Abstract
Context
This study examines the spillover effects of growth in state-level incarceration rates on the functioning and quality of the US health care system.
Methods
Our multilevel approach first explored cross-sectional individual-level data on health care behavior merged to aggregate state-level data regarding incarceration. We then conducted an entirely aggregate-level analysis to address between-state heterogeneity and trends over time in health care access and utilization.
Findings
We found that individuals residing in states with a larger number of former prison inmates have diminished access to care, less access to specialists, less trust in physicians, and less satisfaction with the care they receive. These spillover effects are deep in that they affect even those least likely to be personally affected by incarceration, including the insured, those over 50, women, non-Hispanic whites, and those with incomes far exceeding the federal poverty threshold. These patterns likely reflect the burden of uncompensated care among former inmates, who have both a greater than average need for care and higher than average levels of uninsurance. State-level analyses solidify these claims. Increases in the number of former inmates are associated simultaneously with increases in the percentage of uninsured within a state and increases in emergency room use per capita, both net of controls for between-state heterogeneity.
Conclusions
Our analyses establish an intersection between systems of care and corrections, linked by inadequate financial and administrative mechanisms for delivering services to former inmates.
Keywords: spillover, incarceration, health care
Policy Points:
The steady increase in incarceration is related to the quality and functioning of the health care system. US states that incarcerate a larger number of people show declines in overall access to and quality of care, rooted in high levels of uninsurance and relatively poor health of former inmates.
Providing health care to former inmates would ease the difficulties of inmates and their families. It might also prevent broader adverse spillovers to the health care system.
The health care system and the criminal justice system are related in real but underappreciated ways.
By now the consequences of incarceration are well established for former inmates,1,2 their families,3–5 and groups such as African American males.6 This research rightly emphasizes the extreme concentration of incarceration among an already segregated, disadvantaged, and underserved population. Incarceration is, indeed, more common among African American males with low levels of education, and they suffer most of the damage of incarceration.6,7 Furthermore, former inmates return to a relatively small number of communities, meaning that most of the collateral consequences of incarceration remain localized, even when severe.8–10 But no matter how accurate the focus on concentration, segregation, and the persistence of disadvantage may be, it implicitly casts incarceration as a problem only for the relatively small circle of people immediately surrounding prisoners. Even the strongest moral case against mass incarceration relies on observations of this sort, as when some argue that incarceration is iatrogenic in increasing crime in neighborhoods where crime already is common.8
In contrast, in this article we ask how incarceration affects the health care system as a whole: not the health of individual inmates or their families, but the broader functioning of the health care system available to everyone. By following in a line of research addressing ties between the prison system and other social systems, we assess the broader social costs of incarceration. Other researchers have shown far-reaching effects of incarceration on labor market and political institutions. For example, Western and Beckett11 showed that high rates of criminal punishment can reduce the unemployment rate in the short term while raising it in the long term, thereby characterizing the prison system as a labor market institution. Similarly, Uggen and Manza12 showed how rising rates of punishment and felon voting restrictions have affected elections, tilting the partisan balance in the US Senate by diluting the voting strength of already underrepresented groups.
Like labor markets and politics, the health care system is a foundational institutional setting, with great complexity, generally wide geographic service areas, and critical importance to the functioning of society. The health care system also, of course, provides a sharp contrast to the prison system: the mandate and jurisdiction of the 2 systems are very different, and few would consider the two as residing in the same sector or sharing the same concerns.4 Yet consideration of the health care system is essential to evaluating the total social costs of incarceration13 and, on the flip side, to recognizing the social currents that affect medicine. Like other consequences of incarceration, the spillover effects on health care that we document in this article are hidden from mainstream society—perhaps even more so because they are beyond the purview of any one institution—but they are nonetheless quite powerful. Although former inmates and their families certainly suffer the most with respect to health care, their situation also affects the care of those far removed from them.
Background
Spillover effects occur when the behavior of some members of a community affect the situation of others. By bridging individuals and institutions, a spillover effect is similar to a neighborhood effect, in which residence in a defined geography affects the individuals there through collective processes, such as peer-group influence or socialization.14 In setting the stage for a health care spillover, we thus must consider both the social context of incarceration and the relationship between the behavior of individual health care consumers and the functioning of the organizations that serve them. Several processes are relevant, including the effects of incarceration on health, health care in prison settings, and the availability of health services outside prison. Financial mechanisms are also important to understanding potential spillovers, including the relationships of incarceration, insurance, and uncompensated care. But a more immediate question is whether the population of former inmates is sufficiently large to produce spillovers of this sort. Accordingly, we will review trends in incarceration before turning to the relationship between incarceration and health care consumption.
The Rise of Incarceration
The incarceration rate has risen precipitously since the mid-1970s.13 In 2012, more than 2.4 million prisoners and parolees were under supervision, 8 times more than in 1968.15–18 Although the “stock” of current prisoners is perhaps the most common way to think of incarceration, the “flow” of inmates in and out of prisons also is relevant. Because the vast majority of inmates are eventually returned to the community, any consideration of long-term spillover effects must also consider the number of former inmates, which also has risen precipitously over time. In 2004, more than 4 million people had previously been in prison or were on parole but were no longer under correctional supervision, representing 1.9% of the adult population and 3.5% of the adult male population.15 This, too, represents a remarkable shift over earlier levels. Until the mid-1970s, the number of ex-prisoners remained stable at approximately 1 million, but since 1978 the number has approximately quadrupled. Recent years have seen some fluctuation in the prison population, but the absolute level remains high and the difference is small. In 2013, for example, 623,337 prisoners were released from state and federal prisons, and 631,168 individuals were admitted to them.19
The overall level of incarceration is striking, but there is considerable variation between states and between demographic groups. Some of the largest states also have the highest incarceration rates, like Texas and California, both of which house more than 160,000 prisoners.20 Similarly, Florida has just under 100,000 people in prison and also one of the faster-growing incarceration rates. Despite the nationwide increase in incarceration, some states have remained relatively stable over time, thereby producing a substantial between-state variation. In 2013 the highest incarceration rate was in Louisiana, with a rate of 870 per 100,000 and the lowest rate was in Maine, with 145 per 100,000.19 These between-state differences reflect many factors, quite apart from state differences in crime rates. The size of the prison population is driven by each state’s sentencing policies, administrative procedures, and, to some degree, political preferences for incarceration over other forms of punishment.20
Incarceration is also highly concentrated among already disadvantaged groups. African American males are much more likely to be incarcerated than their non-Hispanic white counterparts. In 2004, 2.9% of the adult population was currently or had previously been in prison or was on parole, but among African Americans this figure was 10.2%.15 For African American men, this figure climbs to 17.1%. By one estimate, about 32% of African American men born in 2001 will go to prison in their lifetimes, compared with about 6% of white men.16 Comparing incarceration with other events of the life course further illustrates its impact. African American men born between 1965 and 1969, for example, are more likely to have a prison record than a bachelor’s degree (22% versus 13%).7
The Social and Institutional Bases for Spillover Effects
Although the number of current and former prisoners has risen precipitously, these groups combined still represent only about 3% of the adult population.15 Yet a population of this size is sufficient to shape unemployment figures, which are usually below 10% and for which small differences are politically and economically meaningful. Conceivably, even a relatively small number of former inmates can affect the economics of health care if former inmates are sicker than other members of the community, if they have especially costly illness configurations, or if they continue to use health services even when their ability to pay for those services is compromised.
The potential spillover effects of incarceration on health care are premised not only on the size of prison populations. They also rest on the particular health care needs of former inmates, on how they consume care, and on who does or does not pay for the services they receive. In all 3 ways, former inmates are unique, and it is the confluence of these factors that sets the stage for spillovers. In sufficient numbers, former inmates may increase the burden of uncompensated care, diminish the financial stability of local providers, force providers to cut services or close altogether, and thereby reduce the quality or availability of services to others. These incarceration effects are magnified by how the insurance system intersects with prison demographics. More than 90% of US prison inmates are male, and about half of them have children.21,22 Because health insurance is provided largely through employers and because many families obtain insurance through the policy of a single employed subscriber, the incarceration of a large number of working-age fathers (and, increasingly, mothers) ripples outward to affect the availability of health insurance to families.
