Background
Over the past decade, the transition from pediatric to adult health care of adolescents and young adults (AYA) with a variety of chronic health conditions has garnered increasing attention (Baldassano et al., 2002; COMMITTEE ON PEDIATRIC AIDS, 2013; Crowley, Wolfe, Lock, & McKee, 2011; DeBaun & Telfair, 2012; Freyer, 2010; Jurasek, Ray, & Quigley, 2010; Peters & Laffel, 2011; Prior, McManus, White, & Davidson, 2014; J. Reiss & Gibson, 2002; Sable et al., 2011; Tuchman, Schwartz, Sawicki, & Britto, 2010). The increased attention is due, in part, to a growing body of evidence that shows that AYA access to and use of healthcare services declines significantly during the transitional period and that this decline in health service utilization is associated with worse health outcomes(Blinder et al., 2013; Camfield & Camfield, 2011; Hemker, Brousseau, Yan, Hoffmann, & Panepinto, 2011; Lotstein et al., 2013; Sawyer, Drew, Yeo, & Britto, 2007; Sheehan, While, & Coyne, 2015). Recent systematic reviews of the transition experiences of young adults with type 1 diabetes and congenital heart disease have shown that young adults have a much lower clinic attendance rate after transferring to adult care(Heery, Sheehan, While, & Coyne, 2015; Sheehan et al., 2015). For example, one Canadian study of AYA with complex congenital heart disease found that less than half of the young adults studied successfully transferred to the adult heart center within a 2 year period and that patients who did not transfer reported significantly more comorbidities than those who did (Reid et al., 2004). The low transfer rate is striking given that clinical guidelines advise follow-up at least every six months. The root causes of such gaps in care and suboptimal transfers are varied, and may be related to loss of health insurance in the United States or to a number of other provider-, patient-, and family-related barriers to health care transition articulated elsewhere (Fair, Sullivan, Dizney, & Stackpole, 2012; Okumura et al., 2010; Peter, Forke, Ginsburg, & Schwarz, 2009; J. G. Reiss, Gibson, & Walker, 2005).
To improve the quality of care of AYA during this critical transitional period, the American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Physicians released a joint clinical report in 2011 that provided detailed guidance for transitioning all youth, including those with special healthcare needs (Cooley & Sagerman, 2011). Based on this guidance, the Got Transition/National Center for Healthcare Transition developed several tools to promote quality improvement efforts within practices and health systems, and enumerated the six core elements of Health Care Transition clinical practice: 1) establishment of a transition policy; 2) transition tracking and monitoring; 3) assessment of transition readiness; 4) transition planning; 5) transfer of care; and 6) transfer completion (Got Transition/Center for Health Care Transition Improvement, 2014).
The joint clinical report on transitions and the Got Transition guidelines have spurred increased investigation of various aspects of health care transition including transition readiness assessment, transition planning, and biomedical outcomes such as disease status following transition (Fernandes et al., 2012; Fredericks et al., 2010; Gurvitz et al., 2013; McPherson, Thaniel, & Minniti, 2009; Moynihan, Saewyc, Whitehouse, Paone, & McPherson, 2013; Nakhla, Daneman, To, Paradis, & Guttmann, 2009; Reid et al., 2004; Sawicki et al., 2011; Wiener, Zobel, Battles, & Ryder, 2007; Wray, Frigiola, & Bull, 2013; Yeung, Kay, Roosevelt, Brandon, & Yetman, 2008). However, to date, the rigorous criteria for evaluating intervention studies in other areas of pediatric research have not been broadly applied to the evaluation of transition interventions. Transfer of care, one of the six Got Transition core principles, is an important health services measure that may reflect on an individual patient’s transition preparation and may predict future outcomes.
The present study aims to systematically review the current health care transition literature to identify studies that evaluated the effect of a transition intervention on the discrete outcome of transfer from pediatric to adult care.
