Abstract
Introduction
Maximal Inspiratory Pressure (MIP) is considered an effective method to estimate strength of inspiratory muscles, but still leads to false positive diagnosis. Although MIP assessment with unidirectional expiratory valve method has been used in patients undergoing mechanical ventilation, no previous studies investigated the application of this method in subjects without artificial airway.
Objectives
This study aimed to compare the MIP values assessed by standard method (MIPsta) and by unidirectional expiratory valve method (MIPuni) in subjects with spontaneous breathing without artificial airway. MIPuni reproducibility was also evaluated.
Methods
This was a crossover design study, and 31 subjects performed MIPsta and MIPuni in a random order. MIPsta measured MIP maintaining negative pressure for at least one second after forceful expiration. MIPuni evaluated MIP using a unidirectional expiratory valve attached to a face mask and was conducted by two evaluators (A and B) at two moments (Tests 1 and 2) to determine interobserver and intraobserver reproducibility of MIP values. Intraclass correlation coefficient (ICC[2,1]) was used to determine intraobserver and interobserver reproducibility.
Results
The mean values for MIPuni were 14.3% higher (-117.3 ± 24.8 cmH2O) than the mean values for MIPsta (-102.5 ± 23.9 cmH2O) (p<0.001). Interobserver reproducibility assessment showed very high correlation for Test 1 (ICC[2,1] = 0.91), and high correlation for Test 2 (ICC[2,1] = 0.88). The assessment of the intraobserver reproducibility showed high correlation for evaluator A (ICC[2,1] = 0.86) and evaluator B (ICC[2,1] = 0.77).
Conclusions
MIPuni presented higher values when compared with MIPsta and proved to be reproducible in subjects with spontaneous breathing without artificial airway.
Introduction
Maximal Inspiratory Pressure (MIP) is considered an effective method to estimate strength of inspiratory muscles [1,2]. This method has been widely used to evaluate the severity and follow-up of inspiratory muscle weakness in several clinical conditions [2–5], as well as for training load prescription and monitoring the outcomes of inspiratory muscle training programs [6–8]. In Intensive Care Units (ICU), MIP has also been used as a predictive index for successful weaning from mechanical ventilation [9,10] and, more recently, as a parameter for early detection of muscle weakness acquired in ICU [11].
The MIP evaluated by standard method (MIPsta) proposed by Black and Hyatt [1] is still the most common method for assessment of maximal respiratory pressures. In this method, MIP is quantified by maintaining the negative pressure for at least one second, against an occluded airway, after a forceful expiration near residual volume. Although this method has been considered well tolerated by patients and easy to perform, the measurement depends on the understanding and cooperation of individuals to perform really maximal respiratory efforts [2,12]. Low values (false positive diagnosis) are not uncommon and may represent poor technique of inspiratory effort instead of muscle weakness [13]. Furthermore, methodological variations such as number of necessary maneuvers, lung volume from which the maneuvers have been made, and types of equipment or interface may also compromise the reliability of measures [2,12], creating a discrepancy between the reference values [14–16].
To overcome the need for collaboration during MIPsta, Marini et al. [17] developed a method which shows optimization of inspiratory effort in critically ill and poorly cooperative patients undergoing mechanical ventilation. These authors proposed the use of a unidirectional expiratory valve, using low resistance to allow expiration in a selective way, while inspiration was prevented–MIP evaluated by unidirectional expiratory valve method (MIPuni). With inspiration blocked, respiratory efforts deflate the chest, making the patients start successive inspiratory efforts increasingly closer to residual volume, stimulating the generation of negative pressure. This method involves less patient-evaluator coordination because it represents a physiological response (increase of the respiratory drive after a prior insufficient inspiration), and can be used in patients unable to collaborate to perform the maneuver by MIPsta [18].
Some authors [19,20] compared MIPsta and MIPuni in mechanically ventilated patients, and observed that MIPuni was significantly higher when compared to MIPsta, demonstrating that MIPuni optimizes inspiratory muscle capacity of action. However, to our knowledge, no study has reported using MIPuni in subjects under spontaneous breathing without artificial airway. We hypothesized that the superiority of this method in the optimization of maximal inspiratory effort may also occur in these conditions, with a high reproducibility and better repeatability compared with MIPsta. In this context, this study aimed to compare MIPsta and MIPuni in subjects under spontaneous breathing without artificial airway. MIPuni reproducibility and repeatability were also evaluated.
