Abstract
We tested the hypothesis that later completion of the Fontan procedure is associated with improved exercise capacity in the current period of staged single-ventricle palliation. We performed a retrospective study, in Fontan patients, of exercise stress test data from April 2003 through March 2011. Patients were included if they had received staged palliations in accordance with current surgical strategy, defined as the performance of a superior cavopulmonary connection at ≤1 year of age, followed in subsequent years by Fontan completion. Patients with a pacemaker or respiratory exchange ratio <1 were excluded. Early and late Fontan groups were created on the basis of whether Fontan completion had been performed at <4 or ≥ 4 years of age. The primary predictor variable was age at Fontan completion, and the primary marker of exercise performance was the percentage of predicted maximum oxygen consumption. During the study period, 55 patients were identified (mean age, 11.7 ± 2.8 yr).
Older age at Fontan completion correlated positively with higher percentages of predicted maximum oxygen consumption (R=0.286, P=0.034). Patients in whom Fontan completion was performed at ≥4 years of age had higher percentages of predicted maximum oxygen consumption than did those in whom completion was at <4 years of age (84.4 ± 21.5 vs 72.9 ± 18.1; P=0.041). Later Fontan completion might be associated with improved exercise capacity in patients palliated in accordance with contemporary surgical strategy.
Keywords: Child, preschool; exercise test; Fontan procedure/adverse effects; heart defects, congenital/surgery; hemodynamics/physiology; hypoplastic left heart syndrome; longitudinal studies; oxygen consumption/physiology; physical exertion; postoperative complications; pulmonary circulation; retrospective studies; tricuspid atresia/surgery; vascular resistance
It has long been understood that exercise performance is diminished in patients who have undergone the Fontan procedure. Poor exercise performance in this population has been linked to decreased heart-rate response to exercise,1 increased body mass index,1 ventricular dysfunction,2 right ventricular morphology of the single ventricle,3 and the atriopulmonary-type Fontan.4 More recently, studies have shown that decreased exercise performance is associated with an increased risk of early death.5,6 Exercise stress test data might then uncover circulatory limitations not seen in the at-rest patient. We reviewed our institution's experience and sought to determine the association between a patient's age at performance of the Fontan procedure and his or her aerobic performance, as measured by the percentage of predicted maximum oxygen consumption (Vo2). We especially focused on those patients who had been treated in accordance with the current strategy of staged single-ventricle palliation, in which a superior cavopulmonary connection (ScPc) precedes the Fontan procedure.
Patients and Methods
In this retrospective clinical study, we reviewed the cases of all Fontan patients who had undergone exercise testing at our center from April 2003 through March 2011. Patient demographics (age and sex) and clinical characteristics were obtained from our cardiology database. The age of each patient at the Fontan operation was also noted. The single-ventricle anatomy type (for example, morphologic right ventricle), the Fontan type (lateral tunnel or extracardiac conduit), and the presence of a fenestration at the time of the Fontan procedure and at the time of exercise testing were documented. Pacemaker dependency was also noted. In order to investigate a group palliated in accordance with current surgical strategy, patients were excluded if they had undergone a single-stage Fontan or a superior cavopulmonary anastomosis at an age older than one year. Patients were also excluded if they had a respiratory exchange ratio of less than 1, or a pacemaker at the time of exercise testing. Approval for this study was obtained from the Baylor College of Medicine Institutional Review Board.
In all patients, treadmill exercise testing was performed in accordance with the Bruce protocol.7 If more than one exercise test was performed on a patient, the most recent study was used. Metabolic measurements were derived from inspired gas. Absolute values were obtained for peak Vo2, Vo2 at anaerobic threshold, peak oxygen pulse, peak heart rate, and chronotropic index. Oxygen pulse is the peak Vo2 divided by the peak heart rate. The oxygen pulse index was calculated as the oxygen pulse divided by the patient's body surface area. On the basis of normative data, we calculated percentiles of predicted maximum Vo2, anaerobic threshold,8 and maximum heart rate.9 A respiratory exchange ratio of ≥1 was considered the equivalent of adequate exercise effort.6
We recorded age, time from Fontan operation, body mass index, and body surface area at the time of exercise testing. Echocardiograms performed within 1 year of exercise testing were reviewed for the presence of moderate or greater atrioventricular valve regurgitation and moderate or greater ventricular systolic dysfunction. For patients who had undergone cardiac catheterization within 3 years of exercise testing, we included mean Fontan pressure and pulmonary vascular resistance index data. Pulmonary vascular resistance index at catheterization was calculated from an assumed Vo2 on the basis of the patient's age, sex, and heart rate. Central branch pulmonary artery (PA) caliber was evaluated by reviewing angiograms, computed tomograms, and magnetic resonance images, provided that the imaging had been performed 4 years before or after the exercise testing. Imaging or catheterization data were excluded if surgical- or catheterization-based interventions had altered the patient's anatomy between the time of exercise testing and imaging. When right and left PA dimensions were available, the Nakata index (combined cross-sectional area of branch PAs divided by body surface area) was calculated for each patient. All computed tomography and magnetic resonance imaging PA measurements were performed retroactively by a single observer (SAM) with expertise in cardiac imaging, who was blinded to the patient outcome data. Branch PA measurements were made in orthogonal planes with use of the AquariusNET® system (TeraRecon, Inc.; Foster City, Calif) at the following locations: proximal branch PA (immediately distal to the main PA), narrowest branch PA, and distal branch PA (immediately proximal to the first segmental branch). The narrowest diameter and smallest cross-sectional area were used to calculate the Nakata index.
