Abstract
Purpose of the Study:
(a) Identify the prevalence of nursing homes providing Medicare supported restorative care programs and of long stay participants, (b) compare characteristics between restorative care participants and nonparticipants, and (c) assess restorative care’s effect on change in activities of daily living (ADL) dependency.
Design and Methods:
Longitudinal analysis of Minimum Data Set assessments linked to the 2004 National Nursing Home Survey using a sample of 7,735 residents, age ≥ 65 years living in 1,097 nursing homes for at least 6 months. Receipt of any restorative care was used as a time varying predictor to estimate change in ADL dependency over 18 months using linear mixed models.
Results:
The sample was 75% female, 89% non-Hispanic White, with a mean age of 85±8, and average length of stay of 3.2±3.4 years. Most nursing homes had restorative care programs (67%), but less than one-third of long-stay residents participated. After controlling for resident and nursing home characteristics, the predicted mean ADL dependency score (range 0–28) at baseline was 18 for restorative care participants and 14 for nonparticipants. Over 18 months, ADL dependency increased 1 point for both participants and nonparticipants (p = .12).
Implications:
A minority of long-stay residents participated in Medicare supported restorative care programs despite their availability and potential benefits. Even though participants had greater vulnerability for deterioration in physical, mental, and functional health than nonparticipants, both groups had similar rates of ADL decline. Future research is needed to determine if providing restorative care to less dependent long-stay residents is effective.
Key words: Restorative care nursing, Activities of daily living, Minimum data set, Long-stay nursing home residents, Function focused care
Introduction
Since the passage of the 1987 Omnibus Reconciliation Act, nursing homes have implemented restorative care programs to meet mandates to optimize the function of each resident. Since 1998, nursing homes can receive additional reimbursement under the Medicare Skilled Nursing Facility Prospective Payment System if they provide two or more restorative care activities related to walking, passive and active range of motion, bed mobility, transferring, dressing, grooming, eating, swallowing, communicating, splint, brace, and prosthesis care at least 15min a day/six days a week (Centers for Medicare and Medicaid Services, n.d.). The decision to reimburse for these activities was based on the results of the Nursing Home Case Mix and Quality Demonstration project completed in 1998 (Reilly, Mueller, & Zimmerman, 2007). Since then there has been no formal evaluation of the effectiveness of Medicare supported restorative care programs needed to guide future practice and research.
Restorative care is more broadly defined as a philosophy of care that emphasizes the evaluation of residents’ underlying capabilities with regard to function and helping them to optimize and maintain functional abilities (Resnick, Galik, & Boltz, 2013). Two different approaches to restorative care (dedicated and integrated) dominate the literature. Medicare supported restorative care programs often follow the dedicated approach where designated staff are trained to provide activities in 15min increments to residents who demonstrate a decline in function or who need to maintain functional gains upon completing physical, occupational, or speech therapy (Centers for Medicare and Medicaid Services, n.d.). Nursing staff generally determine who receives restorative care based on observed functional decline and on their perception of the resident’s potential to benefit, but little else is known about who receives restorative care and who is most likely to benefit (Vahakangas, Noro, & Bjorkgren, 2006). Proponents of the integrated approach focus on training all staff to integrate activities that promote function and physical activity in all care interactions with all residents. However, empirical support for either approach is scant. One large group randomized clinical trial (N = 487 residents in 12 nursing homes) of an integrated approach found improvements in mobility, gait, balance, walking, bathing, and stair climbing, but didn’t find improvements in overall activity of daily living (ADL) function (Resnick et al., 2009). A few quasi-experimental studies have found conflicting results including: improvement (Chang, Wung, & Crogan, 2008; Morris et al., 1999) maintenance (Galik et al., 2008), and deterioration in ADL dependency (Resnick et al., 2006). This study evaluates the effect of Medicare supported restorative care programs to provide additional evidence to guide program implementation and development.
On any given day, over 70% of residents have lived in the nursing home for at least six months (Center for Disease Control and National Center for Health Statistics, n.d.). These long-stay residents may represent a group likely to benefit from restorative care as they typically experience increasing ADL dependency over time that is associated with resident and nursing home characteristics (Arling, Kane, Mueller, Bershadsky, & Degenholtz, 2007; McConnell et al., 2003; Wang, Kane, Eberly, Virnig, & Chang, 2009). Resident characteristics associated with ADL dependency include being older, female, and having a longer length of stay (Ang, Au, Yap, & Ee, 2006; Peres, Verret, Alioum, & Barberger-Gateau, 2005). Pathologies associated with dependency include arthritis, diabetes, heart disease, chronic obstructive pulmonary disease, depression, having multiple chronic illnesses, and stroke (Ang et al., 2006; Arling et al., 2007; Fried & Guralnik, 1997; Frytak, Kane, Finch, Kane, & Maude-Griffin, 2001). Physical impairments with balance, gait and range of motion also contribute to dependency (Ang et al., 2006; Arling et al., 2007; Fried & Guralnik, 1997; McConnell et al., 2003; Sakari-Rantala, Era, Rantanen, & Heikkinen, 1998; Wang et al., 2009). Nursing home characteristics that may influence ADL dependency include: the number of residents, nurse staffing levels, certification of clinical leaders, and type of ownership (Arling et al., 2007; Wang et al., 2009). Providing evidence that restorative care is effective for long stay residents may help nursing homes select participants.
All nursing homes receiving reimbursement from the Centers for Medicare and Medicaid Services are required to report the results of standardized assessments of resident health using the Minimum Data Set (MDS). The MDS also reports restorative care provision. Recently, a sample of MDS data linked to the nationally representative 2004 National Nursing Home Survey became available and provides a means to describe restorative care participants and to evaluate the effectiveness of Medicare supported restorative care programs. Therefore, the purpose of this study was to use this nationally representative sample of MDS data to: (a) identify the prevalence of long stay nursing home residents receiving restorative care and the prevalence of nursing homes providing restorative care programs, (b) compare characteristics of residents who do and do not receive restorative care, and (c) assess restorative care’s effect on change in ADL dependency. The primary hypothesis for this study was that restorative care participants would experience a slower rate of decline in ADL dependency over 18 months than nonparticipants after controlling for resident (i.e., age, length of stay, cognitive impairment, frailty, number of disabling diseases, mood, social engagement, pain, number of physical impairments, baseline ADL function, nurse assessment of ability to improve ADLs) and nursing home characteristics (i.e., percentage of residents with Medicare and Medicaid reimbursement, hours of nursing contact, medical director and director of nursing certification, and facility accreditation) associated with functional decline. The findings can provide information for guiding future restorative care research and practice.