Methods
Subjects
We studied 31 subjects who met the inclusion criteria as follows: (1) age 18–60 years; (2) normal pulmonary function tests (FVC and FEV1 ≥ 80% of predicted and FEV1/FVC ≥ 0.7); (3) non-smokers; (4) absence of cardiopulmonary diseases; and (5) no prior contact with the methods tested. Exclusion criteria were: inability to carry out evaluations within the criteria for technical acceptability. The study was approved by the Sírio-Libanês Hospital Ethics Committee (HSL2011/17), and all subjects provided written informed consent.
Set-up and measurements
Prior to MIP measurements, the subjects underwent assessment of personal history and lifestyle habits through a standard questionnaire, anthropometric evaluation, and pulmonary function test. The level of discomfort during the measurements in both MIP methods was also evaluated.
Pulmonary function test
The spirometry was performed using a portable digital spirometer (model Koko PFtesting; nSpire Healthy; Longmont; Colorado; USA), previously calibrated according to ATS and ERS recommendations [21]. The spirometric parameters were presented as absolute values and as a percentage of the predicted [22].
Maximal inspiratory pressure
MIP values were obtained with a digital vacuum manometer (model MVD500; Microhard; Porto Alegre; RS; Brazil). MIPsta followed the Brazilian Society of Pulmonology and Phthisiology guidelines [12], using a digital vacuum manometer attached to a mouthpiece with a 2-mm diameter air-leak opening. MIPsta was measured from the volume closest to residual volume by instructing the individuals to realize a forceful expiration followed by a maximal inspiration. For this evaluation, 10 maneuvers [23,24] were realized, respecting a rest period of one minute between them, in order to obtain three acceptable maneuvers including at least two repeatable ones. The highest value among the repeatable maneuvers was considered for the study.
MIPuni was performed by using the digital vacuum manometer attached to a unidirectional expiratory valve and a face mask (Fig 1). The subjects were seated on a comfortable chair and remained attached to the mask for 20 seconds. During this period, all individuals were encouraged to make maximal respiratory efforts. For this evaluation, three maneuvers [19,20] were performed, respecting a rest period of one minute between them, and the highest value among the maneuvers was considered for the study.
Fig 1. Materials used for MIP assessment by unidirectional expiratory valve method: (1) unidirectional expiratory valve; (2) straight connector; (3) T-tube; (4) face mask; (5) digital vacuum manometer.
Experimental protocol
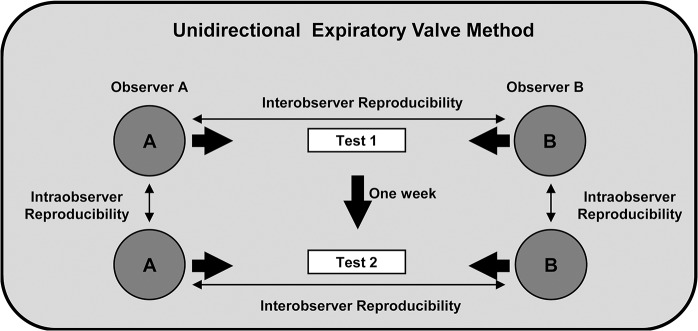
This study used a crossover design. MIP measurements were obtained by MIPsta and MIPuni in all subjects, in a random order of application previously defined through a raffle. A 20-minute rest period was allowed between each method. MIPsta was performed in a single moment (Test 1), and conducted by a single evaluator (evaluator A), who was kept blind to the results. In order to analyze the inter- and intraobserver reproducibility of MIPuni, this method was carried out by two evaluators (A and B), independently and in a random order, at two moments (Tests 1 and 2), at least one week apart (Fig 2). Repeatability was determined for each method (MIPsta and MIPuni) considering the first and the last measurements from each participant obtained by evaluator A. The technical acceptability and recording of the values obtained in MIP maneuvers were performed by a third evaluator, so that evaluators A and B were kept blind to the results. The same conditions were maintained to perform MIPuni, both in Test 1 and Test 2: time of day, position, orientations and randomized order of the evaluators.
Fig 2. Process of MIPuni assessment.
The discomfort caused during MIP assessment in both methods was measured by a visual analogue scale [25] of 10 cm, in which the "zero" point corresponded to "no discomfort", and point "ten" matched "maximum discomfort." The subjects were asked to mark a point on the scale, quantifying this subjective measure.
