Abstract
BACKGROUND & AIMS
Economic factors might affect the use of recommended preventative services. We sought to determine whether the recent, severe economic recession was associated with diminished screening colonoscopy rates among an insured population and to assess the relationship between out-of-pocket (OOP) costs and screening colonoscopy use.
METHODS
Administrative data from 106 health plans (LifeLink™ Health Plan Claims Database) were analyzed to determine monthly rates of screening colonoscopies performed on 50–64 year old beneficiaries between January 2005 and November 2007 (pre-recession), as well as December 2007 through June 2009 (recession). Segmented regression models were used to evaluate changes in screening colonoscopy rates, as well as the relationship between screening and OOP costs before and during the recession.
RESULTS
Compared to pre-recession trends, during the recession screening colonoscopy rates decreased by 68.9 colonoscopies/1,000,000 individuals per month (95% confidence interval, decreased of 84.6–53.1; P<.001). Application of study estimates to the entire US population indicated that during the recession, commercially insured, 50–64 year olds underwent approximately 500,000 fewer screening colonoscopies. Compared to those with low OOP costs, those with high OOP procedure costs had lower rates of screening before and during the recession, and had a greater reduction in screening rates during the recession (P=.035).
CONCLUSIONS
During the recession of December 2007–June 2009, insured individuals reduced their use of screening colonoscopy, compared with the 2 years before the recession began. OOP costs were inversely related to screening use, especially during the recession. Policies to reduce cost sharing could increase adherence to recommended preventive services such as colonoscopy examinations.
Keywords: colon cancer, CRC, prevention, healthcare spending
BACKGROUND
The recent U.S. economic recession was the longest and most severe since World War II.1 During this period, personal health care expenditures2 grew at the slowest rate in almost 50 years.3, 4 Data from surveys5–7 and financial statements8, 9 indirectly suggest that during the recession Americans used less health care. If true, cut-backs were most likely among the five million non-elderly Americans who lost their health insurance.10 However, in the face of falling household incomes11 and rising economic insecurity,12 the majority of Americans who remained continuously insured may have also curtailed their use of health care, especially costly, elective services.5
Colorectal cancer screening is recommended for all adults 50 years or older.13, 14 Colonoscopy is the most popular screening option.15 However, many patients referred for colonoscopy fail to undergo the procedure,16, 17 in part because of high direct out-of-pocket (OOP) costs (e.g., co-payment and co-insurance).18 During tough economic times these costs may become unaffordable and further limit adherence to screening recommendations. Down the line, this may increase health care costs19 and the proportion of individuals diagnosed with late stage colorectal cancer.20
We sought to determine whether rates of screening colonoscopies in an insured population fell during the economic recession. Additionally, we assessed whether changes in utilization rates were associated with patient cost sharing. We hypothesized that during the recession screening rates dropped, especially among those with high direct OOP costs.
METHODS
Study design and population
We conducted a time-series analysis using health insurance claims data within the LifeLink™ Health Plan Claims database (formerly Pharmetrics). The database contains fully adjudicated medical and pharmaceutical claims from approximately 100 health plans across the US and has been reported to be nationally representative of the commercially insured U.S. population.21 The study sample selected consisted of a 10% random sample of all persons in the database with at least 6 months of continuous health plan enrollment. For each month between January, 2005 and June, 2009, we assembled the sample of actively enrolled 50 to 64 years old beneficiaries.
Identification of screening colonoscopies
Colonoscopy is performed for colorectal cancer screening (i.e., asymptomatic individuals without precancerous lesions), colorectal cancer surveillance (i.e., asymptomatic individuals with a history of prior removal of a pre-cancerous lesion),22 and diagnostic purposes (e.g., diarrhea or hematochezia). Algorithms that use administrative claims data to distinguish between these types of colonoscopies have been developed in a health maintenance organization population (Haque et al),23 as well as the Veterans Affairs System (El Serag et al24, subsequently modified by Fisher et al.25). However, these algorithms were not developed for use in commercially insured populations (such as the one in this study) and often misclassify screening and diagnostic procedures.26 This likely stems from the fact that the Haque algorithm, which only includes two colonoscopy Current Procedural Terminology (CPT) codes, does not identify enough colonoscopies, while the Fisher algorithm, which includes over 30 International Classification of Diseases (ICD-9) diagnosis codes, classifies too many colonoscopies as diagnostic. Therefore, we identified patients in the above source population who underwent a screening colonoscopy each month as any beneficiary with at least one inclusionary CPT code from Fisher’s algorithm (Step 1) and without any exclusionary ICD-9 codes from Haque’s algorithm (Steps 2–4) [Appendix 1]. This screening algorithm maximized sensitivity of identifying screening procedures, and optimized statistical power and precision, at the expense of lower specificity. We also performed confirmatory analyses using screening colonoscopies identified with the Haque and Fisher algorithms.
