Abstract
Background
Mechanical ventilation (MV) causes many distressing symptoms. Weaning, the gradual decrease in ventilator assistance leading to termination of MV, increases respiratory effort, which may exacerbate symptoms and prolong MV. Music, a non-pharmacological intervention without side effects may benefit patients during weaning from mechanical ventilatory support.
Methods
A narrative review of OVID Medline, PsychINFO, and CINAHL databases was conducted to examine the evidence for the use of music intervention in MV and MV weaning.
Results
Music intervention had a positive impact on ventilated patients; 16 quantitative and 2 qualitative studies were identified. Quantitative studies included randomized clinical trials (10), case controls (3), pilot studies (2) and a feasibility study.
Conclusions
Evidence supports music as an effective intervention that can lesson symptoms related to MV and promote effective weaning. It has potential to reduce costs and increase patient satisfaction. However, more studies are needed to establish its use during MV weaning.
Keywords: Artificial Respiration, Mechanical Ventilator, Weaning, Airway Management, Music, Music Therapy
Introduction
Initiation of mechanical ventilation (MV)a to treat acute respiratory failure is a lifesaving intervention. Causes of acute respiratory failure include pulmonary disease, neuromuscular disease, shock, and major surgery.1 Recent estimates have found that over half of all ICU patients require MV.2 An estimated 800,000 patients undergo MV in the U.S. each year with a cost of approximately $27 billion.1 On average, patients who receive MV stay 4 days longer in the ICU and an additional 6 days in the hospital compared to ICU patients who do not.3
Generally, as patients recover from acute illness, they can be “weaned” from ventilatory support. Weaning is a gradual decrease in ventilator settings that leads to termination of MV support.4 Successful weaning depends on respiratory muscle strength, adequate respiratory drive, acid base balance, neurological status, as well as psychological readiness.5–7 Nationwide, the mean number of ventilator days is 5.6, but 5% to 20% of intubated patients require support for at least 21 days.3,8 Delays in extubation can be due to severe respiratory muscle deconditioning, poor nutrition, upper airway edema, and decreased level of consciousness secondary to over-use of sedative medications.9 Extubation failure can lead to ventilator-associated pneumonia, airway trauma, increased costs and high mortality rates.10 Patients who require MV for greater than 3 weeks account for more than 50% of total ICU costs.1 MV and MV weaning lead to an array of distressing symptoms such as pain, agitation, lack of sleep, and especially anxiety.13 Unmanaged anxiety stimulates the sympathetic nervous system, increases work of breathing and fatigue, and severely impedes ventilator weaning;4 it can be particularly severe for the ventilated patient, and, if not treated promptly, can increase recovery time and patient mortality.11,12
Current symptom management practice for patients receiving ventilatory support primarily involves the administration of numerous sedative and analgesic medications which can prolong ventilation and increase length of ICU stay.11,13 Overuse of these medications can lead to fatigue, delirium, muscle weakness, and post-traumatic stress disorder (PTSD).14 However, sedative administration is only one symptom management strategy used to help alleviate anxiety. A number of integrative, non-pharmacological interventions have been shown to be beneficial for anxiety symptom management in non-ICU patients such as music, imagery, massage, and animal assisted therapy.13
Music intervention is the non-pharmacological, integrative therapy of interest in this review; it has been shown to decrease anxiety during MV.15 Decreasing anxiety could help promote more efficient ventilator weaning and hasten ICU discharge. This is significant in that “even nominal decreases in length of time spent in the ICU or the duration of mechanical ventilation have the opportunity to significantly reduce hospitalization costs.”3(p. 1271) Incorporating music into the care of the ventilated patient has strong potential to alleviate the symptom burden and the high cost of conventional treatments as well as increase patient satisfaction and promote efficient weaning.4,13,16,17
The purpose of this narrative review was to describe the state of the science on music as an integrative intervention during MV and ventilator weaning, and to identify current gaps in knowledge regarding use of music intervention for symptom management, specifically during weaning. This review provides an evidence-based background for music intervention and supports the need for future studies on music intervention during weaning.