Design and Methods
This study was a longitudinal analysis of nursing home MDS data linked to the nationally representative 2004 National Nursing Home Survey (NNHS). The dataset was provided by the National Center for Health Statistics (NCHS) upon the Center’s approval of the study protocol. Because the analyses required restricted use variables from NCHS, they were accessed through the Minnesota Census Research Data Center. Resident variables came from the MDS data and nursing home variables came from the NNHS.
Sample
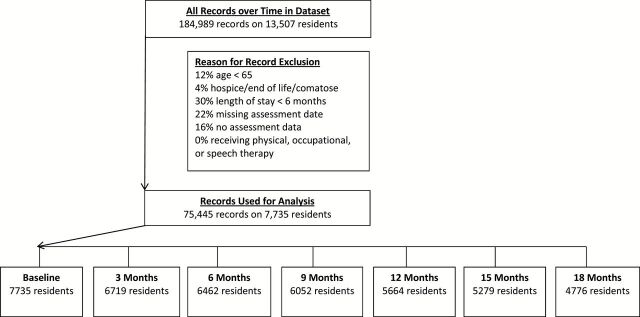
The sample included older long-stay nursing home residents likely to benefit from restorative care. Residents had to be age 65 years or older and live in the nursing home for at least six months. Cases were deleted if residents were bedfast, in a persistent vegetative state, had six or fewer months to live, or had end-stage disease as they are unlikely to maintain or improve function. Residents receiving occupational, physical, or speech therapy were also excluded, as these interventions may account for ADL improvement. Figure 1 summarizes the reasons for record deletion.
Figure 1.
Sample creation and attrition.
Longitudinal Dataset
A full MDS assessment is performed within 14 days of admission and annually; a smaller assessment is done quarterly and with any significant change in health. Admission, quarterly, significant change, and annual MDS data for residents meeting eligibility criteria during 2003–2006 were used to create an 18-month dataset. The dataset was structured into quarterly time points (i.e., baseline, 3, 6, 9, 12, 15, and 18 months). The latest assessment available for each 3-month period was used. Only 7% of assessments came from significant change assessments. The 18-month time frame was selected to provide at least one year of data to examine the long-term effects of restorative care and is consistent with recommendations to determine the long-term sustainability of rehabilitation efforts (Forster et al., 2009). Baseline MDS variables were selected from the first available full or admission assessment. Nursing home characteristics came from the cross-sectional NNHS and were treated as baseline variables. Table 1 summarizes which variables came from which survey. Figure 1 summarizes the attrition rate. At 18 months, 60% of the residents remained in the dataset.
Table 1.
List of Study Variables
| Restorative care | Activities of daily living (ADL) dependency | Resident characteristics | Nursing home characteristics |
|---|---|---|---|
| MDS items | MDS items | MDS items | NNHS items |
| Passive range of motion | ADL self-performance scale | Age | % Residents with Medicare reimbursement |
| Active range of motion | Length of stay | % Residents with Medicaid reimbursement | |
| Splint/brace assistance | Cognitive Performance Scale | Hours of patient contact with nursing staff | |
| Bed mobility | Frailty | Medical Director certification | |
| Transferring | Number of disabling diseases | Director of Nursing certification | |
| Walking | Mood | Facility accreditation | |
| Dressing/grooming | Social engagement | ||
| Eating/swallowing | Pain | ||
| Amputation/prosthesis care | Number of physical impairments | ||
| Communication | Staff assessment of resident’s ability to improve ADL dependency | ||
| Other |
Notes: MDS = minimum data set; NNHS = National Nursing Home Survey.
MDS Variables
MDS Psychometric Properties
The MDS version 2.0 has been used in many outcome and evaluation studies and the reliability and validity of the items has been reported by other researchers. Over 85% of MDS data items have adequate inter-rater reliability (κ > .6) (Mor, 2004). The most reliable and valid MDS scales include those that measure ADLs, cognitive function, and medical diagnoses. Measures with less ideal psychometric properties include pain, depressed mood, and social engagement (Casten, Lawton, Parmelee, & Kleban, 1998; Frederiksen, Tariot, & De Jonghe, 1996; Gambassi et al., 1998; Hartmaier et al., 1995; Lawton et al., 1998; Mor, Intrator, Unruh, & Cai, 2011, Morris et al., 1990; Williams, Li, Fries, & Warren, 1997). Nursing home employees collect MDS data by interviewing direct care staff and reviewing health records, as such, concerns have been raised about variability between facilities in measurement quality (Lum, Lin, & Kane, 2005; Shin & Scherer, 2009). Facilities that over- or under-report resident data tend to do so for all items (Wu, Mor, & Roy, 2009). Therefore, it is important to account for each resident’s nursing home when using MDS data. Despite these limitations, the MDS provides comprehensive, systematically collected data useful for evaluating restorative care delivered in real settings.
ADL dependency was measured with the MDS ADL-7 measure. This additive scale uses seven MDS items that assess residents’ ability to self-perform bed mobility, transferring, dressing, eating, toilet use, personal hygiene and bathing. A 5-point Likert scale from 0 (independent) to 4 (total dependence) measures levels of dependency in each activity. Total scores range from 0–28 with higher scores indicating greater dependency. The ADL-7 has strong internal consistency (Cronbach’s alpha > .85) (Mor, Intrator, Unruh, & Cai, 2011) and moderate to strong correlations with other ADL measures (r = .58–.79) (Frederiksen et al., 1996; Lawton et al., 1998; Snowden et al., 1999), and predicts nursing assistant time utilization (Morris et al., 1999). It has been found sensitive to change in observational and interventional studies (Carpenter, Hastie, Morris, Fries, & Ankri, 2006; Grando et al., 2009; Morris et al., 1999).