Screening colonoscopy rates before and during the recession
A segmented regression model27 was employed to compare trends in the monthly rate of screening colonoscopy utilization (per 1,000,000 eligible beneficiaries) prior to the economic recession (January, 2005 to November, 2007) to monthly rates during the economic recession (December, 2007 to June, 2009). These time periods were defined by the National Bureau of Economic Research,28 the nation’s leading nonprofit economic research organization and official arbiter for dating recessions. Segmented regression may be used to capture changes in both the trend of screenings as well as discontinuity in the use of screenings resulting from the recession. We hypothesized a priori that there would not be an abrupt decline in screenings given the recession’s gradual onset and therefore chose to only model changes in the trend of screenings before and during the recession. The specific time-series model used was:
Y = β0 + β1*Time (month) + β2*Time in Recession(month) + ε
where Y is the monthly rate of colonoscopy screening, Time is a continuous variable indicating time in months for the entire study period from January, 2005 (Time = 1) to June, 2009 (Time = 54). Time in Recession is a continuous variable counting the number of months during the recession from December, 2007 (Time in Recession = 1) to June, 2009 (Time in Recession = 19) and is coded 0 for the months before the recession. In the model, β0 estimates the screening rate at the baseline (January, 2005), β1 estimates the trend of screening rates in pre-recession period (January 2005 to November 2007), β2 estimates the change of the trend of screening rates moving from the pre-recession period to the recession period (December, 2007 through June, 2009), and β1 + β2 estimates the trend of screening rates in the recession period (December, 2007 through June, 2009).
Rates of alternative colorectal cancer screening tests before and during the recession
In addition to colonoscopy, the US Preventive Services Task force also recommends fecal occult blood testing (FOBT) and sigmoidoscopy as options for colorectal cancer screening.17 We used CPT codes to identify FOBT (82270, 82271, and 82272) and flexible sigmoidoscopy (45330, 45331, 45333, 45335, 45338, 45339, G0104) and then calculated monthly rates of these procedures (per 1,000,000 eligible beneficiaries) for each month throughout the study period (January, 2005 through June, 2009).
Screening colonoscopy rates stratified by out-of-pocket costs before and during the recession
In addition to examining the effect of the recession on overall screening colonoscopy trends, we also examined whether these trends differed based on direct OOP costs. We hypothesized that if screening rates declined during the recession, the steepest drop would be observed among those with the highest OOP costs. For subjects who underwent screening colonoscopy, we defined direct OOP costs as the costs a plan contractually allowed for minus the amount the plan itself actually paid. We considered all same-day medical costs, except dispensing of prescription drugs, as colonoscopy related. Based on an assumption that median OOP procedure costs for each plan would, on average, apply to all individuals in that plan, we stratified each plan into a low OOP cost group (less than or equal to $50), average OOP cost group (between $51–$299), and high OOP cost group ($300 and higher) determined over each six month period (January to June, and July to December for each year). Plans with fewer than 20 than colonoscopies were excluded to increase the precision of the cost estimates. These OOP cost cut-offs were determined a priori using the distribution of OOP costs across plans (roughly 1/3rd of the population was assigned to each cost group). Of note, it was possible for a plan to move from one OOP cost strata to another each six month period. Using these data, we created segmented regression models to compare the utilization rate among the three OOP cost strata:
Y = β0low* OOPlow + β1low* OOPow *Time (month) + β2low* OOPlow *Time in Recession(month) + β0avg*OOPavg+ β1avg* OOPavg *Time (month) + β2avg* OOPavg *Time in Recession(month) + β0high*OOPhigh+ β1high* OOPhigh *Time (month) + β2high* OOPhigh *Time in Recession(month) + ε
where OOPlow is the indicator variable representing plans with low median direct OOP costs, OOPavg is for plans with average direct OOP costs, and OOPhigh is for plans with high direct OOP costs. Similar to model 1 above, β0low, β0avg, and β0high estimate the screening rate at baseline (January 2005) for three sub-groups respectively. β1low, β1avg, and β1high estimate the coefficients for the trend of colonoscopies from January 2005 (Time = 1) to June 2009 (Time = 54), while β2low, β2avg, and β2high estimate the change of the trend for each sub-group resulting from the recession from December 2007 (Time in Recession = 1) to June, 2009 (Time in Recession = 19) for beneficiaries in low, medium, and high generosity plans respectively. Finally, the slope change of the high and low OOP plans were compared to assess whether the drop in screening rates was greater among those in the high OOP sub-group compared to those in the low OOP sub-group [( β2low) – ( β2high)].
