Abstract
A new health surveillance protocol for work-related upper-extremity musculoskeletal disorders has been validated by comparing the results with a reference protocol. The studied protocol, Health Surveillance in Adverse Ergonomics Conditions (HECO), is a new version of the reference protocol modified for application in the Occupational Health Service (OHS). The HECO protocol contains both a screening part and a diagnosing part. Sixty-three employees were examined. The screening in HECO did not miss any diagnosis found when using the reference protocol, but in comparison to the reference protocol considerable time savings could be achieved. Fair to good agreement between the protocols was obtained for one or more diagnoses in neck/shoulders (86%, k = 0.62) and elbow/hands (84%, k = 0.49). Therefore, the results obtained using the HECO protocol can be compared with a reference material collected with the reference protocol, and thus provide information of the magnitude of disorders in an examined work group.
Practitioner Summary: The HECO protocol is a relatively simple physical examination protocol for identification of musculoskeletal disorders in the neck and upper extremities. The protocol is a reliable and cost-effective tool for the OHS to use for occupational health surveillance in order to detect workplaces at high risk for developing musculoskeletal disorders.
Keywords: physical examination, OHS, neck/shoulder, upper extremities, upper limb, HECO
1. Introduction
Musculoskeletal disorders (MSDs) in neck and upper extremities are common in the working population in industrial countries (Walker-Bone et al. 2004; Roquelaure et al. 2006). However, according to a review of epidemiological studies (1966–2004), the reported prevalence varies considerably across occupations and working populations (Huisstede et al. 2006). The annual prevalence of neck pain ranged from 19% to 48% and the range for upper-extremity MSDs was 12–41%. These variations are probably due to, for example, different diagnostic criteria and different populations (Buckle and Devereux 1999; Huisstede et al. 2006; Côté et al. 2008). In 2011, 35% of the Swedish working population (women 42%, men 28%) reported experience of pain in neck and upper back during the last week. Thirty per cent (women 36%, men 25%) reported pain in upper extremities (Swedish Work Environmental Authority 2012). In addition to the suffering and decreased quality of life for the individual, these disorders cause a heavy economic burden on society due to costs connected to sick leave, poorer work performance and reduced productivity (Hagberg et al. 2007; Boström et al. 2008).
In 1989, the Council of European Communities identified the importance of regular health surveillance in workplace to detect Work-Related Upper-extremity Musculoskeletal Disorders (Directive 1989/391/EEC). It has been stated by the scientific committee on musculoskeletal disorders of the international commission on occupational health that the methods for health surveillance should be designed for use in practical occupational settings (Hagberg et al. 2012). In order to prevent work-related musculoskeletal disorders, there is a need for methods that can identify both workplaces where the number of musculoskeletal disorders is high as well as individuals who are in an early phase of developing disorders. The occupational health services need methods that are valid, reliable and cost efficient.
Different examination protocols have been developed to identify work-related musculoskeletal disorders in the upper-extremities, e.g. by Sluiter, Rest, and Fring-Dresen (2001) and Walker-Bone et al. (2002). Another standard protocol for clinical examination of the neck and upper extremities with predefined criteria for various diagnoses was developed in 1994 for research purposes by Ohlsson et al. (1994). The criteria used to define diagnoses in this protocol are very similar to those later suggested by Palmer et al. (2000) and Sluiter, Rest, and Fring-Dresen (2001). However, in contrast to these protocols, the protocol by Ohlsson et al. (1994) also includes the diagnosis tension neck syndrome, which later was found to be important as a work-related diagnosis in a review by Palmer and Smedley (2007). Tension neck syndrome is a common diagnosis and furthermore, differences in prevalence between exposed and unexposed groups have been found (Nordander et al. 2009). The protocol has been used in several occupational settings, and comparisons concerning the proportion of affected individuals with musculoskeletal symptoms and diagnoses in different occupational groups have been made in epidemiological studies (Nordander et al. 2009). This means there is a large reference material, described elsewhere (Nordander et al. 2009), which is based on occupational groups to compare new examined groups with. Since the original protocol was developed for research use, it is, however, an unnecessarily long and detailed protocol to use by the Occupational Health Service (OHS). Therefore, the protocol has been modified for onsite health surveillance evaluation at the workplace. Furthermore, for additional cost-efficiency, it has been completed with a screening part prior to the detailed physical examination, similar to other examination protocols with a screening part and a physical examination part (e.g. Sluiter, Rest, and Fring-Dresen 2001). The modified protocol is called Health Surveillance in Adverse Ergonomics Conditions (HECO, in Swedish MEBA). The intention is to offer the OHS a valid, reliable and cost-effective method to identify work places with high risk for developing musculoskeletal disorders in neck and upper extremities but also individuals who are in the early phase of developing musculoskeletal disorders (Nordander et al. 2009). In order to use the reference material for identifying work places with high risks, the HECO protocol need to be valid compared to the original protocol.
The aim of the present study was to validate the HECO protocol in an occupational health service setting.
