Abstract
Purpose of the Study:
Falls are a major problem for the elderly people leading to injury, disability, and even death. An unobtrusive, in-home sensor system that continuously monitors older adults for fall risk and detects falls could revolutionize fall prevention and care.
Design and Methods:
A fall risk and detection system was developed and installed in the apartments of 19 older adults at a senior living facility. The system includes pulse-Doppler radar, a Microsoft Kinect, and 2 web cameras. To collect data for comparison with sensor data and for algorithm development, stunt actors performed falls in participants’ apartments each month for 2 years and participants completed fall risk assessments (FRAs) using clinically valid, standardized instruments. The FRAs were scored by clinicians and recorded by the sensing modalities. Participants’ gait parameters were measured as they walked on a GAITRite mat. These data were used as ground truth, objective data to use in algorithm development and to compare with radar and Kinect generated variables.
Results:
All FRAs are highly correlated (p < .01) with the Kinect gait velocity and Kinect stride length. Radar velocity is correlated (p < .05) to all the FRAs and highly correlated (p < .01) to most. Real-time alerts of actual falls are being sent to clinicians providing faster responses to urgent situations.
Implications:
The in-home FRA and detection system has the potential to help older adults remain independent, maintain functional ability, and live at home longer.
Key words: Falls, Fall risk, Fall detection, Automated algorithms
Older adults want to remain at home for as long as possible (Marek & Rantz, 2000; Rantz, Marek, Aud, et al., 2005). Falls are a major problem for the elderly people leading to injury, disability, and loss of independence. One in three people aged 65 and older falls each year and falls are the leading cause of both fatal and nonfatal injuries (Centers for Disease Control and Prevention, 2014). In 2000, the cost to treat fatal and nonfatal falls was more than $19 billion (Stevens, Corso, Finkelstein, & Miller, 2006). Falls are often a symptom of some other underlying impending health problem or decline in physical function (Woolrych et al., 2014; Zecevic, Salmoni, Speechley, & Vandervoort, 2006) that can be detected by increasing risk of falls and may be amenable to intervention. Researchers have assessed fall risk and provided interventions aimed at reducing falls. In other studies, participants usually perform a multifactorial risk assessment that may be time consuming. Furthermore, these assessments are usually done infrequently for community-dwelling older adults (Perell et al., 2001).
Another approach is the use of a continuous, unobtrusive, automated in-home fall risk assessment (FRA) and detection system that could alert health care providers to increasing fall risk and actual falls. This approach allows for timely interventions that can help older adults maintain functional ability and reduce medical expenses. Researchers at the University of Missouri (MU) Center for Eldercare and Rehabilitation Technology developed and tested a FRA and detection sensor system in the homes of elderly participants with promising results. Results of validation analyses and clinical utility of the system are presented.
In our study, an automated in-home FRA and detection sensor system was installed in apartments of 19 older adults at TigerPlace, a senior living community. The goal was to capture as many clinically valid fall risk measures as possible, including walking speed, and reliably detect actual falls. Prior research indicated that a key variable of FRA is gait velocity (speed). Walking speed has been shown to be a risk factor for disability, cognitive impairment, institutionalization, falls, and mortality (Abellan van Kan et al., 2009). Walking speed is such a reliable and sensitive measure that it was recently recommended to be the sixth vital sign (Fritz & Lusardi, 2009).
To validate the FRA and detection sensor system, “ground truth” data were collected. Ground truth data are objective measures used in algorithm development and for comparison with variables derived from sensor data. In this study, clinically valid, standard FRAs, variables from the GaitRITE mat (an electronic walkway that measures temporal and spatial gait parameters), and real falls performed by stunt actors in participants’ apartments were used as ground truth. The stunt actor falls in the actual living environment of elders were vital in the development of a system that reliably captures actual falls and alerts clinical staff that a person has fallen.
TigerPlace is an independent senior living community operated by Americare Systems, Inc., Sikeston, MO, and the Sinclair School of Nursing. Home care aides are on site 24 hours per day, 7 days per week to assist with on-going daily care needs and urgent situations. In addition, an registered nurse care coordinator staffs the wellness center 5 days per week and is on call 24/7 to triage health conditions. A licensed master’s prepared social worker is available to provide psychosocial care and support to residents. Residents may pay privately for additional home care services including medication management or personal care services such as bathing or dressing (Rantz, Phillips, Aud, et al., 2011).
Design and Methods
Sample
Nineteen participants (9 men, 10 women) agreed to participate in this research. The 19 participants occupied 16 apartments at TigerPlace. The average age of the research participants at the time of the sensor system installation was 87 (age range 67–98). There were 3 couples and the rest of the participants were single. All participants were Caucasian; all signed MU IRB informed consent and agreed to participate in the research. Electronic data from the sensor systems were collected for 2 years, 24 hours per day, 7 days per week. For the radar and Kinect, the average length of install was 478 days or 1.3 years. The range is 62 days (0.17 years) to 1,057 days (2.9 years); 14 people had radar installed for 1 year or more.
