Introduction
Emerging adulthood is a newly recognized developmental period of life from the late teens through the twenties (Arnett, 2000; Garvey et al., 2014; Ritholz et al., 2014). During this period, emerging adults explore their identity and experience many new transitions, demands, expectations, and roles as they develop from dependent adolescents to independent young adults (Arnett, 2000). For emerging adults with chronic health care conditions, one transition that must be considered is the move from parent-directed pediatric to self-managed adult healthcare. This transition addresses the medical, psychosocial, educational, and vocational needs of the emerging adult with a lifelong chronic condition (Blum et al., 1993).
In adolescent diabetes care, transitional care from pediatric to adult health services is a high priority. Diabetes is a complex, chronic disease that is increasing in prevalence worldwide (Patterson et al., 2012; Vehik & Dabelea, 2011). In children and adolescents in the United States between 2001 and 2009, the prevalence of type 1 diabetes increased by 21%, affecting males and females, most racial/ethnic, and age groups (Hamman et al., 2014). The incidence rate of type 1 diabetes is rising across Europe by an average of approximately 3-4% per year (Patterson, et al., 2012). In Europe, new cases of type 1 diabetes for youth under 5 are predicted to double by 2020, and the prevalence of type 1 diabetes in youth under 15 is predicted to rise 70% by 2020 (Patterson, Dahlquist, Gyurus, Green, & Soltesz, 2009). As the prevalence of type 1 diabetes in youth increases worldwide, transition from pediatric to adult healthcare services and learning to live with a lifelong chronic condition will become a global concern.
Type 1 diabetes leads to absolute insulin deficiency due to beta cell destruction (American Diabetes Association, 2015); whereas, type 2 diabetes is due to a progressive insulin secretory defect and insulin resistance, often characterized by excessive weight gain (Cali & Caprio, 2008). Concomitant with the rise in pediatric obesity is an increased risk for the future development of type 2 diabetes and prediabetes (Reinehr et al., 2009). Prediabetes consists of impaired fasting glucose 100 to 125 mg/dL (5.6 to 6.9 mmol/L), impaired glucose tolerance to a 2-hour oral glucose tolerance test (OGTT) of 140 to 199 mg/dL (7.8 to 11.0 mmol/L), or A1C 5.7-6.4% (American Diabetes Association, 2015). In the United States National Health and Nutrition Examination Survey (NHANES) of participants aged 12 to 19 years from 1999 to 2008, the prevalence of prediabetes/diabetes increased from 9% to 23% (May, Kuklina, & Yoon, 2012). Between 2001 and 2009 the prevalence for type 2 diabetes increased by 30.5%, in both sexes for ages 10 years and up, and among Hispanic and non-Hispanic white, and African American youth (Hamman, et al., 2014). In light of these increases, there is an urgent need not only to identify youth at risk for prediabetes and type 2 diabetes, but to also ensure appropriate transitional care and ongoing screening into emerging adulthood.
Not only are the rates of prediabetes and diabetes among adolescents increasing and placing a greater demand on health systems for transitional care, emerging adults are also at increased risk for declining health status during this time in transition of health care. At the beginning of emerging adulthood, which coincides with the transition from pediatric to adult care, glycemic control in those with diabetes is known to decrease significantly (Bryden et al., 2001; Insabella, Grey, Knafl, & Tamborlane, 2007). Optimal glycemic control during this time of life reduces the likelihood of serious long-term health complications later in life. Specifically, tight glycemic control during adolescence and emerging adulthood decreases both microvascular and neurological diabetes complications (Blonde, 2012; Silverstein et al., 2005). Seamless transitional care is needed in order to optimize glycemic control for emerging adults and to reduce future complications.
In 2001, the Institute of Medicine's landmark publication, Crossing the Quality Chasm: A New Health System of the 21st Century, provided evidence that the U.S. health care delivery system too often fails to deliver high quality care. Given the expected onslaught of emerging adults with or at risk for developing diabetes and ongoing challenges to address existing gaps in care delivery, a growing abyss may ensue. More young adults may experience suboptimal health care utilization, poor glycemic control, acute exacerbations, and chronic complications, some of which may go undetected (Peters & Laffel, 2011) .
There are ongoing efforts to promote the value of seamless, coordinated, and developmentally appropriate care by leading United States organizations, such as the U.S. Department of Health and Human Service's Maternal and Child Health Bureau (2008), the American Academy of Pediatrics (Cooley & Sagerman, 2011), and the American Diabetes Association (Peters & Laffel, 2011). However, there is currently no consensus model of transitional care for adolescents and emerging adults with diabetes in the United States. Other countries have also addressed transitional care for adolescents with diabetes; however, the majority of evidence worldwide remains at the level of expert agreement or clinical experience rather than being based upon well-conducted randomized controlled trials or meta-analyses with quality ratings (Peters & Laffel, 2011).
Recent publications address the importance of transitional care for youth with type 1 diabetes and propose frameworks for establishing comprehensive models of care (Hanna, 2012; Van Walleghem, MacDonald, & Dean, 2012). Recent systematic reviews have focused on identifying the level of evidence and describing the evidence on diabetes transitional care (Hanna & Woodward, 2013), examining the impact of transitional care on health outcomes and health behaviors in those with type 1 diabetes (Sheehan, While, & Coyne, 2015), and investigating the experiences of diabetes transitional care from the perspective of the patient, parent, and provider (Sheehan, et al., 2015). However, these reviews excluded adolescents and emerging adults with type 2 diabetes or prediabetes whose numbers have drastically increased (Dabelea et al., 2014). The health risks associated with the emerging adult period for those with diabetes, in addition to the increase in older adolescents diagnosed with diabetes and prediabetes, indicate an urgent need for innovative and successful care models for transitional care and beyond. (Winocour, 2014) Therefore, the purpose of this systematic review was to examine the level of evidence from primary research for the process and outcomes of transitional care programs for adolescents and emerging adults with either type 1 diabetes, type 2 diabetes, or prediabetes. Our original PICO (patient, intervention, comparison, outcome) question was: What are the major components of transitional care programs (interventions) and health outcomes compared to usual care for adolescents or emerging adults with type 1 or type 2 diabetes or prediabetes? We also explored studies that reported perceptions of patients, providers, and parents regarding current and proposed transitional care programs. Our intent was to provide a synthesis of the best evidence to inform clinicians, researchers and policy makers of key components of a model of high quality transitional care for emerging adults with diabetes or prediabetes.
Methods
Design
A systemic review was conducted primarily following the Joanna Briggs Institute (JBI) guidelines (Aromataris & Pearson, 2014) and the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement (Liberati et al., 2009; Moher, Liberati, Tetzlaff, & Altman, 2009). The PRISMA statement provides a 27-item checklist and a four phase flow diagram that include items deemed essential for transparent reporting in systematic reviews. PRISMA helps to ensure transparent and complete reporting so that the benefits and harms of an intervention study may be assessed (Liberati, et al., 2009; Moher, et al., 2009).
Search Criteria
The inclusion criteria for target studies were: a) data-based investigations that addressed health care transition for emerging adults with diabetes or prediabetes; b) focused on adolescents aged 14-18 years and/or emerging adults aged 19-29; c) qualitative or quantitative; and d) conducted in the United States or internationally. Exclusion criteria were: a) non-research articles; b) literature review papers; c) theoretical, expert opinion, or editorial articles that did not report empirical findings; d) not a full text article; e) studies not solely focused on health care transition; and f) studies solely focused on chronic conditions other than diabetes or prediabetes. The electronic databases PubMed, Cumulative Index in Nursing and Allied Health Literature (CINAHL), Ovid/MEDLINE, Scopus, Web of Science, and Embase were used for the search. Articles were retrieved from the last 10 years (2004-2014) because this is the time frame when the need to address transitional care began to appear in the literature. Combinations of search terminologies related to health care transition (continuity of care, transitional care, or transition), diabetes (type 1 diabetes, type 2 diabetes, prediabetes, or maturity onset diabetes of the young (MODY), and emerging adults (young adults, young adult men, young adult women, adolescents, late adolescents, college students, high school students, youths, or pediatrics). The search was limited to publications written in English.