Restorative care activities are reported in the MDS as the number of days in the past 7 days a resident received at least 15min of passive and active range of motion, splint-brace assistance/training and skill practice with bed mobility, transferring, walking, dressing, grooming, eating, swallowing, amputation-prosthesis care, communication, or other skills. In preliminary analyses restorative care was operationalized three ways: (a) dichotomously as having received any restorative care activity, (b) as a count of the number of restorative care activities received, and (c) as a continuous variable summing the number of days each activity was provided. Neither the count (p = .40) nor continuous (p = .76) variable were predictive of ADL dependency in univariable models, so they were not used in the analysis. The dichotomous variable did predict ADL dependency (p = .02) and was used as the independent variable in the multivariate model to represent receiving restorative care. Since the receipt of restorative care can vary quarterly, it was used as a time varying predictor. A question from the NNHS was used to determine the prevalence of nursing homes using specially trained personnel to provide restorative care programs.
Resident Characteristics
MDS measures of age, gender, race/ethnicity and length of stay were used. A variable counting 10 categories of diseases associated with ADL decline was created from MDS items. The categories included: dementia, stroke/paralysis, arthritis, cancer, chronic obstructive pulmonary disease, heart disease, diabetes, neurological disease, depression, and eye disease.
Cognitive impairment was measured with the MDS Cognitive Performance Scale, which defines six levels of impairment. Scores range from 0–6 with higher scores indicated greater impairment. It has strong sensitivity (.94) and specificity (.94) (Hartmaier, Sloane, Guess, & Koch, 1994; Hartmaier et al., 1995; Morris et al., 1994). A physical impairment score ranging from 0–4 was created by awarding one point for having an impairment in each of balance, mobility, range of motion, and voluntary movement. This measure demonstrated good internal consistency with Cronbach’s alpha equal to .70. Frailty was measured with the Edmonton frailty scale. This multi-dimensional scale includes MDS items related to cognition, general health status, functional independence, social support, medication use, nutrition, mood, continence, and functional performance. Scores range from 0–17 with higher scores representing greater frailty (Armstrong, Stolee, Hirdes, & Poss, 2010).
The MDS social engagement scale includes six items related to interactions with others, and engagement in planned, structured, and self-initiated activities. Scores range from 0–6 with higher scores indicating greater social engagement. It has demonstrated good internal consistency with Cronbach’s alpha equal to .79 (Dubeau, Simon, & Morris, 2006; Mor et al., 1995). The Burrow’s mood scale uses seven MDS items to create a scale ranging from 0–14 that indicates depressive symptoms. It has good internal consistency (Cronbach’s alpha > .70) and validity with the Hamilton Depression Rating Scale and the Cornell scale (Burrows, Morris, Simon, Hirdes, & Phillips, 2000). The MDS Pain Scale uses two items on pain frequency and intensity to categorize pain as none, mild, moderate, or severe. It has demonstrated good agreement (93%) and concurrent validity (κ = .71) with nurse administered assessments of pain using a visual analog scale in the post-acute setting (Fries, Simon, Morris, Flodstrom, & Bookstein, 2001). A dichotomous MDS item indicating whether or not direct care staff think the resident is capable of increased independence in at least some ADLs was also included in the analysis (Vahakangas et al., 2006).
NNHS Variables
The following nursing home traits from the NNHS were used in the analysis: percent of residents with Medicare reimbursement, percent of residents with Medicaid reimbursement, hours of patient contact with nursing staff, medical director and director of nursing certification, and facility accreditation. Nursing staff patient contact hours were measured as the average number of full time equivalent hours that registered nurses, licensed practical nurses, and nursing assistants spent on patient care. A dichotomous variable was created to indicate if the medical director had certification in any of these specialties: family medicine, internal medicine, geriatrics, or palliative care. A dichotomous variable was created to indicate if the director of nursing had certification from the National Association of Directors of Nursing Administration in Long Term Care, American Nurses Credentialing Center in gerontological nursing, or other certifying agency. A dichotomous variable was created to indicate if the facility was accredited by the Joint Commission for Accreditation of Healthcare Organizations Rehabilitation Accreditation Commission, or Continuing Care Accreditation Commission. Additionally, the state of nursing home residence was entered as a random effect into the models to account for differential restorative care reimbursement policies and regional variation in MDS data collection.
Analysis
Descriptive statistics were used to identify the prevalence of residents receiving and of nursing homes providing restorative care and to describe resident characteristics. Univariable chi-square or t-tests were used to compare baseline differences between residents who did and did not receive restorative care. Linear mixed models were used to determine restorative care’s effect on ADL dependency over 18 months. The association over time for the dependent variable appeared to be compatible with an autoregressive covariance structure which was used in the model. Resident variables were used as time varying predictors and nursing home variables were used as static predictors. Preliminary analysis indicated that a linear model best described change in ADL dependency over time. Variables with a p < .01 in univariable models (analyses not presented) were included in the final multivariable model. To avoid collinearity among predictors, variables with a correlation of .50 or greater with another variable were excluded. Data analysis was generated using SAS for Unix software (SAS Institute Inc., Cary, NC).
The model for the multivariable analyses is specified here.
Where k represents state, i represents subject ID, j represents time point, and p represents the number of covariates, n k is the total number of subjects in k th state, and n kj is the total number of time points for i th subjects in k th state, and n kj is the total number of time points for i th subject in k th state.
Ethical Considerations
Data collection for the 2004 NNHS was approved by the NCHS Research Ethics Review Board. The University of Minnesota deemed this analysis of de-identified data from the survey to be exempt from federal regulations for the protection of human research participants. Analysis of restricted data through the NCHS Research Data Center was also approved by the NCHS Ethical Review Board.
Results
Prevalence of Restorative Care
About 67% of nursing homes provided restorative care programs. The percentage of residents receiving restorative care increased after the baseline assessment and then stabilized (24% at baseline, 35% at quarter 1, 36% at quarter 2, 36% at quarter 3, 35% at quarter 4, 37% at quarter 5, 37% at quarter 6). The most common restorative care activities were walking, passive and active range of motion, and dressing/grooming (Table 2).
Table 2.