Background
Weaning from Mechanical Ventilation
The weaning process involves a gradual decrease in ventilator settings as a patient’s respiratory status improves, leading to termination of MV support.4 As the acute cause of respiratory failure resolves and the patient can tolerate independent respirations, the artificial airway is removed.9,10,18 For some, weaning can be a lengthy process. Recent estimates state that more than 40% of the total duration of MV is spent enduring the weaning process.6 While advancements in ventilator management protocols have been made, a universal protocol to determine readiness to wean based on strict physiological measures has not been established.10 It has been predicted that patients’ subjective perceptions of weaning may strongly influence weaning outcomes, but the extent of their role in successful outcomes remains unclear.19 Most weaning guidelines require a formal assessment of readiness to wean before beginning weaning trials. Weaning trials generally require a patient to tolerate spontaneous respirations for at least 30 minutes. A patient is usually ready for extubation after two or more successful weaning trials. If a patient fails a weaning trial, extubation is not safe and weaning is continued. Up to 20% of ventilated patients experience extreme weaning difficulty and cannot be extubated.6,8,10
Extubation failure is the inability to sustain spontaneous breathing after removal of the artificial airway with the need for reintubation within 24–72 hours.9 Extubation failure can lead to airway trauma, ventilator-associated pneumonia, gastrointestinal bleeding, and blood clots. It can increase costs, result in longer ICU stays, and increase morbidity and mortality.6,9,10 It has been estimated that extubation failure occurs at least once in up to 47% of mechanically ventilated patients.9 Timely, effective weaning is critical to decreasing the personal and economic cost of MV and extubation failure.19
Anxiety during Mechanical Ventilation and Ventilator Weaning
Anxiety, a state marked by dread, fear, apprehension, increased motor tension and autonomic arousal, is a major psychological stressor with harmful physical manifestations that are often experienced during MV and ventilator weaning.17,20 High stress and anxiety levels in mechanically ventilated patients have been associated with increased patient morbidity and mortality.15,21 Up to 85% of ventilated patients experienced anxiety,12 and 60% of those patients reported feeling scared most of the time.22 Sustained high levels of anxiety activate the sympathetic nervous system, which causes an increase in heart rate, blood pressure, and respiratory rate, and initiates an unfavorable neurohormonal response.23–25 Arousal of the sympathetic nervous system can cause serious complications including arterial and venous constriction, myocardial stimulation, and bronchoconstriction.23 Arterial and venous constriction in the lungs severely impedes the ability to oxygenate tissues effectively,26 which increases the work of breathing, induces fatigue, and can extend the need for MV.7
Weaning requires increased respiratory effort and can further exacerbate anxiety and its manifestations. If patients are not properly educated and encouraged during weaning, they may feel increasingly anxious, which can lead to increased dyspnea, panic, and a fear of abandonment as ventilator support is decreased.7,19 It has been shown that patients who did not wean successfully reported more fatigue, dyspnea, and less weaning self-efficacy.19
Symptom Management with Sedative Medications
Nurses are responsible for ICU patient symptom management. Current practice to alleviate distressing symptoms involves the administration of sedative and analgesic medications which can lead to prolonged ventilation and increased lengths of ICU stays.11,13,17 At times, medication is necessary to facilitate patient comfort, safety, and promote recovery.27 However, these highly potent medications can contribute to a multitude of complications such as fatigue, weakness, delayed weaning, and PTSD.14 Indeed, many side effects have been associated with sedative agents such as hypotension, increased risk for ventilator-associated pneumonia, and delayed ventilator weaning.28,29–33 Overall, deep pharmacological sedation during MV increases patient morbidity. A strong correlation exists between continuous sedation and prolonged ICU stays, increased rates of organ failure and reintubation.28,34 Over-sedation with continuous infusions can greatly alter routine neurologic assessments which may lead to the ordering of unnecessary costly diagnostic exams (i.e., CT scans, MRIs).34 Sedative agents can cause severe short-term and long-term issues with memory and cognition.
There is growing evidence supporting the notion that mechanically ventilated patients can benefit from an increased awareness of their surroundings.34 Recent studies indicate that patients who were most awake and aware of their surroundings during MV had the lowest PTSD-like symptoms after hospital discharge.34 Continuous high doses of sedative medications can cause severe long-term psychological damage such as continued anxiety post-ICU discharge, depression, and paranoid delusions.28 Neurological impairment from sedatives can necessitate reintubation and negatively impact the weaning process.9 Continuous sedation is a major risk factor for extubation failure.9 Integrative therapies such as music, in addition to sedative and analgesic medications, can synergistically enhance comfort and relaxation during MV.13
Symptom Management with Music Intervention
Music is a non-pharmacological intervention that integrates physiological and psychological components to reduce stress and anxiety and promotes overall well-being.23,24 Music intervention can abate the stress response, decrease anxiety during MV, and induce an overall relaxation response by reducing stimuli that cause stress, synchronizing body rhythms such as breathing and heart rate, and by positively influencing emotional feelings of the listener.35 This relaxation response can lower cardiac workload and oxygen consumption, which promotes more effective ventilation and accelerates ventilator weaning.23,36 Music that contains simple repetitive rhythms, low pitch, slow tempos, harmony and lack percussive instruments and vocals have been shown to reduce anxiety.25,28
Although it is noted in the literature that music is commonly used in nursing care, there are currently no standard protocols or guidelines to direct ICU staff on the most appropriate and useful methods to incorporate music into daily care of the ventilated patient. Music is inexpensive when compared to sedative and analgesic medications,17,23 and has been shown to reduce anxiety and sedative exposure, which decreases the time the nurse must spend providing calming techniques and other pharmacological intervention to ventilated patients.5,17,23–25 The success of weaning could be significantly impacted by music intervention, but this assertion requires further examination of existing evidence to determine the influence of music on the weaning process in patients receiving MV. The following research methods were employed to identify the most relevant literature regarding music intervention and MV.