Search Outcome
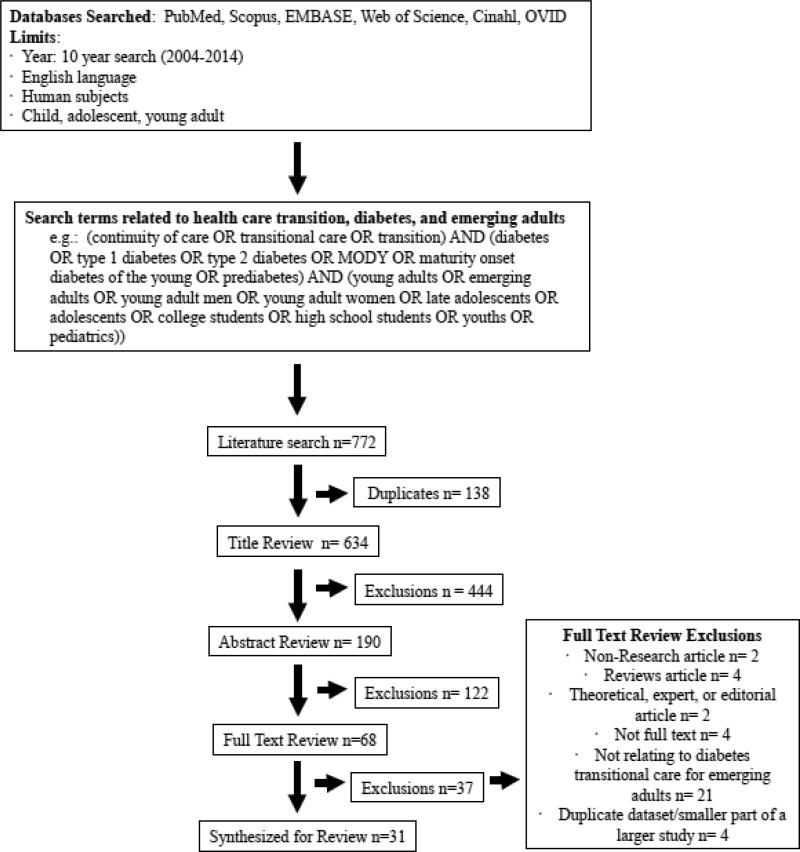
In September, 2014, eligible articles were retrieved independently by two trained graduate student researchers under the supervision of two PhD prepared nurse researchers with the support of a librarian. The initial literature search identified 772 articles across the six databases (Figure 1). Excluding duplicates, 634 articles remained after being evaluated for pre-established inclusion and exclusion criteria. Matched pairs of researchers reviewed the titles of the 634 articles and excluded 444 based upon topics of healthcare that were not related to transitional care or that focused on chronic conditions other than diabetes. An abstract review of 190 articles was then performed by the matched pairs. A total of 122 articles were excluded by review of abstracts; most studies were excluded because they were not designed primarily to explore the diabetes care transition for emerging adults. A full-text review of 68 articles was completed by the matched pairs. Thirty-seven additional articles were excluded in this phase. Reasons for exclusion are noted in Figure 1. The remaining 31 articles were used for the synthesis of the information in this review. Included in this final set of articles were three studies, each of which had separate findings reported in two different articles that used the same data set or a secondary data set (Garvey, et al., 2014; Ritholz, et al., 2014), (Dovey-Pearce, Doherty, & May, 2007; Dovey-Pearce, Hurrell, May, Walker, & Doherty, 2005), and (Allen, Channon, Lowes, Atwell, & Lane, 2011; Allen et al., 2012). Although type 1 diabetes, type 2 diabetes, and prediabetes were all included in the search criteria, the 31 articles remaining for synthesis of the information in this review all focused on individuals with type 1 diabetes. This search process illuminated the absence of research on the transitional needs of individuals with type 2 diabetes and prediabetes and demonstrated the major gap in knowledge in how to best provide transitional care for these individuals.
Figure 1. Search Strategies and Review Process.
The literature search identified 772 articles across the six databases. Duplicates were removed, and articles with titles or abstracts that did not fit within with the inclusion and exclusion criteria were also removed, leaving a total of 68 full text articles for review. Thirty-seven additional articles were excluded during this full text review for the reasons listed in the exclusions box above. The remaining 31 articles were used for synthesis of the information in this review.
Quality Assessment and Grading of Evidence
Once the final set of 31 articles was determined, the quality of each individual article was assessed using three modified scales of assessment criteria based on the JBI (Aromataris & Pearson, 2014; The Joanna Briggs Institute, 2014). The three scales used criteria deemed essential for evaluating either: 1) cross-sectional, 2) intervention and group comparison studies, or 3) qualitative studies (Table 1). The checklists are designed to assess many aspects of a study's quality, including its design, its methods and analysis, and its clinical relevance (Aromataris & Pearson, 2014; The Joanna Briggs Institute, 2014). Assessment included analysis of the aims, methods, results, and conclusions of each research article. Quality assessment was evaluated for inter-rater reliability by matched pairs of researchers using a ten-point system for each scale, with possible total scores ranging from 1 (lowest) to 10 (highest) rating. The score was then used in evaluating the level of evidence for each article.
Table 1.
Quality Assessmenta
| Cross-Sectional Study | Intervention or Group Comparison Study | Qualitative Study |
|---|---|---|
| Did the study address a clearly focused issue? | Is the assignment to treatment groups truly random? | Is there congruity between the stated philosophical perspective and the research methodology? |
| Did the study clearly address the aims? | Are participants blind to treatment allocation? | Is there congruity between the research methodology and the research questions or objectives? |
| Did the authors use an appropriate method to answer their question? | Is allocation to treatment groups concealed from the allocator? | Is there congruity between the research methodology and the methods used to collect data? |
| Were subjects recruited in an acceptable way? | Are the outcomes of people who withdrew described and included in the analysis? | Is there congruity between the research methodology and the representation and analysis of data? |
| Were the measures accurately measured to reduce bias? | Are those assessing the outcomes blind to the treatment allocation? | Is there congruity between the research methodology and the interpretation of results? |
| Were the data collected in a way that addressed the research issue? | Are the control and treatment groups comparable at entry? | Is there a declaration of the researcher's cultural or theoretical orientation? |
| Did the study have enough participants to minimize the play of chance? | Are groups treated identically other than for the named interventions? | Is the influence of the researcher on the research, and vice versa addressed? |
| Was the data analysis sufficiently rigorous? | Are outcomes measured in the same way for all groups? | Is there representation of participants and their voices? |
| Is there a clear statement of findings? | Are outcomes measured in a reliable way? | Is there ethical approval by an appropriate body? |
| Can the results be applied to the local population? | Is appropriate statistical analysis used? | Is there a relationship between the conclusions of the study and the analysis or interpretation of the data? |
Adapted from JBI (Aromataris & Pearson, 2014)
The American Diabetes Association (ADA) evidence grading system of levels A, B, C and E was applied to each article (American Diabetes Association, 2014). Level A indicated clear evidence from a well-conducted generalizable RCT that was adequately powered. Level B indicated supportive evidence from a well-conducted cohort study or case-control study. Level C indicated supportive evidence from poorly controlled or uncontrolled studies, RCT's with one or more major or three or more minor methodological flaws, observational studies with a high potential for bias, case studies or case reports, or conflicting evidence with the weight of the evidence supporting the recommendation. Level E indicated expert consensus or clinical experience.
Results
This systematic review resulted in articles reporting both quantitative studies (18 articles) and qualitative studies (13 articles). The majority of quantitative studies were conducted in North America (United States = 8; Canada =3; Australia = 2; Germany =2; Italy =2; Poland =1), and the majority of qualitative studies were conducted in Europe (United Kingdom = 8, Netherlands =1; Ireland =1; Sweden =1; United Sates = 2) . Only one randomized clinical trial assessing a transitional care intervention met the criteria for evaluation in this review (Huang et al., 2014). Quality scores using the scales adapted from the JBI (Table 1) ranged from 4 to 10, on a scale of 1 (lowest) to 10 (highest). The mean quality score was 8.5 with a standard deviation of 1.7. Level of evidence using ADA grading system ranged from A to C (A: n=1; B: n=6; C: n=24). The majority of studies have a level of evidence rated as C, indicating that the current evidence is primarily of a descriptive and observational nature. The quality score, level of evidence, and summary information for all articles are presented in Table 2.
Table 2.