2. Material and methods
2.1 Examined group
In order to obtain the best conditions to investigate the concurrent validity, data were collected in a sample of female-dominated occupations which are known to have a high prevalence of musculoskeletal disorders in neck and upper extremities (Charles, Loomis, and Demissie 2009; Hayes, Cockrell, and Smith 2009; Nordander et al. 2008). The examinations were performed on 63 employees in dentistry (33), cleaning (17) and kitchen work (13). Their mean age was 49 years (range 23–67), and they were all employed in the public health service in southern Sweden. Sixty of them were females.
2.2 Experimental procedure
Each employee was examined both according to the protocol by Ohlsson et al. (1994) that used as the reference protocol and the HECO protocol. Half of them were randomly examined with the HECO protocol first and the other half with the reference protocol first. They were all examined at their normal workplace according to a 30-minute schedule with an interval of a few minutes between the two examinations.
The examinations according to the reference protocol were carried out by a physician (CN) with long experience of this protocol, and the examinations according to the HECO protocol by an occupational healthcare physiotherapist (DJ) who was experienced with this protocol. The physiotherapist had been trained in HECO by the physician during a one-day course about two years before data collection in the present study, and had since then used it in daily practice.
The two examiners were blinded to each other's findings. During the examination, the results were noted manually on a form by the examiners themselves. The examiners did not discuss their findings with the examined during the examination. The examined were instructed not to provide the second examiner with any information regarding the first examination.
2.2.1 The reference protocol
The protocol by Ohlsson et al. (1994) with small revisions proposed by Nordander et al. (2009) was used as the reference protocol. The reference protocol did not contain any screening part prior to the detailed physical examinations of the neck and upper extremities; all employees answered every question about symptoms and underwent every test, whether they experienced symptoms or not. Tests included range of motion, tenderness at palpation, and pain or tingling at specific provocations of joints, tendons, muscles or nerves. The whole protocol took about 30 minutes to complete. Nine specific diagnoses for the neck/shoulders region and 10 for the elbows/hands region could be established from predefined criteria. The anatomical regions and the predefined diagnoses are shown in Table 1. The criteria for each diagnose have been published earlier (Nordander et al. 2009).
Table 1 . Diagnoses according to predefined criteria (Nordander et al. 2009).
| Anatomical region | Specific diagnoses |
|---|---|
| Neck/shoulder | |
| Neck | Tension neck syndrome |
| Cervicalgia | |
| Cervical syndrome | |
| Thoracic outlet syndrome | |
| Shoulder | Frozen shoulder |
| Acromioclavicular syndrome | |
| Bicipital tendonitis | |
| Supraspinatus tendinitis | |
| Infraspinatus tendonitis | |
| Elbow/hand | |
| Elbow/forearm | Lateral epicondylitis |
| Medial epicondylitis | |
| Ulnar nerve entrapment at the elbow | |
| Pronator teres syndrome | |
| Radial tunnel syndromePeritendonitis/tenosynovitis | |
| Wrist/hand | Overused hand syndrome |
| De Quervains tendonitis | |
| Carpal tunnel syndrome | |
| Ulnar nerve entrapment at the wrist | |
2.2.2 HECO protocol
The HECO protocol contains separate sections for the two anatomical regions neck/shoulders and elbows/hands. Each of these sections consists of two parts: a short screening part and a detailed physical examination part. The detailed examination is performed only if the screening part indicates symptoms in the actual anatomical region. Thus, it was possible for the HECO examination to consist of the screening part only for one anatomical region, e.g. neck/shoulders, and the screening part followed by the full physical examination for the other region. The full HECO protocol, i.e. the screening part and the detailed physical examination part, includes all the questions and tests of the reference protocol that are needed to define the 9 specific diagnoses for the neck/shoulders region and the 10 for the elbows/hands region included in the reference protocol.
2.2.1.2 The screening part
The criteria for diagnoses (Table 1), all require that the examined report ongoing symptoms (most often pain), not only positive reactions to different tests at the detailed examination. Therefore, those who are symptom free can never be diagnosed with a specific disorder. The screening part consists of interview questions about symptoms and a basic physical examination. The examined were asked about perceived symptoms in the neck, shoulders, elbows or hands during the past 7 days and the past 12 months according to the Nordic Questionnaire (Kuorinka et al. 1987). Further frequency of symptoms during the past 12 months and intensity of symptoms during the past 7 days were explored. The basic physical examination for the neck/shoulders section consists of active motions in neck and shoulders and for the elbows/hands section active movements in the elbow and test of hand grip strength. The screening part took about 10 minutes for each subject to perform.