The primary predictor variable was age at completion of the Fontan procedure, and the primary outcome variable was the percentage of predicted maximum Vo2. Patients were divided into early- and late-Fontan groups on the basis of whether Fontan completion had been performed at <4 or ≥4 years of age. Data are expressed as mean ± SD for normally distributed continuous variables, median (interquartile range) for non-normally distributed continuous variables, and number (percentage) for categorical variables. Testing for normality was performed with use of the Shapiro-Wilk test. Means between 2 normally distributed groups of continuous variables were compared via the independent t test. In cases of nonparametric distribution, the Mann-Whitney U test was used for comparison of 2 groups. Comparison of 2 categorical variables was performed via the Pearson χ2 test in the event of normal distribution of variables, and the Spearman correlation in the event of nonparametric distribution. Linear regression was used to evaluate the association of continuous independent variables with exercise-performance values. Multiple regression was performed on all independent variables that achieved a P value of <0.05 in univariate analysis. All statistics were performed with use of SPSS version 19.0 (IBM Corporation; Armonk, NY).
Results
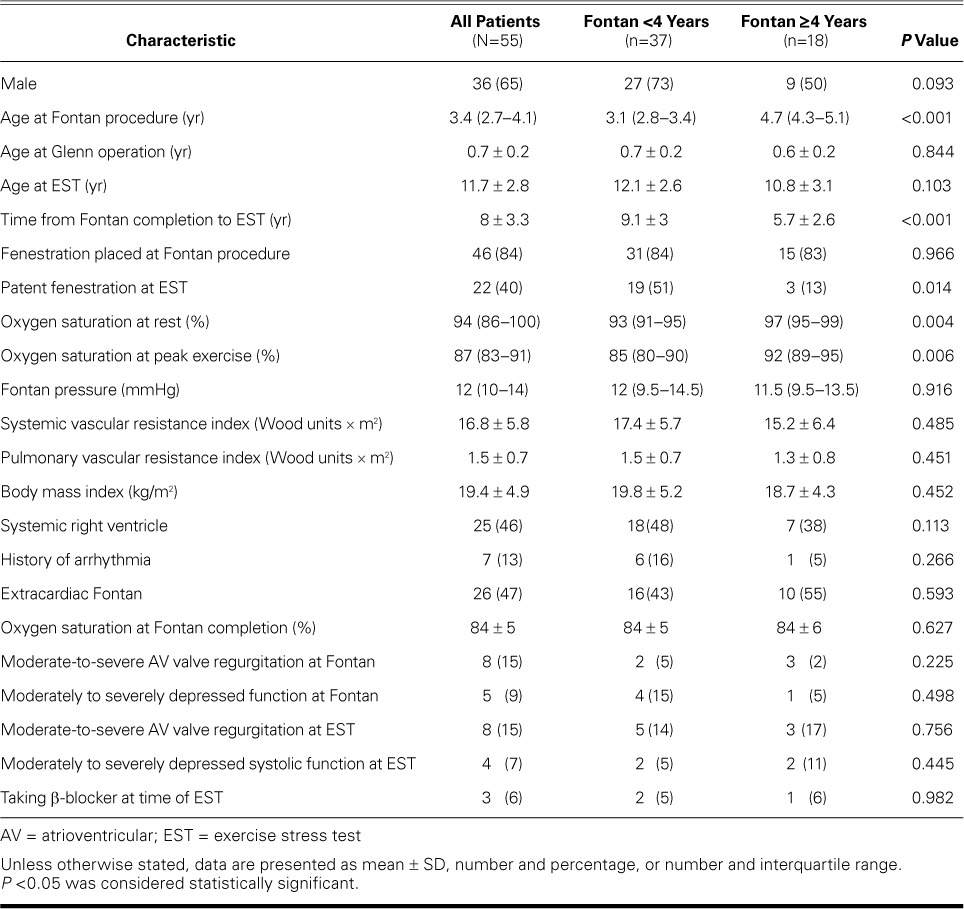
Table I shows characteristics of the study population. From 2003 through 2011, a total of 144 patients identified with Fontan circulation had undergone exercise testing. After excluding patients for a history of pacemaker placement (n=33), a respiratory exchange ratio of <1 (n=16), single-stage Fontan procedure (n=23), and age at the Glenn operation of >1 year (n=17), there were 55 remaining patients who had undergone an exercise stress test after Fontan palliation in accordance with a current surgical approach. Thirty-seven patients underwent early Fontan completion at <4 years of age, and 18 patients underwent late completion at ≥4 years of age. There were significant differences between the early- and late-Fontan groups for percentages of patients with patent fenestration at exercise testing (51% vs 13%, P =0.014), resting oxygen saturation (93% vs 97%, P=0.004), and oxygen saturation at peak exercise (85% vs 92%, P=0.006). Otherwise, there were no significant differences between the groups for the variables investigated.