Study Description and Characteristics
| # | Author/Year | Location of Study | Study Design and Methods | Purpose/Aims | Sample (size, description) | Quality | Level of Evidence |
|---|---|---|---|---|---|---|---|
| 1a | Allen, Channon, Lowes, Atwell, & Lane, 2011 | United Kingdom |
Qualitative; longitudinal qualitative case studies, semi- structured interviews; recruited from 5 different diabetes services throughout the UK |
To explore young adults’ and caregivers’ experiences during transition from child to adult diabetes services |
Adolescents ages 14-22 with T1D (n=46), & mothers (n=39). |
10 | C |
| 2a | Allen et al., 2012 | England | Mixed methods; semi- structured interviews, selected observation, case studies & surveys; recruited from the diabetes services in England |
To identify the mechanisms of a smooth transition to adult diabetes care and the service components through which these can be achieved |
Interviews of health care professionals (n=38), young adults (n=46), and caregivers (n=39); surveys of young adults (n=82). |
10 | C |
| 3 | Begley, 2013 | Ireland | Mixed-methods; surveys with closed and open-ended questions; surveys sent to all known consultants, MDs, CNS's, and APN's |
To clarify how the transition from childhood to adult healthcare is managed in young people with cystic fibrosis (CF) and T1D |
Consultants, MDs, CNS's, and APN's caring for teens with CF and T1D; (n=71; 54% response rate) |
8 | C |
| 4 | Busse et al., 2007 | Germany | Quantitative; cross-sectional structured survey administered through phone interview; Sample eligibility criteria: at least 18 years of age, at least 6 months had elapsed after transition and the patient had no other chronic disorder apart from diabetes |
To determine the patients’ perception of transfer arrangements and to analyze health care use and metabolic control |
Cases identified through diabetes registry of the Clinic and Policlinic for Children and Adolescents, University of Leipzig, Germany; (n=101) |
10 | C |
| 5 | Cadario et al., 2009 | Italy | Quantitative; retrospective cohort study; comparison group of PDS patients discharged with an unstructured transfer; exposure group discharged with structured transition |
To investigate the outcomes of a structured transition program to an unstructured one |
Adolescents and young adults (n=62) discharged from the pediatric diabetes service (PDS) to the adult pediatric service (ADS) |
9 | C |
| 6 | de Beaufort, Jarosz-Chobot, Frank, de Bart, & Deja, 2010 | International | Quantitative; cross-sectional questionnaire |
To evaluate the practices of diabetes health care providers concerning the transition from pediatric to adult diabetes care |
Email with survey link sent to all members of the International Society for Pediatric and Adolescent Diabetes (n=92; 16% response rate) |
9 | C |
| 7b | Dovey-Pearce, Doherty, & May, 2007 | England | Qualitative; thematic analysis of audio recorded interviews; recruited from young adults served by specialist diabetes services |
To describe and understand the influence of diabetes upon psychosocial development and to highlight the implications for healthcare teams. |
16-25 year olds with T1D (n=19); 8 males; 11 females |
10 | C |
| 8b | Dovey-Pearce, Hurrell, May, Walker, & Doherty, 2005 | England | Qualitative; semi-structured interviews and focus groups; recruited from young adults served by specialist diabetes services |
To understand the opinions of young adults with diabetes who were receiving secondary care services about the provision of diabetes services |
16-25 year olds with T1D (n=19); 8 males; 11 females |
10 | C |
| 9c | Garvey et al., 2014 | United States of America |
Qualitative; focus group interviews; recruited from emerging adults receiving adult diabetes care at a single center |
To explore the experience of transition from pediatric to adult diabetes care reported by post- transition emerging adults with T1D |
Young adults with T1D, 22- 30 years old, diagnosed with diabetes at ≤18 years of age (n=26) |
8 | C |
| 10 | Garvey et al., 2013 | United States of America |
Quantitative; cross-sectional survey; recruited from emerging adults with T1D who had been previously followed in the pediatric diabetes clinic at Boston Children's hospital |
To describe the current status of adult diabetes care in young adults with T1D and examine associations between health care transition experiences and care utilization |
205 surveys sent to sample, 65 returned (32% response rate) |
9 | C |
| 11 | Garvey et al., 2012 | United States of America |
Quantitative; cross-sectional survey; recruited from emerging adults with T1D aged 22-30 years, under the care of any adult diabetes specialist at the Joslin Diabetes Center |
To examine characteristics of the transition from pediatric to adult care in emerging adults with T1D and evaluate associations between transition characteristics and glycemic control |
484 mailed surveys, 258 collected (53% response rate) |
10 | C |
| 12 | Gerber, Solomon, Shaffer, Quinn, & Lipton, 2007 | United States of America |
Quantitative; cohort study; no control; one intervention group followed; sample eligibility criteria: fluent in English, diagnosed with diabetes prior to 18th birthday, over 18 years of age at time of recruitment |
To evaluate the effectiveness of an internet-based transition support program, STYLE, in an urban cohort of individuals between 19-26 years of age |
19 participants given intervention, only 12 attended feedback sessions for analysis |
4 | C |
| 13 | Hanna et al., 2013 | United States of America |
Quantitative; longitudinal study; pre-post test design; three consecutive years of recruiting students with T1D in their last 6 months of high school |
To examine: (1) how diabetes care responsibility changed in relation to time and living situation and (2) the association of diabetes self-efficacy, gender and glycemic control with changes in diabetes care responsibility |
n = 113 (17-19 year olds with T1D); |
10 | B |
| 14 | Helgeson et al., 2013 | United States of America |
Quantitative; questionnaire with repeated samples; time 1 during senior year of high school; time 2 one year later; recruited from a previous study in the Children's Hospital of Pittsburgh in 2002-2004 |
To describe the transition of youth with T1D from pediatric to adult healthcare services and examine the link of this transition with self- care and glycemic control and distinguish medical treatment from different physicians |
118 adolescents who utilize either a pediatric endocrinologist or adult physician |
10 | C |
| 15 | Hilliard et al., 2014 | United States of America |
Mixed methods; surveys with open ended questions; pre- transition group was recruited from a pediatric diabetes clinic; post-transition recruited from 18-22 year olds who were treated at the same clinic |
To describe the concerns, expectations, preferences, and experiences of youth and parents before and after transitioning from pediatric to adult care. |
Pre-transition: adolescents aged 15-17 with T1D (n=20) Post-transition: young adults aged 18-22 (n=59) |
9 | C |
| 16 | Holmes- Walker, Llewellyn, & Farrell, 2007 | Australia | Quantitative; simple interrupted time series design; young adults aged 15-25 with T1D were referred to the program that was based at a tertiary adult referral hospital in July 2001 |
To determine if a transition support program could maintain attendance at a specialist clinic, improve diabetes control, and reduce acute hospital admissions in 15-25 year olds with T1D |
Patients (n=191) referred were seen in a young adult diabetes clinic and did not routinely meet the transition coordinator or adult diabetes specialist |
4 | B |
| 17 | Huang et al., 2014 | United States of America |
Quantitative; randomized Clinical Trial; recruited from 1 pediatric tertiary care academic medical center |
To evaluate whether a internet- and mobile phone-delivered disease management intervention improves disease management, self-efficacy, and communication outcomes |
Adolescents (n=81) aged 12- 22 with either inflammatory bowel disease, cystic fibrosis, or T1D |
7 | A |
| 18 | Kime, 2013 | United Kingdom |
Qualitative; focus groups | To report on the transition process and the role of community nurses in young peoples’ diabetes care |
9 acute trusts across the region and more than 300 participants, parents, and professionals |
7 | C |
| 19 | Lotstein et al., 2013 | United States of America |
Quantitative; retrospective cohort study; utilized SEARCH for Diabetes in Youth Study data to find those who completed at least 1 follow up visit after age 18 |
Describe sociodemographic and clinical correlates of poor glycemic control associated with transfer of care of youth with T1D diagnosed in adolescence |
185 American adolescents (ages 13-18) with T1D |
10 | B |
| 20 | Lundin, Ohrn, & Danielson, 2008 | Sweden | Qualitative; ethnographic approach with formal and informal interviews; participants observed from 2 pediatric diabetes clinics and 2 adult diabetes clinics |
Describe care culture in pediatric and adult diabetes outpatient clinics and implications for care of adolescents |
Observations of 51 participants; interviews of 10 physicians |
9 | C |
| 21 | Markowitz & Laffel, 2012 | United States of America |
Quantitative; pre-post test design to evaluate group support program; interested patients recruited through flyers |
To examine the effects of a group support program |
15 emerging adults with T1D; ages 18-30 |
10 | C |
| 22 | Nakhla, Daneman, To, Paradis, & Guttmann, 2009 | Canada | Quantitative; retrospective cohort study; examined health administrative and survey data from Ontario Diabetes Database |
Compare rates of DM related hospitalization & retinopathy screening before and after transition to adult care. |
1507 young adults with T1D | 10 | B |
| 23 | Neu et al., 2010 | Germany | Quantitative; pre-post questionnaire after transition to adult care; recruited from a single hospital |
Identify the type of clinical care received by young T1D patients who transition to adult care, and assess the metabolic status of long term treatment after transition |
99 patients (28 drop outs, 28.2%) average age at transition: 21.8 years |
10 | C |
| 24 | Perry, Steinbeck, Dunbabin, & Lowe, 2010 | Australia | Quantitative; retrospective cohort study; case note audits at 6 diabetes clinics |
To document diabetes health services use and indices of glycemic management of young people with T1D |
239 young adults with T1D ages 18-28; |
10 | C |
| 25 | Price et al., 2011 | United Kingdom |
Qualitative; semi-structured interviews; recruited from adolescents attending a diabetes clinic |
To evaluate the transition pathway in diabetes using qualitative methods in order to explore the experiences and suggestions of the young people |
11 young adults aged 16-18 with T1D |
8 | C |
| 26c | Ritholz et al., 2014 | United States of America |
Qualitative; focus group interviews; recruited from emerging adults receiving adult diabetes care at a single center |
To explore perceptions emerging adults with T1D have of their patient-provider relationships across the transition from pediatric to adult care |
Young adults with T1D, 22- 30 years old, diagnosed with diabetes at ≤18 years of age (n=26) |
8 | C |
| 27 | Scott, Vallis, Charette, Murray, & Latta, 2005 | Canada | Mixed-methods; questionnaire followed by telephone interview; invitation letters were sent to former patients of a tertiary pediatric diabetes care center |
To understand why young adults drop out of diabetes care during transition from pediatric to adult health care and to obtain information as how the care could better meet their needs |
76 participants returned questionnaires (33.3% response rate); 19 telephone interviews |
7 | C |
| 28 | van Staa, Jedeloo, van Meeteren, & Latour, 2011 | Netherlands | Qualitative; semi-structured interviews on young adult patients and on their parents and healthcare providers; potential participants were randomly selected from a list of young adult patients officially discharged in the previous 2 years |
To examine the expectation and experience with transfer and perceived quality of care in pediatric care and adult services |
3 of the 24 randomly selected participants were diagnosed with diabetes; aged 15-22; 24 parents; 17 healthcare providers |
8 | C |
| 29 | Van Walleghem, MacDonald, & Dfan, 2008 | Canada | Quantitative; 2 year prospective cohort study with follow up every 6 months; data gathered from database review and audit of medical records |
To report clinical outcomes and identify barriers to care for young adults with T1D after transfer from pediatric to adult care |
Two cohorts followed: Younger group aged 18 years (n=84) from the “Maestro Project” Older group aged 19-25 (n=64) who were transferred to adult care without the initial support |
6 | C |
| 30 | Vanelli et al., 2004 | Italy | Quantitative; 8 year retrospective cohort study; data gathered from T1D patients at a hospital |
To report the effects of a protocol for an uninterrupted procedure to transfer adolescents with T1D from pediatric to adult clinic in a hospital |
73 patients with T1D, average age of 26.5 years (sd=2.6) |
8 | C |
| 31 | Wilson, 2010 | United States of America |
Qualitative; semi-structured phone interviews; convenience sample recruited from colleges and universities |
To explore the experiences of young adults managing T1D at college or university |
23 young adults with T1D; aged 17-19 |
6 | C |
indicates studies utilizing same dataset or sample
indicates studies utilizing same dataset or sample
indicates studies utilizing same dataset or sample
Qualitative and quantitative articles were reviewed by the authors and it was determined that the goals and purpose of both quantitative and qualitative studies reviewed were similar (Table 2). The authors identified common objectives of the articles, and the results of the articles were synthesized into the following categories: current status of transitional care, perceptions of transitional care, effects of transitional care on diabetes outcomes, and elements of successful transitional care.