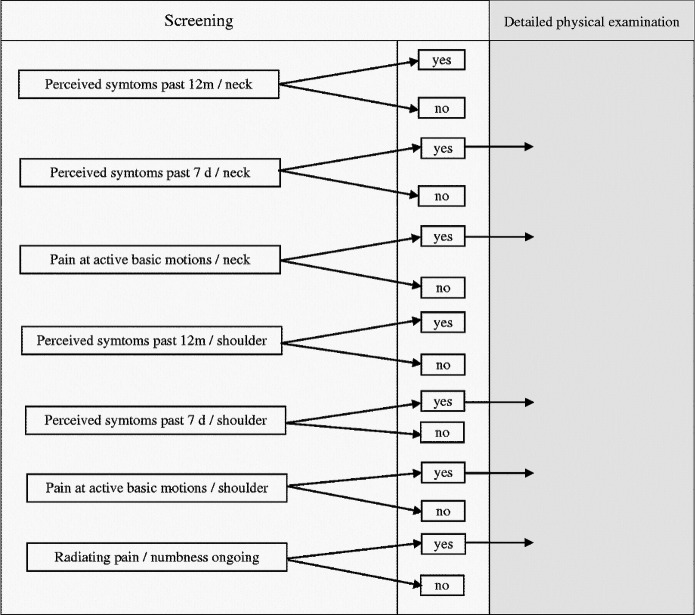
If the examined reported pain or discomfort, radiating pain or numbness during the past 7 days, or if pain or pronounced reduced mobility was elicited in the basic examination, or in the case of doubt, the examiner continued with the detailed physical examination (described below) of the actual anatomical region. Otherwise, only the screening part of HECO was performed (Figure 1).
Figure 1 . Flow chart for the screening procedure in HECO for the neck/shoulders region. Corresponding flow is also used for the elbows/hands region.
The question about perceived pain during the past 12 months was included in the screening procedure because information about this can be valuable in the case of doubt if the actual examined should be qualified for the more detailed physical examination or not (Sluiter, Rest, and Fring-Dresen 2001).
2.2.1.3 The detailed physical examination part
The detailed additional physical examination consisted of further questions about symptoms, palpation and functional examination of the actual anatomical region. All relevant examinations in the reference protocol were performed. Those with shoulder symptoms were also examined regarding neck disorders. As mentioned before, the same diagnoses as in the reference protocol, i.e. 9 specific diagnoses for the neck/shoulders region (whereof seven on either the left or the right side), and 10 for each elbows/hands region could be established if the predefined criteria were fulfilled (Table 1). The physical examination took about 20 minutes for each subject to perform.
2.4 Data analysis
A computer algorithm was used to transform the results from both protocols into the various diagnoses. The observed agreement is presented as a percentage with 95% confidence interval (95% CI). The agreement between the eliciting items for the two protocols was also assessed by calculating Cohen's kappa coefficient (κ) for categorical variables. Kirkwood's criteria were used to assess the kappa values (Kirkwood and Jonatan 2003). According to these criteria, values of κ>0.75 were considered to denote excellent agreement, 0.4–0.75 fair to good agreement and < 0.4 moderate to low agreement. All statistical calculations were performed using SPSS (Chicago, IL, USA, version 15.0).
3. Results
3.1 Screening procedure
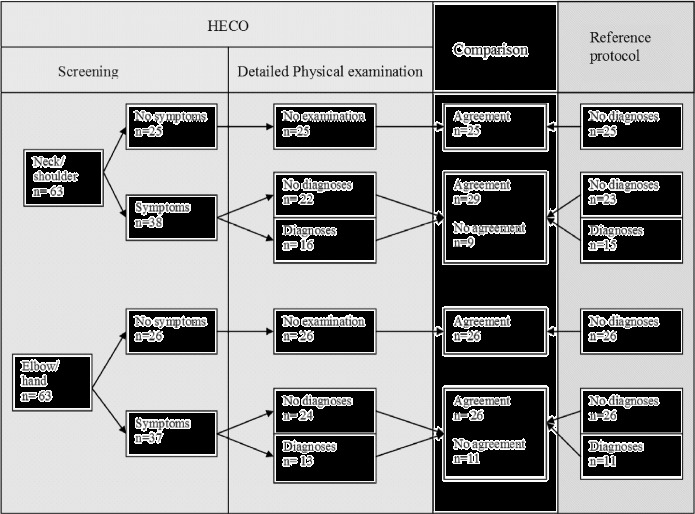
When screening for the neck/shoulders region, 21 examined reported pain as a result of the basic active motions for neck and/or shoulders. These individuals reported also pain in at least one of the three possible types of pain (ongoing radiated pain; pain from the neck and/or pain from the shoulders during the past seven days), qualifying for the detailed physical examination. Fifteen examined reported pain only and two examined had pain only as a result of the basic motions. In total, 38 of the examined were qualified for the detailed physical examination (Figure 2).
Figure 2 . Comparison of the results obtained using the HECO protocol and the reference protocol regarding symptoms and diagnoses in the neck/shoulders and elbows/hands region. N, number of examined employees.
When screening for the elbows/hands region, 15 examined reported pain as a result of the basic active motions for elbows and/or hands. These individuals reported also pain in at least one of the three possible types of pain (ongoing radiated pain; pain from the elbow and /or pain from the hands during the past seven days), qualifying for the detailed physical examination.
Twenty-two reported pain only. In total, 37 of the examined were qualified for the detailed physical examination for the elbows/hands region (Figure 2).
