Abstract
Human immunodeficiency virus (HIV) controllers are patients who control viral replication without antiretroviral therapy. We present the case of an HIV controller who had CD4 and CD8 coexpressed on 40% of his T cells. Although a recent study found that double-positive T cells had superior antiviral capacity in HIV-1 controllers, in this case, the CD4+CD8+ T cells did not have strong antiviral activity.
Keywords: AIDS, double-positive cells, elite controllers, HIV, HIV controllers, immune activation, long-term nonprogressors, viremic controllers
Human immunodeficiency virus (HIV) controllers are patients who control viral replication without antiretroviral therapy [1]. We present the case of an HIV controller who had CD4 and CD8 coexpressed on 40% of his T cells. Although a recent study found that double-positive T cells had superior antiviral capacity in HIV-1 controllers [2], in this case, the CD4+CD8+ T cells did not have strong antiviral activity.
CASE PRESENTATION
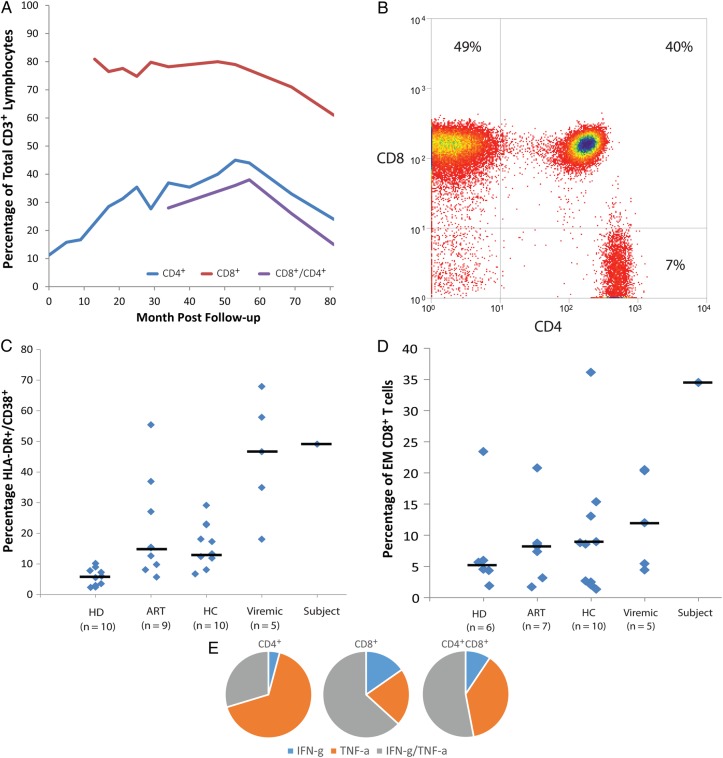
The patient is a 62-year-old African American male with human immunodeficiency virus (HIV) infection diagnosed 12 years ago. His CD4 count was 711 cells/µL, and his viral load was 141 copies/mL plasma without antiretroviral therapy (ART) at diagnosis. His viral load remained undetectable to low (<400 copies/mL), and although his absolute CD4 count was very high, his CD4+ T cell percentage was low and his CD8+ T cell percentage was elevated (Figure 1A). At year 3, it was noted that 26% of lymphocytes coexpressed CD4 and CD8 and the proportion eventually peaked at 40%. These cells were not reported before year 3, but the aggregate percentage of CD4+ and CD8+ T cells exceeded 100%, suggesting that CD4+CD8+ cells had always been present. A malignancy workup included a polymerase chain reaction (PCR) for clonal T cell rearrangement (negative), fluorescent in situ hybridization for B-cell chronic lymphocytic leukemia (negative), and cytogenetics (normal chromosomes). Human T-lymphotropic virus type-1 serology was negative.
Figure 1.
Percentage of different T cell populations over time in the subject (A). Flow cytometry showing the large population of CD4+CD8+ T cells (B). Comparison of activated (C) and effector memory (EM; D) CD8+ T cells in the subject compared with healthy donors (HD), untreated viremic patients, patients on antiretroviral therapy (ART), and human immunodeficiency virus controllers (HC). The percentage of CD4+CD8+ T cells was too low in the other patients for a meaningful comparison to be performed. Percentage of cells that expressed interferon-γ or tumor necrosis factor-α alone or in combination after stimulation with anti-CD3 and anti-CD28 monoclonal antibodies.