Methods
Framework and definitions
In order to evaluate the impact of transition programs on transfer from pediatric to adult care, the population of interest chosen for this review included adolescents and young adults between 14 and 25 years with chronic medical illness since transfer is most likely to occur in this age group. The interventions of interest were any discrete transition interventions that were formal hospital or clinic-affiliated programs that aimed to fulfill at least one of the six Got Transitions core elements. The comparisons of interest were between patients participating in the transition programs and others who were not. The outcome of interest was transfer, which was defined as attending at least one appointment with an adult healthcare provider. Transfer was chosen because it is one of the Got Transitions core principles, and it is an important health services process measure associated with future health outcomes that is discretely measurable.
Literature search
The PubMed, Embase, and PsycInfo databases were searched using a strategy developed by a medical librarian (MvI) in collaboration with the other authors. The search combined a comprehensive list of relevant subject headings and textwords for chronic illness (both in general and including specific chronic illnesses), healthcare transitions, and the adolescent and young adult age group. No date limits were applied, and results were limited to English language publications. Additional articles were identified through review of the reference lists of relevant review articles. The full search strategy is included as on-line supplement Appendix 1.
Study Selection
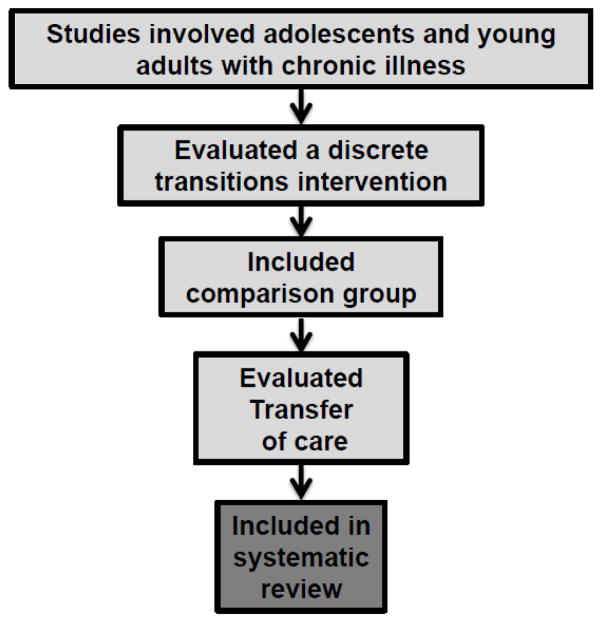
Two reviewers (PC and RC) independently reviewed the titles of all publications produced by the initial search using the framework outlined in Figure 1. Titles that were definitively unrelated to the review focus were excluded. The abstracts of the remaining articles were reviewed with reference to the following criteria: (1) the publication was an evaluative study of a discrete transition intervention and included a comparison group; (2) the population studied included adolescents and/or young adults; and (3) the publication included outcomes data on transfer from pediatric to adult care. Abstracts that definitively did not meet these criteria were excluded. Using the aforementioned criteria, the remaining articles were then reviewed in full by three authors (RC, PC, and GM) to determine final inclusion or exclusion from analysis.
Figure 1.
Analytic framework for study selection.
Data Extraction
Data was extracted by one reviewer and confirmed for accuracy by a second independent reviewer. For each article, the following elements were extracted: the number of subjects reported, age range, sex distribution, primary medical condition of the study population, the country where the study was conducted, a description of the intervention, study design, comparison group, and outcomes measured in the study. The primary outcome of interest was transfer defined as the proportion of patients in transition programs who transferred from pediatric to adult health care settings. Secondary outcomes included clinical laboratory values, quality of life, and patient and family satisfaction as reported in the publications. Conflicts were resolved through consensus with agreement required of all three authors.