TABLE I.
Characteristics of Current Fontan Patients Included in the Study
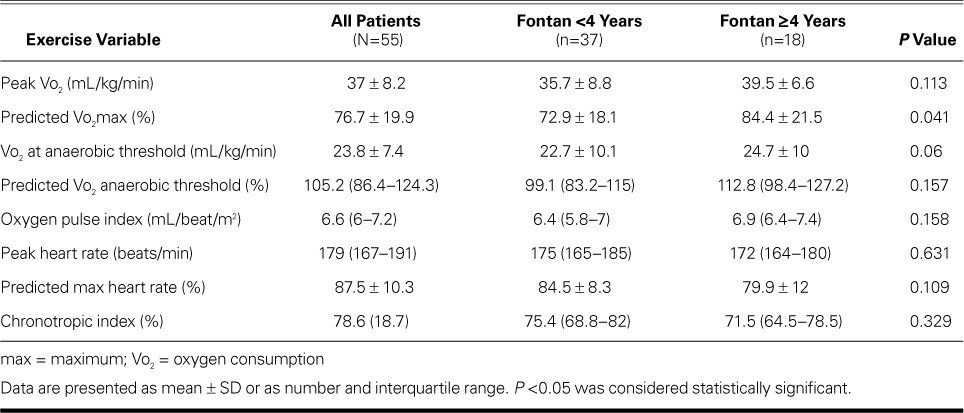
Exercise performance indices for all patients are shown in Table II. For the entire cohort, the average peak Vo2 was 37 ± 8.2 mL/kg/min, and the percentage of predicted maximum Vo2 was 76.7% ± 19.9%. Patients in whom Fontan completion was performed at <4 years of age had lower percentages of predicted maximum Vo2 than did patients in whom the Fontan was done at ≥4 years (72.9% ± 18.1% vs 84.4% ± 21.5%, P =0.041). When the percentage of predicted maximum Vo2 was dichotomized at one SD below the mean (66%), using a cutoff of 4 years of age at Fontan completion gave a specificity of 78% in predicting which patients would exercise at greater than 66% of predicted maximum Vo2.
TABLE II.
Exercise Performance Values for All Patients and for Early- and Late-Fontan Subgroups of Patients
Univariate analysis of the primary predictor and outcome variable showed a significantly positive correlation between age at Fontan completion and percentage of predicted maximum Vo2 (R=0.286, P=0.034) (Fig. 1 and Table III). When patients were excluded for either very early Fontan completion (<2 yr of age) or very late Fontan completion (>6 yr of age), there continued to be significant correlation (R=0.346, P=0.015) (Fig. 2). Table III shows that there were also positive correlations between age at Fontan completion and the secondary outcome variables of peak Vo2 (P=0.03), anaerobic threshold (P=0.04), percentage of predicted anaerobic threshold (P=0.013), and oxygen pulse index (P=0.05).
Fig. 1.
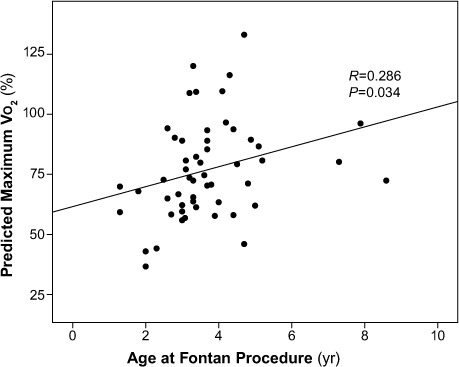
Later age at Fontan completion was positively associated with percentage of predicted maximum oxygen consumption (Vo2) (N=55).
P <0.05 was considered statistically significant.
TABLE III.
Correlation Coefficients for Age at Fontan Procedure and Values of Exercise Performance
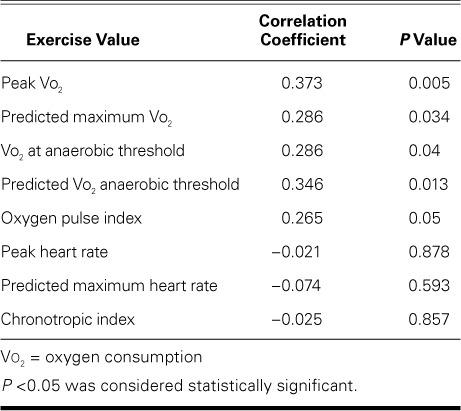
Fig. 2.