Percent of Residents Participating in Restorative Care Activities by Quarter
| Restorative care activity | Baseline, N = 7,735 | Quarter 1, N = 6,719 | Quarter 2, N = 6,462 | Quarter 3, N = 6,052 | Quarter 4, N = 5,664 | Quarter 5, N = 5,279 | Quarter 6, N = 4,676 |
|---|---|---|---|---|---|---|---|
| Passive range of motion | 8.9 | 11.0 | 10.9 | 11.6 | 11.6 | 13.4 | 12.9 |
| Active range of motion | 10.7 | 16.8 | 17.7 | 17.2 | 17.3 | 17.4 | 16.8 |
| Splint/brace assistance | 2.2 | 2.6 | 2.7 | 2.8 | 2.9 | 3.6 | 3.3 |
| Bed mobility | 2.4 | 2.2 | 2.0 | 2.3 | 2.2 | 2.5 | 2.4 |
| Transferring | 4.4 | 6.0 | 5.7 | 5.5 | 5.3 | 5.9 | 5.9 |
| Walking | 9.3 | 15.7 | 16.1 | 16.0 | 15.1 | 14.4 | 14.7 |
| Dressing/grooming | 4.7 | 6.3 | 6.3 | 6.3 | 6.3 | 6.9 | 7.0 |
| Eating/swallowing | 2.5 | 3.3 | 3.3 | 3.5 | 3.3 | 4.0 | 4.1 |
| Amputation/prosthesis | 0.1 | 0.2 | 0.2 | 0.3 | 0.3 | 0.3 | 0.2 |
| Communication | 0.3 | 0.5 | 0.5 | 0.5 | 0.5 | 0.6 | 0.5 |
| Other | 1.7 | 2.8 | 3.0 | 3.1 | 3.0 | 3.1 | 2.7 |
| Received any activity | 24.1 | 35.0 | 35.9 | 35.9 | 35.3 | 36.9 | 36.9 |
Comparison of Residents Who Do and Do Not Receive Restorative Care
While the majority of long stay residents were white females with a mean age of 85±8 years who lived in urban for profit nursing homes for an average of 3.2±3.4 years residents receiving restorative care differed from those not receiving restorative care on a number of baseline characteristics. Restorative care participants had more cognitive impairment (p < .001), disabling diseases (p < .001), depressive symptoms (p < .001), physical impairments (p < .001), and ADL dependency (p < .001) at baseline than nonparticipants (Table 3). Participants were also less likely to have pain (p < .001) and more likely for their nurse to indicate that the resident did not have the ability to improve ADL dependency (p < .001). Restorative care participants were also more likely to live in non-urban (p < .001), non-accredited (p = .008), not for profit (p < .001) facilities with a higher percentage of residents with Medicaid reimbursement (p < .001), and in nursing homes where medical directors (p = .02) and directors of nursing (p = .006) lacked specialty certification.
Table 3.
Baseline Comparisons Between Restorative Care Participants and Nonparticipants
| Total sample, N = 7,735 | Received restorative care, N = 1,864 | Did not receive restorative care, N = 5,871 | Chi-square | t | p valuea | ||||
|---|---|---|---|---|---|---|---|---|---|
| % | Mean ± SD | % | Mean ± SD | % | Mean ± SD | ||||
| Resident traits | |||||||||
| Age in years | 84.8±8.0 | 85.2±8.1 | 84.6±8.0 | −2.8 | .005 | ||||
| Length of stay in years | 3.2±3.4 | 3.3±3.5 | 3.1±3.3 | −2.1 | .04 | ||||
| Female | 75.4 | 74.5 | 75.7 | 1.2 | .27 | ||||
| White race | 88.9 | 89.4 | 88.7 | 0.8 | .38 | ||||
| Live in urban nursing home | 52.2 | 47.5 | 61.1 | 25.0 | <.001 | ||||
| Live in for profit nursing home | 59.2 | 52.8 | 53.8 | 57.5 | <.001 | ||||
| Cognitive Performance Scale score (range 0–6) | 2.3±1.4 | 2.5±1.3 | 2.2±1.4 | −9.0 | <.001 | ||||
| Frailty (range 0–15) | 6.3±2.2 | 6.2±1.9 | 6.3±2.3 | 1.5 | .15 | ||||
| Number of disabling diseases (range 0–10) | 2.5±1.4 | 2.8±1.4 | 2.4±1.3 | −10.3 | <.001 | ||||
| Mood scale (range 0–14) | 0.9±1.6 | 1.0±1.7 | 0.9±1.5 | −4.4 | <.001 | ||||
| Social engagement (range 0–6) | 2.5±1.7 | 2.5±1.7 | 2.5±1.6 | 0.3 | .76 | ||||
| Pain: none | 60.3 | 63.6 | 59.2 | 26.5 | <.001 | ||||
| Pain: mild | 24.0 | 24.0 | 24.0 | ||||||
| Pain: moderate | 13.7 | 11.4 | 14.4 | ||||||
| Pain: severe | 2.0 | 1.0 | 2.4 | ||||||
| Number of physical impairments (range 0–4) | 2.7±1.2 | 3.0±1.1 | 2.5±1.2 | −14.7 | <.001 | ||||
| Activities of daily living dependency at baseline (range 0–28) | 15.3±7.6 | 17.5±7.2 | 14.6±7.7 | −14.2 | <.001 | ||||
| Nurse indicated resident had ability to improve ADL dependency | 26.9 | 17.5 | 29.9 | 111.3 | <.001 | ||||
| Nursing home traits | |||||||||
| Percentage of residents with Medicare reimbursement | 3.0 | 1 | 3.0 | 5.2 | <.001 | ||||
| Percentage of residents with Medicaid reimbursement | 20.0 | 26 | 18 | −7.0 | <.001 | ||||
| Hours of patient contact with nursing staff | 73.3±110.2 | 70.5±107.1 | 74.2±111.2 | 1.2 | .22 | ||||
| Medical Director certification | 84.4 | 82.6 | 84.9 | 5.7 | .02 | ||||
| Director of Nursing certification | 37.3 | 34.6 | 38.2 | 7.7 | .006 | ||||
| Facility accreditation | 11.1 | 9.4 | 11.7 | 7.0 | .008 | ||||
Note: a p value comes from univariable Chi-square test for categorical variables, and t-test for continuous variables. ADL = Activities of daily living.