In-home FRA and Detection Sensor System
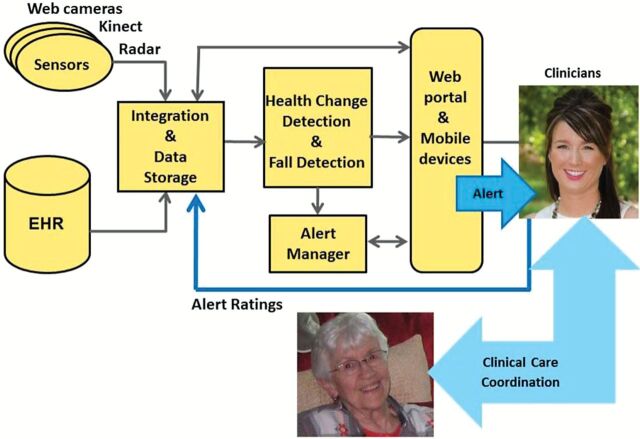
The sensor system consisted of pulse-Doppler radar, a Microsoft Kinect, and two web cameras as a part of a more complete sensor network for in-home use (see Figure 1). A total of 10 systems were used for 2 years or more in apartments at TigerPlace. The radar and the Kinect systems are set up to detect motion within their fields of view. For fall detection specifically, the radar system produces radar signals (electronic wave forms) and employs signal processing techniques that detect sudden changes in motion and then filter out false alarms like sudden door closing or housekeeping activities. The Kinect system produces images in three-dimensional space, uses machine learning approaches to detect falls, and has fewer errors because it can differentiate sudden motion between different directions (e.g., lateral motion vs vertical motion). However, it faces challenges due to occlusions in the form of furniture that may obstruct the sensor’s field of view so that it may not be able to “see” the falls. In contrast, the radar system has the advantage of “seeing” through furniture. Web cameras used as a two-camera system are typical cameras producing images such as traditional video as well as anonymized images in three-dimensional space.
Figure 1.
Sensor network.
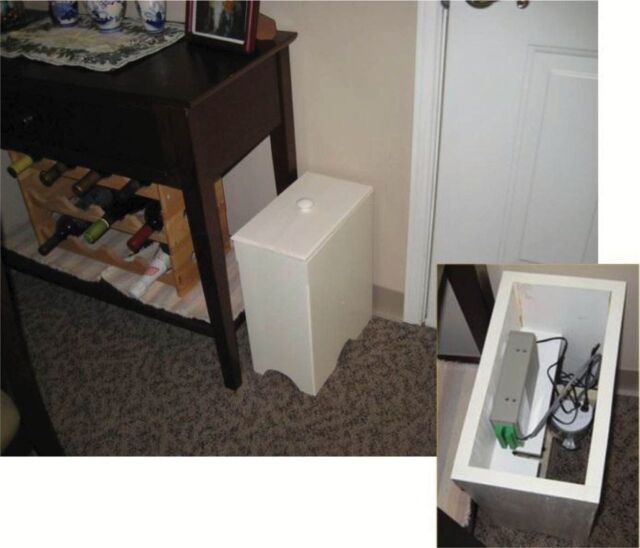
The radar was deployed in a decorative wooden box located next to the front door (see Figure 2). The Kinect was installed on a shelf near the ceiling above the doorway leading to the interior hallway of the building (see Figure 3). Computers for collecting the sensor data were located in a cabinet over the refrigerator, a convenient location for installing a power source and network port because kitchens are located near the front door. To protect the privacy of participants, only the nonidentifiable, three-dimensional, ghost-like depth image from the Kinect is recorded. The depth image is an image in which each pixel is associated with a distance from the camera (Rantz, Skubic, Abbott, et al., 2013; Stone & Skubic, 2011a, 2013a). The web cameras were installed on orthogonal walls in the living room; our research team has used these cameras in other studies to collect nonidentifiable silhouette images for analysis of gait parameters (Wang, Skubic, Abbott, & Keller, 2010). For purposes of this study, they were only used during times each month when research staff performed FRAs with each participant in their apartment. At that time, actual video images were collected for ground truth of the assessments from two points of view, so scores of the assessments could be validated for reliability. At no time was streaming video collected.
Figure 2.
Radar installed in apartment.
Figure 3.

Kinect installed in apartment.
The initial radar and Kinect systems were configured and validated in the Eldertech engineering laboratory at the MU before being installed in the apartments at TigerPlace (Rantz, Skubic, Abbott, et al., 2013). Fifteen adults (8 women, 7 men; ranging in age from 23 to 67, mean age 56.5) from the community completed the FRA protocol while data were collected from the radar and Kinect systems simultaneously as participants walked on a GAITRite mat at two different speeds (normal and slow). The GAITRite (http://www.gaitrite.com) is an electronic walkway that measures temporal and spatial gait parameters, such as velocity, step length, and stride length. The GAITRite also produces the functional ambulation profile (FAP) score (range 0–100) that incorporates specific time and distance parameters to assess overall performance of locomotion (Nelson, 1974). The FAP score has been found to differentiate fallers and nonfallers (p < .05; Nelson et al., 1999).
Initial algorithms were developed to extract gait parameters from the Kinect and Radar data using data collected in the engineering laboratory. MU engineering faculty and students constructed algorithms to extract gait velocity, stride length, and stride time from the Kinect data (Stone & Skubic, 2011a, 2013a). Algorithms to extract gait parameters of velocity and stride time from the radar data were created by collaborators at the General Electric Global Research Laboratories (Cuddihy et al., 2012; Phillips et al., 2012; Yardibi et al., 2011).
Initial fall detection algorithms were developed using falls performed in the laboratory by stunt actors (Liu, Popescu, Ho, Skubic, & Rantz, 2012; Liu et al., 2011; Stone & Skubic, 2015). Two stunt actors performed two protocols, the fall protocol (21 falls from four positions) and the false positive protocol (14 different motions) 4 times to provide adequate initial data. These protocols were developed by clinicians on the research team to be representative of the range of falls by elders, regardless of the underlying cause of the fall, such as slipping, tripping, rolling from a couch or bed, falling from a chair, or from standing positions from episodes of loss of consciousness (Rantz, Aud, et al., 2008).