Methods
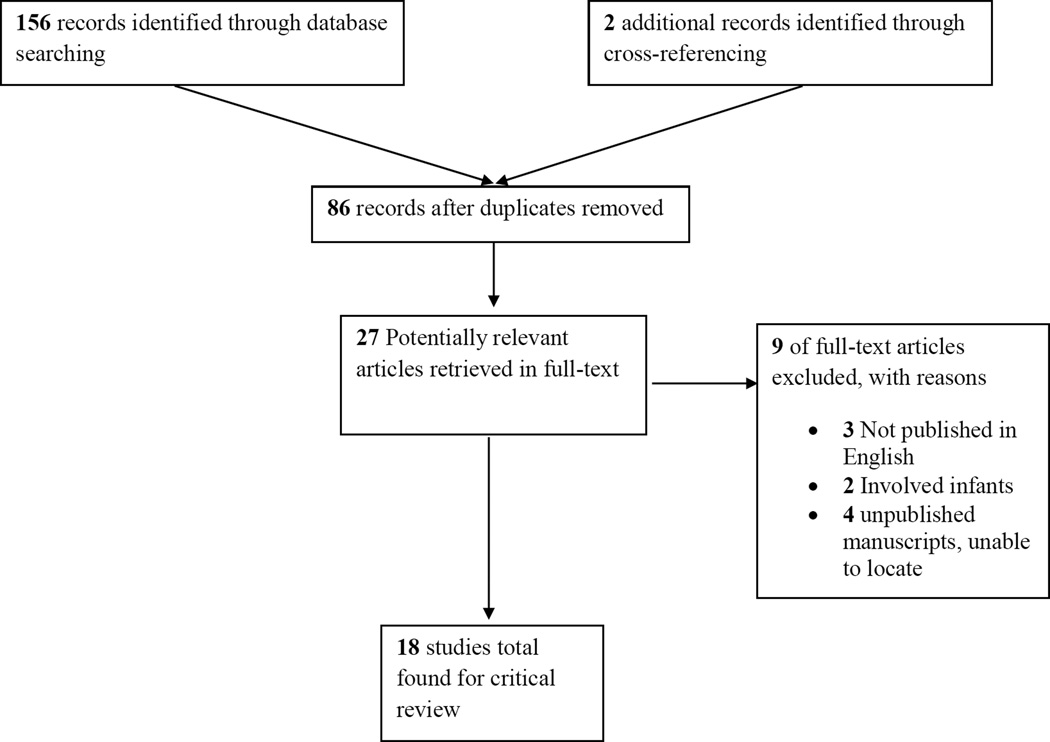
A narrative review was guided by the flowchart described by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement.37 A comprehensive computerized search of the literature on music intervention during MV was conducted using the OVID Medline, PsychINFO, and CINAHL databases with the guidance of an expert professional biomedical librarian. Subject headings used in the searches included “respiration, artificial”, “ventilators, mechanical”, “ventilator patients”, “airway management”, “music”, and “music therapy”. The subject headings were exploded to yield adequate resources for review. Cross-referencing was used to identify additional relevant articles for review. Title and abstract review was used to identify primary research studies. The review was not limited by study design or date published. Quantitative and qualitative studies that examined the use of music intervention during MV and ventilator weaning to reduce physical and psychological symptoms, as well as studies that evaluated the patient experience of music intervention during MV were examined. Studies that assessed the infant and pediatric populations and studies not published in English or translated into English were excluded from the review. Duplicate studies were also excluded.
The initial review yielded 156 potentially relevant articles. After duplicates were removed, 86 abstracts were reviewed; 27 potentially relevant articles were reviewed in full-text. Those not meeting inclusion criteria were excluded (not published in English [n=3], involved infants or pediatrics [n=2]. Four unpublished manuscripts were identified by title. Additional attempts were made to obtain the unpublished manuscripts but were unsuccessful. In total, 18 studies were eligible for review (See Figure 1 for the PRISMA Flowchart used to document the progression of this review). Using the Matrix Method,38 a standardized data display was used to chronologically evaluate and extract information from each study such as author, journal, and year, study purpose, setting, number of subjects, methodical design, sampling design, variable measurement, subject characteristics, findings and limitations, and information related to weaning.
Figure 1.
Audit trail of literature search using PRISMA Flowchart
Results
Most studies investigated music intervention during MV; only one study explored music intervention during ventilator weaning (see Table 1). One qualitative study that explored patients’ experiences with music while ventilated was reviewed. One study used both quantitative and qualitative methods. The remaining 16 studies used quantitative methods to evaluate physiological signs of anxiety as well as a variety of anxiety, agitation, and sedation scales to measure the effectiveness of music intervention. The quantitative studies included randomized clinical trials (n= 10), case controls (n=3), pilot studies (n=2), and a feasibility study (n=1). A variety of control conditions were used such as headphones to promote a relaxing environment, ICU usual care, and historical controls. The results of the review are presented using the following eight subject headings. The first two subheadings relate to methodological aspects of studies: 1) Duration, Frequency and Timing of Music Intervention, 2) Patient Wakefulness, Music Styles, and Music Selection. The remaining six subheadings refer to outcomes and interventions of studies: 3) Influence of Music on Sedation and Agitation, 4) Influence of Music on Physiological Arousal, 5) Influence of Music on Biomarkers of the Stress Response, 6) Influence of Music on Anxiety, 7) Patients’ Self Report of Experiences with Music, and 8) Nurses’ Evaluation of Music Intervention.
Table 1.
Summary of reviewed studies.