Statistical analysis
Data were analyzed using SPSS for Windows, version 17.0 (IMB SPSS Statistics; IBM; Armonk; New York; USA). A sample size of 29 subjects was calculated using the results from a previous study [19] to detect a difference in MIPuni of up to 14.06 with a standard deviation of 18.69 compared with MIPsta (alpha value of 0.05 and a power of 0.8). Shapiro-Wilk test was used to analyze data distribution. The mean values of MIPsta and MIPuni were compared using the paired Student's t-test. This test was also used for comparing the mean values of MIPuni for both evaluators (A and B), in both assessments (Tests 1 and 2). The inter- and intraobserver reproducibility of MIPuni was established by the intraclass correlation coefficient (ICC[2,1]−a two-way random effects model with absolute agreement). The classification system by Munro [26] was used to interpret the ICC[2,1]: 0.0 to 0.25—little if any; 0.26 to 0.49—low; 0.50 to 0.69 –moderate; 0.70 to 0.89—high; 0.90 to 1.00—very high. Interobserver and intraobserver reproducibility was also evaluated by Bland-Altman plots [27] in order to better visualize the measurement agreement. To analyze repeatability of the values in both MIPsta and MIPuni, the first and the last measurements of each participant were considered to calculate ICC[2,1] in the first assessment (Test 1). The Bland-Altman repeatability coefficient [27] was also calculated for MIPsta and MIPuni values. The discomfort caused by both MIPuni and MIPsta was compared by using the Wilcoxon test. The significance level was established at 5%.
Results
Thirty-one subjects were assessed for eligibility: 17 female and 14 male, with a mean age of 30.8 ± 6.2 years. Anthropometric characteristics and pulmonary function are shown in Table 1.
Table 1. Anthropometric characteristics and pulmonary function variables.
n: number of subjects; kg: kilograms; m: meters; BMI: body mass index. FVC (% predicted): estimated percentage of predicted forced vital capacity; FEV1 (% predicted): estimated percentage of predicted forced expiratory volume in the first second; FEF 25–75% (% predicted): estimated percentage of predicted mean forced expiratory flow between 25% and 75% of FVC; VC (% predicted): estimated percentage of predicted vital capacity; IC: inspiratory capacity (L: liter); ERV: expiratory reserve volume.
| Variables | Mean ± Standard deviation(n = 31) |
|---|---|
| Age (years) | 30.8 ± 6.2 |
| Body mass (kg) | 71.8 ± 13.8 |
| Height (m) | 1.70 ± 0.08 |
| BMI (kg/m2) | 24.5 ± 3.5 |
| Pulmonary function | |
| FVC (% predicted) | 92.4 ± 12.1 |
| FEV1 (% predicted) | 93.3 ± 10.6 |
| FEV1/FVC (% predicted) | 101.0 ± 7.2 |
| FEF 25–75% (% predicted) | 95.1 ± 21.1 |
| VC (% predicted) | 90.1 ± 11.1 |
| IC (L) | 2.95 ± 0.63 |
| ERV (L) | 1.02 ± 0.45 |
MIPsta x MIPuni
MIPsta (-102.5 ± 23.9 cmH2O) presented a statistically significant difference when compared to MIPuni (-117.3 ± 24.8 cmH2O; p<0.001). MIPuni was 14.9 ± 19.6 cmH2O above MIPsta in absolute values (percentage difference mean of 16.9 ± 24.4%). By means of the Bland-Altman plots, a low agreement between MIPsta and MIPuni absolute values was observed, since the mean difference between obtained values was not close to zero. The dispersion of differences between values was also shown by Bland-Altman plots, with limits of agreement of -23.6 and +53.3 cmH2O (Fig 3). However, a significant positive linear correlation between the methods was observed: MIPuni = (0.701 x MIPsta) + 45.53 (r = 0.68; p<0.001).
Fig 3. Bland-Altman plots of the agreement between MIPsta and MIPuni values (absolute values).

MIPsta: Maximal inspiratory pressure evaluated by standard method; MIPuni: Maximal inspiratory pressure evaluated by unidirectional expiratory valve method; X axis: Mean of MIP values obtained by MIPuni and MIPsta for each subject of the study (MIPuni value + MIPsta value /2); Y axis: Difference between MIP values obtained by MIPuni and MIPsta for each subject (MIPuni value–MIPsta value); UL: Upper limit; LL: Lower limit.
Inter- and intraobserver reproducibility
MIPuni values obtained by evaluators A and B in both tests are shown in Table 2. No statistically significant difference was found when comparing MIPuni assessed by evaluators A and B, both in Test 1 (p = 0.19) and in Test 2 (p = 0.15). Also, no statistically significant difference was found when comparing MIPuni assessed by evaluator A, in Tests 1 and 2 (p = 0.10), and when comparing MIPuni assessed by evaluator B, in Tests 1 and 2 (p = 0.13).