In-Home Data Collection
FRAs With Instruments Commonly Used in Clinical Practice
Ground truth, or the reference labels of the training and validation data for machine learning techniques, was necessary to develop and validate the automated in-home FRA. This process required having acceptable “standards” for comparison and development of automated algorithms for the technology to apply to the on-going data collected from in-home sensors.
To provide ground truth data for fall risk, each participant performed a FRA in their apartment each month for 2 years. The FRA consisted of 6 standardized clinical assessment instruments commonly used in geriatric FRA, all with known, acceptable validity and reliability: Timed Up and Go (TUG; Podsiadlo & Richardson, 1991; Shumway-Cook, Brauer, & Woollacott, 2000); Single Leg Stance (SLS; Vellas et al., 1997); Berg Balance Scale (BBS-SF; Berg, Wood-Dauphinee, Williams, & Maki, 1992); Short Physical Performance Battery (SPPB; Guralnik et al., 1994), Functional Reach (FR; Newton, 2001); and Habitual Gait Speed (HGS; Bohannon, 1997; Fransen, Crosbie, & Edmonds, 1997). The FRAs were facilitated and scored by a clinician and simultaneously recorded by the sensing modalities. The first FRA was completed on June 27, 2011, and the last assessment was concluded on July 31, 2013. A rolling enrollment maintained continuous data collection, resulting in the number of FRAs varying by participant as people were discharged from the study and others were admitted. Rolling enrollment also resulted in varying numbers of apartments in which participants lived, amount of sensor data, and FRAs available for the analyses. Two participants (one couple) withdrew from the study because they did not like the appearance of the radar box in their apartment; others were discharged due to their leaving TigerPlace. A total of 239 FRAs were collected; the number of FRAs ranged from 1 to 25 (mean 12.6 assessments per participant).
Additional ground truth for FRA was collected using the GAITRite. Each participant walked on the GAITRite mat at least every 6 months, some more frequently. Velocity, step length, and stride length and the FAP score were collected for each participant.
Fall Detection
To provide ground truth for falls, actual falls need to be collected in the in-home environment, as well as nonfall motions. Because naturally occurring falls are not frequent enough in the typical homes of older adults to capture adequate training data for algorithm refinement, trained stunt actors performed falls in each participant’s apartment with the sensing modalities each month during the 2-year data collection. Trained stunt actors were used to generate adequate data and to protect the older adults. The stunt actors were trained based on actual falls older adults commonly experience including loss of consciousness, slip and trip, and loss of balance. Each fall was done on protective padding to ensure actor safety. The stunt actors performed a minimum of four different falls from the fall protocol each month in each apartment. A total of 174 sequences of fall protocols (a minimum of 4 falls per sequence for a total of 882 falls) were collected in 14 apartments; they also performed the nonfall (false positive) protocol that included actions like stooping down to plug in an electrical appliance and picking an object up off the floor from a seated position, in each apartment monthly to provide false positive data for refinement of fall detection algorithms.
Data Analysis
Fall Detection
Data analysis for refinement of fall detection algorithms was iterative, beginning with data collected in the engineering laboratory and progressive as the falls and false positive data were collected by Kinect and radar sensors in the apartments in TigerPlace. Engineering researchers tested a variety of feature selection, signal processing and classification methods in an effort to develop algorithms with high reliability of fall detection and a low false alarm rate (Liu et al., 2011). Positioning of the radar was tested both in the laboratory and in TigerPlace, with the deployment of radar sensors placed above some bathroom and living room ceilings in the attic; ceiling positioning was found to be more reliable than floor or wall mounted for fall detection (Liu et al., 2012). Fusion of data from both radar and motion sensors has promise for improving false alarm rates of radar alone (Liu, Popescu, Skubic, Rantz, & Cuddihy, in press; Liu, Popescu, Skubic, & Rantz, 2014). Additional development and testing of radar to improve reliability and further reduce false alarm rates is needed.
For Kinect, the fall detection algorithms were informed by the team’s research using other vision-based, but privacy protecting image processing for passive activity monitoring in elder housing (Stone & Skubic, 2011b). A two-stage fall detection algorithm was ultimately developed in which the first stage of the detection system characterizes a person’s vertical state in individual depth image frames and then segments “on-ground events” from the vertical state obtained by tracking the person over time. The second stage uses an ensemble of decision trees to compute a confidence that a fall preceded an on-ground event (Stone & Skubic, 2015). With the progress of the iterative improvements for the Kinect algorithm, it was possible to implement the system for real-time fall detection with e-mail alerts to staff of TigerPlace and the research team near the end of data collection, in August 2013. Data collection with Kinect was extended as staff did not want the system removed. See Figure 4 for images of an actual fall of an elder resident.
Figure 4.
Three sequential depth images from the Microsoft Kinect showing an actual elderly resident fall in an apartment. The figure can be seen in contrasting color in the center of the images. The resident uses a walker.
In-Home FRA
To validate the performance of the in-home FRA sensor system, ground truth data (FRAs and GAITRite variables) are compared with radar and Kinect generated gait variables. For all of the analyses, a weighted correlation coefficient (Bland & Altman, 1994) was used to accommodate for the fact that some participants contribute multiple observations to the data. There is no correction for multiple testing; therefore, p values of .01 or less are regarded as significant.