Out-of-pocket costs of screening colonoscopy before and during the recession
We also posited that falling direct OOP costs during the recession would suggest that those with higher direct OOP costs were preferentially forgoing screening colonoscopy, irrespective of their specific health plan. Accordingly, we calculated and compared median direct OOP costs for the procedure before and during the recession using non-parametric two-sample t-tests. We also used segmented regression to assess the trends in median OOP costs before and during the recession.
For all segmented regression models, we explored the possibility of autocorrelation and seasonal trends to improve model fit. We noted the presence of a significant yearly auto-correlation in the disturbances of time points being 12 months apart and therefore used auto-regressive integrative moving average (ARIMA) to correct for it. We employed robust standard errors in these models to correct for heteroskedasticity and improve the precision of our parameter estimation. SAS® (version 9.1.3, Cary NC) was used to extract the study sample from the claims database. Stata® (version 9, College Station TX) was used to conduct the segmented regression analysis. Our study was exempted from review by the University of North Carolina Institutional Review Board.
RESULTS
Screening colonoscopy utilization before and during the recession
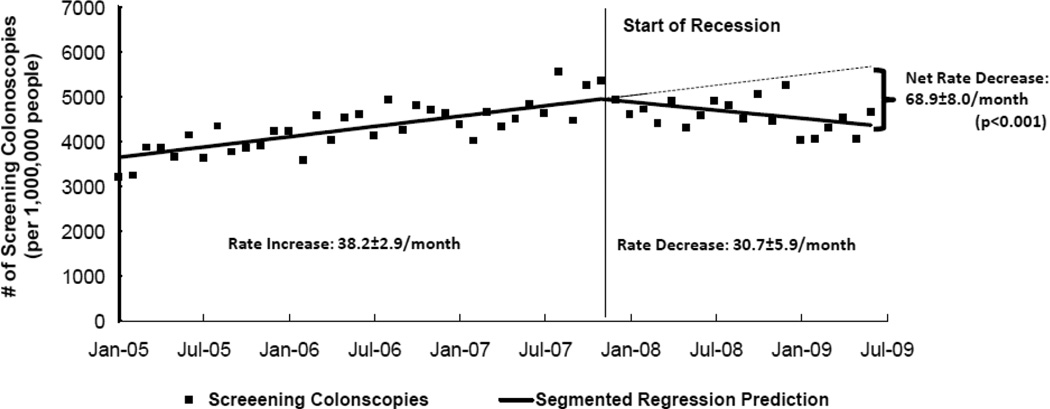
The screening algorithm identified 86,644 individuals who underwent screening colonoscopies (49.7% of 174,312 individuals with at least one colonoscopy CPT code, a very similar proportion to what has been previously reported29, 30) (Appendix Figure A). As predicted, the rates of screening colonoscopy increased before and then decreased during the recession. Prior to the recession screening colonoscopy use increased at a rate of 38.2 (95% Confidence Interval: 32.4, 43.9) more colonoscopies per 1,000,000 insured individuals per month. Conversely, during the recession screening colonoscopy use declined at a rate of 30.7 (− 42.2, −19.1) fewer colonoscopies per 1,000,000 insured individuals per month. In sum, compared to what would have been expected based on pre-recession trends, during the recession screening colonoscopy use declined at a rate of 68.9 (−84.6, −53.1) fewer colonoscopies per 1,000,000 insured individuals per month (p<0.001) (Figure 1; also see Appendix Table 1). The results based on analyses of colonoscopies identified using the other two algorithms were both in the same direction, of similar magnitude, and statistically significant (Appendix Table 1 and Figure 1).
Figure 1. Screening Colonoscopy Utilization among Insurance Beneficiaries Before and During the Economic Recession.
*p-value for test of trend change between pre-recession to recession periods.
Black boxes represent rates of screening colonoscopy each month. Solid lines represents rate predicted by segmented regression models before and during the economic recession. Broken line represents recession era rates that would have been expected based on projections of pre-recession trends. Numerical data displayed in Appendix 2, Table 1. Data source: LifeLink™ Health Plan Claims Database (January, 2005 through June, 2009)
Rates of alternative colorectal cancer screening tests before and during the recession
Rates of FOBT and sigmoidoscopy declined both before and during the economic recession. Between the first and last months of the study, rates of FOBT declined by 34% and sigmoidoscopy by 61%.