Results
Literature Search
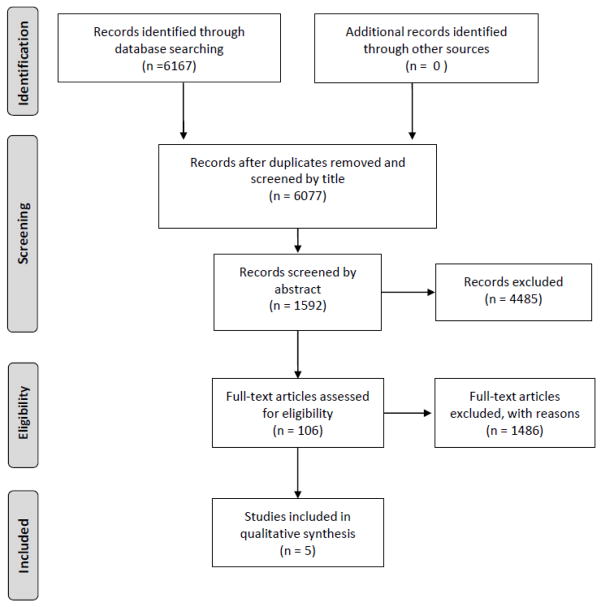
We identified 6167 articles for review and reviewed 106 at the full text level. Five articles met inclusion criteria and were selected for the review (Figure 2).
Figure 2. PRISMA flow diagram.
From Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(6): e1000097.
doi:10.1371/journal.pmed1000097 For more information, visit www.prisma-statement.org
Patient Characteristics
The patients in these studies included adolescents between the ages of 14 to 25 years old. The five interventions were conducted in five different countries including the United States, United Kingdom, Canada, Italy, and Australia. Four of the interventions involved patients with Type 1 diabetes, and one intervention involved patients with sickle cell disease.
Intervention Characteristics
All of the interventions were deployed in specialty care clinics (4 diabetes,1 sickle cell) (Cadario et al., 2009; Hankins et al., 2012; Johnston, Bell, Tennet, & Carson, 2006; Steinbeck, Harvey, Shrewsbury, Donaghue, & Woodhead, 2012; Van Walleghem, MacDonald, & Dean, 2008). Patients were identified as “ready to transition” either based on age or their pediatric provider’s assessment of readiness. The interventions’ characteristics are summarized in Table 1.
Table 1.
Transition intervention characteristics
| Transition Program | Target patient population | Providers | Intervention |
|---|---|---|---|
| Saturday Young Persons’ Clinic at Royal Victoria Hospital, Belfast, United Kingdom (Johnston et al. 2006) | 16 to 25 years old Type 1 diabetes | Pediatric and adult endocrinologist |
|
| The Maestro Project, Manitoba, Canada (Van Walleghem et al. 2008) | 18 to 25 years old Type 1 diabetes | System navigator |
|
| Maggiore della Carita Hospital, Novara, Italy (Cadario et al. 2009) | 18 to 20 years old Type 1 diabetes | Pediatric & adult endocrinologist Transitions coordinator |
|
| Transition Pilot Program at St. Jude’s, Nashville, TN, USA (Hankins et al. 2012) | 17 to 19 years old Sickle Cell Disease (SCD) | Pediatric nurse case manager |
|
| Comprehensive transition program, Children’s Hospital in Westmead or Sydney Children’s Hospital, Australia (Steinbeck et al. 2014) | ≥ 16 years old Type 1 diabetes | Transition-coordinator |
|
The activities, frequency of contact, and types of healthcare providers involved in each transition interventions varied greatly. Three of the interventions were led by pediatric nurse case managers, health system navigators, or transition coordinators (Hankins et al., 2012; Steinbeck et al., 2012; Van Walleghem et al., 2008). The responsibilities of the health system navigators and transition coordinators included contacting patients about the transition process, setting up patients’ first appointments in adult clinics, and making phone calls to check in on patients who transitioned to adult care. The transition interventions occurred outside of clinic time and included activities such as tours of adult clinics and meeting healthcare team members, maintaining websites, and telephone calls. In the other two programs, physicians led the transition intervention during clinic appointments (Cadario et al., 2009; Johnston et al., 2006). In one program, an adult endocrinologist identified pediatric patients that were ready for transition and offered them the option to attend a Saturday morning clinic that was intended specifically for adolescents(Johnston et al., 2006). In the other program, pediatric and adult providers jointly conducted a transitional visit (Cadario et al., 2009). After the joint appointment no formal contact was scheduled by the pediatric care team to follow up on patients after transition.