| Author/Year | Design | Purpose | Setting/Subjects | Variables Measured | Findings |
|---|---|---|---|---|---|
| Almerud&Peters son, (2003)35 | Mixed Methods
|
Purpose: to discover whether music therapy had a measurable relaxing effect on patients who were temporarily on a respirator in an ICU and after completion of respirator treatment investigate those patients’ experiences of music therapy | 16 bed ICU in Sweden
|
|
|
| Beaulieu-Boire, et al. (2013)34 | Randomized Crossover (3 days with a washout on day 2)
|
Purpose: to evaluate the impact of slow tempo music listening periods in mechanically ventilated intensive care unit patients | 16 bed ICU in a tertiary hospital in Canada
|
|
|
| Chlan (1995)33 | Two group experimental design
|
Purpose: to examine selected psychophysiological responses of mechanically ventilated patients to music | Single ICU at a tertiary care center in the US
|
|
|
| Chlan (1998)32 | Two group experimental design
|
Purpose: to test the effects of music therapy on relaxation and anxiety reduction for patients receiving ventilator assistance | 4 urban ICUs in the US
|
|
|
| Chlan et al. (2007)38 | Pilot Study: two group experimental design
|
Purpose: to explore the influence of music on serum biomarkers of the stress response in patients receiving ventilator support | 11 bed ICU in a University medical center in the US
|
|
|
| Chlan et al. (2012)41 | Three group randomized clinical trial
|
Purpose: to explore the influences of music on stress in a sample of patients of the duration of ventilator support | 12 ICUs at 5 urban hospitals in the US
|
|
|
| Chlan et al. (2001)37 | Descriptive pilot study | Purpose: to test feasibility of patient-initiated music intervention protocol over a 3 day trial and to discern the associated barriers to adherence by study participants and nursing staff | 1 ICU at a tertiary care center in the US
|
|
|
| Chlan et al. (2013)17 | Three group randomized clinical trial
|
Purpose: to test whether listening to self-initiated PDM can reduce anxiety and sedative exposure during ventilator support in critically ill patients | 12 ICUS at 5 urban hospitals in the US
|
|
|
| Conrad et al. (2007)40 | Two group randomized clinical trial
|
Purpose: to identify mechanisms of music-induced relaxation using a special selection of slow movements of Mozart’s piano sonatas | 1 ICU
|
|
|
| Dijkstra, et al. (2010)21 | Two group randomized clinical trial
|
Purpose: to determine the effects of music on physiological responses and sedation scores in sedated, mechanically ventilated patients | 3 ICUs in a university hospital in the Netherlands
|
|
|
| Han et al. (2010)28 | Three group randomized clinical trial
|
Purpose: to examine the effects of music intervention on the physiological stress response and the anxiety level among mechanically ventilated patients in the intensive care unit | A single ICU at a large teaching hospital in China
|
|
|
| Hunter et al. (2010)4 | Feasibility study with historical controls
|
Purpose: to determine the feasibility of incorporating music therapy in to the weaning process and to evaluate the efficacy of the intervention based on levels of anxiety, days to wean and patient/nurse satisfaction | A single pulmonary step down unit of a large tertiary teaching hospital in the US
|
|
|
| Korhan et al. (2011)23 | Case control experimental study
|
Purpose: to investigate if relaxing music is an effective method of reducing the physiological signs of anxiety in patients receiving mechanical ventilator support | A single ICU in a teaching hospital in Turkey
|
Vital Signsmeasured immediately before the intervention, at the 30th, 60th, and 90th minutes of the intervention, and 30 minutes after the intervention |
|
| Lee et al. (2005)24 | Two group randomized clinical trial
|
Purpose: to investigate effects of music on the anxiety of patients on mechanical ventilators as assessed by objective parameters and a subjective validated anxiety scale | A single ICU in Hong Kong
|
|
|
| Saadatmand et al. (2013)31 | Two group randomized clinical trial
|
Purpose: to identify the effect of the nature-based sounds’ intervention on agitation, anxiety level, and physiological stress responses in patients under mechanical ventilation support | A single ICU in a teaching hospital in Iran
|
|
|
| Stubbs (2005)39 | Qualitative Study
|
Purpose: to gain insight into patients’ and nurses’ perception of the benefit of music therapy during critical illness and to add to the body of knowledge in nursing around the use of therapies complementary to medicine | A single ICU in a community hospital in the US
|
|
|
| Twiss et al. (2006)36 | Two group randomized clinical trial
|
Purpose: to determine the effect of music listening on postoperative anxiety and intubation time in patients undergoing cardiovascular surgery | A single ICU in the US
|
|
|
| Wong et al. (2001)22 | Crossover design with random assignment
|
Purpose: to assess the effectiveness of music therapy in decreasing anxiety in ventilator dependent patients | A single ICU in Hong Kong
|
|
|
HR-heart rate, BP – blood pressure, RR – respiratory rate
Duration, Frequency and Timing of Music Intervention
The duration, frequency, and timing of music intervention varied greatly across studies. All studies implemented music for a minimum of 30 minutes once per day, but some music listening sessions lasted up to 90 minutes and intervention frequency ranged from one to three times per day. The duration of study protocols ranged from one day to up to 30 days. Four studies implemented music intervention during the late afternoon or early evening.35,39–41 Others implemented the intervention during the morning and then again in the evening21,34 or randomly throughout the day depending on unit and nurse schedules.23,24 One study implemented music listening during nighttime sleep42 and another allowed patients to listen to music continuously during the post-operative period.43 In a study that evaluated music during weaning, the timing of the music intervention depended on where the patient was in the weaning process (early versus more progressed).4 Chlan et al. used a unique approach that allowed patients to self-direct the frequency, length, and timing of the music intervention.17,44 Ultimately, consensus regarding the most effective and appropriate duration, frequency and timing of music intervention could not be determined from the literature.
Patient Wakefulness, Music Styles, and Music Selection
Investigators required varying levels of patient wakefulness for study inclusion. Most investigators required patients to be alert and mentally competent in order to participate in study consent.4,17,23,35,39,40,43–45 Many studies mentioned conditions such as “alert and oriented”, “following commands”, “not confused”, and “able to effectively communicate” as inclusion criteria but few required official screens for delirium as part of the pre-enrollment process. It is not known to what extent wakefulness impacts the physiologic results of music intervention during MV and ventilator weaning.
All studies in this review implemented styles of music that were considered “relaxing” including nature based sounds, classical, and easy listening. Previous research has demonstrated music most effective at reducing anxiety is familiar to the patient, contains 60–80 beats per minute with simple arrangements and lacks words.13 However, whenever possible, patients should be solicited personally for their specific musical preferences because certain styles of music can trigger music memories that evoke profound emotional responses.13 Chlan et al. and Hunter et al. encouraged patients to self-select their preferred music styles.4,17 Some investigators allowed patients and families to choose from a predetermined list of music selections.23,25,35,36,40,41,45,46 One study had patients select their music choice prior to undergoing cardiac surgery. Upon awakening, patients were allowed to change their music choice if desired.43 Hunter and colleagues utilized live music at the bedside.4 Many investigators used the expertise of a music therapist to help design the music portfolio or help implement intervention and evaluate patient preferences.4,17,44,47 It was common for investigators to enhance the environment of both control and experimental groups to promote relaxation by dimming lights, closing curtains/doors, and placing signs outside to alert staff and visitors to the intervention23,25,35,40–42 Some also provided patients with verbal instructions to think of pleasant thoughts during the intervention.35,40 In summary, inconsistencies exist concerning ideal patient wakefulness for study inclusion. However, increased patient wakefulness affords greater patient control and independence in regards to music choice.