Table 2. MIP evaluated by unidirectional expiratory valve method.
n: number of subjects; cmH20: centimeters of water.
| MIPMean ± Standard deviation | ||
|---|---|---|
| Test 1 | Evaluator A | -117.3 ± 24.8 |
| (n = 31) | ||
| Evaluator B | -114.9 ± 23.7 | |
| Test 2 | Evaluator A | -113.5 ± 25.0 |
| (n = 31) | ||
| Evaluator B | -110.2 ± 26.6 | |
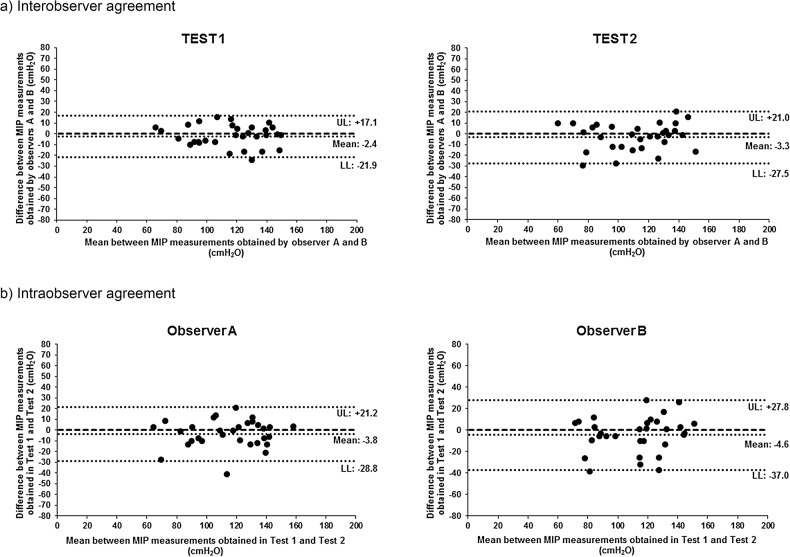
In the interobserver reproducibility evaluation, ICC[2,1] was very high between MIPuni obtained by evaluators A and B, in Test 1 (ICC[2,1] = 0.91). In Test 2, ICC[2,1] was high between the values obtained by these evaluators (ICC[2,1] = 0.88). In the intraobserver reproducibility evaluation, ICC[2,1] was high for both MIPuni obtained by evaluator A (ICC[2,1] = 0.86) and that obtained by evaluator B (ICC[2,1] = 0.77) (Table 3).
Table 3. Inter- and intraobserver reproducibility of unidirectional expiratory valve method.
ICC[2,1]: intraclass correlation coefficient; CI 95%: 95% confidence interval, p: level of significance.
| ICC[2,1] | CI 95% | p | ||
|---|---|---|---|---|
| Interobserver reproducibility | Test 1 | 0.91 | 0.83–0.96 | <0.001 |
| Test 2 | 0.88 | 0.77–0.94 | <0.001 | |
| Intraobserver reproducibility | Evaluator A | 0.86 | 0.74–0.93 | <0.001 |
| Evaluator B | 0.77 | 0.57–0.88 | <0.001 |
The Bland-Altman plots showed the agreement between MIPuni values obtained by evaluators A and B in both assessments (interobserver agreement), and also showed measurement agreement between MIP values obtained by each evaluator at two moments–Tests 1 and 2 (intraobserver agreement) (Fig 4).
Fig 4. Bland-Altman plots of the inter- and intraobserver agreement between MIPuni values (absolute values).
a) X axis: Mean of MIP values obtained by evaluators A and B for each subject of the study (Value by evaluator A + Value by evaluator B /2); Y axis: Difference between MIP values obtained by evaluators A and B for each subject (Value by evaluator B–Value by evaluator A). b) X axis: Mean of MIP values obtained by evaluator A or B for each subject in Tests 1 and 2 (Value by evaluator A or B in Test 1 + Value by evaluator A or B in Test 2 /2); Y axis: Difference between MIP values obtained by evaluator A or B for each subject in Tests 1 and 2 (Value by evaluator A or B in Test 2—Value by evaluator A or B in Test 1). UL: Upper limit; LL: Lower limit.
Repeatability of MIPsta and MIPuni
MIPsta repeatability assessment showed moderate ICC[2,1] (ICC[2,1] = 0.60). On the other hand, MIPuni repeatability assessment showed very high ICC[2,1] both by evaluator A (ICC[2,1] = 0.94) and by evaluator B (ICC[2,1] = 0.91) (Table 4).