Current Status of Transitional Care
Transition from pediatric to adult health care for adolescents with type 1 diabetes is suggested to occur between the ages of 14 to 25 (de Beaufort, Jarosz-Chobot, Frank, de Bart, & Deja, 2010). Median age of transition is 20.1 years (Lotstein et al., 2013). The majority of providers (90%) are in agreement that transition planning should begin at least one year prior to transition (de Beaufort, et al., 2010). Reasons for transition to adult care are topped by the patient's wish to transition followed by suggestion to transition given by the treating pediatric provider (Neu et al., 2010).
The majority of emerging adults feel prepared for the transition from pediatric to adult diabetes care (Garvey et al., 2013; Neu, et al., 2010). Emerging adults know they will age out of pediatric care, and transition is accepted as an inevitable and a natural process (Begley, 2013; Ritholz, et al., 2014); however, 34% of emerging adults still report a gap of longer than six months between pediatric and adult diabetes care (Garvey et al., 2012). There are noticeable differences between the cultures, communication styles, expectations, and parental involvement in care in pediatric and adult care clinics (Kime, 2013; Lundin, Ohrn, & Danielson, 2008; Ritholz, et al., 2014; van Staa, Jedeloo, van Meeteren, & Latour, 2011). These differences often make emerging adults feel uncomfortable in the adult clinic and incompetent to manage their diabetes without parental support and reassurance (Allen, et al., 2011; Hilliard et al., 2014). Staffing and resource availability were also recognized as major differences between pediatric and adult care clinics. In pediatric care clinics, a multidisciplinary team consisting of a doctor, nurse, dietician, and psychologist met emerging adults along with their parents to discuss a care plan. In the adult clinic, emerging adults met only a doctor during the visit and available resources were limited (Example: “I can't remember the last time I saw a nurse or dietician” (Kime, 2013, p.17)). The visit time in the adult clinic was short (≤5 minutes), and the doctor was not knowledgeable on emerging adults’ past glycemic control history and challenges (Kime, 2013; Lundin, et al., 2008). Within the first two years of adult care, 17% of patients have changed adult providers (Neu, et al., 2010).
Perceptions of Transitional Care
Emerging adults expressed mixed feelings on the transition from a pediatric care clinic to an adult care clinic. Perception of the overall transition preparation was significantly associated with overall satisfaction of the transition (p<0.0001) (Garvey, et al., 2012). Those who felt more prepared for transition were also less likely to report a gap in care (Garvey, et al., 2012). Over 40% of emerging adults do not perceive adult care to be profoundly different from pediatric care; however, some emerging adults reported the experiences in the adult clinic as “shocking” (Ritholz, et al., 2014), and 43.6% express that the treatment in the pediatric clinic was more satisfactory than adult care (Busse et al., 2007). The approaches that lessened the perception of differences in care culture were increased preparation of emerging adults to transition between the clinics (Hilliard, et al., 2014; van Staa, et al., 2011) and the existence of an age-specific transition clinic (e.g. a diabetes clinic for 16-25 year olds) rather than an adult clinic targeting the general adult population (Begley, 2013).
Perceived Differences of Pediatric and Adult Clinics
While emerging adults remembered the pediatric clinic and the relationships with the staff as warm, cozy, and trusted, the adult clinic was perceived as a sterile environment that treated them as a number. Emerging adults reported feeling invisible in the adult clinic (Hilliard, et al., 2014; Lundin, et al., 2008; van Staa, et al., 2011). However, some positive aspects of the adult clinic were also reported. The adult clinic treated emerging adults as autonomous and independent people with self-care responsibilities and fostered partnerships with the health care providers, whereas the pediatric clinic treated them as a child, was parent-centric, and judgmental of glycemic results (e.g., A1C) (Ritholz, et al., 2014). Thus, emerging adults who had a difficulty in achieving optimal glycemic control in the pediatric clinic were often pleased about the transition to adult care and viewed it as opportunity to become more autonomous (Ritholz, et al., 2014).
Health Care Provider's Perception of Successful Transitional Care
Health care providers proposed approaches for successful transitional care including: independently seeing adolescents without parents in a pediatric clinic, developing a transition protocol, using checklists, and making transition plans and organizing a joint consultation with health care providers in the adult and pediatric care clinics (van Staa, et al., 2011). Health care providers acknowledged that enhanced communications between pediatric care teams and adult care teams are essential to improving the quality of transitional care (van Staa, et al., 2011). Almost all doctors reported that they did not meet counterpart health care providers and their communication was by document only (van Staa, et al., 2011). Possible solutions for a tighter bond among the health care team are more staff exchanges, holding consultation meetings before and after the transition, and setting up joint clinics to make a seamless transition (Hilliard, et al., 2014; van Staa, et al., 2011).
Effects of Transitional Care on Diabetes Outcomes
Multiple factors of transitional care had an impact on overall diabetes health outcomes such as glycemic control. The time of transition had an effect on diabetes outcomes. Those who stayed in pediatric care longer (through their senior year of high school) demonstrated better self-care and have significantly lower A1C values than those who transitioned to adult care before or during their senior year of high school (Helgeson et al., 2013). How prepared the emerging adult felt for transition was not associated with improvements in A1C values one year after transition to an adult clinic (Garvey, et al., 2012); however, structured transition programs did show improvement in A1C one year after transition as compared to pre-transition A1C values (Holmes-Walker, Llewellyn, & Farrell, 2007; Vanelli et al., 2004).
Emerging adults who are using an infusion pump for diabetes care perceive greater control of their diabetes than those using multiple injections (p<0.001); however, episodes of hyperglycemia and hypoglycemia do not differ between these groups (Maiorino et al., 2014). The type of adult provider the emerging adult chose did have an effect on post-transition outcomes. Those who chose to see a general practitioner versus an endocrinologist had significantly higher A1C levels (p<0.001) (Busse, et al., 2007). Transition to adult care providers has an effect on diabetes-related hospitalizations. Within four years of transition, 10% of emerging adults are hospitalized for type 1 diabetes related complications (acute hypoglycemia or hyperglycemia). This is a significant increase in hospitalization post-transition as compared to pre-transition (p= 0.03) (Nakhla, Daneman, To, Paradis, & Guttmann, 2009).
Elements of Successful Transitional Care
Pediatric Care Providers’ Roles During Transition
Emerging adults who saw their pediatric provider fewer than three times in the year prior to transition were more likely to wait over six months to transition to an adult provider after discharge from the pediatric provider (Garvey, et al., 2013). Emerging adults identified important discussions to have with the pediatric provider during transition to adult care: objective approaches to managing diabetes in day to day life; subjective recollections of interactions with peers without diabetes regarding diabetes; emotions and stress related to insecurities; concerns about incidences of hypoglycemia and hyperglycemia; and learning how to ask questions of their physicians (Gerber, Solomon, Shaffer, Quinn, & Lipton, 2007; Markowitz & Laffel, 2012).
Early preparation for the emerging adults’ transfer between pediatric and adult clinics was identified as a key for successful transitional care. In this preparation, the role of the pediatrician is very important (Ritholz, et al., 2014). During the time in the pediatric care, emerging adults wanted pediatricians to treat and consult them appropriately with an acknowledgement of their shifting lifestyles and physical growth (Dovey-Pearce, et al., 2005; Ritholz, et al., 2014). When transferring to the adult clinic, emerging adults (as well as their parents) expected pediatricians to provide extensive guidance and consultation about adult care and clinics (Garvey, et al., 2014). Also, emerging adults wanted the pediatricians to be a bridge to find an adult doctor matched with their characteristics and to supervise the overall transition process (Ritholz, et al., 2014).
Parental Role During Transition
Parents often remain a ‘safety net’ or ‘safeguard’ for their children's diabetes self-care during the emerging adult period (Allen, et al., 2011; Hilliard, et al., 2014). Parents and emerging adults both acknowledged the need of preparation for transitional care for not only the emerging adults, but also the parents who played a major role for managing children's diabetes during childhood (Allen, et al., 2011; Hilliard, et al., 2014; van Staa, et al., 2011). There is an assumed transition to complete self-management of diabetes during the transfer to adult care, but this is not reflective of the continued role that parents play in diabetes care well into emerging adulthood. Service structures in adult care that recognize the continuing role of familial support in diabetes management are needed for successful transition (Allen, et al., 2011; Hilliard, et al., 2014; van Staa, et al., 2011).
