Abstract
Cancer treatment with traditional Chinese medicine (TCM) has a long history. Heritage provides general conditions for the innovation and development of TCM in oncology. This article reviews the development of TCM in oncology, interprets the position and function of TCM for cancer prevention and treatment, summarizes the innovations of TCM in oncology over nearly fifty years, and suggests the development direction.
Keywords: Cancer, development, history, present situation, traditional Chinese medicine
Introduction
Cancer treatment with traditional Chinese medicine (TCM) has a long history. Discussions of cancer appeared in classical works, such as The Yellow Emperor’s Inner Canon and The Classic of Medical Problems, more than 2000 years ago. Concepts of diagnosis and treatment, such as strengthening body resistance and eliminating pathogens, treating both the manifestation and root cause, treating the same disease with different methods, and treating different diseases with the same methods, have been proven by clinical practice. These concepts have become characteristics and advantages of TCM for cancer prevention and treatment, as demonstrated by modern technology and methods. Heritage has laid the foundation for the innovation and development of cancer treatment with TCM, attracting more and more international attention and cooperation.
History of cancer treatment with traditional Chinese medicine (TCM)
Cancer treatment with TCM remains the most ancient living tradition; the word “tumor” was discovered on 3500-year-old oracle bone inscriptions. The wholism of interconnection and mutual restraint inside the human body, and the concept of treatment according to syndrome differentiation have been reflected in the cognition of cancer etiology and the principles of diagnosis and treatment with TCM.
The diagnosis and treatment of tumors was discussed in the literature of ancient Chinese medicine, where there is a wealth of content. Apart from descriptions of symptoms, prognosis, and differential diagnosis, we can also find summaries of cancer pathogenesis and treatment strategy, revealing that our ancestors recognized that cancer etiology involved exopathogens, environment, emotional maladjustment, and improper diet: “With discomfort, improper diet, cold temperature from time to time, pathogens prevail and accumulation has left” (The Yellow Emperor’s Inner Canon, English translation).1 Chinese ancestors emphasized that cancer stemmed from an endogenous cause: “The form of ulcer is sore, swollen, all because of the cumulative toxicity of five viscera and six bowels, not exclusively for RongWei congestion” (The Central Treasury Canon, English translation), and that the tumor is a partial consequence of systemic disease.2 These theories represent the formulation of TCM treatment strategies for cancer: the combination of partial and systemic therapy, strengthening body resistance and eliminating pathogens, treatment of the body, and the regulation of emotion. Treatment methods, such as strengthening body resistance, heat-clearing and detoxifying, activating blood and removing stasis, and softening and resolving hard masses, were also developed from these theories. Indispensable Medical Reading first proposed cancer treatment by different stages: “In the early stage of the disease, the vital qi is strong, the evil qi is light and easily attacked; in the middle stage, the evil qi is deeper, the vital qi becomes weak and should be attacked or benefit; in the end, the evil qi is strong, the vital qi is weaker and should be well benefit.”3
Some ancient classical prescriptions and medicine are still in use today, such as Xiaojin dan, the Xihuang pill, the Dahuangzhechong pill, the Liushen pill, and Pianzaihuang.
Roles of TCM treatment for cancer
After the founding of People’s Republic of China, domestic scholars have carried out scientific research on the use of TCM for the prevention and treatment of cancer, clarifying the different effects of TCM on cancer in different stages. TCM combined with modern medicinal means could improve symptoms, enhance quality of life, prevent recurrence and metastasis, and prolong patients’ survival (Fig 1).
Figure 1.
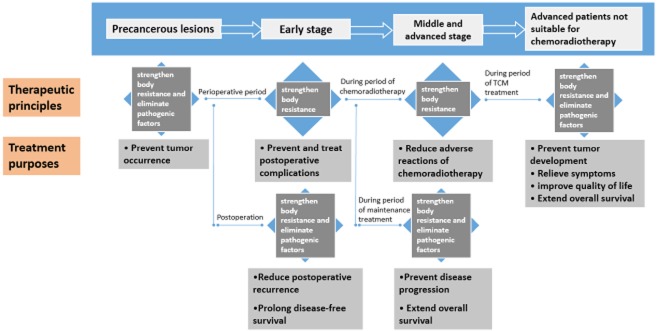
The efficacy of traditional Chinese medicine (TCM) in cancer treatment.