Perhaps the strongest evidence for spillover effects on health care concerns community uninsurance rates, for which there are both a strong conceptual foundation23 and compelling empirical evidence.24,25 In the case of community uninsurance, spillover effects begin with the behavior of uninsured individuals and propagate outward to other consumers, largely through financial mechanisms. Uninsurance is a major barrier to health care. It reduces the likelihood of visiting a physician and the likelihood of providers being compensated for the services they render.26,27 Yet uninsurance does not prevent the consumption of care altogether, and it is not, on average, a reflection of less need. Those without health insurance generally report worse health than do those with insurance; they continue to visit physicians and hospitals; and by law, patients cannot be turned away for emergency care on the basis of their ability to pay.28 If the uninsured population is sufficiently large and providers are unable to absorb the cost of uncompensated care, hospitals and other providers may reduce the availability and/or quality of services they offer, thereby reducing the services available to others. Spillover effects of this sort have been documented in several ways, such as by linking a community’s uninsurance rate to the likelihood of insured individuals reporting an unmet need for care (a multilevel approach)24 and by linking the size of the uninsured population in a region to services available in hospitals within that region (an aggregate-level approach).23
The case for incarceration-based spillover effects reflects many of the same influences. For instance, both types of spillovers are ultimately rooted in the financial dimensions of care. But incarceration’s spillovers are likely magnified beyond uninsurance because incarceration might simultaneously affect access to care, the need for care, and the demand for care. While in prison, inmates are provided with health care services, and on average, they consume more services than they did before being admitted.29,30 For many inmates, prison represents an improvement in overall access to care, especially for those who are ordinarily underserved.31 Overall mortality among African Americans, for example, is lower in prison than outside,31 although to be sure, much of this decline stems from deaths related to accidents, homicide, and drugs and alcohol rather than causes of death amenable to care.32 Even so, incarceration might increase the demand for health care through at least 3 key mechanisms: (1) if it has a negative effect on health after release and thereby increases the real demand for care33,34; (2) if, through testing, it reveals illnesses that had been previously unknown to inmates35–38; and (3) if prisoners are encouraged to seek treatment as part of their reintegration efforts or are required to seek treatment for specific health issues, such as substance abuse.39–41
It is unlikely that all these influences affect inmates simultaneously in all instances. For example, HIV testing varies among prisons, even among prisons in the same system.37 Furthermore, in some instances the demand for treatment outside prison might be quite small, even among former inmates who plainly require treatment. Along these lines, one study found that most HIV-infected inmates who received antiretroviral therapy (ART) medications in prison failed to fill their prescriptions after release, even when those prescriptions were free or low cost.42 Indeed, a robust literature has documented the many ways that even the best discharge planning fails to prevent lapses in treatment. Yet the potential for spillovers rests on the net effect, and in this regard, some aspects of incarceration are clear. It is well established, for example, that the health care needs of former inmates are, in fact, high. Furthermore, their need for care might increase after release if prisons maintain active testing regimens. It is also evident that the level of access provided in prison for most illnesses is unlikely to be maintained after release. To understand spillovers, we need to know whether the barriers to access are large enough to prevent former inmates from seeking services altogether. This seems unlikely, but it is important to understand the precise nature of the bridge between health care inside prison and health care outside prison.
Former inmates’ access to health care is limited in part by their not having insurance. They often are unemployed, and of those who do find work, few are able to secure positions with good benefits.43 Although federal and state programs are available to help provide health care to those who cannot afford it, such safety-net services are limited and may be especially so for former inmates.44 Far more states terminate rather than suspend Medicaid benefits when inmates begin their sentence, leaving a gap in care after release until the former inmates reenroll.45–47 Although most states, at a minimum, support Medicaid enrollment after release, not all states do. One study reported that about one-third of the state prison systems that terminate or suspend Medicaid do not provide assistance in resuming benefits.47
Despite these barriers, however, former inmates do consume health care. Former inmates with health conditions tend to be heavy consumers of health services, and they often utilize health care in cost-intensive ways.30 For example, many use emergency rooms for care,30,48,49 sometimes more frequently than using regular providers.50 These utilization patterns reflect the limited services available to former inmates, as well as their unique needs, which are difficult to treat even under ideal conditions. For instance, former inmates often have comorbid psychiatric disorders, complicating the treatment of other illnesses.51 Furthermore, many suffer from chronic illnesses that in themselves are associated with expensive treatments, including HIV and hepatitis B and C.30 Even if HIV-infected former inmates fail to fill ART prescriptions, they might return to the hospital when their condition worsens and their treatment becomes more expensive. Even a small number of complex cases can affect a hospital’s delivery of services. In the case of emergency room visits, for instance, frequent users represent only 4.5% to 8% of patients but make up 21% to 28% of visits.52 Heavy emergency room users are demographically similar to the former inmate population, suggesting important overlaps in these populations.52
Figure 1 summarizes our conceptual model of spillovers between incarceration and health care. Incarceration decreases access to health care following release and possibly increases the demand for services. In turn, former inmates’ utilization of services increases the amount of uncompensated care in the community. When providers respond to this uncompensated care by reducing services and/or diminishing the quality of their offerings, spillover effects are the result.
Figure 1.
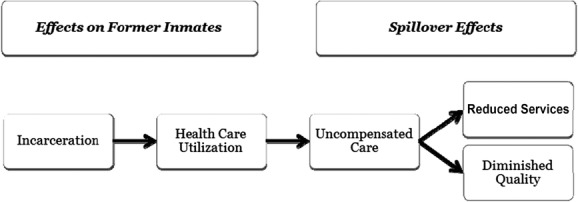
Conceptual Model Linking Incarceration to Health Care Spillover Effects
Although the potential for spillovers is strong, it is not a logical necessity flowing inescapably from the situation of former inmates to the market for health services. Spillovers of this sort depend on how the local market for health care is organized and how it responds. In both respects, incarceration effects could be blunted. Furthermore, the institutional effects of incarceration on health care begin to diverge even more from incarceration’s other institutional effects and therefore deserve emphasis.
Residential Segregation and Market Segmentation
The irony of health care that is not apparent in other institutional effects of incarceration is that the residential segregation of former inmates might limit, rather than facilitate, the potential for spillover effects in health care insofar as segregation leads to market segmentation. In particular, if those hospitals providing care to former inmates are generally distinct from those providing care to others, there may be no need for the latter to reduce services because their revenues would not be affected by the former inmates’ situation. In this case, well-resourced consumers can avoid hospitals servicing uninsured individuals, resulting in a segmented market but no average decline in services across the entire market. Although we have no direct evidence for this, we do have related evidence regarding race, segregation, and hospitals. Hospital care for African Americans is concentrated in a relatively small number of hospitals,53 and hospital segregation is strongly correlated with residential segregation.54,55 Furthermore, the burden of uncompensated care has become more concentrated over time, suggesting that insured persons seek services in more financially secure private hospitals and the uninsured go elsewhere.56 In short, the factors that make prisons so powerful in perpetuating economic disadvantage may be the same forces that blunt spillovers in health care.
Likewise, spillover effects might be blunted if the needs of former inmates differ significantly from those of other consumers. If former inmates are more likely to use specific services, providers might cut those services, thereby minimizing their exposure to former inmates and preventing cuts to other services. Whether the mix of services used by former inmates differs substantially from that of other consumers is unclear. Although former inmates suffer from some diseases at especially high rates, especially addiction and psychiatric disorders, their utilization patterns likely reflect the wide range of conditions from which they are more likely to suffer.34 Yet the possibility of different utilization patterns means that any empirical exploration of spillover effects requires the simultaneous examination of multiple dimensions of health care consumption.
The Empirical Dimensions of Spillover Effects
Testing for spillovers requires 2 elements. First, it requires multilevel data containing aggregate information on the size of the former inmate population matched to individual-level data. Spillover effects are best demonstrated by matching information on individuals’ actual utilization with information on aggregate-level characteristics. This allows analysts to adjust for other characteristics of the individual that drive health care consumption. Yet aggregate-level data alone can be deployed to address between-state heterogeneity, which is also a concern, since the state is the level at which correctional and many public health policies are administered.