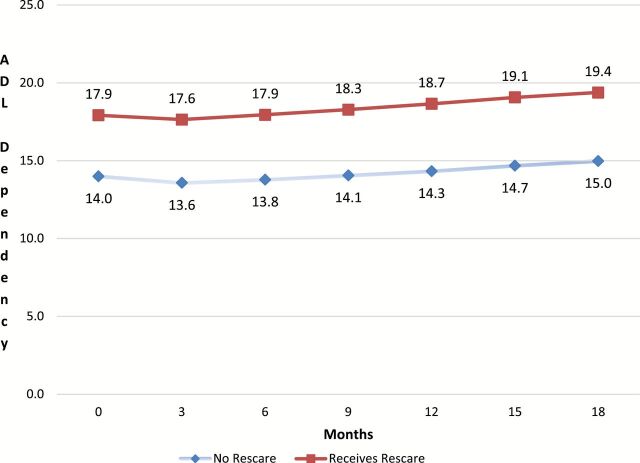
Effect of Restorative Care on ADL Dependency
Table 4 presents the results of the multivariable model. The results indicate that restorative care programs did not have an effect (p = .12) on change in ADL dependency after controlling for resident and nursing homes traits. Figure 2 plots change in ADL dependency for residents who did and did not receive restorative care. After controlling for resident and nursing home traits, the predicted mean ADL dependency score at baseline was 17.9 for restorative care participants and 14.0 for nonparticipants. Participants experienced statistically similar rates of decline in ADL dependency over 18 months as did nonparticipants. Over 18 months ADL dependency increased 0.5 points for restorative care participants and 1.0 point for nonparticipants.
Table 4.
Effect of Restorative Care on Change in Activities of Daily Living (ADL) Dependency Over 18 Months Controlling for Resident and Nursing Home Confounders
| Characteristic | Coefficient | SE | p value |
|---|---|---|---|
| Intercept | −1.6 | .42 | N/A |
| Resident Traits | |||
| Age in years | .01 | .003 | .15 |
| Length of stay in years | <.0001 | <.0001 | .89 |
| Cognitive Performance Scale score (range 0–6) | .38 | .03 | <.001 |
| Frailty (range 0–15) | .63 | .01 | <.001 |
| Number of disabling diseases (range 0–10) | .10 | .02 | <.001 |
| Mood scale (range 0–14) | −.16 | .02 | <.001 |
| Social engagement (range 0–6) | −.39 | .02 | <.001 |
| Pain: mild (reference: severe) | −.57 | .20 | .004 |
| Pain: moderate (reference: severe) | −.37 | .20 | .07 |
| Pain: none (reference: severe) | −.55 | .20 | .006 |
| Number of physical impairments (range 0–4) | .97 | .03 | <.001 |
| Activities of daily living baseline score (range 0–28) | .68 | .01 | <.001 |
| Nurse indicated resident did not have the ability to improve ADL dependency | −.13 | .07 | .06 |
| Received any restorative care over time | .09 | .06 | .12 |
| Nursing home traits | |||
| Percentage of residents with Medicare reimbursement | −.07 | .22 | .76 |
| Percentage of residents with Medicaid reimbursement | −.02 | .08 | .75 |
| Hours of patient contact with nursing staff | −.0001 | .0003 | .68 |
| Medical Director has no certification | .19 | .09 | .04 |
| Director of Nursing has no certification | .07 | .07 | .31 |
| Facility has no accreditation | −.11 | .10 | .29 |
Notes: The model included the resident ID as an indication of which records were repeated on the same subject. State of nursing home location was included as a random effect. If the sign of the coefficient is positive for continuous variables, then as the value of the predictor increases, so does the level of ADL dependency over time. For categorical variables a positive coefficient is associated with increasing ADL dependency in comparison to the reference category for the categorical variable.
Figure 2.
Predicted change in activities of daily living (ADL) dependency by receipt of restorative care after adjusting for confounding resident and nursing home traits. Note: Estimates of ADL scores for each month were computed as follows: The beta coefficients were applied to the values of each covariate for each subject by quarter resulting in an estimate of ADL function for each subject at each quarter. Means were computed for these individual ADL estimates at each time period separately for those who did and did not receive restorative care.
Discussion
Although most nursing homes provided Medicare supported restorative care programs, only a third of long-stay residents participated. Participants had higher levels of ADL dependency, physical and cognitive impairments, and disabling diseases. However, both participants and nonparticipants experienced a similar rate of decline in ADL dependency, suggesting most long-stay residents are candidates for interventions to reduce functional decline.
At baseline 24% of long-stay residents received restorative care and this increased to 37% over 18 months. This study was unable to determine potential causes of low participation, but other researchers have identified resident and organizational characteristics that affect participation (Benjamin, Edwards, Ploeg, & Legault, 2014). Residents may choose not to participate because they don’t find the activities to be valuable, interesting, or beneficial (Benjamin et al., 2014). Nursing staff have identified the following barriers: limited time to develop trust and to motivate residents to participate, learned dependency by the residents, limited knowledge on motivating residents with cognitive impairment, beliefs that residents are unable to participate, pressure to get care tasks done efficiently, and a fear that participation may lead to injurious falls (Resnick et al., 2008). Low participation is also likely influenced by state reimbursement policies. Not all state Medicaid programs reimburse for restorative care and 20% of this sample included Medicaid recipients. Currently, only states with case mix Medicaid programs reimburse for restorative care as part of the Resource Utilization Group alternative criteria. To lessen the influence of this confounder the state of residence was included as a random effect in the model.
The most clinically relevant baseline difference between participants and nonparticipants was that participants had higher levels of ADL dependency (mean ADL score of 17.5 for participants vs. 14.6 for nonparticipants). While participants also had higher levels of cognitive impairment, a greater number of disabling diseases, and greater number of physical impairments, the clinical relevance is minimal as the mean differences are small and statistically significant because of the large sample size. The finding that nurses select residents with greater ADL dependency to receive restorative care is consistent with one previous report (Berg et al., 1997) and most likely reflects the practice of targeting residents for restorative care when functional impairments are most apparent. However, both participants and nonparticipants experienced on average a clinically meaningful increase in care needs for one ADL, indicating that efforts to maintain function are needed for most long-stay residents. A potential alternative explanation for the exclusion of residents with less dependency may be reimbursement policies that provide higher compensation for residents with greater dependency.