Screening rates stratified by out-of-pocket costs before and during the recession
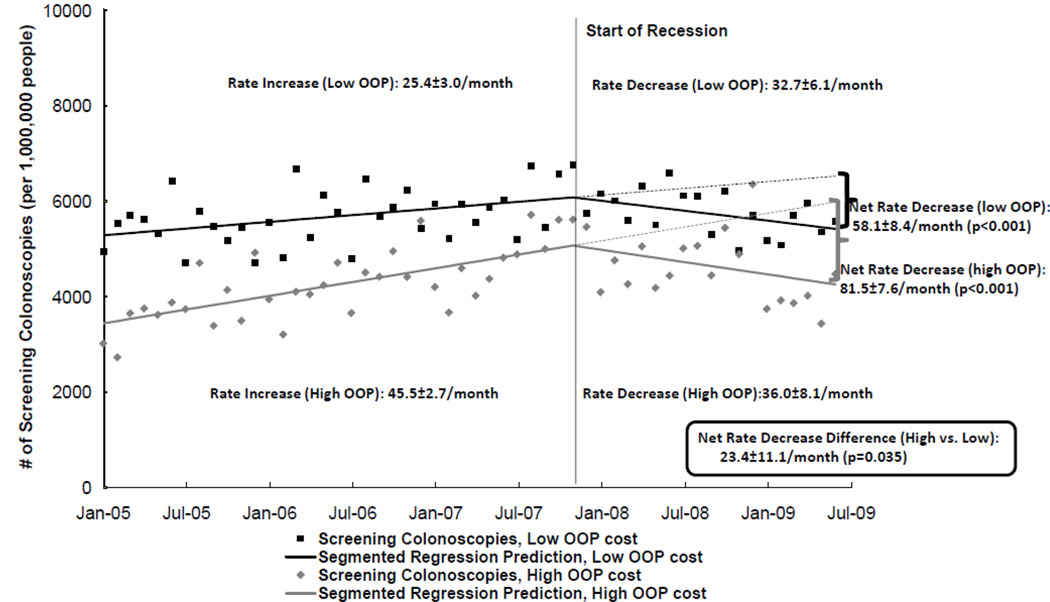
Also as predicted, screening rates were lower among beneficiaries of health plans with high direct OOP costs throughout all time periods. Furthermore, during the recession screening rate trends declined most among members of high OOP cost plans (Figure 2; also see Appendix Table 2). Based on the pre-recession trends, during the recession screening colonoscopy use declined at a rate of 58.1 (−74.5, −41.6) fewer colonoscopies than expected / 1,000,000 insured individuals with low out-of-pocket costs (≤ $50) per month, compared with a rate of 81.5 (−96.3, −66.7) fewer colonoscopies than expected / 1,000,000 insured individuals with high out-of-pocket costs (≥ $300) per month (p=0.035). The results based on analyses of colonoscopies identified using the other two algorithms were in the same direction, though statistically significant for the Haque (p=0.048) but not Fisher (p=0.65) algorithm (Appendix Figure 2 and Table 2).
Figure 2. Screening Colonoscopy Utilization Among Insurance Beneficiaries of Plans with High (≥$300) and Low (≤$50) Out-of-pocket (OOP) Costs Before and During the Recession.
Black boxes represent rates of screening colonoscopy each month and solid black line represents screening colonoscopy rates predicted by segmented regression models before and during the economic recession among members of plans with low OOP costs. Gray diamonds represent rates of screening colonoscopy each month and solid gray line represents screening colonoscopy rates predicted by segmented regression models before and during the economic recession among members of plans with high OOP costs. Broken line represents recession era rates that would have been expected based on projections of pre-recession trends. Net decrease represents the difference between these recession-era predicted rates and observed rates. P-value for test of trend change from pre-recession to recession period between plans with high OOP costs and low OOP costs. Numerical data displayed in Appendix 2, Table 2. Data source: LifeLink™ Health Plan Claims Database (January, 2005 through June, 2009)
Out-of-pocket costs before and during the recession
Median direct OOP costs incurred for screening colonoscopy before the recession were significantly higher than those during the recession ($145 vs. $127, p<0.001). Median OOP costs increased at a rate of $5.52 ($0.48, $10.56) per year prior to the recession, and then decreased at a rate of $33.84 (−$53.4, −$23.04) per year during the recession (p<0.001) (Figure 3 and Appendix Table 3). The results based on analyses of colonoscopies identified using the other two algorithms were both in the same direction and statistically significant (Appendix Figure 3 and Table 3).
Figure 3. Median Out-of-Pocket (OOP) Costs for Screening Colonoscopy.