Of the 63 employees examined with the HECO protocol, 20 were only screened and underwent no detailed physical examination. Among these, no diagnoses were found according to the reference protocol in either the neck/shoulder or elbow/hand regions (Figure 2). Hence, no diagnoses were missed by the screening procedure of the HECO, and there was complete agreement between the protocols concerning examined not reporting symptoms. Screening of both anatomical regions took about 10 minutes to perform. Screening and full examination of both regions took about 30 minutes.
3.2 Prevalence of one or more diagnoses
The prevalence of one or more diagnoses in the neck/shoulders region was 24% using the HECO protocol versus 25% for the reference protocol. The corresponding values for elbows/hands diagnoses were 21% versus 17%.
The observed agreement was high, ranging from 86% to 92% in the neck/shoulders region, and from 84% to 94% in the elbows/hands region (Table 2). For the neck/shoulders region, the kappa coefficients varied between 0.49 and 0.75. The kappa coefficients for the elbows/hands region were lower, varying between 0.32 and 0.56.
Table 2 . Observed agreement between the HECO protocol and the reference protocol for one or more diagnoses.
| HECO/Reference protocola | ||||||
|---|---|---|---|---|---|---|
| One or more diagnoses | − / − | +/ − | − /+ | +/+ | Observed agreement % (95% CI) | κ |
| Neck/shoulder region | 43 | 5 | 4 | 11 | 86 (77–95) | 0.62 |
| Neck | 48 | 5 | 4 | 6 | 86 (77–95) | 0.49 |
| Shoulder | 48 | 3 | 2 | 10 | 92 (85–99) | 0.75 |
| Elbow/hand region | 46 | 6 | 4 | 7 | 84 (75–93) | 0.49 |
| Elbow/lower arm | 58 | 4 | 0 | 1 | 94 (88–100) | 0.32 |
| Wrist/hand | 48 | 4 | 4 | 7 | 89 (81–97) | 0.56 |
Note: Observed agreement in percentage with 95% confidence interval (95% CI) and the kappa coefficients (κ) are given.
− / − , no diagnosis with either protocol;+/ − , positive diagnosis with HECO, no diagnosis with the reference protocol; − /+, no diagnosis with HECO, positive diagnosis with the reference protocol;+/+, positive diagnosis with both protocols.
3.3 Specific neck/shoulder diagnoses
The observed agreement was high (90–100%) for all the diagnoses in the neck and shoulder (Table 3). However, the κ coefficients varied considerably between the specific neck diagnoses, from − 0.04 to 0.68. The highest κ coefficient was found for tension neck syndrome, and the lowest for cervicalgia.
Table 3 . Observed agreement between the HECO protocol and the reference protocol for specific clinical diagnoses of neck/shoulder disorders.
| HECO/reference protocolb | ||||||
|---|---|---|---|---|---|---|
| Diagnosisa | − / − | +/ − | − /+ | +/+ | Observed agreement % (95% CI)c | κd |
| Neck | ||||||
| Tension neck syndrome | 54 | 2 | 2 | 5 | 94 (88 − 100) | 0.68 |
| Cervicalgia | 58 | 2 | 3 | 0 | 92 (85 − 99) | − 0.04 |
| Cervical syndrome R | 62 | 1 | 0 | 0 | 98 (95–101) | – |
| Thoracic outlet Syndrome R | 62 | 1 | 0 | 0 | 98 (95–101) | – |
| Shoulder | ||||||
| Frozen shoulder R | 58 | 4 | 1 | 1 | 94 (88–100) | 0.32 |
| Frozen shoulder L | 62 | 0 | 1 | 0 | 98 (95–101) | – |
| Supraspinatus tendonitis R | 58 | 1 | 3 | 1 | 94 (88–100) | 0.30 |
| Supraspinatus tendonitis L | 62 | 0 | 0 | 1 | 100 (–) | 1.00 |
| Infraspinatus tendonitis R | 60 | 1 | 2 | 0 | 95 (90–100) | − 0.02 |
| Infraspinatus tendonitis L | 62 | 0 | 1 | 0 | 98 (95–101) | – |
| Bicipital tendonitis R | 56 | 2 | 4 | 1 | 90 (83–97) | 0.20 |
| Bicipital tendonitis L | 62 | 0 | 1 | 0 | 98 (95–101) | – |
| Acromioclavicular syndrome R | 52 | 3 | 3 | 5 | 90 (83–97) | 0.57 |
| Acromioclavicular syndrome L | 60 | 0 | 1 | 2 | 98 (95–101) | 0.79 |
Note: Observed agreement in percentage with 95% confidence interval (95% CI) and the kappa coefficients (κ) are given. R, right side; L, left side.
Neither of the examiners found any subjects with cervical syndrome or thoracic outlet syndrome on the left side, and therefore not shown in the table.
− / − , no diagnosis with either protocol;+/ − , positive diagnosis with HECO, no diagnosis with the reference protocol; − /+, no diagnosis with HECO, positive diagnosis with the reference protocol;+/+, positive diagnosis with both protocols.