Influence of Music on Sedation and Agitation
Several studies have evaluated and confirmed the hypothesis that music intervention can decrease the need for sedatives during MV. In a study designed to test whether listening to self-initiated, patient-directed music (PDM) reduced sedative exposure during MV, investigators used a sedative drug intensity score which revealed sedative exposure was significantly reduced in the PDM group.17 In a study by Conrad et al., a continuous infusion of propofol was suspended prior to the intervention for both the experimental and control groups and was reinitiated after the intervention.48 Patients in the experimental group did not require additional doses of propofol during the intervention, whereas patients in the control group occasionally needed extra doses of propofol to maintain ventilator compliance.48 In a study by Saadatmand et al., the Richmond Agitation Sedation Scale (RASS), a 10-point scale with four levels of agitation ranging from combative, to calm and alert, to unarousable, was used as a measurement of sedation effectiveness.39 Results demonstrated the odds of having higher agitation in the control group was approximately 11.24 times that of the intervention group, suggesting that the music intervention, which consisted of nature-based sounds, could decrease agitation levels in sedated, mechanically ventilated patients.39
Influence of Music on Physiological Arousal
Evidence reveals music can reduce the physiological signs of anxiety such as respiratory rate, heart rate, and blood pressure among patients who are mechanically ventilated. In several studies, music intervention groups experienced a significant decrease in respiratory rate.23–25,35,40,41 The significant reduction was seen over time, suggesting a cumulative dose effect.24,35 A number of studies found that music intervention significantly reduced heart rate.24,25,35,40,41,48 The literature also reveals a trend of decreasing heart rates both during and after music intervention. The reductions were also seen over time suggesting a cumulative dose effect.24,35,40 Music intervention was effective at decreasing blood pressure.24,25,35,39,42,48 Conrad et al. found that not only did arterial blood pressure decrease significantly in the music group, it also increased significantly in the control.48 Similarly, Almerud et al. noted a significant decrease in blood pressure during music intervention as well as a corresponding rise after cessation of treatment.42
Influence of Music on Biomarkers of the Stress Response
Several studies explored the influence of music on biomarkers of the stress response by testing blood and urine samples in patients undergoing MV.45,47–49 These biomarkers included blood levels of corticotrophin, cortisol, epinephrine, norepinephrine, dehydroepiandrosterone (DHEA), growth hormone, adrenocorticotropin hormone (ACTH), interleukin-6 (IL-6), prolactin and prolactin monomer, leptin, MET-enkephalin, and C-reactive protein.45,47,48 Chlan et al. evaluated urinary free cortisol (UFC).49 While not significantly different among groups, less profound spikes in urinary free cortisol (UFC) levels were observed. Beaulieu-Boire et al.47 found that blood cortisol and prolactin decreased after music listening. In another study by Conrad et al., decreases were seen in plasma concentrations of IL-6, DHEA, and epinephrine.48 Chlan et al. did not find any statically significant decreases in serum biomarkers, but attributed the results to a wide variability in mean levels of biomarkers and small sample size.45 The connection between biomarkers and clinical observations of anxiety such as increased heart rate and respiratory rate remains unclear. Some hypothesized explanations for inconsistent results provided by investigators were drug administration, number of ventilator days, and large variability in baseline biomarker levels and variability among critically ill patients.
Influence of Music on Self-Reported Anxiety
Over half of the articles reviewed included a self-reported assessment of anxiety. The reliability of these self-reported measures is difficult to assess because most subjects receive sedative medications during MV. A number of instruments were used to measure anxiety across studies with varying results. These included: Visual Analogue Scale for Anxiety (VAS-A), Anxiety Faces Scale (FAS), The Spielberger State-Trait Anxiety Scale (STAI) [20 items and 6 items]. Music was found to be an effective intervention to reduce anxiety in the mechanically ventilated patient.35,40,43 In one study, both the music condition and the rest condition experienced reduced state anxiety scores, but the music intervention was more effective than a rest period in reducing anxiety.23 Another study found that at any point, the music group had a VAS-A score that was significantly lower than the usual care control group. One study detected a significant difference between anxiety scores using the FAS.39 The odds of having a high anxiety score in the control group was 4.5 times the same odds of having higher anxiety scores in the music group.39
Patients’ Self Report of Experiences with Music
Two studies primarily aimed to investigate patients’ experiences of music intervention by interviewing patients after extubation.42,46 Both interviewed patients while they were still in the hospital, shortly after being extubated. When interviewed, no patients were immediately able to recall that they had listened to music.42,46 In one study, the music played during MV was also played during the interview to jog patients’ memory, which was a successful tactic.46 It is unknown whether the timing of the interviews affected patients’ ability to recall information accurately due to the administration of sedative medications in the days before the interviews.