Flow cytometry showed that the density of CD4 was lower on CD4+CD8+ T cells than on CD4+ T cells (Figure 1B). Because HIV infection results in down-regulation of CD4, we measured the frequency of HIV infection with semiquantitative PCR. Infection was detected in 0.01% of CD4+ T cells but <0.001% of CD4+CD8+ cells (Table 1); therefore, double-positive cells were not a major infection target. Consistent with this finding, expression of CCR5 and CXCR4 was lower in CD4+CD8+ T cells than in CD4+ T cells, and there was less viral entry of CD4+CD8+ T cells than CD4+ T cells after spinoculation with CCR5-tropic and CXCR4-tropic viruses (Table 1).
Table 1.
Features of T Cell Subsets
| CD4+ T Cells | CD8+ T Cells | CD4+CD8+ T Cells | |
|---|---|---|---|
| T cell phenotype | |||
| Activated (CD38+/HLA-DR+) | 8% | 49% | 53% |
| Naive (CCR7+/CD45RA+) | 9% | 2% | 1% |
| Terminal Effector (CCR7−/CD45RA+) | 0% | 18% | 2% |
| Central memory (CCR7+/CD45RA−) | 31% | 2% | 1% |
| Effector memory (CCR7−/CD45RA−) | 18% | 35% | 55% |
| HIV-1 susceptibility | |||
| % infected cells (PCR analysis) | 0.01% | NA | <0.001% |
| CCR5 positive | 35% | 25% | 15% |
| CXCR4 positive | 88% | 59% | 76% |
| % CCR5-tropic virus entry | 27% | 0.3% | 6% |
| % CXCR4-tropic virus entry | 20% | 0.4% | 7% |
| Polyclonal T cell responses | |||
| IFN-γ and/or TNF-α expression: Unstimulated cells | 0% | 0.5% | 0.4% |
| IFN-γ and/or TNF-α expression: PHA-stimulated cells | 11.9% | 30.4% | 44.8% |
| IFN-γ and/or TNF-α expression: CD3/CD28-stimulated cells | 25.9% | 40.9% | 39.1% |
| IFN-γ and/or TNF-α expression: PMA/ionomycin-stimulated cells | 72.5% | 78.3% | 69.4% |
| HIV-1-specific responses | |||
| TNF-α expression: Unstimulated cells | 0.4% | 0.1% | 0.1% |
| TNF-α expression: Gag-stimulated cells | 5.2% | 7% | 6.1% |
| TNF-α, IFN-γ, IL-2 expression: Gag-stimulated cells | <0.1% | <0.1% | <0.1% |
| % Inhibition of HIV-1 replication: Day 5 | NA | 29% | 0% |
Abbreviations: HIV, human immunodeficiency virus; IFN, interferon; IL, interleukin; NA, not applicable; PCR, polymerase chain reaction; PHA, phytohemagglutinin; PMA, phorbol 12-myristate 13-acetate; TNF, tumor necrosis factor.
A much larger fraction of CD8+ and CD4+CD8+ T cells was activated compared with CD4+ T cells as measured by HLA-DR/CD38+ expression (Table 1). The percentage of activated CD8+ T cells was comparable to that seen in untreated individuals and higher than that in treated patients, HIV controllers, and uninfected individuals (Figure 1C).
CD4+CD8+ and CD8+ T cell fractions contained high levels of effector memory cells (Table 1) that exceeded the percentage seen in healthy donor and HIV-infected subjects (Figure 1D). The CD4+CD8+ T cells, CD4+ T cells and CD8+ T cell produced comparable levels of cytokines in response to polyclonal stimulation (Table 1), but the pattern of the cytokine production in CD4+CD8+ T cells was more similar to CD8+ T cells than CD4+ T cells (Figure 1E). To determine whether the cells were HIV-1 specific, they were stimulated with HIV-1 antigens. A similar proportion of all 3 cell populations expressed TNF-α in response to stimulation with Gag peptides (Table 1). In contrast to a prior study in which CD4+CD8+ T cells were often multifunctional [2], <0.1% of CD4+, CD8+, and CD4+CD8+ simultaneously expressed TNF-α, IFN-γ, and IL-2 (Table 1). Furthermore, although CD8+ T cells had a modest inhibitory effect on viral replication, CD4+CD8+ T had no detectable effect (Table 1).