Table 4. MIP measurement repeatability.
ICC[2,1]: intraclass correlation coefficient; CI 95%: 95% confidence interval, p: level of significance.
| ICC[2,1] | CI 95% | p | ||
|---|---|---|---|---|
| MIPsta | 0.60 | 0.32–0.79 | <0.001 | |
| Repeatability | MIPuni—Evaluator A | 0.94 | 0.88–0.97 | <0.001 |
| MIPuni—Evaluator B | 0.91 | 0.83–0.96 | <0.001 |
The Bland-Altman repeatability coefficient was 49.6 cmH2O for MIPsta. In MIPuni, the Bland-Altman repeatability coefficient obtained by evaluator A was 17.1 cmH2O and by evaluator B it was 21.8 cmH2O (Fig 5).
Fig 5. Bland-Altman plots of the agreement between MIP values obtained by standard method and by unidirectional expiratory valve method (absolute values).
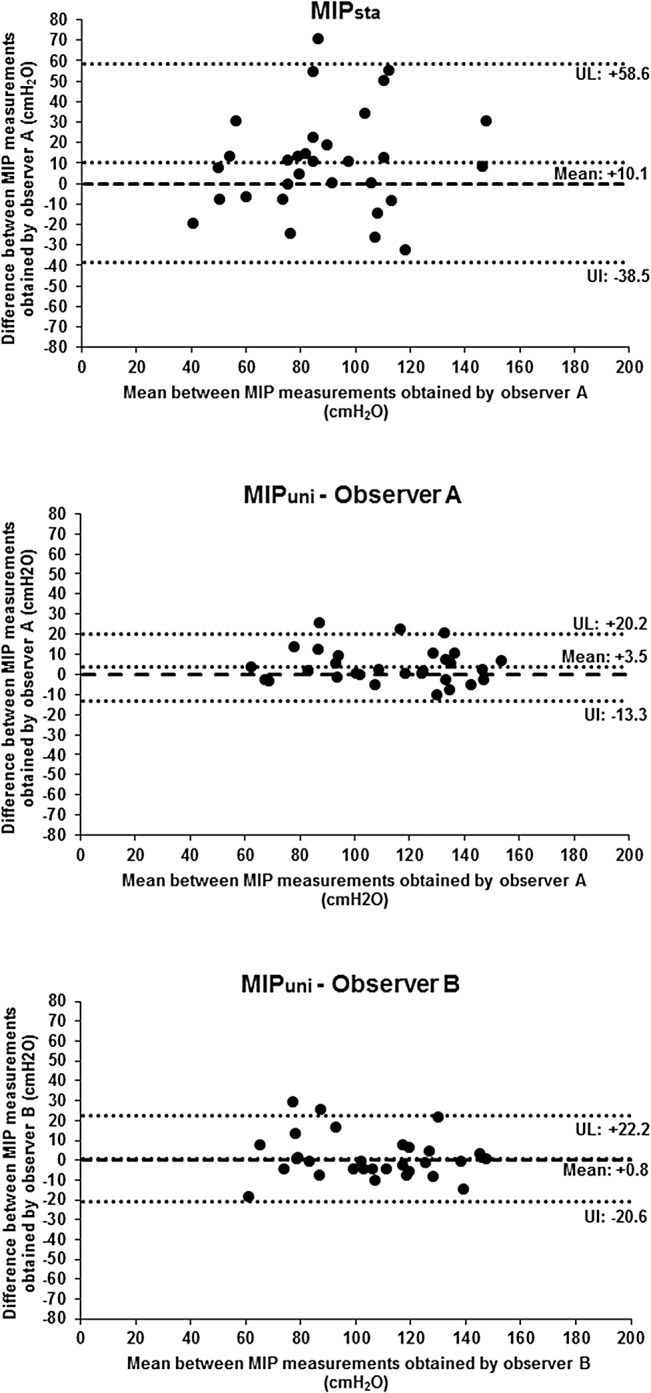
X axis: Mean between the first and last MIP values obtained by each method for each subject (First value + Last value /2); Y axis: Difference between the last and first MIP value obtained by each method for each subject (Last value–First value); UL: Upper limit; LL: Lower limit.
The discomfort reported during MIPuni was higher (5.7 ± 2.8 cm) compared to MIPsta (1.3 ± 1.6 cm; p<0.001).
Discussion
The present study aimed to compare MIPsta and MIPuni in subjects under spontaneous breathing without artificial airway. The results showed significantly higher values of MIPuni when compared to MIPsta values in this population. Furthermore, MIPuni proved to be an inter- and intraobserver reproducible method.