Study Designs
The selected studies examined discrete transitions programs and recorded the outcome of transfer from pediatric to adult healthcare. A summary of the study characteristics can be found in Table 2. The studies involved small-to-moderate samples ranging from 26 to 165 participants. Four of the studies were retrospective observational studies (Cadario et al., 2009; Hankins et al., 2012; Johnston et al., 2006; Van Walleghem et al., 2008) and one was a pilot prospective randomized controlled trial (RCT)(Steinbeck et al., 2012). Of the four retrospective studies, two were cohort studies that compared patients who voluntarily decided to participate in the intervention program with patients who did not participate (Hankins et al., 2012; Johnston et al., 2006). The remaining two studies used pre-post designs and compared outcomes in adolescents cared for prior to inception of the transition program to adolescents care for after inception of the program (Cadario et al., 2009; Van Walleghem et al., 2008).
Table 2.
Study characteristics
| Study design | Cohorts | Outcomes | Results | |
|---|---|---|---|---|
| Johnston et al. 2006 | Retrospective observational cohort study (n=33) | Saturday young persons’ clinic (n=18) vs. Routine weekday adult diabetes clinic (n=15) |
Primary: Number of failed appointments over 2 years post-pediatric transfer Secondary: Hemoglobin A1C over 2 years post-pediatric transfer |
|
| Van Walleghem et al. 2008 | Pre-/post, retrospective observational cohort study (n=165) | Transition pilot program participants (n= 64) vs. non-participants (n=101) |
Primary: Number of medical visits Secondary: 1) Number of education visits; 2) Number of hospitalizations for diabetic ketoacidosis or severe hypoglycemia |
|
| Cadario et al. 2009 | Pre-/post, Retrospective observational cohort study (n=62) | Structured transition program participants (n= 30) vs. non-participants (n=32) |
Primary: Clinic attendance rates Secondary: 1) mean HbA1c; 2) transition experience |
|
| Hankins et al. 2012 | Retrospective observational study (n=83) | Transition pilot program (n= 34) vs. no program (n= 49) | Primary: Visit to adult hematology clinic within 3 months post-pediatric discharge |
|
| Steinbeck et al. 2014 | Randomized controlled trial (n=26) | Comprehensive transition program (CTP) (n= 14) vs. Standard clinical practice (n = 12) |
Primary: Engagement and retention in the adult service 12 months post-transfer from pediatric care Secondary: 1) HbA1C; 2) diabetes-related hospitalizations; 3) microvascular complications; 4) global self-worth |
|
Outcomes
The primary outcome of all of the studies was the proportion of patients who successfully transferred from pediatric to adult clinics or clinic attendance. The follow-up time for evaluating outcomes ranged from three to 24 months after exit from pediatric care. Three of the five studies showed that patients in the transition programs had higher rates of successful transfer and or higher rates of attendance in adult clinics than patients who did not participate in the programs (Cadario et al., 2009; Hankins et al., 2012; Van Walleghem et al., 2008) (Table 2). The remaining two studies found no statistically significant differences in transfer rates between transition and non-transition intervention groups(Johnston et al., 2006; Steinbeck et al., 2012). The two studies that showed no difference in transfer or clinic attendance rates include a prospective RCT (n=26) of a pilot transition program for patients with type 1 diabetes(Steinbeck et al., 2012) and an observational study evaluating an adolescent clinic(Johnston et al., 2006).
Secondary outcomes included laboratory values, hospitalizations, and patient satisfaction. Three of the four diabetes transition programs measured hemoglobin A1C (HbA1C) levels as an indication of glycemic control after transfer(Cadario et al., 2009; Johnston et al., 2006; Steinbeck et al., 2012). One of these studies showed improved HbA1c control for transition program participants(Cadario et al., 2009) while the others showed no improvement (Johnston et al., 2006; Steinbeck et al., 2012).
Discussion
This systematic review examined studies of healthcare transition interventions that included comparison groups and specifically evaluated and reported on the outcome of transfer from pediatric to adult health care. By examining the narrow health services outcome of transfer, this review builds on prior reviews in the literature that have examined discrete outcomes of transition interventions (Prior et al., 2014). This review also highlights specific methodological improvements that could move the study of transition interventions and outcomes forward meaningfully.