Structured Transitional Care Programs
It is estimated that only half of diabetes care providers assist their patients through structured transition programs (de Beaufort, et al., 2010); however, structured transitional care reduces the gap between pediatric and adult care. In unstructured transitions, almost half of young adults in pediatric care do not successfully transition to adult care (Scott, Vallis, Charette, Murray, & Latta, 2005). With structured transition there is an average gap of 0.8 ± 0.6 years. Without using a structured transitional program the gap in care increases to 4.6 ± 1.2 years (Cadario et al., 2009).
Age-Specific Transitional Clinic
Emerging adults felt that a standard adult clinic targeting general adults was an unprepared, unwelcoming, and overwhelming place (Garvey, et al., 2014). Instead, they desired to have an age-specific clinic with a systematic and standard protocol (Dovey-Pearce, et al., 2005; Garvey, et al., 2014; Price et al., 2011). The benefits of this age-specific clinic would make young adults feel comfortable without stigma, have more navigable and available resources (e.g., age-specific specialist), and provide developmentally tailored care to meet emerging adults’ education needs (Dovey-Pearce, et al., 2005; Hilliard, et al., 2014; Price, et al., 2011). Some emerging adults expressed that the ideal time for a transition clinic would be from age 14-16 to age 18 (Begley, 2013), while other emerging adults would prefer two transition clinics that span adolescence and emerging adulthood, the first focusing on ages 16-21 and the second ages 22-25 (Dovey-Pearce, et al., 2005).
Emerging adults did not want to hear routine advice (e.g., lose weight); rather, they preferred to have one-on-one time with health care providers to obtain personally centered and age-specific information on topics such as alcohol and drug use and preventive diabetes care (such as foot care and eye examinations). Also, they wished to have an opportunity to explore additional health care resources such as dietetic and psychological services (Dovey-Pearce, et al., 2005; Garvey, et al., 2014; Price, et al., 2011). A transition clinic would allow for these provider interactions and for the exploration of available resources.
Individual Support
In person and technology-based programs to provide individual support to the emerging adult during health care transition were related to favorable outcomes. Professionally led face-to-face support groups with other emerging adults as part of the transition process decreased scores on the Problem Areas in Diabetes (PAID) survey (p=0.02) and increased self-care inventory scores (p=0.09) (Markowitz & Laffel, 2012). Emerging adults participating in technology-based programs felt that they had greater diabetes control (Gerber, et al., 2007), showed significant improvements in disease management and health-related self-efficacy (Huang, et al., 2014), and had lower rates of long term complications (pregnancy loss, heart failure, blindness, amputation, and death) (Van Walleghem, Macdonald, & Dean, 2008).
One transitional care program in Italy tried to ensure care continuity by introducing the adult care provider to the emerging adult before transition, having the pediatric care provider come to the first adult care appointment, and ensuring the same adult care provider worked with the emerging adult through the first year of transition. In this program, A1C one year post transition was lower than that at the time of pre-transition (Vanelli, et al., 2004).
College Transition
Emerging adults reported that years in college were an especially difficult period to manage their diabetes (Wilson, 2010). They often moved out of their parents’ home and lived independently (Hilliard, et al., 2014; Wilson, 2010); thus, making medical appointments, monitoring supplies, and refilling prescriptions became the responsibility of the emerging adult without parental support (Hilliard, et al., 2014). Social networks are changed, social events (e.g., alcohol consumption, missing injection opportunity) are increased, and new behaviors are adopted (e.g., engaging in sexual behavior) in this period (Garvey, et al., 2014; Wilson, 2010). Unfortunately, a new doctor affiliated with the adult clinic emphasizes “better” self-management behaviors but often does not understand emerging adults’ new challenges in college or their past glycemic control history. Thus, emerging adults felt unaided from the doctor's appointment at the adult clinic (Garvey, et al., 2014; Wilson, 2010).
Adult Care
Once a transition to adult care was completed, those emerging adults receiving care from an adult endocrinologist were more likely to report routine preventative care visits as compared to those receiving diabetes care from a general internist or adult primary care provider (Garvey, et al., 2013). The number of visits to the provider also differed based on the location of the adult care provider (urban, suburban, or rural). Routine preventative care visits were significantly higher in urban and suburban areas compared to rural areas (p<0.001) (Perry, Steinbeck, Dunbabin, & Lowe, 2010). For health care providers in adult clinics, the emerging adults wanted doctors to differentiate them from older adults (Garvey, et al., 2014). They desired one-on-one time with the health care providers to receive full consultations without any interruption (Dovey-Pearce, et al., 2005). Emerging adults did not want to be burdensome to providers, but expressed educational needs regarding independent care planning and management since previous care in the pediatric care clinic was mainly planned and managed by the parents (Allen, et al., 2011; Hilliard, et al., 2014). Emerging adults identified staff qualified for their care as those members of the care team who have consistent contact, civility, rapport, and good listening skills. Providers should also give options and provide honest feedback (positive and negative feedback). Finally, care providers need to be approachable, non-judgmental, and knowledgeable about developmental challenges (Dovey-Pearce, et al., 2005). Emerging adults who dropped out of adult care reported difficulty scheduling appointments, knowing who to see, and establishing relationships with the new team. They also expressed feeling overwhelmed and lost in the system and a lack of perceived value of adult care (Van Walleghem, et al., 2008).
Discussion
Looking at the synthesis of the results, the authors identified four overarching themes and practice implications that emerged from the review of the transitional care literature for emerging adults with diabetes (Table 3): differences between pediatric and adult care cultures; pediatric preparation for transition; structured transitional care programs; and suggestions for successful transition. There are many differences in care culture between pediatric and adult clinics including environment, communication, expectations of the patient, parental involvement, staffing, resource availability, and knowledge of the patient's history (Allen, et al., 2011; Hilliard, et al., 2014; Kime, 2013; Lundin, et al., 2008; Ritholz, et al., 2014; van Staa, et al., 2011). For many emerging adults these differences in care culture can create difficulties during transition between the pediatric and adult clinic settings.
Table 3.
Overarching Themes and Practice Implications
| Theme | Overall Findings | References | Practice Implications |
|---|---|---|---|
| Difference between pediatric and adult care | Differences in the care culture between pediatric and adult clinics: environment, communication, expectations of patient, parental involvement, staffing, resource availability, and knowledge of the patient's history. | Allen, Channon, Lowes, Atwell, & Lane, 2011; Hilliard et al., 2014; Kime, 2013; Lundin, Ohrn, & Danielson, 2008; Ritholz et al., 2014; van Staa, Jedeloo, van Meeteren, & Latour, 2011 | -Pediatric provider: prepare the patient for differences in care cultures -Adult provider: modify care to meet the needs of the emerging adult. |
| Pediatric Transition Preparation | Strong provider relationship is associated with: feeling more prepared for transition, higher transition satisfaction, and smaller gap in care | Dovey-Pearce, Hurrell, May, Walker, & Doherty, 2005; Gerber, Solomon, Shaffer, Quinn, & Lipton, 2007; Garvey et al., 2012; Garvey et al., 2013; Markowitz & Laffel, 2012; Neu et al., 2010, Ritholz et al., 2014 | -Pediatric provider: engage emerging adult during visits, provide personally centered information, and discuss transitional care. |
| Structured Transitional Care Programs | Structured transitional care programs are associated with: better glycemic control, smaller gaps in care, greater perceived diabetes control, improvements in health-related self-efficacy and self-care, and fewer long term complications | Cadario et al., 2009; Gerber, Solomon, Shaffer, Quinn, & Lipton, 2007; Holmes-Walker, Llewelyn, & Farrell, 2007; Huang et al., 2014; Markowitz & Laffel, 2012; Vanelli et al., 2004; Van Walleghem, MacDonald, & Dfan, 2008 | -Pediatric provider: provide patients with and assist patients through a structured transition program -Adult provider: know patient's history and transition program, and modify care to meet emerging adult's needs during transition |
| Health Care Transition Suggestions | Suggestions for successful transition include: enhanced communication between pediatric and adult care providers, age-specific clinics designed to aid in transition, and adult providers tailoring information for emerging adults’ concerns. | Allen, Channon, Lowes, Atwell, & Lane, 2011; Dovey-Pearce, Hurrell, May, Walker, & Doherty, 2005; Garvey et al., 2014; Hilliard et al., 2014; Price et al., 2011; van Staa, Jedeloo, van Meeteren, & Latour, 2011 | -Pediatric and adult care provider: communication before and after transition -Create transition clinics -Adult provider: provide information specific for emerging adults |
Pediatric providers should actively prepare the emerging adult for these differences, and adult providers may need to modify the care plan to meet the individual needs of the emerging adult. Emerging adults who have a strong relationship with their pediatric provider feel more prepared for transition, are more satisfied with their transition, and are less likely to report a gap in care. Strong relationships are those in which the emerging adult sees their provider on a regular basis, the emerging adult and provider engage in conversations about diabetes concerns, and the provider acknowledges changes in the emerging's adults lifestyle that may affect their diabetes management (Dovey-Pearce, et al., 2005; Garvey, et al., 2013; Garvey, et al., 2012; Gerber, et al., 2007; Markowitz & Laffel, 2012; Neu, et al., 2010; Ritholz, et al., 2014). The pediatric provider can increase the chance for a successful transition by engaging the emerging adult during visits, providing personally centered information, discussing transitional care, and implementing a structured transitional care program. Structured transitional care programs and individual support, such as support groups and technology-based programs, are related to better glycemic control, smaller gaps in care, greater perceived diabetes control, improvements in health-related self-efficacy and self-care, and fewer long term complications (Cadario, et al., 2009; Gerber, et al., 2007; Holmes-Walker, et al., 2007; Markowitz & Laffel, 2012; Van Walleghem, et al., 2008; Vanelli, et al., 2004).