Residents who participated in restorative care did not experience a different rate of decline in ADL dependency as nonparticipants, suggesting these Medicare reimbursed programs may not have their intended effect. This may be related to the intensity and structure of Medicare reimbursed programs. It may be that the reimbursable level of providing restorative care activities 15min per day/six days per week lacks the frequency and intensity needed to be effective. For example, walking was the second most common restorative activity provided, yet the 15min threshold is well below the 30min recommended for older adults (Nelson et al., 2007). The structure of restorative care programs was also unknown in this study. For example, it is unknown if nursing homes integrated restorative activities into all care routines or used a dedicated approach. Most likely, these programs used the dedicated approach where restorative activities are provided only by specially designated nursing staff at specific times. There is little empirical evidence to suggest whether an integrated or dedicated approach is more effective. However, a recent systematic literature review found that integrated restorative care provided in controlled settings provides improvement in ADL dependency, physical function, walking, and physical activity (Resnick et al., 2013). An alternative explanation for the lack of effect may be that participants had higher levels of ADL dependency and as such had less room for improvement, thus minimizing the potential effect. However, this alternative explanation is less likely given the findings of a recent group randomized clinical trial that found using an integrative approach to restorative care led to improved physical function, increased physical activity, and reduced falls in long-stay residents with moderate to severe cognitive impairment (Galik et al., 2014).
The findings of this study should not be used to justify eliminating these programs or associated reimbursement as, the majority of long-stay residents who had moderate levels of ADL dependency did not participate in Medicare supported restorative care programs. This group of moderately disabled residents would most likely benefit from restorative care. These findings in conjunction with recent evidence support the current initiative to implement restorative care as a philosophy of care rather than as a program of discrete activities (Resnick, Galik, & Boltz, 2013). Future research is needed to determine if expanding restorative care to all long-stay residents is effective and to compare the efficacy of integrated and dedicated restorative care programs (Resnick, Galik, Remsburg, & Pretzer-Aboff, 2009).
Limitations
There are study limitations worth noting. ADL dependency is not the only outcome to consider when evaluating restorative care. Outcomes specific to each type of restorative activity could provide more precise measures of effect, for example, measuring gait speed for residents in an ambulation program (Forster, Lambley, & Young, 2010). However, these measures were not available in this dataset. The MDS restorative care measures did not permit detection of a dose-response relationship. A potential bias with selecting the latest MDS assessment available each quarter may have skewed the outcome towards residents experiencing a significant change. However, this bias is minimal as only 7% of assessments came from a significant change event. Ideally an admission cohort design would have been used. However, this was not possible because less than 1.5% of the long stay residents were newly admitted. At 18 months 40% of the sample had died or been discharged. The extent to which potential differences between surviving and censored residents impacted the progression of ADL dependency is unknown. Despite these limitations this study provides useful information on who receives restorative care and its effect on participants that can be used to guide future practice and research.
Conclusions
In this nationally representative sample of nursing home MDS data, two thirds of nursing homes provided restorative care programs, but less than one third of long stay residents participated. Participants had higher levels of ADL dependency, but similar rates of progression in ADL dependency as nonparticipants, suggesting that nonparticipants may have benefited from restorative care. It is worthwhile to consider implementing restorative care as a philosophy of integrated care rather than as a program of discrete activities. Future research is needed to compare the effectiveness of integrated and dedicated approaches to restorative care and to identify its effect when it is offered to all long-stay residents.
Funding
This project was supported by Grant Number K12HD055887 from the Building Interdisciplinary Research Careers in Women’s Health Program of the National Institutes of Child Health and Human Development to the Deborah E. Powell Center for Women’s Health at the University of Minnesota and by grant number 1R03AG037127-01A1 from the National Institute on Aging. Research results and conclusions expressed are those of the authors and do not necessarily reflect the views of the Census Bureau, the Research Data Center, the National Center for Health Statistics, the Centers for Disease Control and Prevention, or the National Institutes of Health. K. M. C. Talley was funded by the John A. Hartford Foundation as a Building Academic Geriatric Nursing Capacity pre-doctoral fellow from 2002–2004 and as a Claire M. Fagin post-doctoral fellow from 2008–2010.
Acknowledgements
The research in this article was conducted while the PI (K. M. C. Talley) and statisticians (K. Savik & H. Zhao) were Special Sworn Status researchers of the U.S. Census Bureau at the Minnesota Census Research Data Center. The data for the study was provided by the National Center for Health Statistics at the Centers for Disease Control and Prevention. This article has been screened to insure that no confidential data are revealed.
References
- Ang Y. H., Au S. Y., Yap L. K., Ee C. H. (2006). Functional decline of the elderly in a nursing home. Singapore Medical Journal, 47, 219–224. [PubMed] [Google Scholar]
- Arling G., Kane R. L., Mueller C., Bershadsky J., Degenholtz H. B. (2007). Nursing effort and quality of care for nursing home residents. The Gerontologist, 47, 672–682. doi:10.1093/geront/47.5.672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong J. J., Stolee P., Hirdes J. P., Poss J. W. (2010). Examining three frailty conceptualizations in their ability to predict negative outcomes for home-care clients. Age and ageing, 39, 755–758. doi:10.1093/ageing/afq121 [DOI] [PubMed] [Google Scholar]
- Benjamin K., Edwards N., Ploeg J., Legault F. (2014). Barriers to physical activity and restorative care for residents in long-term care: A review of the literature. Journal of aging and physical activity, 22, 154–165. doi:10.1123/japa.2012-0139 [DOI] [PubMed] [Google Scholar]
- Berg K., Sherwood S., Murphy K., Carpenter G. I., Gilgen R., Phillips C. D. (1997). Rehabilitation in nursing homes: A cross-national comparison of recipients. Age & Ageing, 26(Suppl. 2), 37–42. doi:10.1093/ageing/26.suppl_2.37 [DOI] [PubMed] [Google Scholar]
- Burrows A., Morris J., Simon S., Hirdes J., Phillips C. (2000). Development of a minimum data set-based depression rating scale for use in nursing homes. Age and Ageing, 29, 165–172. doi:10.1093/ageing/29.2.165 [DOI] [PubMed] [Google Scholar]
- Carpenter G. I., Hastie C. L., Morris J. N., Fries B. E., Ankri J. (2006). Measuring change in activities of daily living in nursing home residents with moderate to severe cognitive impairment. BMC Geriatrics, 6, 7. doi:10.1186/1471-2318-6-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casten R., Lawton M. P., Parmelee P. A., Kleban M. H. (1998). Psychometric characteristics of the minimum data set I: Confirmatory factor analysis. Journal of the American Geriatrics Society, 46, 726–735. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. (n.d.). Revised long-term care facility resident assessment instrument user’s manual version 2.0. Retrieved from http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/NHQIMDS20.html.