All participants had multiple monthly FRAs and most had several GAITRite walks (approximately 3- to 6-month intervals) but the two evaluations did not occur on the same day. Thus, for each participant, their GAITRite dates were paired with the FRA that was closest in time. The correlations in Table 1 are based on 17 participants and 32 paired observations. The median number of days between FRA and GAITRite was 7 with a range of 6–44 days. The number of participants is reported as 17 because two couples were participants among the 19 total participants. In the case of couples, the FRA and GAITRite data were averaged to the apartment level and then correlated with the radar data because radar is unable to distinguish between two individuals residing in the same apartment. However, averaging for couples is not needed for Kinect data, as Kinect is able to distinguish between couples using differences in height or distinguishing features of gait.
Table 1.
Correlations Between GAITRite Velocity and Functional Ambulation Profile (FAP) and Fall Risk Assessments (N = 17)
| Pearson’s weighted correlation (p value) | |||||||
|---|---|---|---|---|---|---|---|
| GAITRite | Habitual Gait Speed | Functional Reach | Berg Balance Scale | Timed Up and Go | Short Physical Performance Battery | Single Leg Stance (eyes open) | Single Leg Stance (eyes closed) |
| Velocity | −.79 (<.001)** | .44 (.078) | .61 (.009)** | −.67 (.004)** | .79 (<.001)** | .34 (.180) | .26 (.312) |
| FAP | −.41 (.102) | .40 (.108) | .46 (.062) | −.32 (.206) | .55 (.022)* | .44 (.080) | .44 (.077) |
Note: *p < .05. **p < .01.
Results
Four Key Comparisons With Ground Truth
First, the FRA measures used in the monthly data collection were compared with GAITRite velocity and FAP. This is an important validation step to determine the validity of the FRA instruments selected in the study. The accuracy of GAITRite is used in this comparison as the “gold standard” ground truth. GAITRite velocity and FAP correlations were estimated with the FRA measures as shown in Table 1. All of the correlations are in the expected direction. The GAITRite velocity correlates significantly (p < .01) with the HGS, BBS-SF, TUG, and SPPB. The FAP was highly correlated with the SPPB.
Second, FRA measures were compared with gait variables derived from the Kinect and radar data. In this comparison, the FRA measures are used as the “gold standard” ground truth with the data from the Kinect and radar technologies. The results are displayed in Table 2. For correlations of Kinect and FRA variables, it was possible to match each FRA date to the same day of Kinect data. The Kinect variable correlations are based on 203 paired observations from 18 individuals. As previously explained, the radar system does not distinguish between the individual residents in dual occupant apartments. Thus, to correlate the radar variables with FRA variables, the FRA variables for a given date and apartment are the average of the two occupants. The FRA and Radar data are then merged by apartment and date. The correlations in Table 2 for the radar variables are derived from 138 paired observations in 14 apartments.
Table 2.
Correlations Between Fall Risk Assessments (FRAs) and Kinect and Radar Variables
| Pearson’s weighted correlation (p value) | |||||
|---|---|---|---|---|---|
| FRAs | Kinect stride time | Kinect stride length | Kinect velocity | Radar stride time | Radar velocity |
| N | 18 | 18 | 18 | 15 | 15 |
| Habitual Gait Speed | .43 (.076) | −.76 (<.001)** | −.70 (.001)** | .14 (.627) | −.54 (.039)* |
| Functional Reach | −.34 (.170) | .77 (<.001)** | .65 (.003)** | −.13 (.652) | .67 (.006)** |
| Berg Balance Scale | −.56 (.017)* | .76 (<.001)** | .78 (<.001)** | −.01 (.982) | .62 (.015)* |
| Timed Up and Go | .55 (.017)* | −.78 (<.001)** | −.78 <(.001)** | .22 (.440) | −.66 (.008)** |
| Short Physical Performance Battery | −.64 (.004)** | .78 (<.001)** | .83 (<.0001)** | −.08 (.771) | .70 (.004)** |
| Single Leg Stance (eyes open) | −.49 (.040)* | .59 (.011)* | .65 (.004)** | −.13 (.638) | .63 (.013)* |
| Single Leg Stance (eyes closed) | −.46 (.055) | .64 (.004)** | .65 (.003)** | −.16 (.578) | .65 (.008)** |
Note: *p < .05. **p < .01.
Velocity calculated from the Kinect data was significantly (p < .01) correlated with all of the FRA measures. Velocity as measured by the radar was significantly correlated with FR, TUG, SPPB, and SLS eyes closed (p < .01). Radar velocity was also correlated (all p values < .04 but not reaching <.01) with the HGS, BBS-SF, and SLS eyes open. Stride length as derived from the Kinect was also significantly correlated with all of the FRA measures (p < .01). Stride time as calculated by the Kinect produced only one significant result, SPPB (p = .004), when compared with the FRA measures. Radar stride time did not correlate with any of the FRA measures.
Third, GAITRite ground truth measure of velocity and FAP was compared with the gait variables derived from the Kinect and radar data. A total of 17 participants had both GAITRite and Kinect data but 2 were beyond the limit of a month interval. The Kinect correlations in Table 3 are from 21 observations on 15 unique individuals in 13 apartments meeting this requirement. For the radar data, the GAITRite variables were averaged to the apartment level for dual occupancy cases and then merged with the radar data by apartment and data. There were nine observations from nine apartments for which GAITRite and radar dates were able to be matched. GAITRite velocity was significantly correlated (p < .01) with stride length derived from the Kinect data. GAITRite velocity was also correlated with Kinect velocity (p = .029 but not reaching <.01). Neither the radar stride time nor velocity variables correlated with the GAITRite measures.
Table 3.