For this study, we used a 2-fold design. In Part 1, we focused on individual-level data, showing how individuals actually behave in regions with a large number of former inmates, controlling extensively for individual-level factors. In Part 2, we explored whether traces of these individual-level patterns were detectable in the key aggregate data, controlling extensively for aggregate-level characteristics. In particular, we tested how changes in the former inmate population affected changes in the health care system, thereby holding constant all fixed state-level characteristics. In this way, the first part allowed us to examine between-individual heterogeneity, and the second part allowed us to examine between-state heterogeneity.
Second, testing for spillovers requires granular information on utilization patterns. Although previous research demonstrated the spillover effects of community uninsurance using basic reports of unmet need,24 additional measures allow for more fine-grained conclusions. Depending on the amount of revenue strain and the characteristics of the market, hospitals might be selective in the services they cut. For example, routine primary care visits are less sensitive to scale, as most markets can accommodate more than 1 provider. In this situation, hospitals might cut back instead on emergency room services, which have an important community benefit but are less profitable.57,58 Similarly, certain specialty services require a large consumer base and therefore might be especially vulnerable to financial considerations. Mammography screening is a good example, as it is capital intensive. As a result, the number of screening facilities has been declining over time,59 and the average wait for first-time mammograms has increased.60 Although some regions maintain excess capacity, the percentage of women living in poor-capacity areas has risen.61 Distinctions across service units are important to our study because they allow us to test the limits of spillover effects: if the size of the former inmate population is not sufficiently large, providers might cut back on specialty care but retain primary care.
Process-related information provides additional leverage. The case has been made that community uninsurance diminishes the willingness of individuals to claim health as a right.23 Similar arguments have been raised with respect to incarceration and neighborhood cohesion, with some people arguing—if not empirically demonstrating—that mass incarceration undermines social bonds.8,9 The testable corollary with respect to health care is that large-scale incarceration might undermine trust in physicians by introducing doubt about whether the physician has the patient’s best interests in mind or is, instead, considering revenue.
The outcomes we used have other helpful features. For instance, to the extent that we can demonstrate a relationship between incarceration and services intended for older women, such as mammography, the evidence for spillovers is stronger, as incarceration disproportionately affects young men. No single outcome can provide a perfect test, and each is subject to multiple simultaneous influences. Moreover, unmet need is plainly determined by many factors apart from those emphasized in our framework, including the ability of individuals to schedule convenient appointments. Nevertheless, examining a rich set of outcomes and predictors enabled us to draw reasonable and appropriately cautious inferences about the existence and extent of spillovers.
Data, Methods, and Results
As noted, our analysis was based on 2 levels of data. At the individual level, we used a large, nationally representative survey of individuals. At the state level, we constructed estimates of the number of former inmates by state and year, to which we appended other state-level measures. In the first part of our analysis, we merged these 2 data sources into a multilevel model. In the second part, we used only aggregate-level data in a time-series cross-sectional approach. After describing the data common to both, we will discuss each of these parts.
Estimates of the Number of Former Inmates by State and Year
Both parts of our analysis include estimates of mass incarceration at the state level. In this regard, our framework required specific and unusual data. It is easy to find state-level incarceration rates, which serve as the foundation for evidence regarding mass incarceration. To understand spillovers, however, it is better to measure the number of former inmates rather than the number of current inmates. These 2 numbers are correlated, of course, but only the former inmates contribute to the specific spillovers we described. We estimated the number of former inmates within a state based on demographic life tables applied to each state for each year as described previously.15 Each annual cohort of prison releases was reduced for recidivism and mortality, and subsequent cohorts refreshed the population. Our recidivism rate is duration specific and is based on national studies. We assumed most former inmates will be reincarcerated, but we also assumed the recidivism rate will fall with time since release. We also assumed a higher rate of mortality among former inmates than among those who did not serve prison time. Both of these assumptions are consequential to our estimates, although in a conservative direction. They reduce the risk of overestimating the number of ex-prisoners in state populations, but as we show, the estimates are still quite high. Furthermore, recidivism and mortality adjustments do not directly affect between-state variation, because we assigned the same rates to all states. We used the same procedure to estimate the number released from community supervision as a sensitivity test, because community supervision is correlated with state punitiveness but should not yield the same spillovers as prison. Figure 2 is a map of the percentage for 2010, by state, of the adult population that are ex-prisoners (Panel A), as well as the percentage of uninsured (Panel B).
Figure 2.
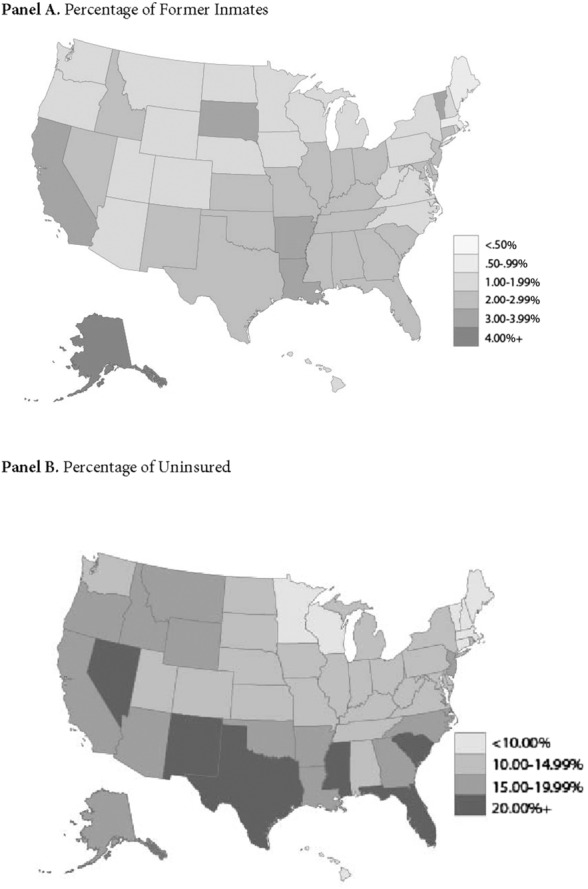
Percentage of Former Inmates and Uninsured by State, United States, 2010
Part 1
The Community Tracking Study (CTS) was designed to examine the effects of changing health care markets on individuals62 and has been used to study, among many other topics, the spillover effects of uninsurance.24,63 The popularity of the CTS for this purpose is no surprise. The CTS is a nationally representative household survey that has been conducted since 1996 in ongoing (approximately) 2-year cross sections. Each of the surveys contains a large number of respondents (no fewer than 37,000 per year for the waves used here) and collects information on health, health insurance, health care utilization, and sociodemographic background. The CTS instrument was designed to cover the relevant features of health care delivery. The CTS also allows researchers to link state-level data to individual observations. Although additional waves of the CTS were collected after 2003, alterations to the sampling design prohibit linking state-level information to post-2003 waves. Our analyses used data from 1996/1997, 1998/1999, 2000/2001, and 2003 (for simplicity, we refer to the waves spanning 2 years by their initial year of collection).
The CTS sample was collected in stages and across clusters, selecting 60 sites to provide a nationally representative sample (within the continental United States) and randomly sampling households in these sites. These site-based samples were supplemented by an independent national sample of households not tied to the sites. Most of these sites were metropolitan areas (9 were not). Although the survey instrument asked some questions about the experiences of the children living in the household, as reported by adults, our analyses were limited to the adult self-reports. Because of the CTS’s complex and geographically nested nature, we used survey weights in all the models.