- Center for Disease Control and National Center for Health Statistics. (n.d.). National Nursing Home Survey. Number of nursing homes, beds, current residents, and discharges: United States, selected years 1973–2004. Retrieved from http://www.cdc.gov/nchs/data/nnhsd/nursinghomefacilities2006.pdf#01.
- Chang S. H., Wung S. F., Crogan N. L. (2008). Improving activities of daily living for nursing home elder persons in Taiwan. Nursing Research, 57, 191–198. doi:10.1097/01.NNR.0000319492.14005.7f [DOI] [PubMed] [Google Scholar]
- Dubeau C. E., Simon S. E., Morris J. N. (2006). The effect of urinary incontinence on quality of life in older nursing home residents. Journal of the American Geriatrics Society, 54, 1325–1333. doi:10.1111/j.1532-5415.2006.00861.x [DOI] [PubMed] [Google Scholar]
- Forster A., Lambley R., Hardy J., Young J., Smith J., Green J., Burns E. (2009). Rehabilitation for older people in long-term care. Cochrane Database of Systematic Reviews, 1, CD004294. doi:10.1002/14651858.CD004294.pub2 [DOI] [PubMed] [Google Scholar]
- Forster A., Lambley R., Young J. B. (2010). Is physical rehabilitation for older people in long-term care effective? Findings from a systematic review. Age and ageing, 39, 169–175. doi:10.1093/ageing/afp247 [DOI] [PubMed] [Google Scholar]
- Frederiksen K., Tariot P., De Jonghe E. (1996). Minimum Data Set Plus (MDS+) scores compared with scores from five rating scales. Journal of the American Geriatrics Society, 44, 305–309. [DOI] [PubMed] [Google Scholar]
- Fried L. P., Guralnik J. M. (1997). Disability in older adults: Evidence regarding significance, etiology, and risk. Journal of the American Geriatrics Society, 45, 92–100. [DOI] [PubMed] [Google Scholar]
- Fries B. E., Simon S. E., Morris J. N., Flodstrom C., Bookstein F. L. (2001). Pain in U.S. nursing homes: Validating a pain scale for the minimum data set. The Gerontologist, 41, 173–179. doi:10.1093/geront/41.2.173 [DOI] [PubMed] [Google Scholar]
- Frytak J. R., Kane R. A., Finch M. D., Kane R. L., Maude-Griffin R. (2001). Outcome trajectories for assisted living and nursing facility residents in Oregon. Health Services Research, 36, 91–111. [PMC free article] [PubMed] [Google Scholar]
- Galik E., Resnick B., Hammersla M., Brightwater J. (2014). Optimizing function and physical activity among nursing home residents with dementia: Testing the impact of function-focused care. The Gerontologist, 54, 930–943. doi:10.1093/geront/gnt108 [DOI] [PubMed] [Google Scholar]
- Galik E. M., Resnick B., Gruber-Baldini A., Nahm E. S., Pearson K., Pretzer-Aboff I. (2008). Pilot testing of the restorative care intervention for the cognitively impaired. Journal of the American Medical Directors Association, 9, 516–522. doi:10.1016/j.jamda.2008.04.013 [DOI] [PubMed] [Google Scholar]
- Gambassi G., Landi F., Peng L., Brostrup-Jensen C., Calore K., Hiris J., … Bernabei R. (1998). Validity of diagnostic and drug data in standardized nursing home resident assessments: Potential for geriatric pharmacoepidemiology. SAGE Study Group. Systematic Assessment of Geriatric drug use via Epidemiology. Medical Care, 36, 167–179. doi:10.1097/00005650-199802000-00006 [DOI] [PubMed] [Google Scholar]
- Grando V. T., Buckwalter K. C., Maas M. L., Brown M., Rantz M., Conn V. S. (2009). A trial of a comprehensive nursing rehabilitation program for nursing home residents post-hospitalization. Research in Gerontological Nursing, 2, 12. doi:10.3928/19404921-20090101-06 [DOI] [PubMed] [Google Scholar]
- Hartmaier S. L., Sloane P. D., Guess H. A., Koch G. G. (1994). The MDS Cognition Scale: A valid instrument for identifying and staging nursing home residents with dementia using the minimum data set. Journal of the American Geriatrics Society, 42, 1173–1179. [DOI] [PubMed] [Google Scholar]
- Hartmaier S. L., Sloane P. D., Guess H. A., Koch G. G., Mitchell C. M., Phillips C. D. (1995). Validation of the Minimum Data Set Cognitive Performance Scale: Agreement with the Mini-Mental State Examination. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 50, M128–133. doi:10.1093/gerona/50a.2.m128 [DOI] [PubMed] [Google Scholar]
- Lawton M. P., Casten R., Parmelee P. A., Van Haitsma K., Corn J., Kleban M. H. (1998). Psychometric characteristics of the minimum data set II: Validity. Journal of the American Geriatrics Society, 46, 736–744. [DOI] [PubMed] [Google Scholar]
- Lum T. Y., Lin W. C., Kane R. L. (2005). Use of proxy respondents and accuracy of minimum data set assessments of activities of daily living. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 60, 654–659. doi:10.1093/gerona/60.5.654 [DOI] [PubMed] [Google Scholar]
- McConnell E. S., Branch L. G., Sloane R. J., Pieper C. F. (2003). Natural history of change in physical function among long-stay nursing home residents. Nursing Research, 52, 119–126. doi:10.1097/00006199-200303000-00008 [DOI] [PubMed] [Google Scholar]
- Mor V. (2004). A comprehensive clinical assessment tool to inform policy and practice: Applications of the minimum data set. Medical Care, 42(Suppl. 4), 50–59. doi:10.1097/01.mlr.0000120104.01232.5e [DOI] [PubMed] [Google Scholar]
