Abstract
A 31-year-old woman was referred to chest clinic with an 18-month history of cough, breathlessness and weight loss. She had previously been treated unsuccessfully with bronchodilators. In clinic she was found to have vocal hoarseness and harsh, monophonic inspiratory breath sounds. A bronchoscopy was arranged, but the patient was found dead before it could be performed. A postmortem examination with histology found evidence of active and chronic inflammation as well as destruction of cartilage, in keeping with a diagnosis of relapsing tracheobronchial polychonditis.
Background
The article describes a case of undiagnosed fatal relapsing polychrondritis identified at autopsy, which we believe to be an exceptional presentation without identifiable cases in the literature. We describe and illustrate the patient's antemortem medical history, her postmortem findings and microscopy. Finally, we discuss relapsing polychronditis and highlight why a prompt diagnosis is essential in patients with respiratory tract involvement.
Case presentation
The authors describe an exceptional case of a 31-year-old woman referred to chest clinic with an ill-defined 18-month history of cough, breathlessness and weight loss. She had been diagnosed with bronchial asthma although combination bronchodilators had failed to satisfactorily alleviate her symptoms. There was no significant medical history save mild childhood epilepsy. At chest clinic, enquiry detailed vocal hoarseness, sacroiliac joint pain and a three-stone weight loss over the preceding 2 years. Chest examination recorded harsh, monophonic, inspiratory breath sounds in keeping with stridor. A chest radiograph was normal. There is no record of lung function testing. Bronchoscopy was arranged for the following week, but the patient was found dead at home prior to this investigation. A Coroner’s postmortem was undertaken.
Investigations
At postmortem examination, the trachea and bronchi were flaccid. The mucosal surface appeared inflamed and the cartilaginous rings were inconspicuous (figure 1). No stenotic or mass lesions were identified. The parenchyma of both lungs appeared unremarkable. There was mild paratracheal lymphadenopathy and the spleen was mildly enlarged (275 g), but all other organs appeared normal.
Figure 1.

Postmortem photo shows the distal trachea and carina. The mucosa is inflamed and the cartilaginous rings cannot be seen.
Histological examination of tissue sections from the larynx, trachea and bronchi showed active inflammation and destruction of cartilage, by a mixed inflammatory cell infiltrate comprising lymphocytes, plasma cells, neutrophils and eosinophils. Residual islands of cartilage had an irregular contour and showed infiltration by granulation tissue (figure 2). Dystrophic calcification of cartilage was also noted. The overlying mucosa showed intense chronic inflammation and vascular congestion. There was no vasculitis and granulomata were not seen. Sections of lung showed focal, peribronchial chronic inflammation with chondritis involving larger intrapulmonary airways. The background lung parenchyma showed no abnormality. Tissue from the nasal septum showed chronic inflammation in the mucosa and replacement of cartilage by fibrous tissue with mild chronic inflammation, possibly indicating a ‘burnt-out’ stage of the same process. The paratracheal lymph nodes showed only non-specific reactive changes and the spleen was histologically normal. A sample of synovium from the right knee showed mild, non-specific, chronic synovitis. Samples of auricular cartilage and intervertebral disc showed no abnormality. Histology from all other organs was unremarkable.
Figure 2.
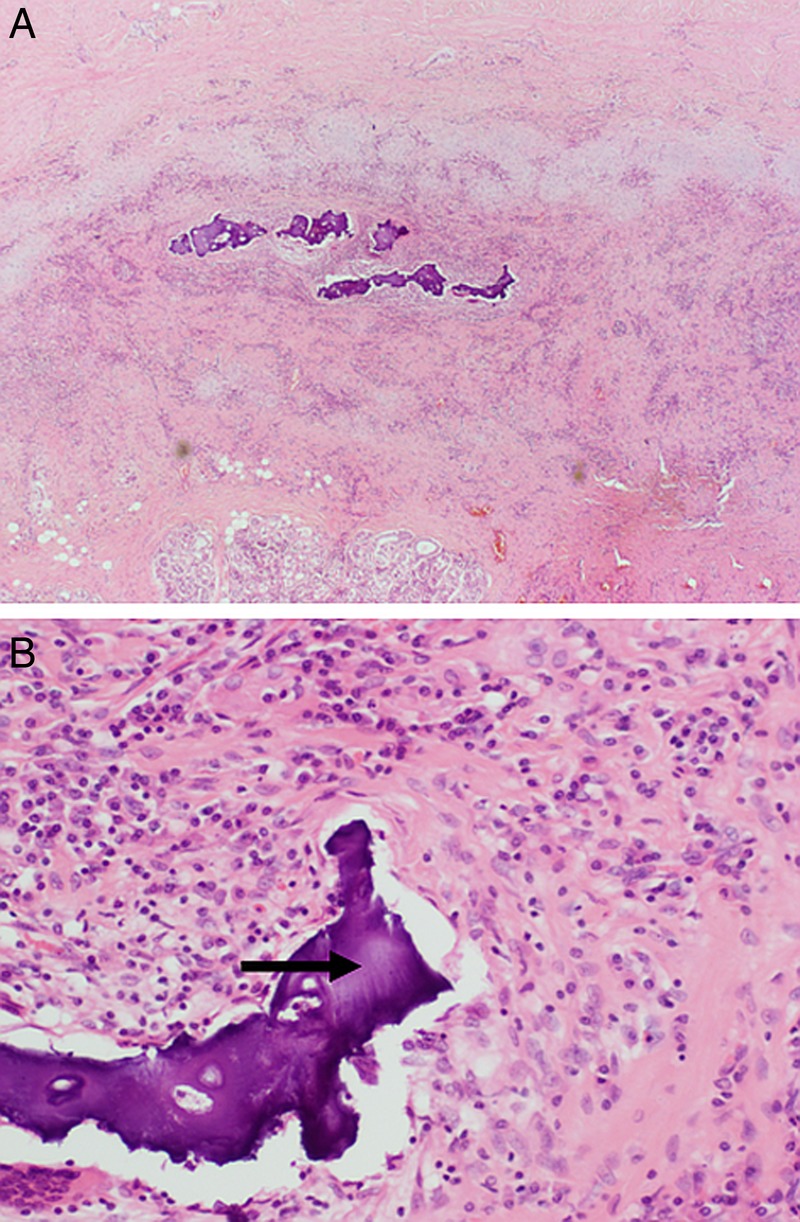