This review found only five studies that included a comparison group and measured transfer as a discrete outcome. This small number may be due to the fact that many transition programs are developed as clinical programs, not research programs. For such programs, using randomization or having a control group that does not receive the intervention may not be practical. The difficulty of rigorously studying the outcome of transfer is further underscored by the fact that only one of the five studies identified was an RCT while the other four studies were small, non-randomized, and used convenience sampling. The lack of prospective evaluation of transfer outcomes may also derive from challenges involved in recruiting and studying AYAs longitudinally. As an example, Steinbeck et al. reported difficulties recruiting AYA participants and achieving adequate evaluative power even though the study staff was experienced in working with AYAs (Steinbeck et al., 2012).
This systematic review also highlights the varied definitions of successful transfer. Some studies focused on attendance at an initial adult-centered appointment, others on the time gap between pediatric and adult visits, and still others on both initiation and continuation in adult care. All three are crucial aspects of transfer, but not all are consistently assessed or reported, and further work is needed to determine which measures of transfer are most closely associated with clinical outcomes. More clearly defining the transfer process and its metrics will help improve the designs of future studies of transition interventions and guide quality improvement initiatives for transitioning AYA with chronic illness.
In addition to variability in defining transfer, there was a great diversity of interventions deployed in these five studies, and each was distinct in intensity and cost. Some interventions included a single intervention such as a joint adult-pediatric clinic visit while others had multiple concurrent components, such as joint adult-pediatric clinic visits and follow-up with a nurse practitioner. Understanding the potential contributions of each component in supporting transfers will be important to ensure that transition interventions are as efficient and cost-effective as possible while achieving the desired outcomes. Future studies should employ designs that measure intervention delivery fidelity and vary the components received to evaluate which components are most effective.
Limitations of this systematic review include the narrow focus on transfer as the central outcome. Many excellent transition interventions that have been evaluated using outcomes other than transfer and that have contributed significantly to the transition literature were not included in this review (Prior et al., 2014). Successful transfer is a process measure and while poor transfer is related to worse outcomes, it has not been definitively established that successful transfer leads to improved outcomes. Also, all of the studies were conducted in different countries with different healthcare systems. Given that healthcare transfer as a process measure is deeply affected by the health system and social context of the patient, a program successfully deployed in one national health system context may not be effective in another. A successful transfer may also be defined differently in distinct health systems. Finally, the focus of this review was on specialty care transfer. Studies of primary care transfer and studies of care models in which AYA continue to see the same provider but with a shift from child- to adult-focused care were not identified nor evaluated. Despite these limitations, it was encouraging to find that for three of the interventions reviewed, participants had higher transfer rates than comparators.
In summary, this systematic review found that few studies have evaluated the impact of transition interventions for AYA with chronic illness on the outcome of transfer from pediatric to adult-centered care, and that the few studies that have reported on this outcome have been limited by methodological challenges including non-randomization and convenience sampling. The goals of transition interventions are not only to prepare young people to thrive in adult-centered care settings, but to help AYA arrive in adult-centered care the first place. Without successful transfer, the benefits of rich healthcare transition interventions are significantly limited. While the current evidence base to guide healthcare transfer is lacking, this systematic review’s findings may provide a foundation for future research that rigorously examines the key components of effective transfer described above. Most notably, establishing clearer definitions and metrics of transfer success, creating infrastructure that facilitates measurement and tracking of patient transfers, and measuring the impact of discrete intervention components on transfer success will be important in extending the evidence base available to guide practice and ensuring that the positive effects of transition interventions are durable into adulthood.
Supplementary Material
Highlights.
Few studies on transition interventions report on the outcome of transfer of care.
The majority of studies in the review were retrospective observational analyses.
The definition of transfer from pediatric to adult care varied between studies.
Three of the five transition interventions in the review improved transfer rates.
