] [Google Scholar]
- Murtagh S., Rowe D. A., Elliott M. A., McMinn D., Nelson N. M. Predicting active school travel: The role of planned behavior and habit strength. International Journal of Behavioral Nutrition and Physical Activity. 2012:65. doi: 10.1186/1479-5868-9-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neal D. T., Wood W., Drolet A. How do people adhere to goals when willpower is low? The profits (and pitfalls) of strong habits. Journal of Personality and Social Psychology. 2013:959–975. doi: 10.1037/a0032626. [DOI] [PubMed] [Google Scholar]
- Neal D. T., Wood W., Labrecque J. S., Lally P. How do habits guide behavior? Perceived and actual triggers of habits in daily life. Journal of Experimental Social Psychology. 2012:492–498. doi: 10.1016/j.jesp.2011.10.011. [DOI] [Google Scholar]
- Neal D. T., Wood W., Wu M., Kurlander D. The pull of the past: When do habits persist despite conflict with motives. Personality and Social Psychology Bulletin. 2011:1428–1437. doi: 10.1177/0146167211419863. [DOI] [PubMed] [Google Scholar]
- Nilsen P., Bourne M., Verplanken B. Accounting for the role of habit in behavioural strategies for injury prevention. International Journal of Injury Control and Safety Promotion. 2008:33–40. doi: 10.1080/17457300701794253. [DOI] [PubMed] [Google Scholar]
- Nilsen P., Roback K., Broström A., Ellström P.-E. Creatures of habit: Accounting for the role of habit in implementation research on clinical behaviour change. Implementation Science. 2012:53. doi: 10.1186/1748-5908-7-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman P. The theory of planned behavior and binge drinking among undergraduate students: Assessing the impact of habit strength. Addictive Behaviors. 2011:502–507. doi: 10.1016/j.addbeh.2011.01.025. [DOI] [PubMed] [Google Scholar]
- Orbell S., Verplanken B. The automatic component of habit in health behavior: Habit as cue-contingent automaticity. Health Psychology. 2010:374–383. doi: 10.1037/a0019596. [DOI] [PubMed] [Google Scholar]
- Ouellette J. A., Wood W. Habit and intention in everyday life: The multiple processes by which past behavior predicts future behavior. Psychological Bulletin. 1998:54–74. doi: 10.1037/0033-2909.124.1.54. [DOI] [Google Scholar]
- Quinn J. M., Pascoe A., Wood W., Neal D. T. Can't control yourself? Monitor those bad habits. Personality and Social Psychology Bulletin. 2010:499–511. doi: 10.1177/0146167209360665. [DOI] [PubMed] [Google Scholar]
- Rhodes R. E. Improving translational research in building theory: A commentary on Head and Noar. Health Psychology Review. 2014:57–60. doi: 10.1080/17437199.2013.814921. [DOI] [PubMed] [Google Scholar]
- Rhodes R., de Bruijn G. J. Automatic and motivational correlates of physical activity: Does intensity moderate the relationship. Behavioral Medicine. 2010:44–52. doi: 10.1080/08964281003774901. [DOI] [PubMed] [Google Scholar]
- Rothman A. J., Sheeran P., Wood W. Reflective and automatic processes in the initiation and maintenance of dietary change. Annals of Behavioral Medicine. 2009;(Suppl 1):S4–S17. doi: 10.1007/s12160-009-9118-3. [DOI] [PubMed] [Google Scholar]
- Schwarzer R. Life and death of health behaviour theories. Health Psychology Review. 2014:53–56. doi: 10.1080/17437199.2013.810959. [DOI] [PubMed] [Google Scholar]
- Sheeran P., Abraham C. Mediator of moderators: Temporal stability of intention and the intention-behavior relation. Personality and Social Psychology Bulletin. 2003:205–215. doi: 10.1177/0146167202239046. [DOI] [PubMed] [Google Scholar]
- Sniehotta F. F. Towards a theory of intentional behaviour change: Plans, planning, and self-regulation. British Journal of Health Psychology. 2009:261–273. doi: 10.1348/135910708X389042. [DOI] [PubMed] [Google Scholar]