Supporting role of TCM during radiochemotherapy
Radiotherapy and chemotherapy can damage the qi and blood, essence and fluid, and the function of the five viscera and six bowels. Common symptoms include fatigue, apocleisis, nausea, vomiting, and leucocyte decline. Local side effects include stigmata, loss of hair, mucosal erosion, ulcer, edema and hemorrhage. During radiotherapy and chemotherapy, TCM treatment can reduce toxic side effects, such as: myelosuppression, gastrointestinal reactions, hepatic or renal impairment, and skin and mucosa radiation injuries. TCM can improve the clinical efficacy of radiotherapy and chemotherapy, guided by therapeutic principles of tonifying qi and producing blood, strengthening the spleen and stomach, nourishing the liver and kidney, and removing heat from blood and toxic material from the body. TCM combined with chemotherapy has shown a favorable effect in improving efficacy with less adverse reactions. This has been substantiated by the inclusion of TCM into the 6th–11th Five-Year Plans, as well as in meta-analyses by scholars in China and abroad. For instance, McCulloch et al. analyzed 34 randomized studies representing 2815 patients.4 Twelve studies (n = 940 patients) reported a reduced risk of death at 12 months (risk ratio [RR] = 0.67; 95% confidence interval [CI], 0.52 to 0.87); 30 studies (n = 2472) reported improved tumor response data (RR = 1.34; 95% CI, 1.24 to 1.46). McCulloch et al.’s study concluded that Astragalus-based TCM may increase the effectiveness of platinum-based chemotherapy for advanced non-small-cell lung cancer (NSCLC). Gan et al. conducted a meta-analysis involving four randomized controlled trials (RCT), and the results showed that Chinese medicine can decrease white blood cell reduction during chemotherapy in gastric cancer patients of advanced stage.5 Li et al. conducted a meta-analysis summarizing 24 trials, with a total of 2103 advanced NSCLC patients, and showed that TCM as an adjuvant therapy combined with conventional chemotherapy increased the one-year survival rate (RR 1.36, 95% CI 1.15–1.60, P = 0.0003) and immediate tumor response (RR 1.36, 95% CI 1.19–1.56, P < 1.0E-5), reduced chemotherapy toxicity, including nausea, vomiting, and the decline of hemoglobins and platelets, and improved Karnofsky performance status (KPS).6 Another meta-analysis of 20 RCTs, using TCM to treat colorectal cancer versus chemotherapy alone, reported that TCM with chemotherapy significantly increased the one and three-year survival rates (odds ratio [OR] 2.41, 95% CI 1.32–4.41; OR 2.40, 95% CI 1.49–3.87], slowed colorectal cancer progression (OR 0.50, 95% CI 0.32–0.77) and improved quality of life (OR 3.43, 95% CI 2.35–5.02).7 These results were supported by a meta-analysis by Mao et al. aimed at assessing the efficacy of TCM with radiotherapy and/or chemotherapy for patients with nasopharyngeal carcinoma, which included 13 RCTs and suggested that TCM as an adjuvant therapy could improve quality of life, alleviate acute adverse effects, and enhance immunoregulation.88 Zhang et al. conducted a RCT to study the use of the Fuzheng Zeng Xiao Formula for reducing the adverse reactions in 60 lung cancer patients to radiotherapy.9 In the TCM treatment group, incidence rates of fatigue, anorexia, thirst and white blood reduction were reduced by 36.4%, 30.7%, 32.3%, and 32.5%, respectively. Using prospective, multi-centre, randomized and controlled clinical research methods, Zhou et al. enrolled 294 patients with inoperable advanced stage III (A + B) and IV NSCLC who were randomly assigned to receive TCM (99 cases), TCM combined with chemotherapy (103 cases), or chemotherapy (92 cases).10 The overall response rates (ORRs) of TCM, TCM combined with chemotherapy, and chemotherapy were 4%, 26.2%, and 14.1%, respectively. Symptoms including cough, shortness of breath, anorexia, and fatigue were improved in the TCM combined with chemotherapy group compared with the chemotherapy only group. The most common grade 3–4 adverse events in every group were decreased leukocyte count (1% vs. 17.5% vs. 32.6%), anemia (5.1% vs. 8.7% vs. 18.5%) and decreased platelet count (3.9% vs. 1% vs. 8.7%). Quality of life was enhanced both physically and emotionally. Xu et al. also conducted a prospective, randomized, controlled, multi-centered trial, in which 121 patients were randomized to receive chemotherapy alone (n = 56) or chemotherapy and TCM combined (n = 65).11 The ORRs were 7.55% versus 15.87% (P = 0.170), and the disease control rates (DCRs) were 85.71% versus 71.70% in the treatment and control groups (P = 0.063), respectively. The median survival time was 16.17 versus 12.00 months in the treatment and control groups (P = 0.165), respectively. In addition, the treatment group experienced fewer adverse reactions, such as leucopenia, compared with the control group (P = 0.039).
The therapeutic function of TCM in advanced cancer patients
For advanced cancer patients, elderly patients, or in those for whom radiotherapy and chemotherapy are unsuitable, TCM has its advantages. For example, with slight adverse reactions, TCM can stabilize tumor lesions, improve symptoms, enhance the quality of life, and prolong survival time. Liu et al. enrolled 304 patients with stage III-IV adenocarcinoma lung cancer in their study and compared chemotherapy and TCM groups.12 The DCR of the TCM group was 67.83% versus 48.12% in the chemotherapy group (P < 0.01). Symptoms such as coughing, hemoptysis, chest pain, pyrexia, and anorexia were improved in the patients treated with TCM. Piao et al. carried out a multi-centre RCT to study 339 advanced NSCLC patients treated with TCM (Feiliuping paste).13,14 The DCR of patients treated with TCM was 86.2% versus 55.6% with chemotherapy. The median survival time (MST) was 9.5 versus 6.0 months in the treatment and control groups (P < 0.05), respectively. Coughing, expectoration, chest pain, shortness of breath, fatigue, and KPS were all improved. In a multi-centre RCT, Sun et al. observed 115 stage III-IV NSCLC patients in order to evaluate the efficacy of navelbine plus cisplatin chemotherapy combined with Gensing Rg3.15 The ORR was 14.5% (8/55) in the placebo group and 33. 3% (17/ 51) in the Rg3 group (P = 0. 011); the MST was 8.0 (placebo group) versus 10.0 months (Rg3 group) (P = 0. 0088). Lin et al. also conducted a multi-centre, randomized placebo controlled study, in which 414 stage III-IV NSCLC patients were assigned to receive the Shen Yi Capsule combined with chemotherapy or a placebo combined with chemotherapy.16 The MST was 12.03 months in the Shen Yi Capsule group versus 8.46 months in the placebo group with a statistically significant difference (P < 0.05). Xu et al. reported on nine small sample and randomized controlled studies in which TCM as maintenance therapy was used as the treatment for advanced NSCLC.17 Their results indicated that TCM as maintenance therapy could prolong progression-free survival and improve patients’ quality of life.