CONCLUSIONS
We present the case of an HIV controller with a very large, persistent population of CD4+CD8+ T cells (15%–40%). There is a prior report of an HIV-infected individual with progressive disease who had elevated CD4+CD8+ T cells (approximately 7.5%) over 8 years [3]. In that case, CD4+CD8+ T cells had a low CD8 density and were phenotypically similar to CD4+ cells, whereas in our case, the CD4+CD8+ T cells are similar to CD8+ T cells based on the cytokine expression pattern and activation and memory markers. Although some studies suggest that CD4+CD8+ T cells have enhanced antiviral activity [2, 4], this was not observed here.
Although we were not able to determine the etiology of the mutual expression of CD4 and CD8 on T cells, flow cytometry revealed that the majority of these CD4+CD8+ T cells were effector memory cells with an activated phenotype. Human immunodeficiency virus controllers generally have higher levels of activated CD8+ T cells [5], elevated inflammatory biomarkers [6, 7], and higher rates of atherosclerosis [8, 9] compared with treated and uninfected individuals. The significance of this inflammation is an active area of investigation. A recent study reported HIV controllers have higher rates of hospitalization than treated patients [10]. Preliminary studies suggest that ART decreases immune activation in some HIV controllers [11–13]. Randomized controlled trials are needed to determine the impact of ART and/or anti-inflammatory treatment in HIV controllers.
Acknowledgments
Author contributions. R. W. B., M. S., and C. W. P. contributed equally to the manuscript.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1.O'Connell KA, Bailey JR, Blankson JN. Elucidating the elite: mechanisms of control in HIV-1 infection. Trends Pharmacol Sci 2009; 30:631–7. [DOI] [PubMed] [Google Scholar]
- 2.Frahm MA, Picking RA, Kuruc JD, et al. CD4+CD8+ T cells represent a significant portion of the anti-HIV T cell response to acute HIV infection. J Immunol 2012; 188:4289–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weiss L, Roux A, Garcia S, et al. Persistent expansion, in a human immunodeficiency virus-infected person, of V beta-restricted CD4+CD8+ T lymphocytes that express cytotoxicity-associated molecules and are committed to produce interferon-gamma and tumor necrosis factor-alpha. J Infect Dis 1998; 178:1158–62. [DOI] [PubMed] [Google Scholar]
- 4.Nascimbeni M, Shin EC, Chiriboga L, et al. Peripheral CD4(+)CD8(+) T cells are differentiated effector memory cells with antiviral functions. Blood 2004; 104:478–86. [DOI] [PubMed] [Google Scholar]
- 5.Hunt PW, Brenchley J, Sinclair E, et al. Relationship between T cell activation and CD4+ T cell count in HIV-seropositive individuals with undetectable plasma HIV RNA levels in the absence of therapy. J Infect Dis 2008; 197:126–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krishnan S, Wilson EM, Sheikh V, et al. Evidence for innate immune system activation in HIV type 1-infected elite controllers. J Infect Dis 2014; 209:931–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Noel N, Boufassa F, Lecuroux C, et al. Elevated IP10 levels are associated with immune activation and low CD4(+) T-cell counts in HIV controller patients. AIDS 2014; 28:467–76. [DOI] [PubMed] [Google Scholar]
- 8.Hsue PY, Hunt PW, Schnell A, et al. Role of viral replication, antiretroviral therapy, and immunodeficiency in HIV-associated atherosclerosis. AIDS 2009; 23:1059–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pereyra F, Lo J, Triant VA, et al. Increased coronary atherosclerosis and immune activation in HIV-1 elite controllers. AIDS 2012; 26:2409–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crowell TA, Gebo KA, Blankson JN, et al. Elite controllers are hospitalized more often than persons with medically controlled HIV [Epub ahead of print]. J Infect Dis 2015; doi:10.1093/infdis/jiu809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sedaghat AR, Rastegar DA, O'Connell KA, et al. T cell dynamics and the response to HAART in a cohort of HIV-1-infected elite suppressors. Clin Infect Dis 2009; 49:1763–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chun TW, Shawn Justement J, Murray D, et al. Effect of antiretroviral therapy on HIV reservoirs in elite controllers. J Infect Dis 2013; 208:1443–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hatano H, Yukl SA, Ferre AL, et al. Prospective antiretroviral treatment of asymptomatic, HIV-1 infected controllers. PLoS Pathog 2013; 9:e1003691. [DOI] [PMC free article] [PubMed] [Google Scholar]