- Mor V., Branco K., Fleishman J., Hawes C., Phillips C., Morris J., Fries B. (1995). The structure of social engagement among nursing home residents. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 50, P1–P8. doi:10.1093/geronb/50b.1.p1 [DOI] [PubMed] [Google Scholar]
- Mor V., Intrator O., Unruh M. A., Cai S. (2011). Temporal and Geographic variation in the validity and internal consistency of the Nursing Home Resident Assessment Minimum Data Set 2.0. BMC Health Services Research, 11, 78. doi:10.1186/1472-6963-11-78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris J. N., Fiatarone M., Kiely D. K., Belleville-Taylor P., Murphy K., Littlehale S., … Doyle N. (1999). Nursing rehabilitation and exercise strategies in the nursing home. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 54, M494–500. doi:10.1093/gerona/54.10.m494 [DOI] [PubMed] [Google Scholar]
- Morris J. N., Fries B. E., Mehr D. R., Hawes C., Phillips C., Mor V., Lipsitz L. A. (1994). MDS Cognitive Performance Scale. Journal of Gerontology, 49(4), M174–182. doi:10.1093/geronj/49.4.m174 [DOI] [PubMed] [Google Scholar]
- Morris J. N., Hawes C., Fries B. E., Phillips C. D., Mor V., Katz S., … Friedlob A. S. (1990). Designing the national resident assessment instrument for nursing homes. The Gerontologist, 30, 293–307. doi:10.1093/geront/30.3.293 [DOI] [PubMed] [Google Scholar]
- Nelson M. E., Rejeski W. J., Blair S. N., Duncan P. W., Judge J. O., King A. C., … Castaneda-Sceppa C. (2007). Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Medicine and Science in Sports and Exercise, 39, 1435–1445. doi:10.1249/mss.0b013e3180616aa2 [DOI] [PubMed] [Google Scholar]
- Peres K., Verret C., Alioum A., Barberger-Gateau P. (2005). The disablement process: Factors associated with progression of disability and recovery in French elderly people. Disability and Rehabilitation, 27, 263–276. doi:10.1080/09638280400006515 [DOI] [PubMed] [Google Scholar]
- Reilly K. E., Mueller C., Zimmerman D. R. (2007). The Centers for Medicare and Medicaid Services’ Nursing Home Case-Mix and Quality Demonstration: A descriptive overview. Journal of Aging & Social Policy, 19, 61–76. doi:10.1300/J031v19n01_04 [DOI] [PubMed] [Google Scholar]
- Resnick B., Galik E., Boltz M. (2013). Function focused care approaches: Literature review of progress and future possibilities. Journal of the American Medical Directors Association, 14, 313–318. doi:10.1016/j.jamda.2012.10.019 [DOI] [PubMed] [Google Scholar]
- Resnick B., Galik E., Remsburg R. E., Pretzer-Aboff I. (2009). Concerns about dedicated restorative care. Journal of Gerontological Nursing, 35, 11–12. [DOI] [PubMed] [Google Scholar]
- Resnick B., Gruber-Baldini A. L., Zimmerman S., Galik E., Pretzer-Aboff I., Russ K., Hebel J. R. (2009). Nursing home resident outcomes from the Res-Care intervention. Journal of the American Geriatrics Society, 57, 1156–1165. doi:10.1111/j.1532-5415.2009.02327.x [DOI] [PubMed] [Google Scholar]
- Resnick B., Petzer-Aboff I., Galik E., Russ K., Cayo J., Simpson M., Zimmerman S. (2008). Barriers and benefits to implementing a restorative care intervention in nursing homes. Journal of the American Medical Directors Association, 9, 102–108. doi:10.1016/j.jamda.2007.08.011 [DOI] [PubMed] [Google Scholar]
- Resnick B., Simpson M., Bercovitz A., Galik E., Gruber-Baldini A., Zimmerman S., Magaziner J. (2006). Pilot testing of the restorative care intervention: Impact on residents. Journal of Gerontological Nursing, 32, 39–47. [DOI] [PubMed] [Google Scholar]
- Sakari-Rantala R., Era P., Rantanen T., Heikkinen E. (1998). Associations of sensory-motor functions with poor mobility in 75- and 80-year-old people. Scandinavian Journal of Rehabilitation Medicine, 30, 121–127. doi:10.1080/003655098444237 [DOI] [PubMed] [Google Scholar]
- Shin J. H., Scherer Y. (2009). Advantages and disadvantages of using MDS data in nursing research. Journal of Gerontological Nursing, 35, 7–17. doi:10.3928/00989134-20090101-09 [DOI] [PubMed] [Google Scholar]
- Snowden M., McCormick W., Russo J., Srebnik D., Comtois K., Bowen J., … Larson E. B. (1999). Validity and responsiveness of the Minimum Data Set. Journal of the American Geriatrics Society, 47, 1000–1004. [DOI] [PubMed] [Google Scholar]
- Vahakangas P., Noro A., Bjorkgren M. (2006). Provision of rehabilitation nursing in long-term care facilities. Journal of Advanced Nursing, 55, 29–35. doi:10.1111/j.1365-2648.2006.03885.x [DOI] [PubMed] [Google Scholar]
- Wang J., Kane R. L., Eberly L. E., Virnig B. A., Chang L. H. (2009). The effects of resident and nursing home characteristics on activities of daily living. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 64, 473–480. doi:10.1093/gerona/gln040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams B. C., Li Y., Fries B. E., Warren R. L. (1997). Predicting patient scores between the functional independence measure and the Minimum Data Set: Development and performance of a FIM-MDS “crosswalk”. Archives of Physical Medicine & Rehabilitation, 78, 48–54. doi:10.1016/s0003-9993(97)90009-5 [DOI] [PubMed] [Google Scholar]
- Wu N., Mor V., Roy J. (2009). Resident, nursing home, and state factors affecting the reliability of Minimum Data Set quality measures. American Journal of Medical Quality, 24, 229–240. doi:10.1177/1062860609332510 [DOI] [PubMed] [Google Scholar]