- Sniehotta F. F., Presseau J. The habitual use of the self-report habit index. Annals of Behavioral Medicine. 2012:139–140. doi: 10.1007/s12160-011-9305-x. [DOI] [PubMed] [Google Scholar]
- Spielberger C. D. Psychological determinants of smoking behavior. In: Tollison R. D., editor. Smoking and society: Toward a more balanced assessment. Lexington: D. C. Heath; 1986. pp. 89–134. Retrieved December 6, 2013, from http://legacy.library.ucsf.edu/tid/pru35d00/pdf. [Google Scholar]
- Strack F., Deutsch R. Reflective and impulsive determinants of social behavior. Personality and Social Psychology Review. 2004:220–247. doi: 10.1207/s15327957pspr0803_1. [DOI] [PubMed] [Google Scholar]
- Tappe K. A., Glanz K. Measurement of exercise habits and prediction of leisure-time activity in established exercise. Psychology, Health and Medicine. 2013:601–611. doi: 10.1080/13548506.2013.764458. [DOI] [PubMed] [Google Scholar]
- Triandis H. Interpersonal behavior. Monterey, CA: Brooks-Cole; 1977. [Google Scholar]
- van Bree R. J. H., van Stralen M. M., Bolman C., Mudde A. N., de Vries H., Lechner L. Habit as moderator of the intention-physical activity relationship in older adults: A longitudinal study. Psychology & Health. 2013:514–532. doi: 10.1080/08870446.2012.749476. [DOI] [PubMed] [Google Scholar]
- van t'Riet J., Sijtsema S. J., Dagevos H., de Bruijn G.-J. The importance of habits in eating behaviour. An overview and recommendations for future research. Appetite. 2011:585–596. doi: 10.1016/j.appet.2011.07.010. [DOI] [PubMed] [Google Scholar]
- Verplanken B. Habits and implementation intentions. In: Kerr J., Weitkunat R., Moretti M., editors. The ABC of behavior change. Oxford: Elsevier; 2005. pp. 99–109. [Google Scholar]
- Verplanken B., Orbell S. Reflections on past behavior: A self-report index of habit strength. Journal of Applied Social Psychology. 2003:1313–1330. doi: 10.1111/j.1559-1816.2003.tb01951.x. [DOI] [Google Scholar]
- Verplanken B., Walker I., Davis A., Jurasek M. Context change and travel mode choice: Combining the habit discontinuity and self-activation hypotheses. Journal of Environmental Psychology. 2008:121–127. doi: 10.1016/j.jenvp.2007.10.005. [DOI] [Google Scholar]
- Verplanken B., Wood W. Interventions to break and create consumer habits. Journal of Public Policy & Marketing. 2006:90–103. doi: 10.1509/jppm.25.1.90. [DOI] [Google Scholar]
- Watson J. B. Psychology as the behaviorist views it. Psychological Review. 1913:158–177. doi: 10.1037/h0074428. [DOI] [Google Scholar]
- Webb T. L., Sheeran P., Luszczynska A. Planning to break unwanted habits: Habit strength moderates implementation intention effects on behaviour change. British Journal of Social Psychology. 2009:507–523. doi: 10.1348/014466608X370591. [DOI] [PubMed] [Google Scholar]
- Weinstein N. D. Misleading tests of health behavior theories. Annals of Behavioral Medicine. 2007:1–10. doi: 10.1207/s15324796abm3301_1. [DOI] [PubMed] [Google Scholar]
- West R., Brown J. Theory of addiction. 2nd ed. Chichester: Wiley-Blackwell; 2013. [Google Scholar]
- Wind M., Kremers S., Thijs C., Brug J. Toothbrushing at school: Effects on toothbrushing behaviour, cognitions and habit strength. Health Education. 2005:53–61. doi: 10.1108/09654280510572303. [DOI] [Google Scholar]
- Wood W., Neal D. T. The habitual consumer. Journal of Consumer Psychology. 2009:579–592. doi: 10.1016/j.jcps.2009.08.003. [DOI] [Google Scholar]
- Wood W., Tam L., Guerrero Witt M. Changing circumstances, disrupting habits. Journal of Personality and Social Psychology. 2005:918–933. doi: 10.1037/0022-3514.88.6.918. [DOI] [PubMed] [Google Scholar]