The therapeutic function of TCM in postoperative cancer patients
Traditional Chinese medicine plays a role in the treatment and prevention of cancer recurrence and metastasis and prolongs the survival time of postoperative cancer patients. Liu et al. studied the effect of Yifei Kangliu decoction in 201 patients with stage III-IV NSCLC.18 The metastasis rate in the TCM combined with chemotherapy group was 13.4% versus 35% in the chemotherapy only group (P < 0.05). Lin and Zhang observed 537 patients with postoperative NSCLC.16 The recurrence and metastasis rates were 45.1%, 50.3%, and 55.8% in the Shen Yi Capsule, Yifei Qinghua mastic, and control groups, respectively. Results showed a trend of reduced recurrence and metastasis when treated with TCM. Sun et al.’s research showed that use of the Jianpiyishen granule obviously prolonged the one, three, and five-year survival rates in gastric postoperative cancer patients.19 A recent meta-analysis of 29 RCTs, including a total of 3142 breast cancer patients treated after mastectomy, showed that TCM could improve the short-term clinical outcome (Z = 7.67, RR = 1.59, 95 % cl [1.41–1.80], P < 0.00001), prolong three (Z = 5.47, RR = 1.26, 95 % cl [1.16–1.37], P < 0.00001) and five-year survival (Z = 5.53, RR = 1.17, 95 % cl [1.11–1.24], P < 0.00001), and decrease the incidence of adverse reactions after mastectomy.20
Prevention and treatment with TCM in precancerous lesions
In view of preventive treatment before disease onset, TCM applied at an early stage can treat precancerous lesions and reduce the incidence of cancer. In a meta-analysis on esophageal cancer, Chen et al. reported that the incidence rate of the precancerous lesions in the TCM treatment group was lower than that of the control group (d = 0.0613, 95% CI 0.0456–0.0769).21 Miu et al. evaluated the clinical effect of TCM in precancerous lesions of esophageal cancer.22 They concluded that TCM could improve atrophy of gastric mucosa and intestinal metaplasia, dysplasia, infection of helicobacter pylori, and the clinical symptoms of patients (RR 1.90, 95% CI 1.60, 2.27).
Furthermore, TCM also plays roles in the perioperative period and rehabilitative stage. In the perioperative period and after surgery, TCM can strengthen a patient’s physique, helping to prevent and treat postoperative complications, facilitate postoperative rehabilitation, and regulate immune functions, such as sputum retention after lung cancer surgery, limb swelling in postoperative breast cancer patients, intestinal adhesion related to abdominal surgery, and bile reflux gastritis after gastric cancer surgery.23–28 Under the guidance of TCM theory, integral regulation aimed at mentality, nutrition, and physical fitness could relieve adverse reactions, alleviate dysfunction, and promote physical and psychological recovery.
Foreign scientists have carried out a series of clinical trials that met international quality standards (double-blinded and placebo-controlled).29,30 These studies have also shown that TCM could reduce the adverse reactions of chemotherapy and prolong overall survival.
Achievements of TCM in oncology in the last fifty years
In the last 50 years, clinical research summarizing clinical experience has proven that the use of TCM in cancer therapy has decreased toxicity and enhanced the efficacy of radiochemotherapy, prolonged survival in advanced cancer patients, and assisted in the prevention and treatment of recurrence and metastasis. Today, studies focus upon designing a comprehensive regimen and diagnostic and treatment practices guidelines. In the field of laboratory research, studies of TCM have moved focus from screening antineoplastic Chinese medicine, anti-tumor metastasis, and immune regulation, to the biological and behavioral research of tumor stem cells, intervention in the body’s internal environment, and the tumor microenvironment. The achievements of the last 50 years in developing the theory and scientific connotation of TCM in cancer prevention and treatment have served to clarify the position and function of TCM, and promote international exchange and cooperation.
The formulation and development of guidelines of diagnosis and therapy in oncology with TCM
With the development and use of Chinese medicine in clinical practice, standardization of diagnosis and treatment has become necessary to improve the level of medical care. In 2006, clinical practice guidelines for lung cancer treated with Chinese medicine received World Health Organization Western Pacific region expert consensus.31 On this basis, we established the Cooperative Organization of Practice Guidelines on TCM and Cancer (a collaboration launched by academic experts), which summarizes and evaluates evidence-based research results. It is the first national recognition of the TCM syndrome differentiation standard, treatment principles, and drug recommendations. Finally, the Guidelines of Diagnosis and Therapy in Oncology with Traditional Chinese Medicine was published in 2014, promoting TCM and highlighting the characteristics and advantages of TCM, using international standards as the yardstick.32
Developments in administration approaches and new drugs
The research and development of new drugs incorporates the disease and syndrome-guided differentiation of cancer treatment with TCM.33 The development of new drugs involves a number of diseases, including lung, gastric, intestinal, and liver cancers. The invention of TCM cancer injections has become a major revolution in TCM development. More than 10 types of TCM cancer injections are now applied to clinical cancer patients, including Shen Qi Fu Zheng (mainly composed of lanceolata and astragalus), compound matrine (mainly composed of matrine and rhizome), and Kang’ai (mainly composed of astragalus, ginseng, and oxymatrine), which provide a stable, efficient, relatively safe, and easy application in cancer patients.34–37
Basic research developments of TCM mechanism
Since 2000, more and more research on the use of TCM in cancer treatment has been published in internationally influential medical journals, including Blood, Cancer Letters, Life Science, the Journal of Ethnopharmacology, Oncology Reports, Anticancer Research, the International Journal of Oncology, and Planta Medica.38 A large number of studies show that the multicomponent nature of TCM decides its mechanism characteristic with multiple target points and links, such as inhibition of tumor angiogenesis, induction of cell differentiation and apoptosis, cell mediated cytotoxicity, and immune regulation (Fig 2).39–55 As altering a key molecule could have unexpected and amplified effects on the entire network, there have been a number of studies identifying the particular effects of various Chinese medicine extracts or derived chemicals.56–59
Figure 2.