Individual-Level Influences
Behavioral models regard health care utilization as a function of 3 categories of influences: (1) perceived need for services, (2) predisposing factors, and (3) enabling factors.64,65 By design, all 3 factors are well represented in the CTS. For perceived need, we controlled for self-rated poor health, generally regarded as the single strongest predictor of health care utilization.66 For predisposing factors, we controlled for age, years of education, race/ethnicity (non-Hispanic white, black, Hispanic, and other), marital status, and sex. For enabling factors, we controlled for household income, residence in a large metropolitan area (more than 200,000 residents), and health insurance, using uninsured as the reference category and dividing the insured by policy type: Medicare, private insurance, military insurance, or other public insurance (the bulk of which is Medicaid). We also controlled for the year of the survey.
These controls are needed to address the set of relevant influences, but including all of them together affected our interpretations. In particular, we expected our interpretations to be conservative to the extent that incarceration has other social, economic, and health effects. For instance, if higher incarceration in a region increased the spread of infectious disease, then controlling for health at the individual level would partly control for one spillover effect of incarceration. Similarly, if incarceration adversely altered the composition of health insurance policies in a market, then controlling for type of health insurance, especially Medicaid, would partly control for one spillover of incarceration. In short, the total spillover effect of incarceration may be greater than we estimated, even though we favored more statistical control over less. The same also applies to some of our state-level influences.
State-Level Influences
Our most important variable at the state level is the percentage of former inmates in the population. But in order to estimate the effects of incarceration per se, we had to control for state-level characteristics that are associated with the number of former inmates and perhaps also with health care. We therefore controlled for the percentage of the population that is African American, the percentage living below the poverty line, the percentage of unemployed, and the average state-level income (in 2000 dollars, set in $10,000 units). We also controlled for the percentage of uninsured, but as a potential mechanism rather than as a control. We assumed that incarceration increased the risk of not having insurance and, therefore, that some of the total effect of incarceration would pass through state-level uninsurance rates. Nevertheless, we hypothesized that incarceration matters even beyond its relationship with uninsurance. Other state-level control variables might render some of our conclusions conservative. If one believes, for example, that the percentage living below the poverty line is partly a consequence of incarceration, including it as a control variable will displace part of incarceration’s spillover effect.
Health Care Utilization and Process
We estimated the influence of state- and individual-level influences on multiple indicators of health care utilization and process. These outcomes vary along several dimensions, including type of service and setting. Exploring different kinds of services allowed us to evaluate spillover effects regardless of whether they operated at an institutional level (eg, hospitals cut services) or a provider level (eg, physicians decide to practice elsewhere). All the dependent variables are coded dichotomously for ease of comparison and comprehension.
Utilization
We examined 6 indicators of health care utilization, of which 3 refer to general utilization and 3 refer to specialized services. Unmet need refers to self-reports of forgoing or delaying necessary care. Respondents were asked, “During the past 12 months, was there any time that you didn’t get the medical care you needed?” This variable reflects a direct report of diminished access, but it conflates a perceived need for care with utilization. The remaining variables measure behavior strictly. Respondents were asked whether, over the preceding 12 months, they had visited a doctor (not including an emergency room or overnight stay in a hospital) or they had spent the night in a hospital (not including for the delivery of a child). To test the specificity of spillover effects, we also considered the utilization of specialized services. Respondents were asked whether, over the preceding 12 months, they had had surgery or had visited a mental health professional, including a psychiatrist, psychologist, psychiatric nurse, or clinical social worker. Women over the age of 40 were also asked whether they had received a mammogram in the last year (this question was not asked in 2003, reducing the available sample for models that use mammography).
Process
Beyond affecting utilization, spillover effects may result in a decline in the quality of services received or how those services were delivered. To test this idea, we examined indicators of the health care process. Respondents were asked whether they had a usual place for care. (A usual place indicates a more robust health care market.) We also examined whether respondents were satisfied with their care (if they visited a health care provider), satisfied with their choice of a primary care physician, satisfied with their choice of a specialist (if they needed or saw a specialist), and whether they trusted their doctor to “put [their] medical needs above all other considerations when treating [their] medical problems” (if they had a usual physician or had visited a physician in the previous 12 months). Respondents were coded as satisfied if they reported being “very satisfied” (the modal response for each satisfaction question) and as mistrusting if they disagreed “somewhat” or “strongly” that their doctor could be trusted.
Results
Tables1 and 2 show the initial basis for spillover effects on health care utilization and process-related outcomes, respectively. The tables present coefficients for both the individual- and state-level variables, although subsequent tables display only state-level coefficients (even though all the same individual-level covariates are also included in the model). Table1 begins with unmet need, perhaps the most common outcome in research assessing access to care. As noted, reports of unmet need are a function of both a self-assessed need for care and whether that need for care was met. This confluence of potentially countervailing influences is apparent in the coefficients: whereas income reduces the likelihood of reporting unmet need, education increases it, even though education and income are positively correlated. Although African Americans have less access to care and worse health, they are less likely than whites to report an unmet need. Other coefficients present a more consistent pattern, including those coefficients that are the focus of this study. Uninsurance is one of the largest barriers to care. All of the insurance coefficients are statistically significant and greater in magnitude than the estimates for all other categorical covariates except self-rated poor health.
Table 1.
Logit Regression Models of Utilization-Related Variables on Individual- and State-Level Covariates, 1996-2003 Community Tracking Study
| Visited | Visited | Psychiatric | ||||
|---|---|---|---|---|---|---|
| Unmet Need | Doctor | Hospital | Surgery | Mammogram | Care | |
| Individual-Level Influences | ||||||
| Insurance (versus none) | ||||||
| Medicare | −1.295*** | 1.742*** | 0.879*** | 0.918*** | 0.901*** | 0.640*** |
| (0.060) | (0.041) | (0.029) | (0.039) | (0.054) | (0.078) | |
| Private | −1.060*** | 1.204*** | 0.379*** | 0.701*** | 1.187*** | 0.343*** |
| (0.030) | (0.030) | (0.027) | (0.029) | (0.042) | (0.060) | |
| Military | −0.585*** | 1.076*** | 0.588*** | 0.782*** | 1.224*** | 0.944*** |
| (0.172) | (0.104) | (0.048) | (0.063) | (0.086) | (0.098) | |
| Public | −0.512*** | 1.458*** | 0.805*** | 0.908*** | 1.138*** | 1.115*** |
| (0.033) | (0.035) | (0.031) | (0.036) | (0.039) | (0.060) | |
| Poor health | 1.092*** | 0.648*** | 1.070*** | 0.561*** | −0.020 | 0.962*** |
| (0.029) | (0.025) | (0.018) | (0.016) | (0.019) | (0.026) | |
| Age | −0.014*** | 0.010*** | 0.015*** | 0.006*** | 0.018*** | −0.018*** |
| (0.001) | (0.001) | (0.000) | (0.001) | (0.001) | (0.001) | |
| Black | −0.085** | −0.106*** | 0.032 | −0.332*** | 0.113*** | −0.506*** |
| (0.032) | (0.028) | (0.031) | (0.022) | (0.027) | (0.055) | |
| Hispanic | −0.315*** | −0.480*** | −0.124*** | −0.368*** | 0.232*** | −0.381*** |
| (0.054) | (0.025) | (0.030) | (0.053) | (0.036) | (0.074) | |
| Other | 0.242*** | −0.327*** | −0.086** | −0.263*** | −0.172*** | −0.300*** |
| (0.065) | (0.031) | (0.031) | (0.046) | (0.039) | (0.055) | |
| Married | 0.096*** | 0.041** | −0.127*** | 0.061*** | 0.315*** | −0.447*** |
| (0.027) | (0.013) | (0.018) | (0.013) | (0.017) | (0.026) | |
| Female | 0.284*** | 0.903*** | 0.002 | 0.200*** | 0.247*** | |
| (0.017) | (0.012) | (0.020) | (0.012) | (0.015) | ||
| Large city | 0.110*** | 0.063*** | −0.020 | −0.015 | 0.120*** | 0.221*** |
| (0.024) | (0.018) | (0.047) | (0.021) | (0.038) | (0.038) | |
| Education | 0.043*** | 0.062*** | −0.006 | 0.032*** | 0.066*** | 0.081*** |
| (0.006) | (0.003) | (0.004) | (0.003) | (0.004) | (0.005) | |
| Ln (Family income) | −0.039*** | 0.077*** | −0.027*** | 0.019*** | 0.046*** | −0.032*** |
| (0.006) | (0.003) | (0.006) | (0.006) | (0.009) | (0.006) | |
| Year | 0.001 | 0.003 | 0.012*** | 0.013*** | 0.054*** | −0.015*** |
| (0.005) | (0.004) | (0.003) | (0.004) | (0.008) | (0.005) | |
| State-Level Influences | ||||||
| % Below poverty | 0.012 | 0.007 | 0.002 | −0.009** | 0.026*** | 0.006 |
| (0.007) | (0.005) | (0.006) | (0.004) | (0.006) | (0.009) | |
| Income | −0.075 | 0.145*** | −0.095** | −0.089*** | 0.166*** | 0.300*** |
| (0.043) | (0.031) | (0.037) | (0.026) | (0.034) | (0.058) | |
| % Unemployed | −0.041* | −0.011 | 0.015 | −0.010 | −0.051** | 0.022* |
| (0.016) | (0.010) | (0.008) | (0.008) | (0.020) | (0.013) | |
| % African American | −0.012*** | 0.007*** | 0.008*** | 0.003** | 0.004*** | −0.004 |
| (0.002) | (0.001) | (0.002) | (0.001) | (0.002) | (0.002) | |
| % Ex-prisoners | 0.102*** | −0.075*** | −0.118*** | −0.061*** | −0.081*** | −0.044 |
| (0.020) | (0.018) | (0.021) | (0.017) | (0.029) | (0.046) | |
| Constant | −4.500 | −9.366 | −26.336 | −29.050 | −112.667 | 26.803 |
| Observations | 179,012 | 179,012 | 179,012 | 179,012 | 46,184 | 179,012 |
*p <. 05; **p <. 01; ***p <. 001 (2-tailed test)
Table 2.