Acknowledgments
Ms. Chu receives support from the National Center for Advancing Translational Sciences of the National Institutes of Health under grant award 1TL1TR001116.
Footnotes
Conflicts of interest: Dr. Chung serves on an advisory board for Pfizer, Inc. Ms. Chu, Dr. Maslow and Ms. von Isenburg have no financial relationships relevant to this article to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Baldassano R, Ferry G, Griffiths A, Mack D, Markowitz J, Winter H. Transition of the patient with inflammatory bowel disease from pediatric to adult care: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. Journal of Pediatric Gastroenterology and Nutrition. 2002;34(3):245–8. doi: 10.1097/00005176-200203000-00001. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11964946. [DOI] [PubMed] [Google Scholar]
- Blinder MA, Vekeman F, Sasane M, Trahey A, Paley C, Duh MS. Age-related treatment patterns in sickle cell disease patients and the associated sickle cell complications and healthcare costs. Pediatric Blood & Cancer. 2013;60(5):828–35. doi: 10.1002/pbc.24459. [DOI] [PubMed] [Google Scholar]
- Cadario F, Prodam F, Bellone S, Trada M, Binotti M, Trada M, Aimaretti G. Transition process of patients with type 1 diabetes (T1DM) from paediatric to the adult health care service: A hospital-based approach. Clinical Endocrinology. 2009;71:346–350. doi: 10.1111/j.1365-2265.2008.03467.x. [DOI] [PubMed] [Google Scholar]
- Camfield P, Camfield C. Transition to adult care for children with chronic neurological disorders. Annals of Neurology. 2011;69(3):437–44. doi: 10.1002/ana.22393. [DOI] [PubMed] [Google Scholar]
- COMMITTEE ON PEDIATRIC AIDS. Transitioning HIV-infected youth into adult health care. Pediatrics. 2013;132(1):192–7. doi: 10.1542/peds.2013-1073. [DOI] [PubMed] [Google Scholar]
- Cooley WC, Sagerman PJ. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128:182–200. doi: 10.1542/peds.2011-0969. [DOI] [PubMed] [Google Scholar]
- Crowley R, Wolfe I, Lock K, McKee M. Improving the transition between paediatric and adult healthcare: a systematic review. Archives of Disease in Childhood. 2011;96:548–553. doi: 10.1136/adc.2010.202473. [DOI] [PubMed] [Google Scholar]
- DeBaun MR, Telfair J. Transition and sickle cell disease. Pediatrics. 2012;130(5):926–35. doi: 10.1542/peds.2011-3049. [DOI] [PubMed] [Google Scholar]
- Fair CD, Sullivan K, Dizney R, Stackpole A. “It’s like losing a part of my family”: transition expectations of adolescents living with perinatally acquired HIV and their guardians. AIDS Patient Care and STDs. 2012;26(7):423–9. doi: 10.1089/apc.2012.0041. [DOI] [PubMed] [Google Scholar]
- Fernandes SM, Khairy P, Fishman L, Melvin P, O’Sullivan-Oliveira J, Sawicki GS, Landzberg MJ. Referral patterns and perceived barriers to adult congenital heart disease care: results of a survey of U.S. pediatric cardiologists. Journal of the American College of Cardiology. 2012;60(23):2411–8. doi: 10.1016/j.jacc.2012.09.015. [DOI] [PubMed] [Google Scholar]
- Fredericks EM, Dore-Stites D, Well A, Magee JC, Freed GL, Shieck V, James Lopez M. Assessment of transition readiness skills and adherence in pediatric liver transplant recipients. Pediatric Transplantation. 2010;14(8):944–53. doi: 10.1111/j.1399-3046.2010.01349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freyer DR. Transition of care for young adult survivors of childhood and adolescent cancer: rationale and approaches. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2010;28(32):4810–8. doi: 10.1200/JCO.2009.23.4278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Got Transition/Center for Health Care Transition Improvement. Six Core Elements of Health Care Transition 2.0. 2014 Retrieved February 20, 2015, from http://www.gottransition.org/providers/index.cfm.