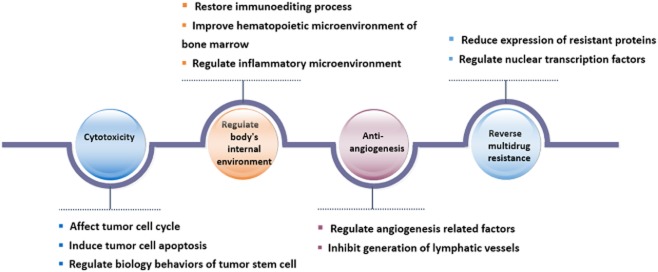
The mechanism of traditional Chinese medicine (TCM) in cancer treatment.
In recent years, research of TCM on tumors has focused on two aspects: “seed” (tumor) and “soil” (body). Studies upon seed showed that TCM could regulate the biological behavior of the tumor stem cell, consequently controlling tumor growth from “the source.”60,61 Studies upon soil investigated the regulating effect of TCM on the tumor-burdened internal environment. For example, a drug strengthening body resistance may upregulate the expression of molecules on the cytomembrane of dendritic cells (DC), promote DC maturity, induce the secretion of interleukin-12, and adjust the combination of DC and T cells.62 It may also reduce CD4+ and CD25+ regulatory T cells of tumor-burdened organisms by inhibiting the secretion of transforming growth factor–β.63 A heat-clearing and detoxicating drug could inhibit transient receptor potential cation channel subfamily V member 1 mediated capsaicin-induced extracellular signal-regulated kinase phosphorylation and reduce tumor-induced proinflammatory cytokine production.64
Establishment of international cooperation and an exchange platform
With the support of the government policy promoting the combination of Eastern and Western medicine and the overseas development of TCM, international academic exchange and cooperation in scientific research has led to new achievements using TCM. From 2011 to 2013, guided by the State Administration of TCM, the United States (US) Department of Health and Human Services (HHS), the Office of Cancer Complementary and Alternative Medicine (OCCAM) of the National Institutes of Health (NIH) and the Cancer Institute of the Chinese Academy of Medical Sciences (CAMS) have co-chaired three sessions of the Sino-US Summit Forum on TCM and Cancer. The sessions attracted positive responses from experts from Australia, South Korea, Singapore, Canada, Japan, and other countries. In order to integrate the international cancer research resources, the headquarters of the Global Consortium of Oncology and Chinese Medicine was held on 2–3 November 2014 at NIH, and involved in-depth discussions of duties and tasks for the future. Meanwhile, the International Exchange Center of the Cancer Institute of CAMS was formally established, which aims to build a new platform for the cultural communication of TCM, high-level talent cultivation, research cooperation, and transformative achievement.
Future direction of TCM in oncology
Basic research
Through the interaction of seed and soil, we explore the mechanisms of TCM therapeutic methods, such as strengthening body resistance, heat clearing and detoxifying, activating blood, and removing stasis, which serve to expand the basis of scientific connotation and materials. Research on the mechanisms of TCM in fields of immune regulation, inflammatory microenvironment, and the biological behavior of cancer stem cells is predicted.60,61 The rapid development of genome sequencing technology, nanoscience, and information science will help us further explore the mechanism of TCM on multiple targets, balance adjustment, and palliative effects. For example, we apply high content analysis technology to screen anti-cancer TCM and find the basis of materials in more effective ways.65,66 The Cancer Genome Atlas will be used in research for the detection of a connection between TCM symptom patterns and genomes.67,68 It can also help identify multiple target effects caused by TCM intervention, in order to predict effects and guide a timely adjustment of treatment.
Efficacy evaluation and drug development of TCM
According to the advantages and characteristics of TCM, new drug development will focus on improving quality of life and cancer-related symptoms. Based on general evaluation criteria and methods, patient outcomes will be incorporated into efficacy assessment, which is currently confined to a doctor’s evaluation.69 It is necessary to develop new drugs for the prevention of tumor recurrence and metastasis after surgery, to relieve the adverse reactions caused by targeted therapy, and improve progression-free survival of advanced cancer patients during maintenance treatment.
The reevaluation of drugs once they have been released into the marketplace is very necessary in order to locate the population who can benefit from the treatment, improve combination regimens, and monitor short and long-term efficacy and adverse reactions. According to new discoveries in clinical practice and basic research, we can continue research by expanding the indications of the marketed drug, as the same disease might be treated in different ways and different diseases might be treated in the same way.70–72
In future, a new generation of medicine will be developed. Leung et al. proposed an integrated network-based medicine (INBM), which considers the interactive nature of the human body and its environment.73 TCM offers us a blueprint for building a personalized approach to cancer.
Evidence-based medical research of TCM in oncology
Clinical research methods, interventions, outcome measures, quality control, and other aspects in clinical study need to be improved in order to achieve high-level evidence. We also need to pay more attention to translational research, including the effect on the metabolism of active pharmaceutical ingredients and efficacy predictors. For example, a clinical trial designed with Bayesian or factorial analysis will include fewer patients, a reduced study period, reduced cost, will quickly filter the best treatment options, and detect the efficacy of individualized therapy in comprehensive treatment.