(A) Mid-trachea showing destruction of the cartilage which has been replaced by granulation tissue (magnification ×20). (B) The stroma is rich in inflammatory cells with destroyed cartilage (arrow) (magnification ×200).
The postmortem diagnosis was that of tracheobronchomalacia due to relapsing polychondritis, with predominant involvement of the upper respiratory tract.
Discussion
Relapsing polychondritis is a rare inflammatory disorder of autoimmune pathogenesis, which is typically characterised by recurrent bouts of inflammation and destruction of cartilage, in particular of the ear pinna, nose, joints and respiratory tract. In addition, it may affect other proteoglycan-rich tissues, such as the eyes, heart, blood vessels, inner ear and kidney.1 2 Relapsing polychondritis typically presents with painful inflammation of the ears or nose. However, involvement of the respiratory tract is seen in 25% of patients at initial presentation and occurs in almost 50% of patients during the course of the disease.2 Our patient's presentation was atypical in that she was relatively young and presented with respiratory tract involvement; although in retrospect, her sacroiliac pain may also have been a manifestation of relapsing polychondritis. To the best of our knowledge, this is the first reported case of relapsing polychondritis to be diagnosed at autopsy.
It is important that clinicians and histopathologists are aware that relapsing polychondritis can affect the respiratory tract and that this may be the presenting and predominant site of involvement. Airway involvement by relapsing polychondritis is a potentially life-threatening condition. This case highlights the importance of accurately distinguishing between wheeze (lower airway obstruction) which indicates asthma, and stridor, caused by upper airway obstruction. Such a clinical misinterpretation resulted in the start of an unnecessary and unsuccessful course of bronchodilators. Endoscopic biopsies of the respiratory tract are potentially hazardous as they may lead to acute respiratory obstruction in patients with stenotic or collapsing airways.2 In addition, they are frequently too superficial to permit adequate assessment of the cartilage. However, the possibility of relapsing polychondritis should at least be considered when there is marked tracheal or bronchial wall inflammation in an appropriate clinical context.
Relapsing polychondritis should also be considered at autopsy in patients with a history of an asthma-like illness, particularly when there are atypical clinical features such as hoarseness, failure to respond to therapy or clinical or laboratory evidence of inflammatory disease.
Learning points.
Relapsing polychondritis is a rare, but potentially fatal disease, if there is involvement of the respiratory tract.
Diagnosis may be difficult, especially if the patient's symptoms are non-specific but failure to respond to initial treatment should prompt the clinician to consider the diagnosis.
Early and aggressive treatment, with placement of a tracheal stent for respiratory involvement, is required. However, the bronchoscopy itself can be potentially hazardous.
Footnotes
Contributors: SW and AB are the co-authors of the manuscript. RA oversaw the manuscript and advised on content and editing.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Letko E, Zafirakis P, Baltatzis S et al. . Relapsing polychonditis: a clinical review. Semin Arthritis Rheum 2002;31:384–95. doi:10.1053/sarh.2002.32586 [DOI] [PubMed] [Google Scholar]
- 2.Molina JF, Eapinoza LR. Relapsing polychonditis. Baillieres Best Pract Res Clin Rheumatol 2000;14:97–109. doi:10.1053/berh.1999.0079 [DOI] [PubMed] [Google Scholar]