The 95% confidence interval cannot be calculated when the observed agreement is 100%.
κcoefficients cannot be calculated when a diagnosis was only recorded by one of the examiners.
The κ coefficients also varied widely for the specific shoulder diagnoses: from − 0.02 to 1.00. The highest values were 0.79 for acromioclavicular syndrome (left side) and 1.00 for supraspinatus tendonitis (left side). Lower κ coefficients were found for bicipital tendonitis, supraspinatus tendonitis and frozen shoulder syndrome on the right side, the values being 0.20, 0.30 and 0.32, respectively. Values of κ could be calculated for nine diagnoses. In the other cases, a diagnosis was made by only one of the examiners (i.e. with one of the protocols), and it was thus not possible to calculate any kappa coefficients.
3.4 Specific elbow/hand diagnoses
An observed agreement of 100% was found in seven of the diagnoses: lateral and medial epicondylitis (bilaterally), radial tunnel syndrome (bilaterally) and pronator teres syndrome on the right side (Table 4). Regarding pronator teres syndrome on the right side, the examiner using the HECO protocol made this diagnosis in three subjects, while the other examiner, using the reference protocol, did not diagnose this condition in any of the subjects.
Table 4 . Observed agreement between the HECO protocol and the reference protocol for specific clinical diagnoses of elbow/hand disorders.
| HECO/Reference protocolb | ||||||
|---|---|---|---|---|---|---|
| Diagnosisa | − / − | +/ − | − /+ | +/+ | Observed agreement % (95% CI) | κc |
| Elbow/forearm | ||||||
| Ulnar nerve entrapment elbow R | 61 | 1 | 0 | 1 | 98 (95–101) | 0.66 |
| Ulnar nerve entrapment elbow L | 62 | 1 | 0 | 0 | 98 (95–101) | – |
| Pronator teres syndrome R | 60 | 3 | 0 | 0 | 95 (90–100) | – |
| Wrist/hand | ||||||
| De Quervain's disease R | 61 | 2 | 0 | 0 | 97 (93–101) | – |
| De Quervain's disease L | 61 | 2 | 0 | 0 | 97 (93–101) | – |
| Overused hand syndrome R | 60 | 0 | 3 | 0 | 95 (90–100) | – |
| Carpal tunnel syndrome R | 52 | 3 | 3 | 5 | 90 (83–97) | 0.58 |
| Carpal tunnel syndrome L | 59 | 0 | 3 | 1 | 95 (90–100) | 0.38 |
| Ulnar nerve entrapment R | 61 | 1 | 1 | 0 | 97 (93–101) | − 0.02 |
| Ulnar nerve entrapment L | 62 | 1 | 0 | 0 | 98 (95–101) | – |
Note: Observed agreement in percentage with 95% confidence interval (95% CI) and the kappa coefficients (κ) are given. R, right side; L, left side.
Neither of the examiners made the diagnoses lateral or medial epicondylitis, radial tunnel syndrome or peritendonitis/tenosynovitis on either side, nor pronator teres syndrome or overused hand syndrome on the left side, and therefore not shown in the table.
− / − , no diagnosis with either protocol;+/ − , positive diagnosis with HECO, no diagnosis with the reference protocol; − /+, no diagnosis with HECO, positive diagnosis with the reference protocol;+/+, positive diagnosis with both protocols.
κ coefficients cannot be calculated when a diagnosis was only recorded by one of the examiners.
Only one κ coefficient could be calculated for the specific elbow/forearm diagnoses, i.e. ulnar nerve entrapment on the right side (κ = 0.66). No kappa coefficients could be calculated for the remaining nine diagnoses.
No differences were found between the two protocols for peritendonitis bilaterally and overused hand syndrome on the left side, giving 100% observed agreement. The κ coefficients for carpal tunnel syndrome on the right and left sides were 0.58 and 0.38, respectively. No kappa coefficients could be calculated for the remaining seven specific diagnoses as one of the examiners made no such diagnoses.
4. Discussion
This study tested the concurrent validity of a modified shortened clinical examination protocol for occupational health surveillance, called the HECO protocol, compared to the original protocol developed by Ohlsson et al. (1994). The original protocol has been used for epidemiological research in many previous studies and is used as the reference protocol in this study.
Different to the original protocol the HECO protocol contains a screening part which takes only 10 minutes to complete. The study results showed that the new screening procedure was reliable. None of the examined which were found to be asymptomatic according to the HECO protocol, and therefore screened out, was found to have a diagnosis using the reference protocol, i.e. the original protocol.