Despite the benefits of structured care, it is estimated that only half of pediatric diabetes care providers assist their patients through structured transition programs (de Beaufort, et al., 2010), and without structured transitions almost one-half of emerging adults in pediatric care do not successfully transition to adult care (Scott, et al., 2005). Suggestions to increase successful transitions include enhanced communication between pediatric and adult care providers, age-specific clinics designed to aid in transition, and adult providers tailoring care for emerging adults’ concerns (Allen, et al., 2011; Dovey-Pearce, et al., 2005; Garvey, et al., 2013; Hilliard, et al., 2014; Price, et al., 2011; van Staa, et al., 2011). These suggested approaches may improve the success of health care transition for emerging adults with diabetes, but further study is needed to determine the effect of these practices.
Limitations of the current research include the gap of knowledge relating to transitional care needs of individuals with type 2 diabetes or prediabetes and the need for more intervention studies in all groups. Additionally there is a lack of attention to vulnerable subgroups that may have challenges such as access to care, poverty, and limited resources for optimal diabetes treatment. Data collected in the in transitional care studies is not consistent; thus, results of these studies are often difficult to compare. Using a consensus model to guide studies would improve the consistency of reported data and allow for more comprehensive conclusions.
Recent reviews and reports on transitional care emphasize the need for consistent transitional care goals in order to develop and evaluate interventions. (Prior, McManus, White, & Davidson, 2014) completed a systematic review based upon the Triple Aim framework developed by the Institute for Health Care Improvement (Berwick, Nolan, & Whittinghton, 2008). This framework is organized around three interdependent goals: improving the individual experience of health care, improving the health of populations, and reducing the per capital costs of care (Berwick, et al., 2008) (Prior, et al., 2014). Prior et al. evaluated transition interventions for youth with chronic conditions (n=33), 12 of which included patients with type 1 diabetes. Out of the 12 studies included in the Prior et al. review, four were included in our systematic review (Cadario, et al., 2009; Holmes-Walker, et al., 2007; Markowitz & Laffel, 2012; Van Walleghem, et al., 2008). The other eight studies did not meet our inclusion criteria, such as key words, publication date, or not being accessible via database searches used. In summary, Prior et al. concluded that transition programs are inconsistently evaluated using the Triple Aim framework and that a more unified approach including applicable measures is needed. The 2014 report on “Transition Care for Children with Special Health Needs” also concluded that transitional care lacks a consistent and accepted way of measuring transition success (Mcpheeters et al., 2014).
The current review illuminated that the majority of research in diabetes transitional care is descriptive in nature (Level C: n=24). In order to address the ongoing challenges and gaps in care delivery, future studies need to develop and evaluate interventional programs that thoroughly investigate transitional care from all perspectives including cost analysis. Well-designed studies will guide the formation of a consensus model for implementing transitional care into routine practice for emerging adults with diabetes or who are at risk for developing diabetes.
The current review also revealed that much of the research on transitional care for emerging adults with diabetes has been conducted outside of the United States (Table 2). While this international research is certainly still valid and applicable to the Unites States, it is interesting that there have been position statements developed by the American Academy of Pediatrics (Cooley & Sagerman, 2011) and the American Diabetes Association (Peters & Laffel, 2011) without further testing these interventions in United States clinic populations. Because research has not kept pace with the current position statements, additional study is needed to evaluate the aspects of care outlined in these position statements. According to the synthesis of available studies on transitional care, current protocols developed by proponents of these position statements are not yet being followed. A recent publication of the American Academy of Pediatrics, American Academy of Family Physicians, American College of Physicians (AAP/AAFP/ACP) Clinical Report on Transition from Adolescence to Adulthood (Cooley & Sagerman, 2011) focuses on the initiation of a planned transition process, beginning at ages 12-14 years, in hopes of making it a part of routine primary and specialty care. McManus and colleagues (2015) reported that published transition studies have not incorporated this 2011 Clinical Report recommended algorithm. McManus conducted an intervention with five large academic primary care practices in the District of Columbia to promote the use of a 2-year learning collaborative to improve transition services for youth with chronic conditions. Training consisted of five 1 ½ day sessions combined with coaching via phone calls and on-site visits for each team consisting of a physician, care coordinator (nurse, social worker, family navigator) and a consumer (parent/caregiver or young adult). Coaching was implemented using the Six Core Elements of Transition from the federally funded national resource center on transition (www.GotTransition.org), which defines a sequential process and aligns with the algorithm in the Clinical Report. As a result of this intervention, all sites developed a practice policy on transition and an organized process for tracking transition preparation. Approximately 73-88% of eligible youth (n = 400) and young adults (n = 128) were assessed for transition readiness with transition plans prepared for 29-33%. This research supports the use of an organized approach for transition from pediatric to adult health care and potential for improvement in outcomes for young adults with chronic conditions. Nurses are integral members of team-based care for adolescents and emerging adults with diabetes, possess the knowledge and skill regarding their developmental concerns, and can lead in program development and evaluation for structured approaches to transitional care delivery.
Transitional care program development must also address a major gap in the existing literature, the lack of research addressing the needs of the growing numbers of emerging adults with type 2 diabetes or prediabetes. This review included type 2 diabetes and prediabetes in its literature search (Figure 1) but found no studies pertaining to transitional care for these populations. This is particularly concerning given the 30.5% increase in prevalence for type 2 diabetes from 2001 to 2009 (Hamman, et al., 2014) and the projected 178% increase in youth with type 2 diabetes by 2050 (Imperatore et al., 2012). The American Diabetes Association (2015) has recommendations for screening youth for prediabetes and type 2 diabetes. These recommendations are for youth who are overweight and have two of the following risk factors: family history of type 2 diabetes in first or second-degree relatives; race/ethnicity of Native American, African American, Hispanic, Asian American or Pacific Islander; signs of insulin resistance (acanthosis nigricans, hypertension, dyslipidemia, polycystic ovarian syndrome, or small for gestation-age birth weight); or maternal history of diabetes or gestational diabetes during the child's gestation. This screening needs to continue beyond pediatric care and into emerging adulthood to prevent long term diabetes complications. Type 2 diabetes and prediabetes transitional care are likely to mirror type 1 diabetes transitional protocols in suggestions for diet, activity, and glucose control. Additionally after screening for comorbidities at diagnosis, the ADA position statement suggests that screening guidelines and treatment recommendations for hypertension, dyslipidemia, albumin excretion, and retinopathy in adolescents with type 2 diabetes are essentially the same as those with type 1 diabetes (American Diabetes Association, 2015). However, type 2 diabetes and prediabetes transitional care will most likely need to incorporate additional elements that will not be identified without research in this population. The Treatment Options for type 2 Diabetes in Adolescents and Youth (TODAY) study reported that youth with type 2 diabetes experience complications and comorbidities that are similar to those seen in adults (hypertension, high LDL-cholesterol, micoalbuminuria, and retinopathy) but on an accelerated timeline. This acceleration in complications suggests that cardiovascular disease, nephropathy, and retinopathy may be prevalent in this group during their 30's and 40's (Tryggestad & Willi, 2015). These life threatening complications and comorbidities make transitional care even more important for emerging adults with type 2 diabetes. Aggressive treatment needs to be continued from pediatric into adult care without the gap in care that is prevalent today.
In summary, this systematic review sought to examine the extent and quality of evidence for the process and outcomes of transitional care programs for adolescents and emerging adults with either type 1 diabetes, type 2 diabetes, or prediabetes with the intent to inform clinicians, researchers, and policy makers of key components of a model of high quality transitional care. This review revealed that the majority of current studies are descriptive in nature and many are conducted outside of the United States. There are no studies that address type 2 diabetes or prediabetes transitional care. Key components of transitional care practices that are associated with positive outcomes are structured transitional care programs, individual support (in person or technology based), and strong relationships with providers (physicians, nurses, dieticians). In order to develop a consensus model for implementing transitional care into routine practice quality research incorporating all perspectives must be conducted and evaluated systematically. This research is essential in creating a seamless system of care for emerging adults with diabetes, to enhance individual quality of life and help to prevent long term diabetes complications and comorbidities.
Highlights.
Available studies focus on adolescents or emerging adults with T1D.
Studies on the unique needs of adolescents and emerging adults with T2D and prediabetes are needed.
Structured transitional care programs are associated with better glycemic control.
Future research should incorporate recommendations of leading pediatric organizations.