Logit Regression Models of Process-Related Variables on Individual- and State-Level Covariates, 1996-2003 Community Tracking Study
| Satisfied | Satisfied With | Satisfied With | Physician | ||
|---|---|---|---|---|---|
| Usual Place | With Care | Choice of Doctor | Choice of Specialist | Mistrust | |
| Individual-Level Influences | |||||
| Insurance (versus none) | |||||
| Medicare | 1.224*** | 0.807*** | 1.290*** | 1.306*** | −0.774*** |
| (0.039) | (0.026) | (0.047) | (0.053) | (0.035) | |
| Private | 1.144*** | 0.496*** | 0.787*** | 0.935*** | −0.394*** |
| (0.029) | (0.019) | (0.025) | (0.035) | (0.025) | |
| Military | 1.415*** | 0.468*** | 0.410*** | 0.537*** | −0.101 |
| (0.105) | (0.042) | (0.087) | (0.106) | (0.096) | |
| Public | 1.402*** | 0.618*** | 0.672*** | 0.781*** | −0.337*** |
| (0.045) | (0.022) | (0.036) | (0.061) | (0.046) | |
| Poor health | 0.254*** | −0.427*** | −0.467*** | −0.581*** | 0.494*** |
| (0.025) | (0.013) | (0.021) | (0.027) | (0.032) | |
| Age | 0.014*** | 0.012*** | 0.005*** | 0.016*** | −0.005*** |
| (0.001) | (0.000) | (0.001) | (0.001) | (0.001) | |
| Black | −0.085** | −0.136*** | −0.065 | −0.182*** | 0.106*** |
| (0.030) | (0.020) | (0.035) | (0.044) | (0.029) | |
| Hispanic | −0.698*** | −0.083** | −0.229*** | −0.047 | 0.201*** |
| (0.033) | (0.027) | (0.044) | (0.050) | (0.031) | |
| Other | −0.470*** | −0.369*** | −0.208*** | −0.409*** | 0.206*** |
| (0.044) | (0.032) | (0.057) | (0.081) | (0.047) | |
| Married | 0.311*** | 0.003 | 0.043** | 0.107*** | 0.039* |
| (0.023) | (0.013) | (0.015) | (0.031) | (0.019) | |
| Female | 0.567*** | 0.062*** | 0.006 | 0.001 | −0.165*** |
| (0.016) | (0.007) | (0.015) | (0.030) | (0.018) | |
| Large city | −0.194*** | −0.048** | −0.125*** | −0.050 | 0.156*** |
| (0.054) | (0.017) | (0.032) | (0.037) | (0.024) | |
| Education | 0.027*** | −0.017*** | −0.015*** | −0.004 | 0.011** |
| (0.004) | (0.003) | (0.004) | (0.007) | (0.004) | |
| Ln (Family income) | 0.082*** | 0.034*** | 0.035*** | 0.042*** | −0.019** |
| (0.004) | (0.006) | (0.004) | (0.010) | (0.007) | |
| Year | −0.008 | 0.022*** | 0.034*** | 0.017* | −0.051*** |
| (0.010) | (0.003) | (0.008) | (0.007) | (0.006) | |
| State-Level Influences | |||||
| % Below poverty | −0.009 | 0.010 | 0.004 | −0.002 | 0.022*** |
| (0.011) | (0.006) | (0.007) | (0.007) | (0.007) | |
| Income | 0.041 | 0.025 | −0.029 | −0.038 | 0.061 |
| (0.062) | (0.041) | (0.050) | (0.047) | (0.035) | |
| % Unemployed | 0.044* | −0.027*** | −0.020 | −0.012 | −0.001 |
| (0.019) | (0.008) | (0.012) | (0.011) | (0.012) | |
| % African American | 0.006 | 0.006*** | 0.014*** | 0.017*** | −0.013*** |
| (0.003) | (0.001) | (0.002) | (0.002) | (0.001) | |
| % Ex-prisoners | −0.157*** | −0.128*** | −0.146*** | −0.198*** | 0.167*** |
| (0.030) | (0.021) | (0.019) | (0.028) | (0.020) | |
| Constant | 14.247 | −43.516 | −65.791 | −32.408 | 98.330 |
| Observations | 179,012 | 166,087 | 175,482 | 74,243 | 161,189 |
*p <. 05; **p <. 01; ***p <. 001 (2-tailed test)
Outside these characteristics, however, the percentage of former inmates in a state is consistently and positively related to unmet need. The average marginal effect of a unit change in the percentage of ex-prisoners is 0.007 (dy/dx[.102]). In comparison with the other covariates, the marginal change from uninsurance to other public insurance is −0.052. Other studies found that a percentage-point increase in the uninsured resulted in a 2% increase in the odds of reporting unmet need (exp[0.020] = 1.02, Table 4, Pagán and Pauly24), whereas we found that each additional percentage point of ex-prisoners resulted in an 11% increase in the odds of reporting unmet need (exp[0.102] = 1.11). The ex-prisoner coefficient is also statistically significant controlling for state-level factors correlated with it, including the percentage of African Americans, the percentage of unemployed, and the percentage below the poverty line. (We explore the mediating effects of state-level uninsurance later.)
The relationship between incarceration and health care quality is apparent for all but one of the remaining utilization outcomes. Individuals in states with a large number of former inmates are less likely to visit a doctor, spend the night in a hospital, undergo surgery, and receive a mammogram. There is no relationship between the percentage of ex-prisoners and the likelihood of seeking care from a mental health professional. Notably, however, this question pertains to a wider variety of potential service providers, including clinical social workers, suggesting a broader market than is available for the other outcomes. There is little variation in the size of the relationship between the percentage of ex-prisoners and the outcomes, although the relationship is somewhat stronger for visiting a hospital than for visiting a physician.
Table2 estimates the same models for the process-related outcomes. The individual-level coefficients fit well-established patterns from the treatment-disparities literature. African Americans, for instance, are less likely than whites to have a usual place for care, to be satisfied with their care and choices, and to trust their physician. Family income is also positively associated with better health care experiences.