Black boxes represent the median out-of-pocket (OOP) cost incurred for all colonoscopies performed each month. Solid lines represent median cost predicted by segmented regression models before and during the economic recession. Broken line represents what the expected recession-era OOP costs would have been based on projection of pre-recession trends. Net decrease represents the difference between median costs during the recession that would have been expected based on pre-recession trends and the median costs that were actually observed. p-value is for test of trend change between pre-recession to recession periods. Numerical data displayed in Appendix 2, Table 3.
Data source: LifeLink™ Health Plan Claims Database (January, 2005 through June, 2009)
DISCUSSION
During the recent economic recession insured 50 – 64 year old Americans reduced their use of screening colonoscopy. Applying the decreased utilization documented here to the 39.5 million commercially insured, 50–64 year old Americans,31 over the entire 19 month recession period this would have resulted in 516,309 (95% CI: 456,360, 576,258) fewer colonoscopies than what would have been expected based on pre-recession trends. Screening rates fell most among individuals with high direct OOP costs for the procedure. These findings reflect the intimate link between socioeconomic factors and health care use;32 when faced with economic insecurity, asymptomatic individuals may be unable to afford screening colonoscopy, or may perceive it to be less important than competing demands for their more limited resources.
Because colonoscopy is a cost-effective19, 33 screening modality recommend by multiple governmental agencies17 and professional societies,13 reduced screening rates during the recession -- which were undoubtedly even more extreme among those who lost their health insurance34 and were not met by a commensurate rise in FOBT nor sigmoidoscopy utilization-- may ultimately increase health care costs and result in cancer related deaths. This is consistent with literature in other fields of medicine. For instance, during difficult economic times women are more likely to be diagnosed with advanced rather than local breast cancer.35, 36 Similarly, over one-half of family physicians surveyed in May, 2009 reported seeing more health problems caused by their patients forgoing needed preventive care.6
Those with high OOP procedure costs had lower screening rates over time, and experienced a greater drop in screening rates during the recession. While factors aside from OOP costs may have affected the decision to undergo screening colonoscopy during the recession, our findings add to the growing body of literature suggesting that cost-sharing is a disincentive for preventive services.37, 38 For example, when a group of employees were compelled to switch to a high-deductible health plan (an extreme form of cost sharing) they significantly reduced their use of screening colonoscopy.39, 40 Likewise, requiring women to pay a mere $10 to $20 copayment makes them 8% less likely to undergo mammography.41 In our study, those individuals in health plans with high direct OOP costs for colonoscopy were less likely to undergo the procedure throughout the entire study period, and during the recession this tendency was accentuated. Taken together, these studies argue for strategies to reduce patient cost sharing for colorectal cancer screening. Recently, the Patient Protection and Affordable Care Act eliminated Medicare and Medicaid copayments and deductible requirements for all preventive services recommended by the United States Preventive Services Task Force, including screening colonoscopy.42 Commercial insurers may follow suit by offering value based insurance designs that promote high value services through financial incentives, such as reduced copayments.43
The study had several potential limitations related to the use of administrative data. First, algorithms for distinguishing screening from surveillance and diagnostic colonoscopy are not exact and none have been assessed in a commercially insured popualtion.26 We are reassured that the proportion of colonoscopies our algorithm classified as screening (approximately one-half) was nearly identical to those reported in two other national studies that used medical records and practice surveys to classify colonoscopies.29, 30 Additionally, we performed confirmatory analyses using two other classification algorithms. In all these analyses, the direction and magnitude of the results were consistently similar. Finally, any misclassification (i.e., considering a diagnostic colonoscopy as screening and vice versa) would be non-differential with respect to time and should therefore bias the results towards the null.44 A second limitation is that we relied on median OOP costs at the health plan level as a surrogate for OOP costs at the individual level. However, we also demonstrated that median direct OOP costs at the individual level irrespective of health plan increased before and decreased during the recession, further suggesting that during the recession those with high direct OOP costs were preferentially less likely to have undergone screening. Third, other factors such as socioeconomic status may have affected the associations between the economic recession, cost-sharing, and screening colonoscopy utilization. However, lower income Americans tend to belong to health plans with less cost-sharing,45 so it would be expected that any confounding by socioeconomic status would bias our study’s results to the null. Fourth, it is possible that non-economic factors such as a change in the proportion of individuals due for colon cancer screening, increased use of computed tomographic colonography (CTC) use, and other secular trends may have reduced screening colonoscopy utilization during the recession. With regards to CTC, the growth of this screening modality has been generally slow. In 2005, 13% of hospitals offered CTC; by the end of 2008, this proportion only increased to 17%.46 Even at the select hospitals that offer this test, the use of CTC likely pales in comparison to use of conventional (optical) colonoscopy, in part because screening CTC is not covered by most commercial insurers.47 Finally, while the study population was representative of the commercially insured U.S. population, it is unclear if these data generalize to the Medicare population. For this reason, we conservatively extrapolated these data only to insured Americans between the ages of 50 and 64 years old.