Acknowledgements
The project was supported by Grant Number T32NR01275 from the National Institute of Nursing Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allen D, Channon S, Lowes L, Atwell C, Lane C. Behind the scenes: the changing roles of parents in the transition from child to adult diabetes service. Diabet Med. 2011;28:994–1000. doi: 10.1111/j.1464-5491.2011.03310.x. [DOI] [PubMed] [Google Scholar]
- Allen D, Cohen D, Hood K, Robling M, Atwell C, Lane C, Lowes L, Channon S, Gillespie D, Groves S, Harvey J, Gregory J. Continuity of care in the transition from child to adult diabetes services: a realistic evaluation study. J Health Serv Res Policy. 2012;17:140–148. doi: 10.1258/JHSRP.2011.011044. [DOI] [PubMed] [Google Scholar]
- American Diabetes Association Standards of medical care in diabetes--2014. Diabetes Care. 2014;37(Suppl 1):S14–80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- American Diabetes Association Classification and Diagnosis of Diabetes. Diabetes Care. 2015;38:S8–s16. doi: 10.2337/dc15-S005. [DOI] [PubMed] [Google Scholar]
- Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol. 2000;55:469–480. [PubMed] [Google Scholar]
- Aromataris E, Pearson A. The systematic review: an overview. Am J Nurs. 2014;114:53–58. doi: 10.1097/01.NAJ.0000444496.24228.2c. [DOI] [PubMed] [Google Scholar]
- Begley T. Transition to adult care for young people with long-term conditions. Br J Nurs. 2013;22506:508–511. doi: 10.12968/bjon.2013.22.9.506. [DOI] [PubMed] [Google Scholar]
- Berwick DM, Nolan TW, Whittinghton J. The triple aim: care, health and cost. Health Affairs (Millwood) 2008;27:759–769. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- Blonde L. Benefits and risks for intensive glycemic control in patients with diabetes mellitus. Am J Med Sci. 2012;343:17–20. doi: 10.1097/MAJ.0b013e31823ea23e. [DOI] [PubMed] [Google Scholar]
- Blum RW, Garell D, Hodgman CH, Jorissen TW, Okinow NA, Orr DP, Slap GB. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. J Adolesc Health. 1993;14:570–576. doi: 10.1016/1054-139x(93)90143-d. [DOI] [PubMed] [Google Scholar]
- Bryden KS, Peveler RC, Stein A, Neil A, Mayou RA, Dunger DB. Clinical and psychological course of diabetes from adolescence to young adulthood: a longitudinal cohort study. Diabetes Care. 2001;24:1536–1540. doi: 10.2337/diacare.24.9.1536. [DOI] [PubMed] [Google Scholar]
- Busse FP, Hiermann P, Galler A, Stumvoll M, Wiessner T, Kiess W, Kapellen TM. Evaluation of patients’ opinion and metabolic control after transfer of young adults with type 1 diabetes from a pediatric diabetes clinic to adult care. Horm Res. 2007;67:132–138. doi: 10.1159/000096583. [DOI] [PubMed] [Google Scholar]
- Cadario F, Prodam F, Bellone S, Trada M, Binotti M, Trada M, Allochis G, Baldelli R, Esposito S, Bona G, Aimaretti G. Transition process of patients with type 1 diabetes (T1DM) from paediatric to the adult health care service: a hospital-based approach. Clin Endocrinol (Oxf) 2009;71:346–350. doi: 10.1111/j.1365-2265.2008.03467.x. [DOI] [PubMed] [Google Scholar]
- Cali AM, Caprio S. Prediabetes and type 2 diabetes in youth: an emerging epidemic disease? Curr Opin Endocrinol Diabetes Obes. 2008;15:123–127. doi: 10.1097/MED.0b013e3282f57251. [DOI] [PubMed] [Google Scholar]
- Cooley WC, Sagerman PJ. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128:182–200. doi: 10.1542/peds.2011-0969. [DOI] [PubMed] [Google Scholar]
- Dabelea D, Mayer-Davis EJ, Saydah S, Imperatore G, Linder B, Divers J, Bell R, Badaru A, Talton JW, Crume T, Liese AD, Merchant AT, Lawrence JM, Reynolds K, Dolan L, Liu LL, Hamman RF. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. Jama. 2014;311:1778–1786. doi: 10.1001/jama.2014.3201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Beaufort C, Jarosz-Chobot P, Frank M, de Bart J, Deja G. Transition from pediatric to adult diabetes care: smooth or slippery? Pediatr Diabetes. 2010;11:24–27. doi: 10.1111/j.1399-5448.2009.00524.x. [DOI] [PubMed] [Google Scholar]
- Dovey-Pearce G, Doherty Y, May C. The influence of diabetes upon adolescent and young adult development: A qualitative study. British Journal of Health Psychology. 2007;12:75–91. doi: 10.1348/135910706X98317. [DOI] [PubMed] [Google Scholar]
- Dovey-Pearce G, Hurrell R, May C, Walker C, Doherty Y. Young adults’ (16-25 years) suggestions for providing developmentally appropriate diabetes services: a qualitative study. Health Soc Care Community. 2005;13:409–419. doi: 10.1111/j.1365-2524.2005.00577.x. [DOI] [PubMed] [Google Scholar]
- Garvey KC, Beste MG, Luff D, Atakov-Castillo A, Wolpert HA, Ritholz MD. Experiences of health care transition voiced by young adults with type 1 diabetes: a qualitative study. Adolesc Health Med Ther. 2014;5:191–198. doi: 10.2147/AHMT.S67943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garvey KC, Finkelstein JA, Laffel LM, Ochoa V, Wolfsdorf JI, Rhodes ET. Transition experiences and health care utilization among young adults with type 1 diabetes. Patient Preference and Adherence. 2013;7:761–769. doi: 10.2147/PPA.S45823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garvey KC, Wolpert HA, Rhodes ET, Laffel LM, Kleinman K, Beste MG, Wolfsdorf JI, Finkelstein JA. Health care transition in patients with type 1 diabetes: young adult experiences and relationship to glycemic control. Diabetes Care. 2012;35:1716–1722. doi: 10.2337/dc11-2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerber BS, Solomon MC, Shaffer TL, Quinn MT, Lipton RB. Evaluation of an Internet diabetes self-management training program for adolescents and young adults. Diabetes Technology & Therapeutics. 2007;9:60–67. doi: 10.1089/dia.2006.0058. [DOI] [PubMed] [Google Scholar]
- Hamman RF, Bell RA, Dabelea D, D'Agostino RB, Jr., Dolan L, Imperatore G, Lawrence JM, Linder B, Marcovina SM, Mayer-Davis EJ, Pihoker C, Rodriguez BL, Saydah S. The SEARCH for Diabetes in Youth study: rationale, findings, and future directions. Diabetes Care. 2014;37:3336–3344. doi: 10.2337/dc14-0574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanna KM. A framework for the youth with type 1 diabetes during the emerging adulthood transition. Nurs Outlook. 2012;60:401–410. doi: 10.1016/j.outlook.2011.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanna KM, Woodward J. The transition from pediatric to adult diabetes care services. Clin Nurse Spec. 2013;27:132–145. doi: 10.1097/NUR.0b013e31828c8372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson VS, Reynolds KA, Snyder PR, Palladino DK, Becker DJ, Siminerio L, Escobar O. Characterizing the transition from paediatric to adult care among emerging adults with Type 1 diabetes. Diabet Med. 2013;30:610–615. doi: 10.1111/dme.12067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilliard ME, Perlus JG, Clark LM, Haynie DL, Plotnick LP, Guttmann-Bauman I, Iannotti RJ. Perspectives From Before and After the Pediatric to Adult Care Transition: A Mixed-Methods Study in Type 1 Diabetes. Diabetes Care. 2014;37:346–354. doi: 10.2337/dc13-1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes-Walker DJ, Llewellyn AC, Farrell K. A transition care programme which improves diabetes control and reduces hospital admission rates in young adults with Type 1 diabetes aged 15-25 years. Diabet Med. 2007;24:764–769. doi: 10.1111/j.1464-5491.2007.02152.x. [DOI] [PubMed] [Google Scholar]
- Huang JS, Terrones L, Tompane T, Dillon L, Pian M, Gottschalk M, Norman GJ, Bartholomew LK. Preparing adolescents with chronic disease for transition to adult care: a technology program. Pediatrics. 2014;133:e1639–1646. doi: 10.1542/peds.2013-2830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imperatore G, Boyle JP, Thompson TJ, Case D, Dabelea D, Hamman RF, Lawrence J, Liese AD, Liu LL, Mayer-Davis EJ, Rodriguez BL, Standiford D. Projections of type 1 and type 2 diabetes burden in the U.S. population aged <20 years through 2050: Dynamic modeling of incidence, mortality, and population growth. Diabetes Care. 2012;35:2515–2520. doi: 10.2337/dc12-0669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Insabella G, Grey M, Knafl G, Tamborlane W. The transition to young adulthood in youth with type 1 diabetes on intensive treatment. Pediatr Diabetes. 2007;8:228–234. doi: 10.1111/j.1399-5448.2007.00266.x. [DOI] [PubMed] [Google Scholar]