We look forward to further results of clinical studies of TCM in cancer prevention and rehabilitation. TCM has been proven to prevent tumor recurrence and metastasis in postoperative cancer patients, prolong disease-free progression for advanced cancer patients, delay resistance to targeted therapy, and promote physical and psychological rehabilitation of cancer patients.14,74–80
As evidence is continually updated, experts will continue to discuss syndrome differentiation, differentiation methods, treatment principles, treatment options, recommended drugs, and recommended levels in order to reach consensus. TCM oncology guidelines corresponding to the National Comprehensive Cancer Network, the European Society for Medical Onocology or other internationally recognized oncology clinical practice guidelines can be developed and published.69
As modern medical concepts adjust from curing to preventing disease and improving the physique, the advantages of TCM become more obvious than they have been in the past. Focusing on the characteristics and advantages of TCM in cancer treatment, we can make use of advanced methods and technologies in various disciplines with international cooperation and communication in order to improve the development of clinical and basic research of TCM in oncology.
Acknowledgments
This research was supported by grants from the State Administration of Traditional Chinese Medicine 201307006, and the International S&T Cooperation Program Office of China 2013DFA32540.
Disclosure
No authors report any conflict of interest.
References
- Wang B. Ancient Books of TCM Publishing House, Beijing 2003(Tang Dynasty). The Yellow Emperor’s Inner Canon.
- Hua T. People’s Medical Publishing House, Beijing 2007(Han Dynasty). The Central Treasury Canon.
- Li ZZ. People’s Medical Publishing House, Beijing 2006(Ming Dynasty). Indispensable Medical Reading.
- McCulloch M, See C, Shu XJ, et al. Astragalus-based Chinese herbs and platinum-based chemotherapy for advanced non-small-cell lung cancer: Meta-analysis of randomized trials. J Clin Oncol. 2006;24:419–430. doi: 10.1200/JCO.2005.03.6392. [DOI] [PubMed] [Google Scholar]
- Gan T, Wu Z, Tian L, Wang Y. Chinese herbal medicines for induction of remission in advanced or late gastric cancer. Cochrane Database Syst Rev. 2010;(1) doi: 10.1002/14651858.CD005096.pub2. CD005096. [DOI] [PubMed] [Google Scholar]
- Li SG, Chen HY, Ou-Yang CS, et al. The efficacy of Chinese herbal medicine as an adjunctive therapy for advanced non-small cell lung cancer: A systematic review and meta-analysis. PLoS ONE. 2013;8(2):e57604. doi: 10.1371/journal.pone.0057604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong LL, Chen HY, Cho WC, Meng XM, Tong Y. The efficacy of Chinese herbal medicine as an adjunctive therapy for colorectal cancer: A systematic review and meta-analysis. Complement Ther Med. 2012;20:240–252. doi: 10.1016/j.ctim.2012.02.004. [DOI] [PubMed] [Google Scholar]
- Mao CG, Tao ZZ, Wan LJ, Han JB, Chen Z, Xiao BK. The efficacy of traditional Chinese medicine as an adjunctive therapy in nasopharyngeal carcinoma: A systematic review and meta-analysis. J BUON. 2014;19:540–548. [PubMed] [Google Scholar]
- Zhang DZ, Xu JD. Clinical and experimental researches on improving radiation sensibility for lung cancer patients. Chin J Surg Integr Tradit West Med. 1998;4:71–75. (In Chinese.) [Google Scholar]
- Zhou DH, Lin LZ, Zhou YQ. Effect of Chinese herbal medicine in prolonging median survival time in patients with non-small-cell lung cancer. J Guangzhou Univ Tradit Chin Med. 2005;7:255–258. (In Chinese.) [Google Scholar]
- Xu ZY, Jin CJ, Zhou CC, et al. Treatment of advanced non-small-cell lung cancer with Chinese herbal medicine by stages combined with chemotherapy. J Cancer Res Clin Oncol. 2011;137:1117–1122. doi: 10.1007/s00432-011-0975-3. [DOI] [PubMed] [Google Scholar]
- Liu JX, Shi ZM, Xu ZY. Studies on late primary adenocarcinoma of lung treated by methods of nourishing yin to replenish fluid and warming Yang to benefit Qi. J Tradit Chin Med. 1995;36:155–158. (In Chinese.) [Google Scholar]
- Piao BK, Tang WX, Zhang ZQ, Lin HS, Duan FW, Yu GQ. The clinical observation of Feiliuping paste curing advanced lung cancer–and clinical analysis of 339 cases. J Tradit Chin Med. 1991;4:21–23. (In Chinese.) [Google Scholar]
- Tang WX, Zhang ZQ, Lin HS, Hou W, Piao BK. The clinical observation of the TCM treatment of NSCLC. J Tradit Chin Med. 1994;5:283–285. (In Chinese.) [Google Scholar]
- Sun Y, Lin HS, Zhu YZ, et al. A randomized, prospective, multi-centre clinical trial of NP regimen (vinorelbine+cisplatin) plus Gensing Rg3 in the treatment of advanced non-small cell lung cancer patients. Chin J Lung Cancer. 2006;9:254–258. doi: 10.3779/j.issn.1009-3419.2006.03.09. (In Chinese.) [DOI] [PubMed] [Google Scholar]
- Lin HS, Zhang Y. Evidence-based medical study of TCM on non small cell lung cancer. World Sci Technol. 2008;10:121–125. (In Chinese.) [Google Scholar]