- Gurvitz M, Valente AM, Broberg C, Cook S, Stout K, Kay J, Landzberg M. Prevalence and predictors of gaps in care among adult congenital heart disease patients: HEART-ACHD (The Health, Education, and Access Research Trial) Journal of the American College of Cardiology. 2013;61(21):2180–4. doi: 10.1016/j.jacc.2013.02.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankins JS, Osarogiagbon R, Adams-Graves P, McHugh L, Steele V, Smeltzer MP, Anderson SM. A Transition Pilot Program for Adolescents With Sickle Cell Disease. Journal of Pediatric Health Care. 2012;26(December):45–49. doi: 10.1016/j.pedhc.2012.06.004. [DOI] [PubMed] [Google Scholar]
- Heery E, Sheehan AM, While AE, Coyne I. Experiences and Outcomes of Transition from Pediatric to Adult Health Care Services for Young People with Congenital Heart Disease: A Systematic Review. Congenital Heart Disease. 2015 doi: 10.1111/chd.12251. [DOI] [PubMed] [Google Scholar]
- Hemker BG, Brousseau DC, Yan K, Hoffmann RG, Panepinto JA. When children with sickle-cell disease become adults: lack of outpatient care leads to increased use of the emergency department. American Journal of Hematology. 2011;86(10):863–5. doi: 10.1002/ajh.22106. [DOI] [PubMed] [Google Scholar]
- Johnston P, Bell PM, Tennet H, Carson D. Audit of young people with type 1 diabetes transferring from paediatric to adult diabetic services. Practical Diabetes International. 2006;23(3):106–108. doi: 10.1002/pdi.914. [DOI] [Google Scholar]
- Jurasek L, Ray L, Quigley D. Development and implementation of an adolescent epilepsy transition clinic. The Journal of Neuroscience Nursing: Journal of the American Association of Neuroscience Nurses. 2010;42(4):181–189. doi: 10.1097/JNN.0b013e3181e26be6. [DOI] [PubMed] [Google Scholar]
- Lotstein DS, Seid M, Klingensmith G, Case D, Lawrence JM, Pihoker C, Waitzfelder B. Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatrics. 2013;131(4):e1062–70. doi: 10.1542/peds.2012-1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPherson M, Thaniel L, Minniti CP. Transition of patients with sickle cell disease from pediatric to adult care: Assessing patient readiness. Pediatric Blood & Cancer. 2009;52(7):838–41. doi: 10.1002/pbc.21974. [DOI] [PubMed] [Google Scholar]
- Moynihan M, Saewyc E, Whitehouse SR, Paone MC, McPherson G. 105. Evaluation of the Transition Readiness Assessment Questionnaire (TRAQ) in a Younger Adolescent Population. Journal of Adolescent Health. 2013;52(2):S71–S72. doi: 10.1016/j.jadohealth.2012.10.167. [DOI] [Google Scholar]
- Nakhla M, Daneman D, To T, Paradis G, Guttmann A. Transition to adult care for youths with diabetes mellitus: findings from a Universal Health Care System. Pediatrics. 2009;124:e1134–e1141. doi: 10.1542/peds.2009-0041. [DOI] [PubMed] [Google Scholar]
- Okumura MJ, Kerr EA, Cabana MD, Davis MM, Demonner S, Heisler M. Physician views on barriers to primary care for young adults with childhood-onset chronic disease. Pediatrics. 2010;125(4):e748–54. doi: 10.1542/peds.2008-3451. [DOI] [PubMed] [Google Scholar]
- Peter NG, Forke CM, Ginsburg KR, Schwarz DF. Transition from pediatric to adult care: internists’ perspectives. Pediatrics. 2009;123(2):417–23. doi: 10.1542/peds.2008-0740. [DOI] [PubMed] [Google Scholar]
- Peters A, Laffel L. Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems: a position statement of the American Diabetes Association, with representation by the American College of Osteopathic Family Physicians, the A. Diabetes Care. 2011;34(11):2477–85. doi: 10.2337/dc11-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prior M, McManus M, White P, Davidson L. Measuring the “triple aim” in transition care: a systematic review. Pediatrics. 2014;134(6):e1648–61. doi: 10.1542/peds.2014-1704. [DOI] [PubMed] [Google Scholar]