In summary, during the recent economic recession rates of screening colonoscopy decreased among insured Americans. Members of health plans with high colonoscopy OOP costs were less likely to undergo colonoscopy at all time points, and this differential utilization worsened during the recession. Thus, policies to reduce patient cost sharing for colonoscopy and other recommended, cost-effective preventive services should be considered.
Supplementary Material
Acknowledgments
Grant Support: This research was supported, in part, by grants from the National Institutes of Health (K12HS019468 (SDD), P30 DK034987 (RSS)) and a career development award from the Crohn’s and Colitis Foundation of America (MDK).
Abbreviations
- CPT
Current Procedural Terminology
- CTC
computed tomographic colonography
- ICD-9
International Classification of Diseases-9
- OOP
out-of-pocket.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial disclosures/Conflicts of interest: none
Note: The statements, findings, conclusions, views and opinions contained and expressed in this article are based in part on data obtained under license from the following IMS Health Incorporated information service: LifeLink™ Health Plan Claims Database (January, 2005 through June, 2009), IMS Health Incorporated. All Rights Reserved. The statements, findings, conclusions, views, and opinions contained and expressed herein are not necessarily those of IMS Health Incorporated or any of its affiliated or subsidiary entities.
David Wei and Michael Kappelman had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Author Contribution:
Study concept: SDD, MDK
Study design: SDD, DW, JFF, NDS, NJS, RSS, MDK
Data analysis: DW, SDD, MDK
Manuscript preparation: SDD, MDK
Manuscript review: DW, JF, NDD, NJS, RSS
REFERENCES
- 1.Temin P. The Great Recession and The Great Depression. NBER Working Paper No. 15645. 2010
- 2.Centers for Medicare and Medicaid Services. National Health Expenditures Accounts: Definitions, Sources, and Methods. 2009
- 3.Hartman M, Martin A, Nuccio O, Catlin A. Health spending growth at a historic low in 2008. Health Aff (Millwood) 2010;29:147–155. doi: 10.1377/hlthaff.2009.0839. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Medicare and Medicaid Services. [Accessed March 1, 2011];Growth in persional health care expenditures and percent distribution of factors affecting growth: United States, 1960–2008. 2010 from http://www.cdc.gov/nchs/data/hus/2010/124.pdf.
- 5.Lusardi A, Schneider DJ, Tuftano P. NBER Working Paper No. 15843. 2010. The economic crisis and medical care usage. [Google Scholar]
- 6.American Academy of Family Practice. Patient Care during the 2008–2009 Recesssion - Online Survey Executive Summary. 2009 [Google Scholar]
- 7.American Hospital Association. [Accessed on October 10, 2010];The Economic Crisis: The Toll on the Patints and the Communities Hospitals Serve. 2009 from http://www.aha.org/aha/content/2009/pdf/090427econcrisisreport.pdf&embedded=true&chrome=true.