Correlation Between GAITRite Velocity and Functional Ambulation Profile (FAP) and Kinect and Radar Variables
| Pearson’s weighted correlation (p value) | |||||
|---|---|---|---|---|---|
| GAITRite | Kinect stride time | Kinect stride length | Kinect velocity | Radar stride time | Radar velocity |
| N | 15 (individuals) | 15 (individuals) | 15 (individuals) | 9 (apartments) | 9 (apartments) |
| Velocity | −.15 (.589) | .67 (.006)** | .56 (.029)* | −.507 (.164) | .235 (.542) |
| FAP | −.09 (.755) | .46 (.083) | .40 (.142) | −.232 (.548) | .297 (.438) |
Note: *p < .05. **p < .01.
Fourth, as a final step, the Kinect gait variables were compared with the radar gait variables. To estimate the correlations between the Kinect and radar variables, Kinect variables are the average for the two occupants in dual occupant apartments, as radar must be averaged because it cannot distinguish between occupants. After averaging the Kinect data, it is merged with the radar data by apartment and date. The correlations in Table 4 are based on 3,942 observations from 15 apartments. Radar velocity was significantly correlated in the expected direction with Kinect stride time and velocity (p < .01). Radar velocity was also correlated with the Kinect stride length (p = .017 but not reaching <.01). Radar stride time performed poorly and did not correlate with any of the Kinect variables. In fact, all of the radar stride time correlations are in the opposite direction than expected.
Table 4.
Correlation Between Radar and Kinect Variables (N = 15 Participants)
| Pearson’s weighted correlation (p value) | |||
|---|---|---|---|
| Radar | Kinect stride time | Kinect stride length | Kinect velocity |
| Stride time | −.28 (.321) | .26 (.347) | .29 (.296) |
| Velocity | −.67 (.006)** | .61 (.017)* | .71 (.003)** |
Note: *p < .05. **p < .01.
Fall Detection Using Kinect and Radar
Radar false alarm rates for fall detection when the radar is located near the floor were widely variable from apartment to apartment, ranging from one every 3 days to four per hour, clearly unacceptable for real-time fall detection in a living environment (Liu et al., in press). Better performance was achieved with ceiling radar installed in the attic above the apartment ceiling and using a different algorithm, with 100% detection and less than two false alarms per day when the resident is alone in the apartment (Su, Ho, Rantz, & Skubic, 2015). The ceiling location appears promising. However, the current approach of placement of the sensor in the attic area limits the practicality of continuous usage in living environments. Additional research and development is needed for wide-scale application of the radar sensor for fall detection.
With iterative improvements, the Kinect algorithms achieved high reliability: 98% detection with one false alarm per month (Stone & Skubic, 2015). Real-time fall detection with automated alerts e-mailed to staff of TigerPlace and members of the research team was so successful with staff and residents that the system has been implemented as an important feature in the integrated sensor system for early detection of health changes (Rantz, Skubic, Miller, et al., 2013).
Continuous In-Home Assessment of Fall Risk
Automated algorithms track three features of fall risk continuously: gait velocity, stride length, and stride time. Using multiple features and models, the algorithm developed can correctly differentiate the primary occupant or in the case of couples, it can differentiate between each person (Stone & Skubic, 2013a, 2013b). Trends in the gait parameters are computed with a sliding window over time so that changes in the gait and fall risk are graphed over time for clinician interpretation and potential interventions for improvement. A web-based interface displays this gait information for clinicians, caregivers, and residents to visualize and interpret readily. Automated alerts of changes in gait and fall risk are sent to clinicians and caregivers and may be sent to the older person, according to their preference.
Discussion
An in-home FRA and detection sensor system with radar and Kinect sensors was developed and deployed for 2 years of data collection in the private apartments of 19 older adults. Extensive monthly data collection of well-known FRA measures administered by clinical research staff provided the “ground truth” for comparison of the accuracy of the FRA sensor system developed in the study. FRA data were systematically evaluated to assure the sensor system would be a robust measure of fall risk, making risk assessment an everyday part of one’s life, rather than an infrequent event when seeking health care services for some health concern. All of the correlations with the “gold standard” ground truth of GAITRite are in the expected direction with the seven FRAs collected in this study; those involving gait (HGS, TUG, and SPPB) were highly correlated (p < .01) as was the BBS-SF, commonly used in clinical evaluation of balance.
For radar, velocity is highly correlated in the expected direction with four of the seven FRAs (FR, TUG, SPPB, and SLS eyes closed); however, radar stride time is not correlated with any of the FRAs. For Kinect, both velocity and stride length are both highly correlated in the expected direction with all seven FRAs and stride time is with the SPPB.
The less robust results for radar are a likely reflection of the algorithmic challenges with the radar signals for reliable automated FRA. The researchers made progress with improving the accuracy of walking speed estimation and making methodological adjustments to the estimate for correcting the effect of the wide variety of walking angles that occur in the living environment (Rui, Chen, Ho, Rantz, & Skubic, 2014). It is possible to improve performance by putting environmental constraints in place that would “force” routine daily walking toward or away from the radar sensor, the most precise way to obtain consistently comparable signals. This routine would be counterproductive to the goals of developing sensors that can be unobtrusive to the living patterns of the people using them. However, existing constraints such as hallways could be used if already present. Additionally, we were not successful at identifying other features in the signals that could be used to distinguish between multiple people living in the same apartment. Identifying such features could be the focus of future research. Finally, radar cannot capture spatial parameters and therefore limits the number of fall risk measures it can assess.