Previous studies [19,20] have also demonstrated superiority of MIPuni when compared to MIPsta but in patients with artificial airway. Possible explanations for the higher MIP values obtained by MIPuni were mentioned by Caruso et al [19]. According to the authors, the respiratory drive increase during maneuvers might be due to the blockage of inspiration by using a unidirectional expiratory valve, which would cause carbon dioxide retention and subsequent release of chemical stimuli after the previous ineffective inspiration. In MIPsta, however, the respiratory drive would depend more on the collaboration of subjects than on physiologic response. Another plausible explanation is that, with the use of a unidirectional expiratory valve and the 20-second blockage of inspiration, patients could be forced to progressively reduce pulmonary volumes, performing inspiratory effort at a pulmonary volume closer to residual volume, optimizing the inspiratory muscle capacity of action (force–length relationship). It is important to mention that, both in MIPsta and MIPuni, the negative pressure generated when the inspiratory effort is realized from the volume closest to residual volume reflects not only the pressure developed by the respiratory muscles, but also the passive elastic recoil pressure of the respiratory system including the lung and chest wall. According to the ATS [2], subjects find it easier to maximize their inspiratory efforts at low lung volumes; therefore, by convention and to standardize measurement, MIP is measured at or close to residual volume.
In the present study, it is worth noting that, for MIPsta evaluation, a mouthpiece was used as interface, while in MIPuni a face-mask was used. The superiority of MIPuni cannot be attributed to the type of interface used, since previous studies have shown no significant difference between MIP values obtained when using a mouthpiece or a face-mask [28,29].
With respect to the differences observed between MIPsta and MIPuni, previous findings have shown that MIPuni presented a variation of approximately 27–30% above MIPsta [19,20]. In our study, the difference between the methods was 14.3%. This lower variation can be due to the differences in the population. The subjects of the present study were younger, healthy and without artificial airway. Older and hospitalized individuals, with artificial airway, such as those included in previous studies, could present less cooperation and worse performance during MIPsta maneuvers.
We also aimed to assess the inter- and intraobserver reproducibility of MIPuni, showing that the method is reproducible. To determine the interobserver reproducibility of MIPuni, ICC[2,1] showed high correlation between values obtained by different evaluators, when the same conditions were maintained during the assessment. Good agreement between values was observed using Bland-Altman plots, since the mean difference between values obtained by the evaluators was close to zero. Concerning the limits of agreement in the Bland-Altman plots, 95% of the difference between values obtained by both evaluators was less than 27.5 cmH2O. The study also assessed the intraobserver reproducibility and showed high ICC[2,1] between values obtained by the same evaluator, at two moments, maintaining similar conditions. The dispersion of differences between values was also shown by Bland-Altman plots, with limits of agreement lower than 37 cmH2O. The same conditions were attempted in the present study for both Tests 1 and 2. Intraindividual variation factors, however, such as motivation during the test day, may have interfered with the results.
The repeatability of the values obtained by MIPsta and MIPuni was also compared. The repeatability analysis allows us to verify if the repeated measurements obtained by a single evaluator varied, when assessing the same subject with the same instrument, preserving identical conditions during a short period of time [26]. The ICC[2,1] showed very high correlation between MIPuni values while it showed moderate correlation between MIPsta measurements. The repeatability coefficient for MIPsta was 49.6 cmH2O, which means that 95% of the difference between the paired measures was up to 49.6 cmH2O. For MIPuni, the repeatability coefficient between measurements was lower, with less dispersion between the measurements (17.1 cmH2O for evaluator A and 21.8 cmH2O for evaluator B). The better repeatability of MIPuni can be explained by a lesser coordination between subject and evaluator and a lesser learning effect [19].