Patients who underwent music intervention during MV were able to recall memories of pain, anxiety and discomfort, as well dreams and delusions. For many, music was a happy memory among traumatic memories while undergoing MV.46 Lee et al. conducted a post intervention satisfaction survey, and 88% of subjects expressed satisfaction with music.25 Another study reported that 95% of the time, participants felt that music was helpful, and 100% of study subjects would participate in a music intervention again.4 In addition, 98% of music sessions that were surveyed, the participant felt less anxious, and after 80% of the music sessions surveyed, the participant reported less stress than expected.4
Nurses’ Evaluation of Music Intervention
Several investigators solicited nurses for their subjective evaluation of patients’ response to music intervention. Nurses expressed positive feelings towards music intervention. Stubbs reported that none of the nurses’ interviewed felt there were any disadvantages to music.46 Chlan et al. did not receive any comments from nurses that would suggest the music protocol was burdensome to their patient care practices.17 Lee et al., created a resting behavior observation list which was a checklist for research staff to identify four types of behavior: restlessness, facial distortion, restfulness, and sleep.25 A greater increase in the proportion of “comfortable behaviors” were observed in the music group compared to the control group.25
Hunter and colleagues4 administered Likert-type scale surveys [1 = strongly disagree, 5=strongly agree] to bedside nurses to investigate their observations and satisfaction with the protocol. Nurses ranked the statements “patient appeared less anxious” and “there was less need for medical intervention” with a mean score of at least 4.2 or greater. In addition, nurses felt that music reduced their personal stress, was incorporated unobtrusively, and was useful for their patient. Chlan et al. found that nurses were willing to use the music intervention and had a positive view of the intervention.44 This is important, since nurses are primarily the ones who are responsible for promoting and implementing music intervention at the bedside.
Discussion
This narrative literature review supports the use of music intervention in patients undergoing MV. While the aim was to focus on music to reduce psychophysiological symptoms, especially anxiety, during weaning trials, there is a striking lack of studies testing music listening during weaning. Of the three studies that examined music during ventilator weaning, only one was in English4 and it was a feasibility study. While a majority of the evidence centers on symptom management with music during MV, important aspects are gained from the review.
Hunter et al.4 specifically evaluated music during ventilator weaning. This study demonstrated that music is an effective complement in difficult to wean patients by decreasing the physical signs of anxiety.4 Music was well received by both patients and staff, which adds to its feasibility in practice.4 Failure to wean from the ventilator is a complex physical and psychological setback that frequently impacts ventilated patients. Little is understood regarding the influence of psychophysiological symptoms on weaning trials and ways in which music can lessen these symptoms during weaning trials to promote efficient ventilator termination. There is a critical need for more studies that investigate music to reduce distressing symptoms during ventilator weaning.
Incorporating music during weaning trials is an innovative intervention that warrants more thorough investigation for the following reasons: (1) Close to 1 million individuals endure MV each year in the United States.1 (2) Weaning is a necessary process for MV to be terminated and spontaneous independent breathing achieved. (3) More than 40% of the total duration of MV is spent enduring the weaning process.6 (4) Music is a feasible non-pharmacological intervention to help alleviate anxiety and other distressing symptoms in order to promote successful weaning.4
Limitations to this Review
There are several limitations to this review. A single author evaluated the studies and only studies published in English were included. Three original non-English studies were identified in the search of the literature but were not used in this review. In addition, only published literature was included. Unpublished literature such as abstracts and unpublished dissertations and theses were not included in this review. Only adults over 18 were included in the studies reviewed. Music has a strong influence on the psychological wellbeing of adolescents, and it is not known how music intervention can impact adolescent ventilated patients. Many studies had small sample sizes. There is a need for randomized clinical trials that are adequately powered to answer questions asked, and a need for consistent measures and protocols so that findings can be compared across studies. The majority of studies focused on music to manage symptoms of anxiety; examination of additional symptoms of MV weaning such as agitation, lack of sleep, and pain is warranted.
Conclusion
Collectively, the studies included in this review indicate that music can decrease psychophysiological symptoms for patients undergoing MV, which may lead to improved patient satisfaction and promote overall recovery from conditions requiring MV.43 A decrease in distressing symptoms could encourage a beneficial relaxation response. Achieving a more relaxed state can help reduce the necessity for sedative medications and may eventually decrease the overall length of time ventilatory support is needed.24 While ICU staff can easily implement music as a non-pharmacological intervention,42 patient initiated music listening is a plausible and effective intervention strategy.17 The evidence from the studies evaluated for this review suggests that music can decrease the physiological and psychological symptoms as well as reduce sedative exposure in the ventilated patient. However, this review reveals the noticeable absence of research that examines the influence of music intervention during weaning from mechanical ventilation. Further research in this area is warranted in order to determine if music intervention can reduce distressing symptoms and favorably impact important clinical factors such as time to weaning trials, length of weaning trials, successful weaning readiness, and ultimately, total ventilator days and ICU length of stay.
Acknowledgements
Research reported in this publication was supported by National Institute of Nursing Research of the National Institutes of Health under award number [FNR014591A].