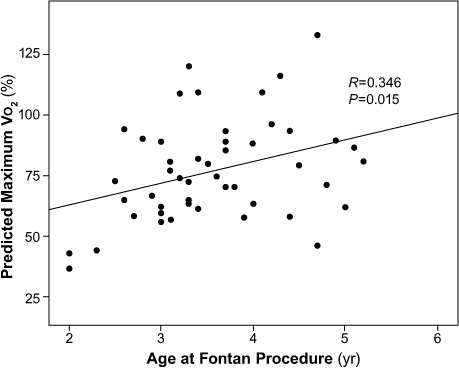
Association between age at Fontan completion and percentage of predicted maximum oxygen consumption (Vo2) (N=55), when patients <2 years and >6 years of age at Fontan completion were excluded. Later age at Fontan completion was positively associated with percentage of predicted maximum Vo2.
P <0.05 was considered statistically significant.
Table IV shows exercise-performance indices by dichotomous patient characteristics. There were no significant differences in percentage of predicted maximum Vo2 for sex, systolic function, degree of atrioventricular valve regurgitation, presence of a fenestration at exercise testing, type of Fontan procedure, or single-ventricle morphology.
TABLE IV.
Exercise Performance for Dichotomous Patient Variables
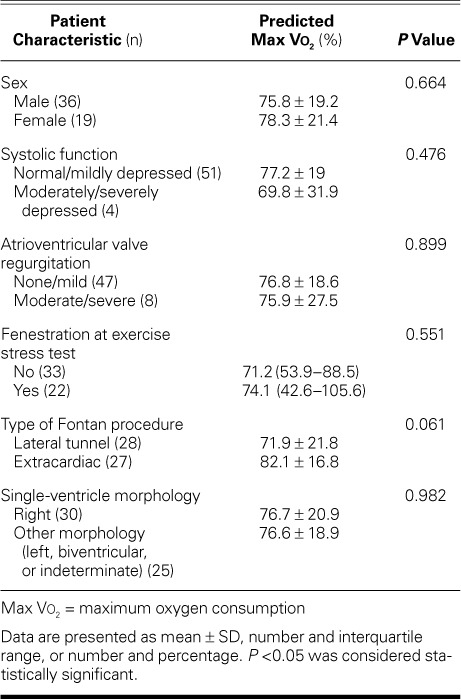
Table V shows the relationships between predictor variables and percentage of predicted maximum Vo2. Percentile of the body mass index (P=0.019) and the Nakata index (P=0.049) were positively associated with the primary outcome variable. Age at exercise testing (P=0.034) and Fontan pressure (P=0.015) showed negative associations with percentage of predicted maximum Vo2. There was also a negative correlation between the time from Fontan to stress test and percentage of predicted maximum Vo2 (P <0.001) (Fig. 3 and Table V).
TABLE V.
Association Between Candidate Predictor Variables and Percentage of Predicted Maximum Oxygen Consumption
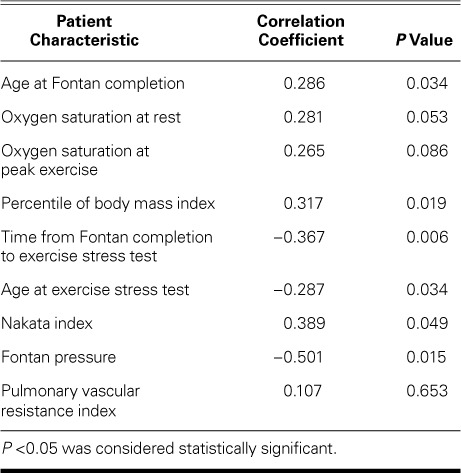
Fig. 3.
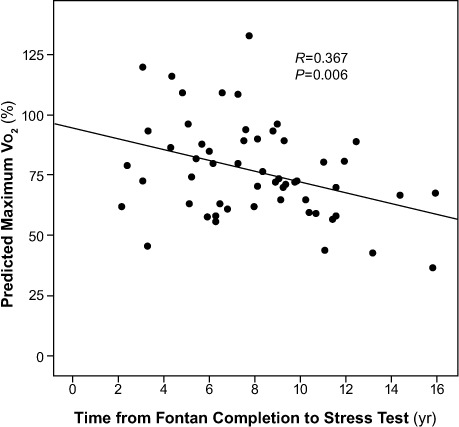
Association between time from Fontan completion to stress test and percentage of predicted maximum oxygen consumption (Vo2) (N=55). Increased time from Fontan completion to stress test was negatively associated with percentage of predicted maximum Vo2.