In addition, however, the percentage of ex-prisoners within a state significantly diminishes the quality of care. It does so across each of the process outcomes: having a usual place for care, being satisfied with the care received, and being satisfied with the choice of primary care physician and specialist. The percentage of ex-prisoners also increases the likelihood of mistrusting one’s physician. The strength of this relationship is consistent across outcomes. A percentage-point increase in the number of ex-prisoners within a state, for example, decreases the odds of having a usual place for care by approximately 14%, a difference larger than that between African Americans and whites. All of the ex-prisoner coefficients for the process-related outcomes exceed in absolute magnitude the same coefficients for the utilization-related outcomes. The single largest coefficient is for satisfaction with choice of a specialist, which is expected insofar as financial strains are especially consequential for specialized services.
Table3 turns to the mediating effects of uninsurance. State-level uninsurance should explain some of the ex-prisoner coefficient, but we do not expect uninsurance to reduce the coefficient to zero. Consistent with this, controlling for uninsurance decreases the ex-prisoner coefficient for most of the outcomes, but almost all the coefficients that were significant without controls remain significant with controls. The ex-prisoner coefficient for unmet need, for instance, is reduced by about half but remains significant. The most robust coefficients for state-level uninsurance apply to the process outcomes, but even there, the coefficient for the percentage of uninsured is much smaller than the coefficient for the percentage of ex-prisoners. With regard to the breadth of incarceration effects, the only outcome for which the coefficient for the percentage of ex-prisoners is eliminated is mammogram utilization.
Table 3.
Logit Regression of Utilization- and Process-Related Outcomes on Individual- and State-Level Influences, With Controls for Uninsurance, 1996-2003 Community Tracking Study
| Panel A. Utilization Outcomes | ||||||
|---|---|---|---|---|---|---|
| Unmet | Visited | Visited | Psychiatric | |||
| Need | Doctor | Hospital | Surgery | Mammogram | Care | |
| % Ex-prisoners | 0.056* | −0.052*** | −0.112*** | −0.060*** | −0.056 | −0.019 |
| (0.022) | (0.019) | (0.022) | (0.017) | (0.032) | (0.050) | |
| % Uninsured | 0.023*** | −0.012*** | −0.003 | −0.001 | −0.011* | −0.112* |
| (0.004) | (0.003) | (0.004) | (0.005) | (0.004) | (0.005) | |
| Panel B. Process Outcomes | |||||
|---|---|---|---|---|---|
| Usual | Satisfied | Satisfied With | Satisfied With | Physician | |
| Place | With Care | Choice of Doctor | Choice of Specialist | Mistrust | |
| % Ex-prisoners | −0.086** | −0.096*** | −0.090*** | −0.131*** | 0.098*** |
| (0.031) | (0.021) | (0.019) | (0.029) | (0.020) | |
| % Uninsured | −0.367*** | −0.015*** | −0.029*** | −0.033*** | 0.035*** |
| (0.005) | (0.003) | (0.004) | (0.005) | (0.005) | |
Finally, Tables4 and 5 present 2 types of sensitivity tests, one regarding the effect of prison relative to other modes of correctional supervision (presented in Panel A) and the other regarding the potential for market segmentation (presented in Panel B). To distinguish the effects of prison per se from other forms of punishment (and also to distinguish the effects of simply living in a more punitive state from living in a state where prison is used more frequently), we estimated the percentage of individuals within a state who had been convicted of a felony but were punished with community supervision rather than prison. The 2 forms of punishment are likely very different with respect to health. Community supervision does not entail exposure to the prison environment, but it also does not entail the same access to health care and it still results in a criminal record. For this reason, we expected the effects of the percentage of ex-community supervision to be between those of the percentage of ex-prisoners.
Table 4.
Logit Regression of Utilization-Related Variables, Sensitivity and Subgroup Analyses, 1996-2003 Community Tracking Study
| Unmet Need | Visited Doctor | Visited Hospital | Surgery | Mammogram | Psychiatric Care | |
|---|---|---|---|---|---|---|
| Panel A. Prisons Versus Community Supervision | ||||||
| % Ex-prisoners | 0.100*** | −0.075*** | −0.123*** | −0.062*** | −0.083*** | −0.047 |
| (0.020) | (0.018) | (0.020) | (0.017) | (0.030) | (0.045) | |
| % Ex-community | 0.019* | 0.001 | 0.026*** | 0.004 | 0.003 | 0.013 |
| supervision | (0.009) | (0.005) | (0.007) | (0.014) | (0.009) | (0.010) |
| Panel B. Social Distance Analysis | ||||||
| Among the insured | ||||||
| % Ex-prisoners | 0.154*** | −0.069*** | −0.101*** | −0.049** | −0.084** | −0.043 |
| (0.023) | (0.018) | (0.022) | (0.017) | (0.029) | (0.047) | |
| Among those 50 and older | ||||||
| % Ex-prisoners | 0.140*** | −0.129*** | −0.118*** | −0.049** | −0.028 | 0.015 |
| (0.030) | (0.029) | (0.015) | (0.017) | (0.033) | (0.046) | |
| Among whites | ||||||
| % Ex-prisoners | 0.162*** | −0.083*** | −0.089*** | −0.041 | −0.087** | 0.032 |
| (0.027) | (0.023) | (0.021) | (0.031) | (0.029) | (0.048) | |
| Among those at least 2× poverty level | ||||||
| % Ex-prisoners | 0.163*** | −0.080*** | −0.086** | −0.047** | −0.102*** | −0.011 |
| (0.024) | (0.017) | (0.028) | (0.018) | (0.024) | (0.042) | |
| Among the college educated | ||||||
| % Ex-prisoners | 0.125*** | −0.042 | 0.004 | −0.005 | −0.104** | 0.009 |
| (0.028) | (0.024) | (0.031) | (0.027) | (0.037) | (0.048) | |
| Among women | ||||||
| % Ex-prisoners | 0.139*** | −0.075*** | −0.115*** | −0.062** | −0.081** | −0.076 |
| (0.026) | (0.018) | (0.026) | (0.020) | (0.029) | (0.044) | |
*p <. 05; **p <. 01; ***p <. 001 (2-tailed test)
All models also include the covariates described in Table1. Coefficients are from 49 separate models.
Table 5.
Logit Regression of Process-Related Variables, Sensitivity and Subgroup Analyses, 1996-2003 Community Tracking Study
| Usual | Satisfied | Satisfied With | Satisfied With | Physician | |
|---|---|---|---|---|---|
| Place | With Care | Choice of Doctor | Choice of Specialist | Mistrust | |
| Panel A. Prisons Versus Community Supervision | |||||
| % Ex-prisoners | −0.154*** | −0.124*** | −0.141*** | −0.193*** | 0.162*** |
| (0.030) | (0.020) | (0.018) | (0.027) | (0.019) | |
| % Ex-community | −0.030*** | −0.023*** | −0.046*** | −0.034* | 0.037*** |
| supervision | (0.009) | (0.006) | (0.010) | (0.015) | (0.009) |
| Panel B. Social Distance Analysis | |||||
| Among the insured | |||||
| % Ex-prisoners | −0.167*** | −0.135*** | −0.157*** | −0.232*** | 0.167*** |
| (0.029) | (0.021) | (0.020) | (0.027) | (0.019) | |
| Among those 50 and older | |||||
| % Ex-prisoners | −0.119*** | −0.104*** | −0.181*** | −0.138*** | 0.172*** |
| (0.024) | (0.017) | (0.026) | (0.041) | (0.032) | |
| Among whites | |||||
| % Ex-prisoners | −0.153*** | −0.149*** | −0.210*** | −0.258*** | 0.203*** |
| (0.031) | (0.032) | (0.025) | (0.026) | (0.027) | |
| Among those at least 2× poverty level | |||||
| % Ex-prisoners | −0.164*** | −0.121*** | −0.163*** | −0.202*** | 0.182*** |
| (0.026) | (0.023) | (0.025) | (0.038) | (0.024) | |
| Among the college educated | |||||
| % Ex-prisoners | −0.115** | −0.158*** | −0.071* | −0.097** | 0.194*** |
| (0.038) | (0.026) | (0.036) | (0.033) | (0.023) | |
| Among women | |||||
| % Ex-prisoners | −0.156*** | −0.115*** | −0.168*** | −0.234*** | 0.158*** |
| (0.032) | (0.019) | (0.021) | (0.034) | (0.024) | |
*p <. 05; **p <. 01; ***p <. 001 (2-tailed test)
All models also include the covariates described in Table2. Coefficients are from 49 separate models.