- Kime N. Young people with type 1 diabetes and their transition to adult services. Br J Community Nurs. 2013;18:14, 16–18. doi: 10.12968/bjcn.2013.18.Sup12.S14. [DOI] [PubMed] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- Lotstein DS, Seid M, Klingensmith G, Case D, Lawrence JM, Pihoker C, Dabelea D, Mayer-Davis EJ, Gilliam LK, Corathers S, Imperatore G, Dolan L, Anderson A, Bell RA, Waitzfelder B. Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatrics. 2013;131:e1062–1070. doi: 10.1542/peds.2012-1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundin CS, Ohrn I, Danielson E. From multidimensional support to decreasing visibility: a field study on care culture in paediatric and adult diabetes outpatient clinics. Int J Nurs Stud. 2008;45:180–190. doi: 10.1016/j.ijnurstu.2006.07.022. [DOI] [PubMed] [Google Scholar]
- Maiorino MI, Bellastella G, Petrizzo M, Improta MR, Brancario C, Castaldo F, Olita L, Giugliano D, Esposito K. Treatment satisfaction and glycemic control in young Type 1 diabetic patients in transition from pediatric health care: CSII versus MDI. Endocrine. 2014;46:256–262. doi: 10.1007/s12020-013-0060-6. [DOI] [PubMed] [Google Scholar]
- Markowitz JT, Laffel LM. Transitions in care: support group for young adults with Type 1 diabetes. Diabet Med. 2012;29:522–525. doi: 10.1111/j.1464-5491.2011.03537.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May AL, Kuklina EV, Yoon PW. Prevalence of cardiovascular disease risk factors among US adolescents, 1999-2008. Pediatrics. 2012;129:1035–1041. doi: 10.1542/peds.2011-1082. [DOI] [PubMed] [Google Scholar]
- McManus M, White P, Barbour A, Downing B, Hawkins K, Quion N, Tuchman L, Cooley WC, McAllister JW. Pediatric to adult transition: A quality improvement model for primary care. Journal of Adolescent Health. 2015;56:73–78. doi: 10.1016/j.jadohealth.2014.08.006. [DOI] [PubMed] [Google Scholar]
- Mcpheeters M, Davis AM, Taylor JL, Brown RF, Potter SA, Espstein RA. Transition care for children with special health needs. Technical Breif No.15 (Prepared by the Vanderbilt University Evidence-based Practice Center under Contract No.290-2012-00009-I). AHRQ Publication No.14-EHC027. Agency for Healthcare Research and Quality; Rockville, MD: 2014. [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Nakhla M, Daneman D, To T, Paradis G, Guttmann A. Transition to adult care for youths with diabetes mellitus: findings from a Universal Health Care System. Pediatrics. 2009;124:e1134–1141. doi: 10.1542/peds.2009-0041. [DOI] [PubMed] [Google Scholar]
- Neu A, Losch-Binder M, Ehehalt S, Schweizer R, Hub R, Serra E. Follow-up of adolescents with diabetes after transition from paediatric to adult care: results of a 10-year prospective study. Exp Clin Endocrinol Diabetes. 2010;118:353–355. doi: 10.1055/s-0029-1246215. [DOI] [PubMed] [Google Scholar]
- Patterson CC, Dahlquist GG, Gyurus E, Green A, Soltesz G. Incidence trends for childhood type 1 diabetes in Europe during 1989-2003 and predicted new cases 2005-20: a multicentre prospective registration study. Lancet. 2009;373:2027–2033. doi: 10.1016/S0140-6736(09)60568-7. [DOI] [PubMed] [Google Scholar]
- Patterson CC, Gyurus E, Rosenbauer J, Cinek O, Neu A, Schober E, Parslow RC, Joner G, Svensson J, Castell C, Bingley PJ, Schoenle E, Jarosz-Chobot P, Urbonaite B, Rothe U, Krzisnik C, Ionescu-Tirgoviste C, Weets I, Kocova M, Stipancic G, Samardzic M, de Beaufort CE, Green A, Dahlquist GG, Soltesz G. Trends in childhood type 1 diabetes incidence in Europe during 1989-2008: evidence of non-uniformity over time in rates of increase. Diabetologia. 2012;55:2142–2147. doi: 10.1007/s00125-012-2571-8. [DOI] [PubMed] [Google Scholar]
- Perry L, Steinbeck KS, Dunbabin JS, Lowe JM. Lost in transition? Access to and uptake of adult health services and outcomes for young people with type 1 diabetes in regional New South Wales. Med J Aust. 2010;193:444–449. doi: 10.5694/j.1326-5377.2010.tb03997.x. [DOI] [PubMed] [Google Scholar]
- Peters A, Laffel L. Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems: a position statement of the American Diabetes Association, with representation by the American College of Osteopathic Family Physicians, the American Academy of Pediatrics, the American Association of Clinical Endocrinologists, the American Osteopathic Association, the Centers for Disease Control and Prevention, Children with Diabetes, The Endocrine Society, the International Society for Pediatric and Adolescent Diabetes, Juvenile Diabetes Research Foundation International, the National Diabetes Education Program, and the Pediatric Endocrine Society (formerly Lawson Wilkins Pediatric Endocrine Society). Diabetes Care. 2011;34:2477–2485. doi: 10.2337/dc11-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price CS, Corbett S, Lewis-Barned N, Morgan J, Oliver LE, Dovey-Pearce G. Implementing a transition pathway in diabetes: a qualitative study of the experiences and suggestions of young people with diabetes. Child Care Health Dev. 2011;37:852–860. doi: 10.1111/j.1365-2214.2011.01241.x. [DOI] [PubMed] [Google Scholar]
- Prior M, McManus M, White P, Davidson L. Measuring the “triple aim” in transition care: A systematic review. Pediatrics. 2014;134:e164801661. doi: 10.1542/peds.2014-1704. [DOI] [PubMed] [Google Scholar]
- Reinehr T, Wabitsch M, Kleber M, de Sousa G, Denzer C, Toschke AM. Parental diabetes, pubertal stage, and extreme obesity are the main risk factors for prediabetes in children and adolescents: a simple risk score to identify children at risk for prediabetes. Pediatr Diabetes. 2009;10:395–400. doi: 10.1111/j.1399-5448.2008.00492.x. [DOI] [PubMed] [Google Scholar]
- Ritholz MD, Wolpert H, Beste M, Atakov-Castillo A, Luff D, Garvey KC. Patient-Provider Relationships Across the Transition From Pediatric to Adult Diabetes Care A Qualitative Study. Diabetes Educator. 2014;40:40–47. doi: 10.1177/0145721713513177. [DOI] [PubMed] [Google Scholar]
- Scott L, Vallis TM, Charette M, Murray A, Latta R. Transition of care: researching the needs of young adults with type 1 diabetes. Canadian Journal of Diabetes. 2005;29:203–210. [Google Scholar]
- Sheehan AM, While AE, Coyne I. The experiences and impact of transition from child to adult healthcare services for young people with Type 1 diabetes: a systematic review. Diabet Med. 2015;32:440–458. doi: 10.1111/dme.12639. [DOI] [PubMed] [Google Scholar]
- Silverstein J, Klingensmith G, Copeland K, Plotnick L, Kaufman F, Laffel L, Deeb L, Grey M, Anderson B, Holzmeister LA, Clark N. Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association. Diabetes Care. 2005;28:186–212. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- The Joanna Briggs Institute . Joanna Briggs Institute Reviewers’ Manual: 2014 edition. 2014 ed. The Joanna Briggs Institute; Austrailia: 2014. [Google Scholar]
- Tryggestad JB, Willi SM. Complications and comorbidities of T2DM in adolescents: findings from the TODAY clinical trial. J Diabetes Complications. 2015;29:307–312. doi: 10.1016/j.jdiacomp.2014.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, Health Resources and Services Administration, & Maternal and Child Health Bureau . The National Survey of Children with Special Health Care Needs Chartbook 2005-2006. US Department of Health and Human Services; Rockville, MD: 2008. [Google Scholar]
- van Staa AL, Jedeloo S, van Meeteren J, Latour JM. Crossing the transition chasm: experiences and recommendations for improving transitional care of young adults, parents and providers. Child Care Health Dev. 2011;37:821–832. doi: 10.1111/j.1365-2214.2011.01261.x. [DOI] [PubMed] [Google Scholar]
- Van Walleghem N, Macdonald CA, Dean HJ. Evaluation of a systems navigator model for transition from pediatric to adult care for young adults with type 1 diabetes. Diabetes Care. 2008;31:1529–1530. doi: 10.2337/dc07-2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Walleghem N, MacDonald CA, Dean HJ. Transition of care for young adults with type 1 and 2 diabetes. Pediatr Ann. 2012;41:e16–20. doi: 10.3928/00904481-20120426-20. [DOI] [PubMed] [Google Scholar]
- Vanelli M, Caronna S, Adinolfi B, Chiari G, Gugliotta M, Arsenio L. Effectiveness of an uninterrupted procedure to transfer adolescents with Type 1 diabetes from the Paediatric to the Adult Clinic held in the same hospital: eight-year experience with the Parma protocol. Diabetes Nutr Metab. 2004;17:304–308. [PubMed] [Google Scholar]
- Vehik K, Dabelea D. The changing epidemiology of type 1 diabetes: why is it going through the roof? Diabetes Metab Res Rev. 2011;27:3–13. doi: 10.1002/dmrr.1141. [DOI] [PubMed] [Google Scholar]
- Wilson V. Students’ experiences of managing type 1 diabetes... includes discussion. Paediatric Nursing. 2010;22:25–28. doi: 10.7748/paed2010.12.22.10.25.c8134. [DOI] [PubMed] [Google Scholar]
- Winocour PH. Care of adolescents and young adults with diabetes - much more than transitional care: a personal view. Clin Med. 2014;14:274–278. doi: 10.7861/clinmedicine.14-3-274. [DOI] [PMC free article] [PubMed] [Google Scholar]