Footnotes
MV – mechanical ventilation
References
- 1.Wunsch H, Linde-Zwirble WT, Angus DC, Hartman ME, Milbrandt EB, Kahn JM. The epidemiology of mechanical ventilation in the United States. Crit Care Med. 2010;38(0):1947–1953. doi: 10.1097/CCM.0b013e3181ef4460. [DOI] [PubMed] [Google Scholar]
- 2.Metnitz PGH, Metnitz B, Moreno RP, et al. Epidemiology of mechanical ventilation: Analysis of the SAPS 3 database. Intens Care Med. 2009;35(5):816–825. doi: 10.1007/s00134-009-1449-9. [DOI] [PubMed] [Google Scholar]
- 3.Dasta JF, McLaughlin TP, Mody SH, Piech CT. Daily cost of an intensive care unit day: The contribution of mechanical ventilation. Crit Care Med. 2005;33(6):1266–1271. doi: 10.1097/01.ccm.0000164543.14619.00. [DOI] [PubMed] [Google Scholar]
- 4.Hunter BC, Oliva R, Sahler LJZ, Gaisser D, Salipante DM, Arezina CH. Music therapy as an adjunctive treatment in the management of stress for patients being weaned from mechanical ventilation. J Music Ther. 2010;47(3):198–219. doi: 10.1093/jmt/47.3.198. [DOI] [PubMed] [Google Scholar]
- 5.Cawley MJ, Dasta JF. Pharmacotherapeutic challenges in weaning from mechanical ventilation. US Respiratory Disease. 2007:63–65. [Google Scholar]
- 6.Eskandar N, Apostolakos MJ. Weaning from mechanical ventilation. Crit Care Clin. 2007;23(3):263–274. doi: 10.1016/j.ccc.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 7.Blackwood B. The art and science of predicting patient readiness for weaning from mechanical ventilation. Int J Nurs Stud. 2000;37(2):145–151. doi: 10.1016/s0020-7489(99)00062-0. [DOI] [PubMed] [Google Scholar]
- 8.White AC, O'Connor HH, Kirby K. Prolonged mechanical ventilation: Review of care settings and an update on professional reimbursement. CHEST. 2008;133(2):539–545. doi: 10.1378/chest.07-0656. [DOI] [PubMed] [Google Scholar]
- 9.Kulkami AP, Agarwal V. Extubation failure in intensive care unit: Predictors and management. Indian J Crit Care Med. 2008;12(1):1–9. doi: 10.4103/0972-5229.40942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stawicki SP. Mechanical ventilation: Weaning and extubation. OPUS 12 Scientist. 2007;1(2):13–16. [Google Scholar]
- 11.Silverman HJ. Symptom management in the intensive care unit: Toward a more holistic approach. Crit Care Med. 2002;30(4):936–937. doi: 10.1097/00003246-200204000-00041. [DOI] [PubMed] [Google Scholar]
- 12.Puntillo KA, Arai S, Cohen NH, et al. Symptoms experienced by intensive care unit patients at high risk of dying. Crit Care Med. 2010;38(11):2155–2160. doi: 10.1097/CCM.0b013e3181f267ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tracy MF, Chlan L. Nonpharmacological interventions to manage common symptoms in patients receiving mechanical ventilation. Crit Care Nurs. 2011;31(3):19–28. doi: 10.4037/ccn2011653. [DOI] [PubMed] [Google Scholar]
- 14.Volk B, Grassi F. Treatment of the post-ICU patient in an outpatient setting. Am Fam Physician. 2009;79(6):459–464. [PubMed] [Google Scholar]
- 15.Bradt J, Dileo C, Grocke D. Music interventions for mechanically ventilated patients. Cochrane Database of Syst Rev. 2010;12:1–35. doi: 10.1002/14651858.CD006902.pub2. [DOI] [PubMed] [Google Scholar]
- 16.Disch J, Kreitzer MJ. Shaping the future of complementary and alternative therapies for critical care nursing. Crit Care Nurs Clin of North America. 2003;15(3):387–392. doi: 10.1016/s0899-5885(02)00097-7. [DOI] [PubMed] [Google Scholar]
- 17.Chlan LL, Weinert CR, Heiderscheit A, Tracy MF, Skaar DJ, Guttormson JL, Savik K. Effects of patient-directed music intervention on anxiety and sedative exposure in critically ill patients receiving mechanical ventilatory support. JAMA. 2013;309(22):2335–2344. doi: 10.1001/jama.2013.5670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pruitt B. Weaning patients from mechanical ventilation. Nursing. 2006;36(9):36–41. doi: 10.1097/00152193-200609000-00030. [DOI] [PubMed] [Google Scholar]
- 19.Twibell R, Siela D, Mahmoodi M. Subjective perceptions and physiological variables during weaning from mechanical ventilation. Am J of Crit Care. 2003;12(2):101–112. [PubMed] [Google Scholar]
- 20.Chlan L, Savik K. Patterns of anxiety in critically ill patients receiving mechanical ventilator support. Nurs Res. 2011;60(3):S50–S57. doi: 10.1097/NNR.0b013e318216009c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moser DK, Dracup K. Is anxiety early after myocardial infarction associated with subsequent ischemic and arrhythmic events? Psychosom Med. 1996;58(5):395–401. doi: 10.1097/00006842-199609000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Rattray J, Johnston M, Wildsmith JA. The intensive care experience: development of the ICE questionnaire. J Adv Nurs. 2004;47:64–73. doi: 10.1111/j.1365-2648.2004.03066.x. (2004) [DOI] [PubMed] [Google Scholar]
- 23.Wong HLC, Lopez-Nahas V, Molassiotis A. Effects of music therapy on anxiety in ventilator-dependent patient. Heart Lung. 2001;30(5):376–386. doi: 10.1067/mhl.2001.118302. [DOI] [PubMed] [Google Scholar]
- 24.Korhan EA, Khorshid L, Uyar M. The effect of music therapy on physiological signs of anxiety in patients receiving mechanical ventilatory support. J Clin Nurs. 2011;20(7–8):1026–1034. doi: 10.1111/j.1365-2702.2010.03434.x. [DOI] [PubMed] [Google Scholar]
- 25.Lee OKA, Chung YFL, Chan MF, Chan WM. Music and its effect on the physiological responses and anxiety levels of patients receiving mechanical ventilation: A pilot study. Intens Care. 2004;14(5):609–619. doi: 10.1111/j.1365-2702.2004.01103.x. [DOI] [PubMed] [Google Scholar]