The radar has shown some promise in detecting actual falls (Su et al., 2015). The radar was installed in the ceiling above the bathroom in several apartments, where privacy is the utmost concern and moisture may prohibit performance of other sensor options. However, the radar fall detection system has never been implemented real time with alerts sent to clinicians in TigerPlace because of a high false alarm rate. Additional work is needed on this system. We think the radar has good potential with further research and development that will require small unobtrusive packaging of the device so it can be installed on the ceiling, not in the attic. Other issues to be resolved include accessing power in an unobtrusive way in that location and more extensive data collection in a variety of settings. Radar is a particularly appealing solution for private areas such as bedroom or bathroom, where images, regardless of their anonymity, may be unacceptable to those living with the sensors.
Kinect automated measurement of velocity and stride length were both highly correlated with all FRAs and stride time was correlated with most FRAs in this 2-year data collection period. Having continuous measurement and automated analysis of gait has not been previously available, so we now have access to new, more finely grained information that could be used to predict risk of falls and overall function. In additional analyses, a new metric of average in-home gait speed is proposed as a more accurate and precise way to continuously monitor for changes in overall mobility and risk of falls (Stone, Skubic, Rantz, Abbott, & Miller, 2015). Traditional assessment of increasing fall risk or impairments in mobility are infrequent, at best. In-home automated assessment of fall risk could provide information for proactive interventions that are keys to maintaining strength and independence through the end of life, a common goal of many older adults and their families.
Based on the positive results from this study, real-time in-home automated fall detection and FRA using Kinect generated gait measures were implemented in August 2013, in TigerPlace. Real-time fall alerts are sent to the TigerPlace nursing care coordinator, social worker, nursing assistant staff, and the research staff. False alarms generated by pets jumping from furniture or objects dropped on the floor were analyzed and incorporated in the fall detection training to reduce false alarms from these challenging events (Stone & Skubic, 2015). The current false alarm rate of one per month is an acceptable rate for clinicians. Staff and researchers receive an e-mail alert of the fall with a link to a short video of the depth images for a few seconds before and after the event that triggered the alarm. They can easily view the anonymous images and determine if the alert is from a fall or a false alarm. This process avoids the unnecessary interruptions of people’s lives when they have not fallen. Similarly, Kinect is being used to automatically track gait parameters so alerts of increasing fall risk can alert staff to subtle changes. A web-based interface displays gait information for clinicians, caregivers, and residents. A limitation of Kinect is that depth images can be reliably processed for a room about 20 feet in depth, so positioning is important to get a nearly complete view of the room. Large spaces will require careful placement of multiple Kinects when attempting to do automated fall detection in a larger environment. The ghost-like depth images protect privacy and are acceptable to residents; however, at TigerPlace, we have limited the location of Kinect to the general living area of each apartment where most falls occur and where the best paths for gait data for automated FRA can be collected in that particular setting.
Expansion into 13 assisted living sites is currently under way in a larger study using health alerts (NINR 5R01NR014255, M. J. Rantz, PI). Health alerts are generated from a combination of environmentally embedded sensors that have been successfully pilot tested for early illness detection in TigerPlace (Rantz, Skubic, Koopman, et al., 2012). The sensor networks include real-time in-home automated fall detection and FRA using Kinect. Commercialization of the sensor network is also in progress and systems are anticipated to be affordable for deployment in senior housing, assisted living as well as private homes.
Limitations of this study include the relatively small sample size of only 19 participants, the single study site, and the limited collection of the GAITRite ground truth data. A larger sample of users in diverse settings is needed to validate the results. More frequent GAITRite assessments would have provided more data for comparisons. Future efforts will concentrate on the use and refinement of algorithms using Kinect for in-home, continuous FRA and real-time fall detection in a variety of settings.
Conclusion
A real-time in-home automated fall detection and FRA sensor system was successfully developed following 2 years of continuous data collection for refinement and validation of the system in the private apartments of 19 older adults. Today, the system is deployed and operating real time in more apartments at TigerPlace and in several other locations in senior housing in Missouri. Automated algorithms developed and validated during the study continuously monitor for increasing risk of falls as well as reliably detect and alert staff or others when a fall occurs. Some older adults are benefiting by living with the automated sensor system. With further deployment and refinement, the system has the potential to help numerous older adults remain independent, maintain functional ability, and live at home longer; exactly what they tell us they want.
Funding
This research was funded by grant number R01HS018477 from the Agency for Healthcare Quality and Research. The content is solely the responsibility of the authors and does not necessarily reflect the views of the Agency for Healthcare Quality and Research and partially supported by grant number CNS-0931607 from the National Science Foundation.
Acknowledgments
Authors acknowledge contributions of graduate students, Liang Liu, Liyang Rui, Bo-Yu Su, Shanjie Chen, Tanvi Banerjee, other members of the Eldertech Research Team, and Paul Cuddihy with General Electric Global Research, Niskayuna, NY.