- 8.Johnson A, Rockoff JD, Wilde Matthews A. Americans Cut Back on Visits to Doctor. Wall Street Journal. 2010 Jul 29; [Google Scholar]
- 9.Goldman E. Specialists Are Feeling the Recession's Pinch. Internal Medicine News. 2009 Nov 15; [Google Scholar]
- 10.Holahan J. The 2007-09 recession and health insurance coverage. Health Aff (Millwood) 2010;30:145–152. doi: 10.1377/hlthaff.2010.1003. [DOI] [PubMed] [Google Scholar]
- 11.DeNavas-Walt C, Proctor BD, Smith JCUS. Census Bureau, Current Population Reports, P60-238, Income, Poverty, and Health Insurance Coverage in the United States, 2009. Washington, DC: U.S. Government Printing Office; 2010. [Google Scholar]
- 12.Hacker JS, Rehm P, Schlesinger M. Standing on Shaky Ground: Americans' Experiences with Economic Insecurity: Economic Security Index. 2010 [Google Scholar]
- 13.Levin B, Lieberman DA, McFarland B, Andrews KS, Brooks D, Bond J, Dash C, Giardiello FM, Glick S, Johnson D, Johnson CD, Levin TR, Pickhardt PJ, Rex DK, Smith RA, Thorson A, Winawer SJ. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008;134:1570–1595. doi: 10.1053/j.gastro.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 14.Whitlock EP, Lin JS, Liles E, Beil TL, Fu R. Screening for colorectal cancer: a targeted, updated systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2008;149:638–658. doi: 10.7326/0003-4819-149-9-200811040-00245. [DOI] [PubMed] [Google Scholar]
- 15.Klabunde CN, Lanier D, Nadel MR, McLeod C, Yuan G, Vernon SW. Colorectal cancer screening by primary care physicians: recommendations and practices, 2006–2007. Am J Prev Med. 2009;37:8–16. doi: 10.1016/j.amepre.2009.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Denberg TD, Melhado TV, Coombes JM, Beaty BL, Berman K, Byers TE, Marcus AC, Steiner JF, Ahnen DJ. Predictors of nonadherence to screening colonoscopy. J Gen Intern Med. 2005;20:989–995. doi: 10.1111/j.1525-1497.2005.00164.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.U.S. Preventive Services Task Force. AHRQ Publication 08-05124-EF-3. Rockville, MD: Agency for Healthcare Research and Quality; 2008. Oct, Screening for Colorectal Cancer: U.S. Preventive Services Task Force Recommendation Statement. [Google Scholar]
- 18.Pignone M. Patient preferences for colon cancer screening: the role of out-of-pocket costs. Am J Manag Care. 2007;13:390–391. [PubMed] [Google Scholar]
- 19.Pignone M, Saha S, Hoerger T, Mandelblatt J. Cost-effectiveness analyses of colorectal cancer screening: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;137:96–104. doi: 10.7326/0003-4819-137-2-200207160-00007. [DOI] [PubMed] [Google Scholar]
- 20.Gross CP, Andersen MS, Krumholz HM, McAvay GJ, Proctor D, Tinetti ME. Relation between Medicare screening reimbursement and stage at diagnosis for older patients with colon cancer. Jama. 2006;296:2815. doi: 10.1001/jama.296.23.2815. [DOI] [PubMed] [Google Scholar]
- 21.Stempel DA, Mauskopf J, McLaughlin T, Yazdani C, Stanford RH. Comparison of asthma costs in patients starting fluticasone propionate compared to patients starting montelukast. Respir Med. 2001;95:227–234. doi: 10.1053/rmed.2000.1027. [DOI] [PubMed] [Google Scholar]
- 22.Mysliwiec PA, Brown ML, Klabunde CN, Ransohoff DF. Are physicians doing too much colonoscopy? A national survey of colorectal surveillance after polypectomy. Ann Intern Med. 2004;141:264–271. doi: 10.7326/0003-4819-141-4-200408170-00006. [DOI] [PubMed] [Google Scholar]
- 23.Haque R, Chiu V, Mehta KR, Geiger AM. An automated data algorithm to distinguish screening and diagnostic colorectal cancer endoscopy exams. J Natl Cancer Inst Monogr. 2005:116–118. doi: 10.1093/jncimonographs/lgi049. [DOI] [PubMed] [Google Scholar]
- 24.El-Serag HB, Petersen L, Hampel H, Richardson P, Cooper G. The use of screening colonoscopy for patients cared for by the Department of Veterans Affairs. Arch Intern Med. 2006;166:2202–2208. doi: 10.1001/archinte.166.20.2202. [DOI] [PubMed] [Google Scholar]
- 25.Fisher DA, Grubber JM, Castor JM, Coffman CJ. Ascertainment of colonoscopy indication using administrative data. Dig Dis Sci. 2010;55:1721–1725. doi: 10.1007/s10620-010-1200-y. [DOI] [PubMed] [Google Scholar]
- 26.Holden DJ, Harris R, Poterfield DS, Jonas DE, Morgan LC, Reuland D, Gilchrist M, Viswanthan M, Lohr KN, Lyda-McDonald B. AHRQ Publication No. 10-E-002. Rockville, MD: Agency for Healthcare Research and Quality; 2010. Feb, Enhancing the Use and Quality of Colorectal Cancer Screening. Evidence Report/Technology Assessment No. 190. [PMC free article] [PubMed] [Google Scholar]
- 27.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin.Pharm.Ther. 2002;27:299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- 28.National Bureau of Economic Research. [Accessed October 20, 2010];Business Cycle Dating Committee, National Bureau of Economic Research. 2010 from http://www.nber.org/cycles/sept2010.html.