- 26.Ledingham IM, Bion JF, Newman LH, McDonald JC, Wallace PGM. Mortality and morbidity amongst sedated intensive care patients. Resuscitation. 1988;16:69–77. doi: 10.1016/0300-9572(88)90008-1. [DOI] [PubMed] [Google Scholar]
- 27.Rotondi AJ, Chelluri L, Sirio C, et al. Patients' recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Crit Care Med. 2002;30(4):746–752. doi: 10.1097/00003246-200204000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Chlan L. Integrating nonpharmacological, adjunctive interventions into critical care practice: A means to humanize care? Am J Crit Care. 2002;11(1):14–16. [PubMed] [Google Scholar]
- 29.De Jonghe B, Cook D, Sharshar T, Lefaucheur J, Carlet J, Outin H. Acquired neuromuscular disorders in critically ill patients: a systematic review. Intensive Care Med. 1999;24:1242–1250. doi: 10.1007/s001340050757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hansen-Flaschen JH, Brazinsky S, Basile C, Lanken PN. Use of sedating drugs and neuromuscular blocking agents in patients requiring mechanical ventilation for respiratory failure: a national survey. JAMA. 1991;266:2870–2875. [PubMed] [Google Scholar]
- 31.Hansen-Flaschen J. Improving patient tolerance of mechanical ventilation: challenges ahead. Crit Care Clin. 1994;10:659–671. [PubMed] [Google Scholar]
- 32.Mazzeo AJ. Sedation for the mechanically ventilated patient. Crit Care Clin. 1995;11:937–955. [PubMed] [Google Scholar]
- 33.Watling SM, Dasta JF, Seidl EC. Sedatives, analgesics, and paralytics in the ICU. Ann Pharmacother. 1997;31:148–153. doi: 10.1177/106002809703100202. [DOI] [PubMed] [Google Scholar]
- 34.Brush DR, Kress JP. Sedation and analgesia for the mechanically ventilated patient. Clin Chest Med. 2009;30(1):131–141. doi: 10.1016/j.ccm.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 35.Han L, Li JP, Sit JWH, Chung L, Jiao ZY, Ma WG. Effects of music intervention on physiological stress response and anxiety level of mechanically ventilated patients in China: A randomized controlled trial. J Clin Nurs. 2008;19(7–8):978–987. doi: 10.1111/j.1365-2702.2009.02845.x. [DOI] [PubMed] [Google Scholar]
- 36.Dijkstra BM, Gamel C, van der Bijl JJ, Bots ML, Kesecioglu J. The effects of music on physiological responses and sedation scores in sedated, mechanically ventilated patients. J Clin Nurs. 2010;19(7–8):1030–1039. doi: 10.1111/j.1365-2702.2009.02968.x. [DOI] [PubMed] [Google Scholar]
- 37.Moher D, Liberati A, Tetziaff J, Altman DG, The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. Ann Int Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 38.Garrard J. Health sciences literature review made easy. 3rd ed. Sudbury, MA: Jones & Bartlett Learning, LLC; 2011. [Google Scholar]
- 39.Saadatmand V, Rejeh N, Heravi-Karimooi M, et al. Effect of nature-based sounds' intervention on agitation, anxiety, and stress in patients under mechanical ventilator support: A randomized controlled trial. Int J Nurs Stud. 2013;50(7):895–904. doi: 10.1016/j.ijnurstu.2012.11.018. [DOI] [PubMed] [Google Scholar]
- 40.Chlan L. Effectiveness of a music therapy intervention on relaxation and anxiety for patients receiving ventilatory assistance. Heart Lung. 1998;27(3):169–176. doi: 10.1016/s0147-9563(98)90004-8. [DOI] [PubMed] [Google Scholar]
- 41.Chlan LL. Psychophysiological responses of mechanically ventilated patients to music: A pilot study. Am J Crit Care. 1995;4(3):233–238. [PubMed] [Google Scholar]
- 42.Almerud S, Petersson K. Music therapy -- a complementary treatment for mechanically ventilated intensive care patients. Intensive Crit Care Nurs. 2003;19(1):21–30. doi: 10.1016/s0964-3397(02)00118-0. [DOI] [PubMed] [Google Scholar]
- 43.Twiss E, Seaver J, McCaffrey R. The effect of music listening on older adults undergoing cardiovascular surgery. Nurs in Crit Care. 2006;11(5):224–231. doi: 10.1111/j.1478-5153.2006.00174.x. [DOI] [PubMed] [Google Scholar]
- 44.Chlan L, Tracy MF, Nelson B, Walker J. Feasibility of a music intervention protocol for patients receiving mechanical ventilatory support. Altern Ther. 2001;7(6):80–83. [PubMed] [Google Scholar]
- 45.Chlan LL, Engeland WC, Anthony A, Guttormson J. Influence of music on the stress response in patients receiving mechanical ventilatory support: A pilot study. AJCC. 2007;16(2):141–145. [PubMed] [Google Scholar]
- 46.Stubbs T. Experiences and perceptions of music therapy in critical illness. Nurs Times. 2005;101(45):34–36. [PubMed] [Google Scholar]
- 47.Beaulieu-Boire G, Bourque S, Chagnon F, Chouinard L, Gallo-Payet N, Lesur O. Music and biological stress dampening in mechanically-ventilated patients at the intensive care unit ward -- a prospective interventional randomized crossover trial. J Crit Care. 2013;28(4):442–450. doi: 10.1016/j.jcrc.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 48.Conrad C, Niess H, Jauch K, Bruns CJ, Hartl WH, Welker L. Overture for growth hormone: Requiem for interleukin-6. Crit Care Med. 2007;35(12):2709–2713. doi: 10.1097/01.ccm.0000291648.99043.b9. [DOI] [PubMed] [Google Scholar]
- 49.Chlan LL, Engeland WC, Savik K. Does music influence stress in mechanically ventilated patients? Inten Crit Care Nurs. 2012;29(3):121–127. doi: 10.1016/j.iccn.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]