Limitations
A major limitation in our study was that MIPsta was performed using a mouthpiece with a 2-mm diameter air-leak opening while in MIPuni there was no air-leak opening in the face mask. Even though the use of an air-leak opening in the interface is recommended, this issue remains controversial in the literature. In a previous study, Smyth et al. [30] showed that the creation of a needle leak in the mouthpiece (18 gauge) had no effect on MIP for the prevention of glottis closure and artifactually high MIP. The authors suggest that careful instruction and observation of the subject may be more valuable than reliance on a small leak in the mouthpiece to prevent glottis closure. In the present study, a rigorous monitoring of the subjects was carried out in order to disregard maneuvers with evident signs of muscle contractions of the mouth and pharynx, rather than inspiratory muscles. In addition, our results showed a difference of more than 20 cmH2O for various individuals, even higher than 30 cmH2O in 6 subjects. It is very unlikely that such difference is due only to the absence of the air-leak opening. On the other hand, if the superiority of MIPuni had been only due to the absence of the air-leak, we would not have observed individuals with lower MIPuni values in relation to MIPsta, which is not true. We had around 6 individuals with lower MIPuni values. Nevertheless, it is essential to conduct further studies aiming to verify the real influence of different sizes of orifices in determining MIPuni. Furthermore, the majority of subjects reported discomfort due to the interruption of inspiratory flow during MIPuni, which can be confirmed by higher values of discomfort evaluated quantitatively by the Discomfort Scale. However, only one subject reported mild headache after the test. Although no significant adverse effects were observed during maneuvers, future studies should be conducted to assess the feasibility and safety of this method in different clinical situations and comorbidities. In mechanically ventilated patients, Marini et al. [17] demonstrated that approximately 10 respiratory efforts or a 20-second rest period are needed after airway occlusion to obtain MIPuni. Further studies should investigate if a 20-second period is actually required to obtain MIPuni in subjects under spontaneous breathing without artificial airway. A shorter time of attachment could minimize discomfort during this method.
Conclusions
According to the present study results, it is evident that the evaluation by MIPsta underestimates the inspiratory effort in patients without artificial airway. In this context, we recommend the use of MIPuni to determine the strength of inspiratory muscles in individuals under spontaneous breathing without artificial airway, since this method presented higher MIP values, high inter- and intraobserver reproducibility and higher repeatability when compared to MIPsta. Considering that the normal reference values available [14–16] were determined by using MIPsta, further studies will have to establish new reference values of normality using MIPuni.
Acknowledgments
Wellington P. Yamaguti presented preliminary study results in abstract form at the European Respiratory Society Annual Congress, held September 1–5, 2012, in Vienna, Austria.
Data Availability
All relevant data are within the paper.
Funding Statement
The authors have no support or funding to report.
References
- 1. Black LF, Hyatt RE. Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis 1969;99(5):696–702. [DOI] [PubMed] [Google Scholar]
- 2. American Thoracic Society / European Respiratory Society. ATS/ERS Statement on respiratory muscle testing. Am J Respir Crit Care Med 2002;166(4):518–624. [DOI] [PubMed] [Google Scholar]
- 3. Terzano C, Ceccarelli D, Conti V, Graziani E, Ricci A, Petroianni A. Maximal respiratory static pressures in patients with different stages of COPD severity. Respir Res 2008;9(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gayraud J, Ramonatxo M, Rivier F, Humberclaude V, Petrof B, Matecki S. Ventilatory parameters and maximal respiratory pressure changes with age in Duchenne muscular dystrophy patients. Pediatr Pulmonol 2010;45(6):552–559. 10.1002/ppul.21204 [DOI] [PubMed] [Google Scholar]
- 5. Parreira VF, Matos CM, Athayde FT, Moraes KS, Barbosa MH, Britto RR. Evolution of respiratory muscle strength in post-operative gastroplasty. Rev Bras Fisioter 2012;16(3):225–230. [DOI] [PubMed] [Google Scholar]
- 6. Fregonezi GA, Resqueti VR, Güell R, Pradas J, Casan P. Effects of 8-week, interval-based inspiratory muscle training and breathing retraining in patients with generalized myasthenia gravis. Chest 2005;128(3):1524–1530. [DOI] [PubMed] [Google Scholar]