4.1 Concurrent validity for having one or more diagnoses
Reasonably good agreement was observed between the two protocols for subjects with symptoms. The validity of the HECO protocol for the neck/shoulders region was higher than for the elbows/hands region. The κ coefficients for the neck/shoulder and the elbow/hand regions were 0.62 and 0.49, respectively, indicating a fair to good agreement between the protocols for both anatomical regions. This is in accordance with other studies (Smith et al. 2010; Walker-Bone et al. 2002). The weaker agreement values for the elbow/hand region could be explained by difficulties to find correct physical signs in the hand and wrist region, also discussed by Walker-Bone et al. (2002). Also, Walker-Bone et al. (2002) reported poorer reliability between two examiners when examining a general population than an orthopaedic outpatient with soft tissue disorders of the upper limb, possibly due to the absence of clear-cut cases in the general population. Thus, as the present examined group were more like the general working population than orthopaedic outpatients, fairly low agreement between examiners could be expected.
These differences are probably not caused by differences in the protocols, but by different judgments of the examiners, and could be reduced by training and calibration.
4.2 Agreement for specific diagnoses
In total, 36 specific diagnoses were possible for the two anatomical regions. In general, the observed agreement between the HECO protocol and the reference protocol was good for all these diagnoses. However, as several of these diagnoses were not found by both examiners, only nine values of κ could be calculated for the neck/shoulder regions, and only four for the elbow/hand regions.
Concerning the neck/shoulders region, good to excellent agreement was found for diagnoses of tension neck syndrome, acromioclavicular syndrome and supraspinatus syndrome. Low to moderate agreement was found for infraspinatus tendonitis, bicipital tendonitis and frozen shoulder. However, we do not believe that supraspinatus tendonitis, for example, is easier than bicipital tendonitis for examiners to agree on; rather we believe that these differences were due to chance. The prevalence of tension neck syndrome was as high as 11%, regardless of which protocol was used. This confirms the importance of including tension neck syndrome in health surveillance protocols when examining work-related musculoskeletal disorders in upper extremities, which has been suggested in earlier studies (Palmer and Smedley 2007; Nordander et al. 2009).
Concerning the elbows/hands region, fair to good agreement was obtained for carpal tunnel syndrome and ulnar nerve entrapment, both on the right side. However, the overused hand syndrome was identified only by the examiner using the reference protocol and not by the one using the HECO protocol, while only the HECO examiner made the diagnosis of pronator teres syndrome. These differences are probably not caused by differences in the protocols, but by different judgments of the examiners, and could be reduced by training and calibration.
4.3 Methodological considerations
The sample was sufficiently large to allow the reliability of screening to be evaluated, and the concurrent validity concerning the prevalence of disorders in two anatomical regions to be determined. Although the study group consisted of 63 employees engaged in types of work known for a high prevalence of musculoskeletal disorders in the neck and upper limbs (Charles, Loomis, and Demissie 2009; Hayes, Cockrell, and Smith 2009), the majority did not have any of the specific diagnoses, making the analysis at this level uncertain. This would also increase the probability of agreement by chance alone. The kappa coefficient is, however, designed to correct for this effect, as greater agreement is required between observers for a given value of κ when the prevalence is much lower (or higher) than 50%.
The inter-rater agreement between two experienced examiners has formerly been evaluated and shown to be generally good, with κ 0.7–0.9 for the different tests performed (Nordander 2004). In the present study, the agreement between the examiners was not perfect on the individual level. However, the prevalence of diagnosis assessed by these methods was of the same magnitude. No systematic differences were seen between the protocols. Sometimes one of the examiners made a diagnosis and not the other examiner, and sometimes vice versa. The symptoms in these subjects were probably not severe. One explanation may be that the first examination may have elicited symptoms, and the second examiner, therefore, had made more diagnoses than the first one. As half of the subjects were examined according to the HECO protocol first and the other half according to the reference protocol first, such an effect should not have confounded the overall result. However, it might as mentioned have influenced the differences between the two examiners when only one of them identified a diagnosis.
A limitation in the study is that the proportion of men is low. Therefore, we are unable to generalise the findings to men. Men may report disorders differently than women and in this case, the deviation is not included in the study. It would also have been desirable to have more occupations included, which together with more men could have generated those diagnoses which were not found in this study.
The examination time for both the HECO and the reference protocol was not exactly measured. However, the employees were scheduled according a 30-minute scheme and the examiners did not differ any time from this schedule. Based on this, it has been possible to estimate the time required.
4.4 Implications
Specific features of systematic health surveys including physical examinations at the workplace have been discussed in an earlier study (Fine et al. 1986) which found that this method was more sensitive and reliable in making diagnoses than standardised questionnaires. In addition, the possibility of detecting WRUEDs at an early stage was highlighted. However, the additional cost of such time-consuming routines was questioned.
Comparing the HECO protocol with the Sluiter protocol (Sluiter, Rest, and Fring-Dresen 2001) also developed for health surveillance evaluating work relatedness of musculoskeletal disorders in neck and upper extremities, the HECO screening consists of only two parts, while the Sluiter protocol consists of separate screening parts for each of the 12 possible diagnoses. Hence, the Sluiter protocol is due to comprehensive screening procedure more difficult to implement as a surveillance instrument for occupational health services.
The HECO protocol can easily be used nearby the work station since no special equipment are required, which means the employees have a minimum of working time loss. In addition, the screening part of HECO takes only 10 minutes, compared with the 30 minutes required for the original protocol. Since the majority of employees are often symptom-free, this will lead to a considerable saving in time when surveying individuals with the HECO protocol at workplaces.