- Reid GJ, Irvine MJ, McCrindle BW, Sananes R, Ritvo PG, Siu SC, Webb GD. Prevalence and correlates of successful transfer from pediatric to adult health care among a cohort of young adults with complex congenital heart defects. Pediatrics. 2004;113(3 Pt 1):e197–205. doi: 10.1542/peds.113.3.e197. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/14993577. [DOI] [PubMed] [Google Scholar]
- Reiss JG, Gibson RW, Walker LR. Health care transition: youth, family, and provider perspectives. Pediatrics. 2005;115(1):112–20. doi: 10.1542/peds.2004-1321. [DOI] [PubMed] [Google Scholar]
- Reiss J, Gibson R. Health care transition: destinations unknown. Pediatrics. 2002;110(6 Pt 2):1307–14. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12456950. [PubMed] [Google Scholar]
- Sable C, Foster E, Uzark K, Bjornsen K, Canobbio MM, Connolly HM, Williams RG. Best practices in managing transition to adulthood for adolescents with congenital heart disease: the transition process and medical and psychosocial issues: a scientific statement from the American Heart Association. Circulation. 2011;123(13):1454–85. doi: 10.1161/CIR.0b013e3182107c56. [DOI] [PubMed] [Google Scholar]
- Sawicki GS, Lukens-Bull K, Yin X, Demars N, Huang IC, Livingood W, Wood D. Measuring the transition readiness of youth with special healthcare needs: validation of the TRAQ--Transition Readiness Assessment Questionnaire. Journal of Pediatric Psychology. 2011;36(2):160–71. doi: 10.1093/jpepsy/jsp128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawyer SM, Drew S, Yeo MS, Britto MT. Adolescents with a chronic condition: challenges living, challenges treating. Lancet. 2007;369(9571):1481–9. doi: 10.1016/S0140-6736(07)60370-5. [DOI] [PubMed] [Google Scholar]
- Sheehan AM, While AE, Coyne I. The experiences and impact of transition from child to adult healthcare services for young people with Type 1 diabetes: a systematic review. Diabetic Medicine: A Journal of the British Diabetic Association. 2015;32(4):440–58. doi: 10.1111/dme.12639. [DOI] [PubMed] [Google Scholar]
- Steinbeck KS, Harvey V, Shrewsbury Va, Donaghue K, Woodhead H. Outcomes for adolescents with type 1 diabetes mellitus participating in a comprehensive program to aid transition from pediatric to adult care: A pilot randomized controlled trial. Journal of Adolescent Health. 2012;1(2):S77. doi: 10.1111/pedi.12229. [DOI] [Google Scholar]
- Tuchman LK, Schwartz LA, Sawicki GS, Britto MT. Cystic fibrosis and transition to adult medical care. Pediatrics. 2010;125(3):566–73. doi: 10.1542/peds.2009-2791. [DOI] [PubMed] [Google Scholar]
- Van Walleghem N, MacDonald C, Dean H. Evaluation of a systems navigator model for transition from pediatric to adult care for young adults with type 1 diabetes. Diabetes Care. 2008;31(8):1529–1530. doi: 10.2337/dc07-2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiener LS, Zobel M, Battles H, Ryder C. Transition from a pediatric HIV intramural clinical research program to adolescent and adult community-based care services:assessing transition readiness. Social Work in Health Care. 2007;46(1):1–19. doi: 10.1300/J010v46n02_01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wray J, Frigiola A, Bull C. Loss to specialist follow-up in congenital heart disease; out of sight, out of mind. Heart (British Cardiac Society) 2013;99(7):485–90. doi: 10.1136/heartjnl-2012-302831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeung E, Kay J, Roosevelt GE, Brandon M, Yetman AT. Lapse of care as a predictor for morbidity in adults with congenital heart disease. International Journal of Cardiology. 2008;125(1):62–5. doi: 10.1016/j.ijcard.2007.02.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.