P <0.05 was considered statistically significant.
Multiple linear regression analysis was performed to predict percentage of predicted maximum Vo2 from age at exercise stress test, age at Fontan procedure, presence of fenestration, Nakata index, percentile of body mass index, and Fontan pressure (predictor variables that were significant in univariate analysis). Only age at exercise stress test (P=0.007) and age at Fontan procedure (P=0.03) were statistically significant predictors of percentage of predicted maximum Vo2.
Discussion
We found that older age at Fontan operation, in the current period of staged palliations, was associated with improved exercise performance. Larger Nakata indices and percentiles of body mass index likewise conferred improved exercise performance, whereas increasing age at exercise testing and elevated Fontan pressures were associated with declines in performance.
Although the Fontan surgical approach results in a stable physiology, there are attendant circulatory disadvantages, including elevated central venous pressures,10 reduced ventricular filling,11,12 and overall decreased cardiac output.13 During exertion, these shortcomings are intensified. They have been studied and described: patients with Fontan physiology have diminished maximum Vo2,14,15 decreased anaerobic threshold,14,15 and lower peak heart rate.15–17 The fact that the principal limiting factor (absence of a subpulmonary ventricle) is unalterable has necessarily placed tremendous focus on modifiable factors, including surgical timing, use of a fenestration, PA size, and even the configuration of the Fontan anastomosis.18
The age at Fontan completion has varied across surgical periods and among institutions. Before the 1990s, single-stage total cavopulmonary connection was common, and in that setting an age of >4 years was recommended for Fontan completion.19 Since the widespread adoption of the earlier ScPc, timing of the Fontan has varied from 1 to >5 years of age.20 Mahle and colleagues21 found that younger age at volume-unloading (Glenn or single-stage Fontan) is associated with improved subsequent exercise performance. In that study, however, two thirds of the patients had undergone single-stage Fontan completion without an intervening ScPc. Several other investigators have shown that younger age at Fontan is associated with improved exercise performance.1,22 Yet again, a significant portion of the study cohorts did not undergo Glenn anastomosis or other volume-unloading surgery before Fontan completion. Hence, in those reports the Fontan was the first volume-unloading procedure for a significant proportion of the study cohorts. In 2008, results of a study from the Pediatric Heart Network (PHN) showed that later Fontan is associated with a higher incidence of non-sinus rhythm and worse atrioventricular valve regurgitation, although the investigators did not show a correlation between age at Fontan and exercise performance.3 As was the case in other studies, a significant proportion of patients in the PHN study did not undergo volume-unloading before the Fontan procedure.
Comparing results of outcome studies in the single-ventricle population requires an understanding of the significant changes in palliative strategy that have occurred over recent decades. Our current study reviewed performance evaluated by exercise testing from 2003 through 2011—and indeed Fontan completion in this cohort was performed during 3 separate decades by surgeons who used both the lateral-tunnel and extracardiac techniques. A simple statement of factors associated with performance, then, can inadvertently overlook important contributions from changes in approach, including use of the ScPc, timing of the ScPc and the Fontan, and the use or abandonment of the fenestration. Our study differs from the aforementioned studies because we attempted to identify a group of single-ventricle patients undergoing Fontan palliation in accordance with the most current surgical strategy. We studied patients who, before their Fontan procedure, underwent ScPc during infancy and did not have a pacemaker. This cohort more closely reflects the patients undergoing staged palliation at the present time. Among this cohort who had undergone volume-unloading at age <1 year, older age at subsequent Fontan was associated with improved performance.
The primary benefit of Fontan completion is the attendant improvement in oxygenation. However, an understanding of the long-term drawbacks to total cavopulmonary connection is growing, particularly among caregivers of adults and adolescents with Fontan circulation. Our study highlights one important drawback to prolonged Fontan circulation: a gradual, progressive deterioration in exercise performance. This diminution has been characterized in other studies.17,23 In addition, central venous pressures increase over time after Fontan completion.24 Elevation of venous pressures exerts deleterious effects upon renal, intestinal (protein-losing enteropathy), and hepatic function.25 There is evidence that, after Fontan completion, hepatic dysfunction ensues. Several investigators have shown that hepatic synthetic dysfunction,26 coagulopathy,27 and cirrhosis28,29 are time-dependent phenomena after the Fontan operation.
Whereas the benefits of early Fontan are few, the drawbacks of long-standing Fontan circulation appear to be numerous. Our data suggest that delaying the Fontan operation until after 4 years of age, when feasible, is preferable for most patients. This delay decreases the total time that a patient is exposed to the imperfect physiology imposed by the total cavopulmonary connection. Although not investigated in this study, there is most likely an age at which progressive desaturation necessitates Fontan completion. We therefore suggest an ideal but limited window of time for the Fontan completion, beginning at 4 years of age.