- 7. Gosselink R, De Vos J, van den Heuvel SP, Segers J, Decramer M, Kwakkel G. Impact of inspiratory muscle training in patients with COPD: what is the evidence? Eur Respir J 2011;37(2):416–425. 10.1183/09031936.00031810 [DOI] [PubMed] [Google Scholar]
- 8. Lin SJ, McElfresh J, Hall B, Bloom R, Farrell K. Inspiratory muscle training in patients with heart failure: a systematic review. Cardiopulm Phys Ther J 2012;23(3): 29–36. [PMC free article] [PubMed] [Google Scholar]
- 9. Sahn SA, Lakshminarayan S. Bedside criteria for discontinuation of mechanical ventilation. Chest 1973;63(6):1002–1005. [DOI] [PubMed] [Google Scholar]
- 10. Feeley TW, Hedley-White J. Weaning from controlled ventilation and supplemental oxygen. N Engl J Med 1975;292(17):903–906. [DOI] [PubMed] [Google Scholar]
- 11. Tzanis G, Vasileiadis I, Zervakis D, Karatzanos E, Dimopoulos S, Pitsolis T, et al. Maximum inspiratory pressure, a surrogate parameter for the assessment of ICU-acquired weakness. BMC Anesthesiology 2011;11:14 10.1186/1471-2253-11-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Souza RB. Pressões respiratórias estáticas máximas. J Pneumol 2002;28(Suppl 3):S.155–165. [Google Scholar]
- 13. Steier J, Kaul S, Seymour J, Jolley C, Rafferty G, Man W, et al. The value of multiple tests of respiratory muscle strength. Thorax 2007;62(11):975–980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Neder JA, Andreoni S, Lerario MC, Nery LE. Reference values for lung function tests. II Maximal respiratory pressures and voluntary ventilation. Braz Med Biol Res 1999;32(6):719–727. [DOI] [PubMed] [Google Scholar]
- 15. Parreira VF, França DC, Zampa CC, Fonseca MM, Tomich GM, Britto RR. Maximal respiratory pressures: actual and predicted values in healthy subjects. Rev Bras Fisioter 2007;11(5):361–368. [Google Scholar]
- 16. Costa D, Gonçalves HA, Lima LP, Ike D, Cancelliero KM, Montebelo MI. New reference values for maximal respiratory pressures in the Brazilian population. J Bras Pneumol 2010;36(3):306–312. [DOI] [PubMed] [Google Scholar]
- 17. Marini JJ, Smith TC, Lamb V. Estimation of inspiratory muscle strength in mechanically ventilated patients: the measurement of maximal inspiratory pressure. J Crit Care 1986;1(1):32–38. [Google Scholar]
- 18. Truwit JD, Marini JJ. Validation of a technique to assess maximal inspiratory pressure in poorly cooperative patients. Chest 1992;102(4):1216–1219. [DOI] [PubMed] [Google Scholar]
- 19. Caruso P, Friedrich C, Denari SD, Ruiz SA, Deheinzelin D. The unidirectional valve is the best method to determine maximal inspiratory pressure during weaning. Chest 1999;115(4):1096–1101. [DOI] [PubMed] [Google Scholar]
- 20. Yamaguti WPS, Alves LA, Kauss IAM, Galvan CCR, Brunetto AF. Comparison between maximal inspiratory pressure measure by one-way valve method and conventional method in patients under weaning from invasive mechanical ventilation. Rev Bras Ter Intensiva 2004;16(3):142–145. [Google Scholar]
- 21. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Series “ATS/ERS task force: Standardisation of lung function testing”. Standardisations of spirometry. Eur Respir J 2005;26(2):319–338. [DOI] [PubMed] [Google Scholar]
- 22. Pereira CAC, Rodrigues SC, Sato T. New reference values for forced spirometry in white adults in Brazil. J Bras Pneumol 2007;33(4):397–406. [DOI] [PubMed] [Google Scholar]
- 23. Wen AS, Woo MS, Keens TG. How many maneuvers are required to measure maximal inspiratory pressure accurately? Chest 1997;111(3):802–807. [DOI] [PubMed] [Google Scholar]
- 24. Fiz JA, Montserrat JM, Picado C, Plaza V, Agusti-Vidal A. How many maneuvers should be done to measure maximal inspiratory mouth pressure in patients with chronic airflow obstruction? Thorax 1989; 44(5):419–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Grant S, Aitchison T, Henderson E, Christie J, Zare S, McMurray J, et al. A comparison of the reproducibility and the sensitivity to change of visual analogue scales, Borg scales, and Likert scales in normal subjects during submaximal exercise. Chest 1999;116(5):1208–1217. [DOI] [PubMed] [Google Scholar]
- 26. Munro BH. Statistical methods for health care research 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1997. [Google Scholar]
- 27. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;327(8476):307–310. [PubMed] [Google Scholar]
- 28. Junior JFF, Paisani DM, Franceschini J, Chiavegato LD, Faresin SM. Maximal respiratory pressures and vital capacity: comparison mouthpiece and face-mask evaluation methods. J Bras Pneumol 2004;30(6):515–520. [Google Scholar]
- 29. Wohlgemuth M, van der Kooi EL, Hendriks JC, Padberg GW, Folgering HT. Face mask spirometry and respiratory pressures in normal subjects. Eur Respir J 2003;22(6):1001–1006. [DOI] [PubMed] [Google Scholar]
- 30. Smyth RJ, Chapman KR, Rebuck AS. Maximal inspiratory and expiratory pressures in adolescents. Normal values. Chest 1984;86(4):568–772. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.