The second test explicitly addressed the breadth of spillover effects. If the effects we have shown are truly reflective of spillovers and thus are applied to the entire market rather than specific consumers, they should be observed even among those furthest removed from incarceration. Most studies of the spillover effects of community uninsurance, for instance, consider the situation of the insured. In a parallel fashion, we examined the ex-prisoner effect among the insured. In addition, we examined the ex-prisoner effect among older persons (aged 50 or older), whites, those with incomes at least 200% of the federal poverty line, those with at least a 4-year college degree, and women. In this way, we explored the moderating influence of social distance as an instrument for evaluating the breadth of spillovers. Of course, we had already done this to a limited degree by examining the ex-prisoner effect on mammograms, but here we expanded the scope of this idea. If the spillover effects of incarceration apply to the entire market, we should observe significant effects in each of these subpopulations.
Table4 presents utilization-related outcomes. The models include all the control variables presented in Table1, although we show only the coefficients for the percentage of ex-prisoners (and the percentage of ex-community supervision in the first set of models). As expected, the effects of being an ex-prisoner exceeded those of being under ex-community supervision. In no case was the effect of being an ex-prisoner reduced a great deal, and in all cases the absolute value of the ex-prisoner coefficient exceeded that of ex-community supervision. The remaining models revealed remarkably robust associations across subgroups. Of the coefficients that were significant in the initial specification, only 4 were insignificant in the sensitivity analysis, despite, in many cases, a substantial reduction in the sample size. The effects of incarceration thus spill over to those least likely to be personally affected by it, including the insured, older persons, whites, the well educated, the non-poor, and women. In all these subsamples, the coefficients generally paralleled the coefficients drawn from the entire sample.
The same was true of the process-related outcomes, presented in Table5. Indeed, the percentage of ex-prisoner coefficients were particularly robust with respect to these outcomes: all the ex-prisoner coefficients remained statistically significant, regardless of the subpopulation. Of the subpopulations we explored, the college educated were perhaps least susceptible to the influence of the ex-prisoner population. But even in this case, the effects were significant and the coefficients were reduced at most by just over 50% (in the case of being satisfied with the choice of specialist).
Part 2
The analyses presented thus far are premised on the idea that spillovers from incarceration to health care reflect incarceration per se and not some other aggregate-level characteristic. The models presented in Part 1 are strong on individual-level controls, but they are vulnerable to the influence of unobserved state-level influences. A more appropriate test for between-state heterogeneity would try to capture all potential influences at the state level, recognizing the complex set of potential influences.
In Part 2, we estimated models that address unobserved heterogeneity in a rigorous way. We did so by looking at trends in 2 key outcomes related to our model but observed entirely at the aggregate level. What these outcomes lost in terms of specificity, they gained in statistical control. We first considered ex-prisoner effects on state-level uninsurance rates, a key mechanism in our framework (which was based on a series in the March Current Population Survey but reweighted by the State Health Access Data Assistance Center).67 We next considered ex-prisoner effects on emergency room utilization per 1,000 state residents (this series was based on the American Hospital Association’s Annual Survey but drawn for our study from the Kaiser State Health Facts online database).68 Interpreted in tandem, the 2 outcomes allowed us to see the process we described: Does incarceration increase uninsurance even as it also increases emergency room use?
Each outcome is observed over time, from 1987 to 2010 for the percentage of uninsured and from 1999 to 2010 for emergency room visits. Although the start dates for the 2 series differed, we wished to use as much time-series data as possible. The fact that we observed these outcomes over time allowed us to estimate the effects of change in the independent variables on change in the dependent variables. This also allowed us to control for unobserved influences. Specifically, we included state fixed-effects, which eliminated the influence of all stable state-level characteristics. This was especially important to our research questions, as state-level characteristics, such as political culture, safety-net service generosity, and overall policy environment, might vary in ways that affect both health care and criminal justice.69 Furthermore, most influences of this sort are enduring over time, and most of the variation is between states, meaning that state-level fixed-effects will eliminate their influence.
It is also clear, however, that some influences of this sort are dynamic. For instance, state-level demographic composition can change in meaningful ways, as can the health of state economies. Furthermore, previous research points to important dynamic policy influences: at the state level, growth in incarceration is associated with retrenchment in the welfare system.70,71 For this reason, we also controlled for time-variant demographic and policy-related influences. For the former we included the percentage of unemployed, the percentage below the poverty line, the percentage of African Americans, the percentage of Hispanics, and the violent crime rate. For the latter, we included indicators of the generosity of the state’s welfare system, drawn from the University of Kentucky Center for Poverty Research National Welfare Data.72 We included controls for the maximum monthly Temporary Assistance for Needy Families (TANF) benefit for a 4-person household, adjusted for inflation to reflect 2000 dollars. We also controlled for the ratio of the state minimum wage to the federal minimum wage, thereby evaluating the relative generosity of state-level income supports. Both variables are related to poverty, which we already statistically controlled, but presumably also reflect the generosity of states with respect to other needs. There was considerable variation between states and over time in both of these quantities.
The unit of analysis in Part 2 is state-years. The spatial and temporal properties of this type of data make ordinary least squares regression problematic. In particular, state-level errors are both geographically and temporally correlated. To address this, we used a panel-corrected standard errors approach, which allows for correlated errors between states, as well as state-specific heteroskedasticity. Furthermore, we dealt with over-time dynamics in 2 ways, each allowing for a different type of relationship between incarceration and health care outcomes over time. For each outcome, we present results from both a lagged dependent variable model, which assumes a more gradual impact on the outcome, and a first-order autoregressive model (AR1), which assumes an immediate impact.73 Both are plausible specifications for estimating incarceration spillovers, and differences between the two are instructive.
Results
Table6 shows the results. First, we found a positive association between the number of ex-prisoners in a state and the state-level uninsurance rate (but not between the number formerly under community supervision and the state-level uninsurance rate). The coefficient is significant at the. 05 level only when assuming an enduring impact rather than an immediate impact. To be sure, the coefficient was the same when we assumed an immediate impact (ie, under the AR1 specification), although the standard error was larger and the coefficient did not reach statistical significance by conventional standards. Each percentage-point increase in the ex-prisoner population led to a 0.32 percentage-point increase in the uninsured population.
Table 6.