Increasing the age at Fontan completion was also positively correlated with oxygen pulse index. Because the arteriovenous oxygen difference at peak exercise is similar among patients, the oxygen pulse index has been postulated as a surrogate for stroke volume. A publication in 2008 from the PHN showed that oxygen pulse was the most important factor accounting for variance in the percentage of predicted maximum Vo2.4 Our data suggest that the reason for improved exercise performance after delayed Fontan completion is due in part to preserved stroke volume.
Although more patients in our early-Fontan-completion group had a fenestration, there was no difference in exercise performance in association with the presence of a fenestration at time of exercise testing. This is similar to data published in 2011 from the PHN.30 In addition, oxygen saturations at rest and peak exercise were different between groups, which were accounted for by the presence or absence of a fenestration. However, we did not find statistically significant associations between oxygen saturations and exercise performance, a result also encountered by the PHN.4 Although our study was not designed to judge the role of fenestration patency and its impact on exercise performance, our data do not support the practice of routinely closing fenestrations for the purpose of improving the percentage of predicted maximum Vo2.
We also found that the percentage of predicted maximum Vo2 was diminished in patients with a smaller Nakata index. In addition, we found a negative association between Fontan pressure and exercise performance. Computerized flow models have demonstrated increased Fontan circulatory power loss when PA caliber is reduced.31 The correlations between both Nakata index and Fontan pressure with exercise performance might provide a rationale for intervening on hypoplastic and stenotic branch PAs to promote unobstructed Fontan physiology. Future studies investigating the impact of such interventions on Fontan patients at peak exercise would clarify the benefits of such an approach.
Although right ventricular morphology has been shown to result in a worse composite functional state, which includes exercise capacity, ventricular morphology was not associated with any exercise performance value in our study.32 This finding is similar to those previously reported.13 A larger study from the PHN showed a weak association between exercise performance and ventricular morphology, with the left-ventricle subgroup having a higher percentage of predicted maximum Vo2.3
Our study failed to uncover any relationship between either ventricular systolic function or valvar regurgitation and exercise performance. These findings are consistent with those of previous studies.3 Because only a small proportion of our cohort had ventricular or valvar dysfunction, our study might have been too underpowered to determine any important relationship.
Because of the complexity of the Fontan circulation, no single independent variable can be expected to account for all the variance in exercise performance. As this imperfect circulation is incrementally improved, small gains in modifiable factors have become the goal. We therefore did not find large correlation coefficients for any single independent variable.
Limitations. There were several limitations to this study. Our institution does not include pulmonary function testing with all exercise tests. An appropriately functioning diaphragm provides a driving force for pulmonary blood flow in the absence of a subpulmonary ventricle.33 In addition, only patients who were able to perform treadmill exercise testing were included. A significant number of patients might have been excluded because of death, deconditioning, or musculoskeletal limitations.
In conclusion, later completion of the Fontan procedure might be associated with improved exercise capacity in patients who received palliation in accordance with recent surgical strategy. Our data suggest that delaying the Fontan operation until after 4 years of age, when feasible, is preferable for most patients.
Acknowledgments
We thank William A. Payne, BS, from the Department of Pediatrics, Lillie Abercrombie Section of Pediatric Cardiology, Texas Children's Hospital, Baylor College of Medicine, for his help with data acquisition.
Footnotes
From: Department of Pediatrics, Lillie Abercrombie Section of Pediatric Cardiology, Texas Children's Hospital, Baylor College of Medicine (Drs. Bolin, Maskatia, and Petit); and Department of Exercise Science (Ms Tate), Texas Children's Hospital; Houston, Texas 77030
Dr. Petit is now at the Section of Pediatric Cardiology, Children's Healthcare of Atlanta, Emory University School of Medicine, Atlanta, Georgia.