References
- Abellan van Kan G., Rolland Y., Andrieu S., Bauer J., Beauchet O., Bonnefoy M., Vellas B. (2009). Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. The Journal of Nutrition, Health & Aging, 13, 881–889. doi:10.1007/s12603-009-0246-z [DOI] [PubMed] [Google Scholar]
- Berg K. O., Wood-Dauphinee S. L., Williams J. I., Maki B. (1992). Measuring balance in the elderly: Validation of an instrument. Canadian Journal of Public Health, 83(Suppl. 2), S7–S11. [PubMed] [Google Scholar]
- Bland J. M., Altman D. G. (1994). Correlation, regression and repeated data. British Medical Journal, 308, 398. doi:10.1136/bmj.308.6933.896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohannon R. W. (1997). Comfortable and maximum walking speed of adults aged 20-79 years: Reference values and determinants. Age and Ageing, 26, 15–19. doi:10.1093/ageing/26.1.15 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2014). Falls among older adults: An overview. Retrieved from http://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html
- Cuddihy P. E., Yardibi T., Legenzoff Z. J., Liu L., Phillips C. E., Abbott C., Rantz M. J. (2012). Radar walking speed measurements of seniors in their apartments: Technology for fall prevention. In Proceedings, 34th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Diego CA, August 28–September 1, 2012 (pp. 260–264). Piscataway, NJ: IEEE Press. doi:10.1109/EMBC.2012.6345919 [DOI] [PubMed] [Google Scholar]
- Guralnik J. M., Simonsick E. M., Ferrucci L., Glynn R. J., Berkman L. F., Blazer D. G., Wallace R. B. (1994). A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology, 49, M85–M94. doi:10.1093/geronj/49.2.M85 [DOI] [PubMed] [Google Scholar]
- Fransen M., Crosbie J., Edmonds J. (1997). Reliability of gait measurements in people with osteoarthritis of the knee. Physical Therapy, 77, 944–953. [DOI] [PubMed] [Google Scholar]
- Fritz S., Lusardi M. (2009). White paper: “Walking speed: The sixth vital sign”. Journal of Geriatric Physical Therapy, 32, 2–5. doi:10.1519/00139143-200932020-00002 [PubMed] [Google Scholar]
- Liu L., Popescu M., Ho K. C., Skubic M., Rantz M. (2012). Doppler radar sensor positioning in a fall detection system. In Proceedings, 34th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Diego CA, August 28–September 1, 2012 (pp. 256–259). Piscataway, NJ: IEEE Press. [DOI] [PubMed] [Google Scholar]
- Liu L., Popescu M., Skubic M., Rantz M. (2014). An automatic fall detection framework using data fusion of Doppler radar and motion sensor network. In Proceedings, 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC’14), Chicago, IL, August 26–August 30, 2014. Piscataway, NJ: IEEE Press. doi:10.1109/EMBC.2012.6345918 [DOI] [PubMed] [Google Scholar]
- Liu L., Popescu M., Skubic M., Rantz M., Cuddihy P.(in press). An automatic in-room fall detection system using Doppler radar signatures. Journal of Ambient Intelligence and Smart Environments. doi:10.1109/EMBC.2014.6944981 [Google Scholar]
- Liu L., Popescu M., Skubic M., Rantz M., Yardibi T., Cuddihy P. (2011). Automatic fall detection based on Doppler radar motion. In Proceedings, 5th International Conference on Pervasive Computing Technologies for Healthcare, Dublin, Ireland, May 23–26, 2011 (pp. 222–225). IEEE Press, Piscataway, NJ. [Google Scholar]
- Marek K. D., Rantz M. J. (2000). Aging in place: A new model for long-term care. Nursing Administration Quarterly, 24, 1–11. doi:10.1097/00006216-200004000-00003 [DOI] [PubMed] [Google Scholar]
- Nelson A. J. (1974). Functional ambulation profile. Physical Therapy, 54, 1059–1065. [DOI] [PubMed] [Google Scholar]
- Nelson A. J., Certo L. J., Lembo L. S., Lopez D. A., Manfredonia E. F., Vanichpong S. K., Zwick D. (1999). The functional ambulation performance of elderly fallers and non-fallers walking at their preferred velocity. NeuroRehabilitation, 13, 141–146. [Google Scholar]
- Newton R. A. (2001). Validity of the multi-directional reach test: A practical measure for limits of stability in older adults. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 56, M248–M252. doi:10.1093/gerona/56.4.M248 [DOI] [PubMed] [Google Scholar]
- Perell K. L., Nelson A., Goldman R. L., Luther S. L., Prieto-Lewis N., Rubenstein L. Z. (2001). Fall risk assessment measures: An analytic review. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 56, M761–M766. doi:10.1093/gerona/56.12.M761 [DOI] [PubMed] [Google Scholar]
- Phillips C. E., III, Keller J., Popescu M., Skubic M., Rantz M. J., Cuddihy P. E., Yardibi T. (2012). Radar walk detection in the apartments of elderly to assist with assessing fall risk. In Proceedings, 34th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC’12), San Diego, CA, August 28–September 1, 2012 (pp. 5863–5866). Piscataway, NJ: IEEE Press. [DOI] [PubMed] [Google Scholar]
- Podsiadlo D., Richardson S. (1991). The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. Journal of the American Geriatrics Society, 39, 142–148. doi:10.1109/EMBC.2012.6347327 [DOI] [PubMed] [Google Scholar]
- Rantz M. J., Aud M. A., Alexander G., Wakefield B. J., Skubic M., Luke R. H., Keller J. M. (2008). Falls, technology, and stunt actors: New approaches to fall detection and fall risk assessment. Journal of Nursing Care Quality, 23, 195–201. doi:10.1097/01.NCQ.0000324581.59557.42 [DOI] [PubMed] [Google Scholar]
- Rantz M. J., Marek K. D., Aud M. A., Johnson R. A., Otto D., Porter R. (2005). TigerPlace: A new future for older adults. Journal of Nursing Care Quality, 20, 1–4. doi:10.1097/00001786-200501000-00001 [DOI] [PubMed] [Google Scholar]
- Rantz M. J., Phillips L., Aud M., Popejoy L., Marek K. D., Hicks L. L., Miller S. J. (2011). Evaluation of aging in place model with home care services and registered nurse care coordination in senior housing. Nursing Outlook, 59, 37–46. doi:10.1016/j.outlook.2010.08.004 [DOI] [PubMed] [Google Scholar]
- Rantz M. J., Skubic M., Abbott C., Galambos C., Pak Y., Ho D. K., Miller S. J. (2013). In-home fall risk assessment and detection sensor system. Journal of Gerontological Nursing, 39, 18–22. doi:10.3928/00989134-20130503-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rantz M. J., Skubic M., Koopman R. J., Alexander G. L., Phillips L., Musterman K., Miller S. J. (2012). Automated technology to speed recognition of signs of illness in older adults. Journal of Gerontological Nursing, 38, 18–23. doi:10.3928/00989134-20120307-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rantz M. J., Skubic M., Miller S. J., Galambos C., Alexander G., Keller J., Popescu M. (2013). Sensor technology to support Aging in Place. Journal of the American Medical Directors Association, 14, 386–391. doi:10.1016/j.jamda.2013.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rui L., Chen S., Ho K. C., Rantz M., Skubic M. (2014). Estimation of human walking speed by Doppler radar for elderly care. Manuscript submitted for publication.