- Xu W, Yang G, Xu Y, et al. The possibility of traditional Chinese medicine as maintenance therapy for advanced nonsmall cell lung cancer. Evid Based Complement Alternat Med. 2014;2014:278917. doi: 10.1155/2014/278917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu L, Liu JX. Effect of yifei kangliu yin on lung cancer metastasis and immune function. Chin J Integr Med. 1997;17:401–403. (In Chinese.) [PubMed] [Google Scholar]
- Sun GZ, Yu GQ, Zhang PT. Clinical and mechanism research on Fu Zheng Pei Ben serial formulas’ application on gastric cancer treatment. J Zhejiang Univ Tradit Chin Med. 2005;33:695–700. (In Chinese.) [Google Scholar]
- Wang W, Xu L, Shen C. Effects of traditional Chinese medicine in treatment of breast cancer patients after mastectomy: A meta-analysis. Cell Biochem Biophys. 1999 doi: 10.1007/s12013-014-0348-z. doi: 10.1007/s12013-014-0348-z. [DOI] [PubMed] [Google Scholar]
- Chen ZF, Zhang JH. Meta research of TCM treatment for precancerous lesions of esophageal cancer. Traditi Chin Med Res. 2014;12:20–21. (In Chinese.) [Google Scholar]
- Miu CR, Shen H. Meta-analysis of effectiveness of Chinese medicinal herbs in treating precancerous lesions of gastric cancer. J Liaoning Univ Tradit Chin Med. 2009;11:35–37. (In Chinese.) [Google Scholar]
- Lin Y, Fu J. Effect of Fei’an decoction on the symptomatic relief in postoperative pulmonary carcinoma. J Guangzhou Univ Tradit Chin Med. 1998;02:21–23. (In Chinese.) [Google Scholar]
- Me H, Chen ZC. The effect of shenfu injection on human immune function at lung cancer patients. Guizhou Med J. 2003;27:796. [Google Scholar]
- He Y. Objective to Tanreqing Injection for Sputum Retention after lung cancer operation. J Emerg Tradit Chin Med. 2009;2:194. (In Chinese.) [Google Scholar]
- Luo XB, Li L, Liu NM. Effect observation of TCM treatment for breast cancer patients after operation. J Emerg Tradit Chin Med. 2008;17:770–771. (In Chinese.) [Google Scholar]
- Zuo MH, Li QW, Sun T. 76 malignancy intestinal obstruction cases of clinical observation by enema with Chinese medicine. China J Tradit Chin Med Pharm. 2007;22:654–655. (In Chinese.) [Google Scholar]
- He HB, Wang F. The idea and method of treatment of Bile Reflex Gastritis with Zheng-dan decoction. Med Philos. 1995;16:599–600. (In Chinese.) [Google Scholar]
- Saif MW, Li J, Lamb L, et al. First-in-human phase II trial of the botanical formulation PHY906 with capecitabine as second-line therapy in patients with advanced pancreatic cancer. Cancer Chemother Pharmacol. 2014;73:373–380. doi: 10.1007/s00280-013-2359-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aoyama T, Nishikawa K, Takiguchi N, et al. Double-blind, placebo-controlled, randomized phase II study of TJ-14 (hangeshashinto) for gastric cancer chemotherapy-induced oral mucositis. Cancer Chemother Pharmacol. 2014;73:1047–1054. doi: 10.1007/s00280-014-2440-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2010. Chinese Academy of Medical Sciences (CAMS) TCM Guidelines of Evidence-based Clinical Practice – Internal Medicine of TCM. China Press of Traditional Chinese Medicine, Beijing.
- Lin HS. Guidelines of Diagnosis and Therapy in Oncology with Traditional Chinese Medicine. 2014. People’s Health Publishing House, Beijing.
- Wang YH, Xu AL. Zheng: A systems biology approach to diagnosis and treatments. Science. 2014;346(6216 Suppl):s13–s15. [Google Scholar]
- Yao K, Ma Y, Ma W, et al. Shenqifuzheng injection combined with chemotherapy in the treatment of advanced gastric cancer: A systematic review and meta-analysis. J Cancer Res Ther. 2014;10(Suppl. 1):70–74. doi: 10.4103/0973-1482.139768. [DOI] [PubMed] [Google Scholar]
- Zhao Z, Fan H, Higgins T, et al. Fufang Kushen injection inhibits sarcoma growth and tumor-induced hyperalgesia via TRPV1 signaling pathways. Cancer Lett. 2014;355:232–241. doi: 10.1016/j.canlet.2014.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan CX, Lin CL, Liang L, et al. Enhancing effect of compound Kusheng injection in combination with chemotherapy for patients with advanced non-small cell lung cancer. Chin J Oncol. 2010;32:294–297. (In Chinese.) [PubMed] [Google Scholar]
- Liu S, Wang H, Lin H. The clinical research of Kangai injection with chemotherapy in the treatment of advanced non-small cell lung cancer. World Chin Med. 2014;03:323–325. (In Chinese.) [Google Scholar]
- Hu B, An HM, Shen KP. Documents research of TCM cancer treatment of SCI journals. Chin J Ethnomedicine Ethnopharmacy. 2009;20:26–27. (In Chinese.) [Google Scholar]
- Dong Y, Lu B, Zhang X, et al. Cucurbitacin E, a tetracyclic triterpenes compound from Chinese medicine, inhibits tumor angiogenesis through VEGFR2-mediated Jak2-STAT3 signaling pathway. Carcinogenesis. 2010;31:2097–2104. doi: 10.1093/carcin/bgq167. [DOI] [PubMed] [Google Scholar]
- Tsai CH, Lin FM, Yang YC, et al. Herbal extract of Wedelia chinensis attenuates androgen receptor activity and orthotopic growth of prostate cancer in nude mice. Clin Cancer Res. 2009;15:5435–5444. doi: 10.1158/1078-0432.CCR-09-0298. [DOI] [PubMed] [Google Scholar]