References
- 1.Ohuchi H, Yasuda K, Hasegawa S, Miyazaki A, Takamuro M, Yamada O et al. Influence of ventricular morphology on aerobic exercise capacity in patients after the Fontan operation. J Am Coll Cardiol. 2001;37(7):1967–74. doi: 10.1016/s0735-1097(01)01266-9. [DOI] [PubMed] [Google Scholar]
- 2.Giardini A, Hager A, Pace Napoleone C, Picchio FM. Natural history of exercise capacity after the Fontan operation: a longitudinal study. Ann Thorac Surg. 2008;85(3):818–21. doi: 10.1016/j.athoracsur.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 3.Anderson PA, Sleeper LA, Mahony L, Colan SD, Atz AM, Breitbart RE et al. Contemporary outcomes after the Fontan procedure: a Pediatric Heart Network multicenter study. J Am Coll Cardiol. 2008;52(2):85–98. doi: 10.1016/j.jacc.2008.01.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paridon SM, Mitchell PD, Colan SD, Williams RV, Blaufox A, Li JS et al. A cross-sectional study of exercise performance during the first 2 decades of life after the Fontan operation. J Am Coll Cardiol. 2008;52(2):99–107. doi: 10.1016/j.jacc.2008.02.081. [DOI] [PubMed] [Google Scholar]
- 5.Fernandes SM, Alexander ME, Graham DA, Khairy P, Clair M, Rodriguez E et al. Exercise testing identifies patients at increased risk for morbidity and mortality following Fontan surgery. Congenit Heart Dis. 2011;6(4):294–303. doi: 10.1111/j.1747-0803.2011.00500.x. [DOI] [PubMed] [Google Scholar]
- 6.Inuzuka R, Diller GP, Borgia F, Benson L, Tay EL, Alonso-Gonzalez R et al. Comprehensive use of cardiopulmonary exercise testing identifies adults with congenital heart disease at increased mortality risk in the medium term. Circulation. 2012;125(2):250–9. doi: 10.1161/CIRCULATIONAHA.111.058719. [DOI] [PubMed] [Google Scholar]
- 7.Cumming GR, Everatt D, Hastman L. Bruce treadmill test in children: normal values in a clinic population. Am J Cardiol. 1978;41(1):69–75. doi: 10.1016/0002-9149(78)90134-0. [DOI] [PubMed] [Google Scholar]
- 8.Cooper DM, Weiler-Ravell D. Gas exchange response to exercise in children. Am Rev Respir Dis. 1984;129(2 Pt 2):S47–8. doi: 10.1164/arrd.1984.129.2P2.S47. [DOI] [PubMed] [Google Scholar]
- 9.Robergs RA, Landwehr R. The surprising history of the “HRmax=220-age” equation. JEPonline. 2002;5(2):1–10. Available from: http://www.cyclingfusion.com/pdf/220-Age-Origins-Problems.pdf. [Google Scholar]
- 10.Kaulitz R, Luhmer I, Bergmann F, Rodeck B, Hausdorf G. Sequelae after modified Fontan operation: postoperative haemodynamic data and organ function. Heart. 1997;78(2):154–9. doi: 10.1136/hrt.78.2.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krishnan US, Taneja I, Gewitz M, Young R, Stewart J. Peripheral vascular adaptation and orthostatic tolerance in Fontan physiology. Circulation. 2009;120(18):1775–83. doi: 10.1161/CIRCULATIONAHA.109.854331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hsia TY, Khambadkone S, Deanfield JE, Taylor JF, Migliavacca F, De Leval MR. Subdiaphragmatic venous hemodynamics in the Fontan circulation. J Thorac Cardiovasc Surg. 2001;121(3):436–47. doi: 10.1067/mtc.2001.112527. [DOI] [PubMed] [Google Scholar]
- 13.Gewillig M, Brown SC, Eyskens B, Heying R, Ganame J, Budts W et al. The Fontan circulation: who controls cardiac output? Interact Cardiovasc Thorac Surg. 2010;10(3):428–33. doi: 10.1510/icvts.2009.218594. [DOI] [PubMed] [Google Scholar]
- 14.Gewillig MH, Lundstrom UR, Bull C, Wyse RK, Deanfield JE. Exercise responses in patients with congenital heart disease after Fontan repair: patterns and determinants of performance. J Am Coll Cardiol. 1990;15(6):1424–32. doi: 10.1016/s0735-1097(10)80034-8. [DOI] [PubMed] [Google Scholar]
- 15.Joshi VM, Carey A, Simpson P, Paridon SM. Exercise performance following repair of hypoplastic left heart syndrome: a comparison with other types of Fontan patients. Pediatr Cardiol. 1997;18(5):357–60. doi: 10.1007/s002469900199. [DOI] [PubMed] [Google Scholar]
- 16.Durongpisitkul K, Driscoll DJ, Mahoney DW, Wollan PC, Mottram CD, Puga FJ, Danielson GK. Cardiorespiratory response to exercise after modified Fontan operation: determinants of performance. J Am Coll Cardiol. 1997;29(4):785–90. doi: 10.1016/s0735-1097(96)00568-2. [DOI] [PubMed] [Google Scholar]
- 17.Harrison DA, Liu P, Walters JE, Goodman JM, Siu SC, Webb GD et al. Cardiopulmonary function in adult patients late after Fontan repair. J Am Coll Cardiol. 1995;26(4):1016–21. doi: 10.1016/0735-1097(95)00242-7. [DOI] [PubMed] [Google Scholar]