- Shumway-Cook A., Brauer S., Woollacott M. (2000). Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Physical Therapy, 80, 896–903. [PubMed] [Google Scholar]
- Stevens J. A., Corso P. S., Finkelstein E. A., Miller T. R. (2006). The costs of fatal and non-fatal falls among older adults. Injury Prevention, 12, 290–295. doi:10.1136/ip.2005.011015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone E., Skubic M. (2011a). Evaluation of an inexpensive depth camera for in-home gait assessment. Journal of Ambient Intelligence and Smart Environments, 3:349–361. doi:10.3233/AIS-2011-0124 [Google Scholar]
- Stone E. E., Skubic M. (2011b). Silhouette classification using pixel and voxel features for improved elder monitoring in dynamic environments. In Proceedings, 2011 IEEE International Conference on Pervasive Computing and Communications Workshops (PERCOM Workshops), Seattle, WA, March 21–25, 2011 (pp. 655–661). Piscataway, NJ: IEEE Press. [Google Scholar]
- Stone E. E., Skubic M. (2013a). Unobtrusive, continuous, in-home gait measurement using the Microsoft Kinect. IEEE Transactions on Biomedical Engineering, 60, 2925–2932. doi:10.1109/TBME.2013.2266341 [DOI] [PubMed] [Google Scholar]
- Stone E., Skubic M. (2013b). Mapping Kinect-based in-home gait speed to TUG time: A methodology to facilitate clinical interpretation. In Proceedings of the 2013 7th International Conference on Pervasive Computing Technologies for Healthcare and Workshops: PervasiveHealth 2013, Venice, Italy, May 5–8, 2013 (pp. 57–64). doi:10.4108/icst.pervasivehealth.2013.252097 [Google Scholar]
- Stone E. E., Skubic M. (2015). Fall detection in homes of older adults using the Microsoft Kinect. IEEE Journal of Biomedical and Health Informatics, 19, 290–301. doi:10.1109/JBHI.2014.2312180 [DOI] [PubMed] [Google Scholar]
- Stone E., Skubic M., Rantz M., Abbott C., Miller S. (2015). Average in-home gait speed: Investigation of a new metric for mobility and fall risk assessment of elders. Gait & Posture, 41, 57–62. doi:10.1016/j.gaitpost.2014.08.019 [DOI] [PubMed] [Google Scholar]
- Su B. Y., Ho K. C., Rantz M. J., Skubic M. (2015). Doppler radar fall activity detection using the wavelet transform. IEEE Transactions on Biomedical Engineering, 62, 865–875. doi:10.1109/TBME.2014.2367038 [DOI] [PubMed] [Google Scholar]
- Vellas B. J., Wayne S. J., Romero L., Baumgartner R. N., Rubenstein L. Z., Garry P. J. (1997). One-leg balance is an important predictor of injurious falls in older persons. Journal of the American Geriatrics Society, 45, 735–738. [DOI] [PubMed] [Google Scholar]
- Yardibi T., Cuddihy P., Genc S., Bufi C., Skubic M., Rantz M., Phillips C. (2011). Gait characterization via pulse-Doppler radar. In Proceedings, 9th Annual IEEE International Conference on Pervasive Computing and Communications: Workshop on Smart Environments to Enhance Health Care, Seattle, WA, March 21–25, 2011 (pp. 662–667). Piscataway, NJ: IEEE Press. doi:10.1109/PERCOMW.2011.5766971 [Google Scholar]
- Wang F., Skubic M., Abbott C., Keller J. (2010). Body sway measurement for fall risk assessment using inexpensive webcams. In Proceedings, 32nd Annual International Conference of the IEEE Engineering in Medicine and Biology Society: “Merging Medical Humanism and Technology”, Buenos Aires, Argentina, August 31–September 4, 2010 (pp. 2225–2229). Piscataway, NJ: IEEE Press. doi:10.1109/IEMBS.2010.5626100 [DOI] [PubMed] [Google Scholar]
- Woolrych R., Zecevic A., Sixsmith A., Sims-Gould A., Feldman F., Chaudhury H., Robinovitch S. N. (2014). Using video capture to investigate the causes of falls in long-term care. The Gerontologist. Advance online publication. doi:10.1093/geront/gnu053 [DOI] [PubMed] [Google Scholar]
- Zecevic A. A., Salmoni A. W., Speechley M., Vandervoort A. A. (2006). Defining a fall and reasons for falling: Comparisons among the views of seniors, health care providers, and the research literature. The Gerontologist, 46, 367–376. doi:10.1093/geront/46.3.367 [DOI] [PubMed] [Google Scholar]