- Yue GG, Chan BC, Kwok HF, et al. Anti-angiogenesis and immunomodulatory activities of an anti-tumor sesquiterpene bigelovin isolated from Inula helianthus-aquatica. Eur J Med Chem. 2013;59:243–252. doi: 10.1016/j.ejmech.2012.11.029. [DOI] [PubMed] [Google Scholar]
- Yeh JC, Cindrova-Davies T, Belleri M, et al. The natural compound n-butylidenephthalide derived from the volatile oil of Radix Angelica sinensis inhibits angiogenesis in vitro and in vivo. Angiogenesis. 2011;14:187–197. doi: 10.1007/s10456-011-9202-8. [DOI] [PubMed] [Google Scholar]
- Zhang XW, Yan XJ, Zhou ZR, et al. Arsenic trioxide controls the fate of the PML-RARalpha oncoprotein by directly binding PML. Science. 2010;328:240–243. doi: 10.1126/science.1183424. [DOI] [PubMed] [Google Scholar]
- Zhang H, Su X, Guo L, et al. Silencing SATB1 inhibits the malignant phenotype and increaes sensitivity of human osteosarcoma U2OS cells to arsenic trioxide. Int J Med Sci. 2014;11:1262–1269. doi: 10.7150/ijms.10038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu SS, Wang XP, Li XB, et al. Zoledronic acid exerts antitumor effects in NB4 acute promyelocytic leukemia cells by inducing apoptosis and S phase arrest. Biomed Pharmacother. 2014;68:1031–1036. doi: 10.1016/j.biopha.2014.09.004. [DOI] [PubMed] [Google Scholar]
- Luo KW, Ko CH, Yue GG, et al. Green tea (Camellia sinensis) extract inhibits both the metastasis and osteolytic components of mammary cancer 4T1 lesions in mice. J Nutr Biochem. 2014;25:395–403. doi: 10.1016/j.jnutbio.2013.11.013. [DOI] [PubMed] [Google Scholar]
- Li PC, Lam E, Roos WP, Zdzienicka MZ, Kaina B, Efferth T. Artesunate derived from traditional Chinese medicine induces DNA damage and repair. Cancer Res. 2008;68:4347–4351. doi: 10.1158/0008-5472.CAN-07-2970. [DOI] [PubMed] [Google Scholar]
- Zhang L, Wu C, Zhang Y, et al. Comparison of efficacy and toxicity of traditional Chinese medicine (TCM) herbal mixture LQ and conventional chemotherapy on lung cancer metastasis and survival in mouse models. PLoS ONE. 2014;9(10):e109814. doi: 10.1371/journal.pone.0109814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prasad S, Gupta SC, Tyagi AK, Aggarwal BB. Curcumin, a component of golden spice: From bedside to bench and back. Biotechnol Adv. 2014;32:1053–1064. doi: 10.1016/j.biotechadv.2014.04.004. [DOI] [PubMed] [Google Scholar]
- Li L, Yue GG, Pu JX, et al. Eriocalyxin B-induced apoptosis in pancreatic adenocarcinoma cells through thiol-containing antioxidant systems and downstream signalling pathways. Curr Mol Med. 2014;14:673–689. doi: 10.2174/1566524014666140603102459. [DOI] [PubMed] [Google Scholar]
- Tang PM, Zhang DM, Xuan NH, et al. Photodynamic therapy inhibits P-glycoprotein mediated multidrug resistance via JNK activation in human hepatocellular carcinoma using the photosensitizer pheophorbide a. Mol Cancer. 2009;8:56. doi: 10.1186/1476-4598-8-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Murakami T, Oppenhei JJ, Howard OM. Triptolide, a constituent of immunosuppressive Chinese herbal medicine, is a potent suppressor of dendritic-cell maturation and trafficking. Blood. 2005;106:2409–2416. doi: 10.1182/blood-2005-03-0854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho WC, Leung KN. In vitro and in vivo anti-tumor effects of Astragalus membranaceus. Cancer Lett. 2007;252:43–54. doi: 10.1016/j.canlet.2006.12.001. [DOI] [PubMed] [Google Scholar]
- Ragupathi G, Yeung KS, Leung PC, et al. Evaluation of widely consumed botanicals as immunological adjuvants. Vaccine. 2008;26:4860–4865. doi: 10.1016/j.vaccine.2008.06.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yue GG, Chan BC, Han XQ, et al. Immunomodulatory activities of Ganoderma sinense polysaccharides in human immune cells. Nutr Cancer. 2013;65:765–774. doi: 10.1080/01635581.2013.788725. [DOI] [PubMed] [Google Scholar]
- Zhang QY, Mao JH, Liu P, et al. A systems biology understanding of the synergistic effects of arsenic sulfide and Imatinib in BCR/ABL-associated leukemia. Proc Natl Acad Sci U S A. 2009;106:3378–3383. doi: 10.1073/pnas.0813142106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J, Jiang P, Zhang W. Molecular networks for the study of TCM pharmacology. Brief Bioinform. 2010;11:417–430. doi: 10.1093/bib/bbp063. [DOI] [PubMed] [Google Scholar]
- Lam W, Bussom S, Guan F, et al. The four-herb Chinese medicine PHY906 reduces chemotherapy-induced gastrointestinal toxicity. Sci Transl Med. 2010;2(45):45ra59. doi: 10.1126/scitranslmed.3001270. [DOI] [PubMed] [Google Scholar]
- Guo B, Zhang T, Su J, Wang K, Li X. Oxymatrine targets EGFR(p-Tyr845) and inhibits EGFR-related signaling pathways to suppress the proliferation and invasion of gastric cancer cells. Cancer Chemother Pharmacol. 2015;75:353–363. doi: 10.1007/s00280-014-2651-1. [DOI] [PubMed] [Google Scholar]