The personal contact between the employee and the occupational health physiotherapist or physician may also be beneficial as it provides the opportunity to give advice on health and working techniques and equipment, before problems arise.
Comparing the results obtained on group level using the HECO protocol with the results obtained from earlier studies using the original protocol, described elsewhere (Nordander et al. 2009; HECO 2014), provides information on whether the prevalence of disorders in an examined work group can be considered reasonable, or is higher than expected. In the latter case, measures can be taken by the employer, e.g. in the work organisation or in ergonomics settings, to reduce the prevalence. Furthermore, performing HECO regularly allows interventions on both the organisational and individual level to be evaluated.
4.5 Conclusions
The HECO protocol with the screening procedure is reliable to use for occupational health surveillance of work-related musculoskeletal disorders in the upper extremities. This gives the OHS a powerful and cost-efficient tool to detect work places with high risk for developing musculoskeletal disorders in the neck and upper extremities, but also employees who are in the early phase of developing disorders.
Acknowledgements
The standard reference protocol was originally published by Professor Kerstina Ohlsson, who also participated in the development of HECO. We would also like to thank Anna Larsson for her valuable help with data handling, and the staff at the Occupational Safety and Health Centre at the County Hospital Ryhov, Jönköping, Sweden for cooperation during the study.
Funding Statement
This study was financed by the Swedish Council for Working Life and Social Research, AFA Insurance, the Medical Faculty of Lund University and the County Councils of Southern Sweden We would also like to thank Futurum – Academy for Health and Care, Jönköping, Sweden for the support by grants.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Boström M., Dellve L. , Thomee S. , Hagberg M. . Risk Factors for Generally Reduced Productivity: A Prospective Cohort Study of Young Adults with Neck or Upper-Extremity Musculoskeletal Symptoms. Scandinavian Journal of Work, Environment & Health . 2008;34(2):120–132. doi: 10.5271/sjweh.1218. [DOI] [PubMed] [Google Scholar]
- Buckle P., Devereux J. . Bilbao: European Agency for Safety and Health at Work; 1999. Work-Related Neck and Upper Limb Musculoskeletal Disorders. [Google Scholar]
- Charles L. E., Loomis D. , Demissie Z. . Occupational Hazards Experienced by Cleaning Workers and Janitors: A Review of the Epidemiologic Literature. Work . 2009;34(1):105–116. doi: 10.3233/WOR-2009-0907. [DOI] [PubMed] [Google Scholar]
- European, Labour, Force & Survey . 2009. Statistics in focus 63/2009. Luxembourg. http://www.ncbi.nlm.nih.gov/pubmed/19923681. [Google Scholar]
- Cote P., van der Velde G. , Cassidy J. D. , Carroll L. J. , Hogg-Johnson S. , Holm L. W. . The Burden and Determinants of Neck Pain in Workers. Spine . 2008;17(S1):60–74. doi: 10.1007/s00586-008-0626-9. doi: [DOI] [PubMed] [Google Scholar]
- The Council of the European Communities . 1989. Directive of the Introduction of Measures to Encourage Improvements in Safety and Health of Workers at Work 89/391/EEC [Google Scholar]
- Fine L. J., Silverstein B. A. , Armstrong T. J. , Anderson C. A. , Sugano D. S. . Detection of Cumulative Trauma Disorders of Upper Extremities in the Workplace. Journal of Occupational Medicine . 1986;28(8):674–678. doi: 10.1097/00043764-198608000-00027. doi: [DOI] [PubMed] [Google Scholar]
- Hagberg M., Vilhemsson R. , Tornqvist E. W. , Toomingas A. . Incidence of Self-Reported Reduced Productivity Owing to Musculoskeletal Symptoms: Association with Workplace and Individual Factors Among Computer Users. Ergonomics . 2007;50(11):1820–1834. doi: 10.1080/00140130701674539. doi: [DOI] [PubMed] [Google Scholar]
- Hagberg M., Violante F. S. , Bonfiglioli R. , Descatha A. , Gold J. , Evanoff B. , Sluiter J. K. . Prevention of Musculoskeletal Disorders in Workers: Classification and Health Surveillance – Statements of the Scientific Committee on Musculoskeletal Disorders of the International Commission on Occupational Health. BMC Musculoskeletal Disorders . 2012;13(1):109. doi: 10.1186/1471-2474-13-109. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes M., Cockrell D. , Smith D. R. . A Systematic Review of Musculoskeletal Disorders Among Dental Professionals. International Journal of Dental Hygiene . 2009;7(3):159–165. doi: 10.1111/j.1601-5037.2009.00395.x. doi: [DOI] [PubMed] [Google Scholar]