- 29.Seeff LC, Richards TB, Shapiro JA, Nadel MR, Manninen DL, Given LS, Dong FB, Winges LD, McKenna MT. How many endoscopies are performed for colorectal cancer screening? Results from CDC's survey of endoscopic capacity. Gastroenterology. 2004;127:1670–1677. doi: 10.1053/j.gastro.2004.09.051. [DOI] [PubMed] [Google Scholar]
- 30.Lieberman DA, Faigel DO, Logan JR, Mattek N, Holub J, Eisen G, Morris C, Smith R, Nadel M. Assessment of the quality of colonoscopy reports: results from a multicenter consortium. Gastrointest Endosc. 2009;69:645–653. doi: 10.1016/j.gie.2008.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smolka G, Purvis L, Figueiredo C. Health Coverage among 50- to 65-Year-Olds. Data Digest #155. Washington, DC: AARP Public Policy Institute; 2007. [Google Scholar]
- 32.Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Annu Rev Sociol. 1995;21:349–386. [Google Scholar]
- 33.Song K, Fendrick AM, Ladabaum U. Fecal DNA testing compared with conventional colorectal cancer screening methods: a decision analysis. Gastroenterology. 2004;126:1270–1279. doi: 10.1053/j.gastro.2004.02.016. [DOI] [PubMed] [Google Scholar]
- 34.Robinson JM, Shavers V. The role of health insurance coverage in cancer screening utilization. J Health Care Poor Underserved. 2008;19:842–856. doi: 10.1353/hpu.0.0048. [DOI] [PubMed] [Google Scholar]
- 35.Catalano RA, Satariano WA, Ciemins EL. Unemployment and the detection of early stage breast tumors among African Americans and non-Hispanic whites. Ann Epidemiol. 2003;13:8–15. doi: 10.1016/s1047-2797(02)00273-9. [DOI] [PubMed] [Google Scholar]
- 36.Catalano RA, Satariano WA. Unemployment and the likelihood of detecting early-stage breast cancer. Am J Public Health. 1998;88:586–589. doi: 10.2105/ajph.88.4.586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rice T, Morrison KR. Patient cost sharing for medical services: a review of the literature and implications for health care reform. Med Care Rev. 1994;51:235–287. doi: 10.1177/107755879405100302. [DOI] [PubMed] [Google Scholar]
- 38.Solanki G, Schauffler HH. Cost-sharing and the utilization of clinical preventive services. Am J Prev Med. 1999;17:127–133. doi: 10.1016/s0749-3797(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 39.Wharam JF, Galbraith AA, Kleinman KP, Soumerai SB, Ross-Degnan D, Landon BE. Cancer screening before and after switching to a high-deductible health plan. Ann Intern Med. 2008;148:647–655. doi: 10.7326/0003-4819-148-9-200805060-00004. [DOI] [PubMed] [Google Scholar]
- 40.Wharam JF, Graves AJ, Landon BE, Zhang F, Soumerai SB, Ross-Degnan D. Two-year Trends in Colorectal Cancer Screening After Switch to a High-deductible Health Plan. Med Care. 2011;49:865–871. doi: 10.1097/MLR.0b013e31821b35d8. [DOI] [PubMed] [Google Scholar]
- 41.Trivedi AN, Rakowski W, Ayanian JZ. Effect of cost sharing on screening mammography in Medicare health plans. N Engl J Med. 2008;358:375–383. doi: 10.1056/NEJMsa070929. [DOI] [PubMed] [Google Scholar]
- 42.H.R. 3590--111th Congress: Patient Protection and Affordable Care Act. 2009 [Google Scholar]
- 43.Chernew ME, Rosen AB, Fendrick AM. Value-based insurance design. Health Aff (Millwood) 2007;26:w195–w203. doi: 10.1377/hlthaff.26.2.w195. [DOI] [PubMed] [Google Scholar]
- 44.Hennekens CH, Burning JE. Epidemiology in Medicine. Lipincott Williams & Wilkins; 1987. [Google Scholar]
- 45.Baicker K, Goldman D. Patient cost-sharing and healthcare spending growth. J Econ Perspect. 2011;25:47–68. doi: 10.1257/jep.25.2.47. [DOI] [PubMed] [Google Scholar]
- 46.McHugh M, Osei-Anto A, Klabunde CN, Galen BA. Adoption of CT Colonography by US Hospitals. J Am Coll Radiol. 2011;8:169–174. doi: 10.1016/j.jacr.2010.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McFarland EG, Keysor KJ, Vining DJ. Virtual Colonoscopy: From Concept to Implementation. In: Dachman AH, Laghi A, editors. Atlas of Virtual Colonoscopy. 2nd ed. Springer; 2011. pp. 3–7. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.