- Xu W, Lin H, Zhang Y. Compound Kushen Injection suppresses human breast cancer stem-like cells by down-regulating the canonical Wnt/β-catenin pathway. J Exp Clin Cancer Res. 2011;30:103. doi: 10.1186/1756-9966-30-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Piao B, Zhang Y. Oxymatrine diminishes the side population and inhibits the expression of β-catenin in MCF-7 breast cancer cells. Med Oncol. 2011;28(Suppl. 1):S99–107. doi: 10.1007/s12032-010-9721-y. [DOI] [PubMed] [Google Scholar]
- Zheng HG, Piao BK, Lin HS. Molecular mechanism of Fei Liu Ping ointment and its modified formulas regulating antigen presentation function of DC. Chin Arch Tradit Chin Med. 2007;25:1133–1136. (In Chinese.) [Google Scholar]
- Fan HT, Lin HS, Li J, Qi X, Pei YX, Wu H. Effect of cultured cordyceps militaris on CD4+CD25+ regulatory T cells in Lewis lung carcinoma bearing mice. Chin J Cancer Prev Treat. 2009;15:1130–1134. (In Chinese.) [Google Scholar]
- Zhao Z, Fan H, Higgins T, et al. Fufang Kushen injection inhibits sarcoma growth and tumor-induced hyperalgesia via TRPV1 signaling pathways. Cancer Lett. 2014;355:232–241. doi: 10.1016/j.canlet.2014.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu D, Lao Y, Xu N, et al. Identification and characterization of anticancer compounds targeting apoptosis and autophagy from Chinese native Garcinia species. Planta Med. 2015;81:79–89. doi: 10.1055/s-0034-1383356. [DOI] [PubMed] [Google Scholar]
- Brandl MB, Pasquier E, Li F, et al. Computational analysis of image-based drug profiling predicts synergistic drug combinations: Applications in triple-negative breast cancer. Mol Oncol. 2014;8:1548–1560. doi: 10.1016/j.molonc.2014.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang C, Liu HW, Wang LC. Study on the differential gene expressions of chronic hepatitis B patients of gan depression Pi deficiency syndrome and Pi-Wei damp-hear syndrome. Chin J Integr Med. 2012;08:1032–1037. (In Chinese.) [PubMed] [Google Scholar]
- Xie LH, Zhao YP, Chen K, Lai YL, Ge JR. Bioinformatics analysis of genes expression profiles of postmenopausal osteoporosis with Kidney Yin deficiency. Journal of Clinical Rehabilitative Tissue Engineering Research. 2011;15:2833–2837. (In Chinese.) [Google Scholar]
- Li J, Li L, Liu R, Lin HS. Establishing Chinese medicine characteristic tumor response evaluation system is the key to promote internationalization of Chinese medicine oncology. Chin J Integr Med. 2012;18:730–736. doi: 10.1007/s11655-012-1254-0. [DOI] [PubMed] [Google Scholar]
- Hou W, Liu J, Shi WG, Lin HS. Multi-center, randomized, controlled clinical study of radiation pneumonitis treated with compound matrine injection in primary lung cancer patients. Chin J New Drugs. 2013;17:2065–2068. (In Chinese.) [Google Scholar]
- Lin HS, Yang ZY, Zhang PT, et al. Clinical efficacy observation of Shengxue Pills in treating hematology decline caused by chemotherapy in nonsmall-cell lung cancer. China J Tradit Chin Med Pharm. 2013;08:2491–2494. (In Chinese.) [Google Scholar]
- Lin HS, Sun GP, Qing FZ, et al. A randomized, double-blinded, drug-controlled and multicentre clinical trial of chemotherapy assisted with Jinlong capsule on gastric cancer. Cancer Res Prev Treat. 2013;1:12–15. [Google Scholar]
- Leung ELH, Wong VKW, Jiang ZH, Li T, Liu L. Integrated network-based medicine: The role of traditional Chinese medicine in developing a new generation of medicine. Science. 2014;346(6216 Suppl):s16–18. [Google Scholar]
- Tian HQ, Wang YJ, Wang B, et al. Effect of ruji recipe on the post-surgical survival of female breast cancer patients. Chin J Integr Med. 2013;33:1336–1340. (In Chinese.) [PubMed] [Google Scholar]
- Yang XB, Wu WY, Long SQ, Deng H, Pan ZQ. Effect of gefitinib plus Chinese herbal medicine (CHM) in patients with advanced non-small-cell lung cancer: A retrospective case-control study. Complement Ther Med. 2014;22:1010–1018. doi: 10.1016/j.ctim.2014.10.001. [DOI] [PubMed] [Google Scholar]
- You YL. TCM cut into the targeted therapy of lung cancer. Liaoning J Tradit Chin Med. 2006;10:1227–1229. (In Chinese.) [Google Scholar]
- Johnston MF, Hays RD, Subramanian SK, et al. Patient education integrated with acupuncture for relief of cancer-related fatigue randomized controlled feasibility study. BMC Complement Altern Med. 2011;11:49. doi: 10.1186/1472-6882-11-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesa K, Gubili J, Cassileth B. Integrative oncology: Complementary therapies for cancer survivors. Hematol Oncol Clin North Am. 2008;22:343–353. doi: 10.1016/j.hoc.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Running A, Seright T. Integrative oncology: Managing cancer pain with complementary and alternative therapies. Curr Pain Headache Rep. 2012;16:325–331. doi: 10.1007/s11916-012-0275-x. [DOI] [PubMed] [Google Scholar]
- Piao BK, Wang YX, Xie GR, et al. Impact of complementary mistletoe extract treatment on quality of life in breast, ovarian and non-small cell lung cancer patients: A prospective randomized controlled clinical trial. Anticancer Res. 2004;24:303–309. [PubMed] [Google Scholar]