- HECO . 2014. Health Surveillance in Adverse Ergonomics Conditions. Information Brochure: MEBA [Medicinsk kontroll i ergonomiskt belastande arbete (In Swedish)]. http://fhvmetodik.se/wp-content/uploads/2014/01/MEBA_folder140116.pdf. [Google Scholar]
- Huisstede BM., Bierma-Zeinstra SM. , Koes BW. , Verhaar JA . Incidence and Prevalence of Upper-Extremity Musculoskeletal Disorders. A Systematic Appraisal of the Literature. BMC Musculoskeletal Disorders . 2006;7(1):7. doi: 10.1186/1471-2474-7-7. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkwood B. R., Jonatan A. C. S. . 2nd ed. . Oxford: Oxford University Press; 2003. Essential Medical Statistics. [Google Scholar]
- Kuorinka I., Jonsson B. , Kilbom A. , Vinterberg H. , Biering-Sorensen F. . Standardised Nordic Questionnaires for the Analysis of Musculoskeletal Symptoms. Applied Ergonomics . 1987;18(3):233–237. doi: 10.1016/0003-6870(87)90010-X. doi: [DOI] [PubMed] [Google Scholar]
- Nordander C. 2004. Work-Related Musculoskeletal Disorders – Exposure Assessment and Gender Aspects. Thesis (PhD). Department of Occupational and Environmental Medicine. Lund, Lund University. [Google Scholar]
- Nordander C., Ohlsson K. , Åkesson I. , Arvidsson I. , Balogh I. , Hansson G. A. , Strömberg U. , Rittner R. , Skerfving S. . Risk of Musculoskeletal Disorders Among Females and Males in Repetitive/Constrained Work. Ergonomics . 2009;52(10):1226–1239. doi: 10.1080/00140130903056071. doi: [DOI] [PubMed] [Google Scholar]
- Nordander C., Ohlsson K. , Balogh I. , Hansson G. A. , Axmon A. , Persson R. , Skerfving S. . Gender Differences in Workers with Identical Repetitive Industrial Tasks: Exposure and Musculoskeletal Disorders. International Archives of Occupational and Environmental Health . 2008;81(8):939–947. doi: 10.1007/s00420-007-0286-9. doi: [DOI] [PubMed] [Google Scholar]
- Ohlsson K., Attewell R. G. , Johnsson B. , Ahlm A. , Skerfving S. . An Assessment of Neck and Upper Extremity Disorders by Questionnaire and Clinical Examination. Ergonomics . 1994;37(5):891–897. doi: 10.1080/00140139408963698. doi: [DOI] [PubMed] [Google Scholar]
- Palmer K. T., Smedley J. . Work Relatedness of Chronic Neck Pain with Physical Findings: A Systematic Review. Scandinavian Journal of Work, Environment & Health . 2007;33(3):165–191. doi: 10.5271/sjweh.1134. doi: [DOI] [PubMed] [Google Scholar]
- Palmer K., Walker-Bone K. , Linaker C. , Reading I. , Kellingray S. , Coggon D. , Cooper C. . The Southampton Examination Schedule for the Diagnosis of Musculoskeletal Disorders of the Upper Limb. Annals of the Rheumatic Diseases . 2000;59(1):5–11. doi: 10.1136/ard.59.1.5. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roquelaure Y., Ha C. , Leclerc A. , Touranchet A. , Sauteron M. , Melchior M. , Imbernon E. , Goldberg M. . Epidemiologic Surveillance of Upper-Extremity Musculoskeletal Disorders in the Working Population. Arthritis Rheum . 2006;55(5):765–778. doi: 10.1002/art.22222. doi: [DOI] [PubMed] [Google Scholar]
- Sluiter J. K., Rest K. M. , Fring-Dresen M. H. . Criteria Document for Evaluating the Work-Relatedness of Upper-Extremity Musculoskeletal Disorders. Scandinavian Journal of Work, Environment & Health . 2001;27(Suppl 1):1–102. doi: 10.5271/sjweh.637. doi: [DOI] [PubMed] [Google Scholar]
- Smith C. K., Bonauto D. K. , Silverstein B. A. , Wilcox D. . Inter-Rater Reliability of Physical Examinations in a Prospective Study of Upper Extremity Musculoskeletal Disorders. Journal of Occupational and Environmental Medicine . 2010;52(10):1014–1018. doi: 10.1097/JOM.0b013e3181f4396b. doi: [DOI] [PubMed] [Google Scholar]
- Swedish Work Environmental Authority Work-Related Disorders . 2012:5. [Google Scholar]
- Walker-Bone K., Byng P. , Linaker C. , Reading I. , Coggon D. , Palmer K. T. , Cooper C. . Reliability of the Southampton Examination Schedule for the Diagnosis of Upper Limb Disorders in the General Population. Annals of the Rheumatic Diseases . 2002;61(12):1103–1106. doi: 10.1136/ard.61.12.1103. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker-Bone K., Palmer K. T. , Reading I. , Coggon D. , Cooper C. . Prevalence and Impact of Musculoskeletal Disorders of the Upper Limb in the General Population. Arthritis & Rheumatology . 2004;51(4):642–651. doi: 10.1002/art.20535. doi: [DOI] [PubMed] [Google Scholar]