- 18.de Zelicourt DA, Haggerty CM, Sundareswaran KS, Whited BS, Rossignac JR, Kanter KR et al. Individualized computer-based surgical planning to address pulmonary arteriovenous malformations in patients with a single ventricle with an interrupted inferior vena cava and azygous continuation. J Thorac Cardiovasc Surg. 2011;141(5):1170–7. doi: 10.1016/j.jtcvs.2010.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Norwood WI, Jacobs ML. Fontan's procedure in two stages. Am J Surg. 1993;166(5):548–51. doi: 10.1016/s0002-9610(05)81151-1. [DOI] [PubMed] [Google Scholar]
- 20.Wallace MC, Jaggers J, Li JS, Jacobs ML, Jacobs JP, Benjamin DK et al. Center variation in patient age and weight at Fontan operation and impact on postoperative outcomes. Ann Thorac Surg. 2011;91(5):1445–52. doi: 10.1016/j.athoracsur.2010.11.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mahle WT, Wernovsky G, Bridges ND, Linton AB, Paridon SM. Impact of early ventricular unloading on exercise performance in preadolescents with single ventricle Fontan physiology. J Am Coll Cardiol. 1999;34(5):1637–43. doi: 10.1016/s0735-1097(99)00392-7. [DOI] [PubMed] [Google Scholar]
- 22.Shiraishi S, Yagihara T, Kagisaki K, Hagino I, Ohuchi H, Kobayashi J, Kitamura S. Impact of age at Fontan completion on postoperative hemodynamics and long-term aerobic exercise capacity in patients with dominant left ventricle. Ann Thorac Surg. 2009;87(2):555–61. doi: 10.1016/j.athoracsur.2008.11.015. [DOI] [PubMed] [Google Scholar]
- 23.Cohen MI, Wernovsky G, Vetter VL, Wieand TS, Gaynor JW, Jacobs ML et al. Sinus node function after a systematically staged Fontan procedure. Circulation. 1998;98(19 Suppl):II352–9. [PubMed] [Google Scholar]
- 24.Ohuchi H, Ono S, Tanabe Y, Fujimoto K, Yagi H, Sakaguchi H et al. Long-term serial aerobic exercise capacity and hemodynamic properties in clinically and hemodynamically good, “excellent”, Fontan survivors. Circ J. 2012;76(1):195–203. doi: 10.1253/circj.cj-11-0540. [DOI] [PubMed] [Google Scholar]
- 25.Anne P, Du W, Mattoo TK, Zilberman MV. Nephropathy in patients after Fontan palliation. Int J Cardiol. 2009;132(2):244–7. doi: 10.1016/j.ijcard.2007.11.079. [DOI] [PubMed] [Google Scholar]
- 26.Baek JS, Bae EJ, Ko JS, Kim GB, Kwon BS, Lee SY et al. Late hepatic complications after Fontan operation; non-invasive markers of hepatic fibrosis and risk factors. Heart. 2010;96(21):1750–5. doi: 10.1136/hrt.2010.201772. [DOI] [PubMed] [Google Scholar]
- 27.Tomita H, Yamada O, Ohuchi H, Ono Y, Arakaki Y, Yagihara T, Echigo S. Coagulation profile, hepatic function, and hemodynamics following Fontan-type operations. Cardiol Young. 2001;11(1):62–6. doi: 10.1017/s1047951100012439. [DOI] [PubMed] [Google Scholar]
- 28.Ghaferi AA, Hutchins GM. Progression of liver pathology in patients undergoing the Fontan procedure: chronic passive congestion, cardiac cirrhosis, hepatic adenoma, and hepatocellular carcinoma. J Thorac Cardiovasc Surg. 2005;129(6):1348–52. doi: 10.1016/j.jtcvs.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 29.Shah H, Kuehl K, Sherker AH. Liver disease after the Fontan procedure: what the hepatologist needs to know. J Clin Gastroenterol. 2010;44(6):428–31. doi: 10.1097/MCG.0b013e3181d476fc. [DOI] [PubMed] [Google Scholar]
- 30.Atz AM, Travison TG, McCrindle BW, Mahony L, Quartermain M, Williams RV et al. Late status of Fontan patients with persistent surgical fenestration. J Am Coll Cardiol. 2011;57(24):2437–43. doi: 10.1016/j.jacc.2011.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dasi LP, Krishnankuttyrema R, Kitajima HD, Pekkan K, Sundareswaran KS, Fogel M et al. Fontan hemodynamics: importance of pulmonary artery diameter. J Thorac Cardiovasc Surg. 2009;137(3):560–4. doi: 10.1016/j.jtcvs.2008.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Williams IA, Sleeper LA, Colan SD, Lu M, Stephenson EA, Newburger JW et al. Functional state following the Fontan procedure. Cardiol Young. 2009;19(4):320–30. doi: 10.1017/S1047951109990382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Penny DJ, Redington AN. Doppler echocardiographic evaluation of pulmonary blood flow after the Fontan operation: the role of the lungs. Br Heart J. 1991;66(5):372–4. doi: 10.1136/hrt.66.5.372. [DOI] [PMC free article] [PubMed] [Google Scholar]