Panel-Corrected Standard Errors Regression of State-Level Health Care System Variables on Felon Estimates and Other Independent Variables
| Percentage Uninsured | Emergency Room Visits | |||
|---|---|---|---|---|
| Lagged | Auto- | Lagged | Auto- | |
| Dependent | regressive | Dependent | regressive | |
| Variable | Model (AR1) | Variable | Model (AR1) | |
| % Ex-prisoners | .316* | .316 | 17.567+ | 28.174* |
| (.148) | (.200) | (10.110) | (12.515) | |
| % Ex- | −.039 | −.098 | 1.003 | 1.682 |
| community | (.066) | (.082) | (1.455) | (1.677) |
| supervision | ||||
| % Below | .227*** | .251*** | .003 | −.218 |
| poverty | (.031) | (.031) | (.952) | (.945) |
| % Unemployed | .130** | .177*** | 1.340 | 2.462* |
| (.043) | (.055) | (1.150) | (1.136) | |
| % African | −.103 | −.028 | 11.093** | 12.402** |
| American | (.103) | (.141) | (4.033) | (4.342) |
| % Hispanic | .102** | .155*** | .304 | 1.223 |
| (.036) | (.043) | (1.825) | (2.695) | |
| Violent crime | −.0001 | .0006 | .0851* | .1006* |
| rate | (.0006) | (.0007) | (.0383) | (.0438) |
| Maximum | −.0009 | −.0026*** | −.1138** | −.1355*** |
| TANF | (.0006) | (.0008) | (.0371) | (.0406) |
| benefit | ||||
| State minimum | .810* | .774 | 39.490 | 39.468 |
| wage/federal minimum wage | (.409) | (.528) | (25.594) | (23.513) |
| Lagged | .346*** | .354* | ||
| dependent | (.049) | (.176) | ||
| variable | ||||
| Rho (ρ) | .336 | .428 | ||
| State fixed-effects | ✓ | ✓ | ✓ | ✓ |
| Constant | 6.156* | 8.602* | −88.019 | 10.332 |
| Observations | 1,150 | 1,200 | 550 | 600 |
| States | 50 | 50 | 50 | 50 |
| Years | 1987-2010 | 1987-2010 | 1999-2010 | 1999-2010 |
+p <. 10; *p <. 05; **p <. 01; ***p <. 001 (standard errors in parentheses)
The second pair of models predicts emergency room visits. If growth in the former inmate population was positively associated with an increase in the number of uninsured individuals but did not affect (or even reduced) the demand for care, its estimated impact would be weaker. Our models revealed, however, that an increase in the percentage of ex-prisoners was associated with an increase in the rate of ER visits per capita. In this case, the relationship was larger when we assumed an immediate impact, perhaps reflecting the particularly strong needs of those recently released from prison.74 For each percentage-point increase in the ex-prisoner population, there were around 28 more ER visits for every 1,000 residents. The coefficient under the first model is not significant under conventional standards, although it would be if we used a 2-tailed p-value of less than. 10. The relationship seems large, although a single individual can make several visits to the ER. The observed range in values was as high as 901 visits per year. In the case of this model, a single former inmate would need to visit the ER 2 to 4 times per year. This number is not implausible: among Medicaid beneficiaries under the age of 65, approximately 15% made 2 or more ER visits in a year, and 5% had 4 or more.75 If the presence of former inmates in a household also increases ER use by family members, the rate of ER use by inmates need not be this high. Overall, the patterns found in Table6 were consistent with the patterns shown at the individual level, albeit with much greater control for between-state heterogeneity (and much less insight regarding individual-level influences).
Discussion
Our study established a robust relationship between the number of ex-prisoners within a state and the functioning and quality of its health care system. Although this finding contributes to particular substantive research literatures, we start with its broadest implications.
As is the case for labor markets and political institutions, our study demonstrates that the correctional system affects another system that would seem, on its face, far removed from criminal justice. The absolute number of former prisoners within a state is usually small, especially relative to the number of people who have more direct problems with access to care. For example, the percentage of uninsured exceeds the percentage of ex-prisoners by at least 5% and, in many states, by more than 15%. Yet the number of ex-prisoners is sufficiently large to affect the experiences of other health care consumers. This connection is perhaps even more remarkable given the considerable heterogeneity within regional health care markets, a characteristic that might ordinarily blunt the potential for spillovers. In any region, for example, the quality of service providers varies, as does how consumers decide where and when to seek care. Yet regardless of their personal situation, individuals are affected by the number of people who cycle through the prison system.
These spillovers are deep as well as broad and are not limited to a particular type of service. A general indicator of health care quality is reporting an unmet need for care. An even more sensitive indicator of spillover effects is whether an individual has difficulty receiving specialty care or technology-intensive screenings. We found spillover effects for virtually all these indicators, from basic access to care, to referrals, to the source of care, to the quality of care. We found that in states with a larger percentage of former inmates, people were less likely to report a usual place for care, to be satisfied with the care they received, to report satisfaction with their choice of health care provider, and to be convinced that their physician had their best interests in mind. Although some studies suggest that incarceration undermines the social fabric of neighborhoods,76 our study is one of the few to empirically demonstrate effects on trust among agents not directly tied to criminal justice.
From the perspective of the incarceration literature, these spillovers might be surprising. In recent years, punishment research has focused on the dramatic increase in incarceration and its heavy concentration among young African American men. Incarceration, then, is sometimes interpreted as an expanding institution oriented to the penalization of poverty.77 This research also emphasizes that former inmates usually return to a relatively small number of communities that are already disadvantaged and segregated.10 From these observations, incarceration is seen as deepening existing forms of inequality: already disadvantaged men are further harmed by a criminal record; their families suffer as a result of their absence and their diminished socioeconomic prospects; and the communities to which they return are further stigmatized for having high rates of both crime and incarceration. These themes are relevant to health care, too, inasmuch as health care is also sensitive to poverty. But these themes do not set the stage for spillover effects per se and, on the contrary, make some spillovers unlikely. It thus would be useful to consider how the institutional effects documented here differ from those documented elsewhere.
Because the communities in which incarceration is common are often isolated from the hospitals that provide services to other communities,78 the potential for spillover effects could be minimal. That is, segregation could blunt spillovers in health care rather than provide a pathway for them, as segregation does for economic outcomes. Our results show, however, that the health care system is not immune from incarceration, despite any market segmentation. Similarly, most of the work on the institutional effects of incarceration argues that incarceration exacerbates existing inequality. Yet spillover effects with respect to health care appear to affect the entire market for services rather than the experiences of a particular subset of consumers.
These results also speak to debates regarding the paradoxical effects of prisons as social service institutions.4 One strand of the incarceration literature shows that the prison system represents a real improvement in the social services available to many inmates, albeit one that is lost once inmates are released.79 Similarly, some people argue that the prison system provides an opportunity to deliver screening and treatment to an underserved and otherwise difficult-to-reach population.40 The results of our study do not diminish these opportunities, but they do suggest that efforts to improve the health of inmates will be shortsighted if they fail to provide support after release or if they focus too narrowly on specific services. For instance, efforts to improve care for inmates to date have referred largely to the risk of spreading infectious disease, as well as the potential cost savings of rigorous prison health programs.41 Likewise, some evidence shows that ex-prisoners with HIV who are not provided with services upon release see a rebound in their viral loads80 and that programs providing postrelease services save costs by preventing new infections.81 These arguments are compelling, but perhaps an even more persuasive case could be made if spillover effects of this sort were not limited to infectious disease. Viewing former inmates broadly as health care consumers in a revenue-sensitive system implies a much different set of possibilities than regarding them narrowly as disease vectors in neighborhoods.
Our results point to another paradox: systems that may be progressive from the standpoint of punishment may not be as progressive from the standpoint of health. We found a sharp difference in the effects of community supervision and prison. Ordinarily, community supervision is seen as a less severe form of punishment and a more affordable alternative to incarceration. The appeal of such programs has grown as the costs of maintaining overcrowded prisons have risen. Our results suggest that community supervision does not result in spillover effects in the same fashion as prison does, but community supervision nonetheless has some negative effects and, in certain instances, could lead to worse outcomes. The lower average effect of community supervision likely masks considerable between-state heterogeneity, as the character of community supervision varies. Not all states provide health care to those under supervision, and some serving under community supervision might benefit from the consolidated health services made available in some prison settings. It is likely that virtually all those who were once under community supervision suffered the detrimental effects of a criminal record, especially on employment, which could ultimately diminish access to care. In evaluating alternative punishments and their costs, it is essential to consider linkages between criminal justice and health care.
Limitations
Our study has several limitations, some of which affected how we interpreted the findings. The first pertains to geography. We focused on state-level indicators of incarceration and health insurance, but there is a potential asymmetry between what we could gather at the state level and the actual topography of care. We used state-level data because the state is the level at which correctional policy and many public health insurance programs, including Medicaid, are administered. For this reason, the policy levers for redressing spillover effects reside largely with states. Yet some spillover effects almost certainly occur in a much smaller geographic area. Consumers tend to visit providers that are near to them, and physicians are affiliated with hospitals close to their own practices.82 As a result, our state-level indicators are imperfectly correlated with the market experiences of the CTS respondents. This made our results conservative, but it also pointed to some useful sensitivity tests. We found significant relationships between incarceration and health care even among well-resourced patients, including the well educated, who are less likely to be restricted to providers in their immediate area.
It also was useful to compare our estimates of the effects of uninsurance with those based on smaller geographic units. Using the 2000 Community Tracking Study, Pagán and Pauly24 estimated, as we did, the spillover effects of aggregate uninsurance on unmet need. But they focused on communities rather than states. Despite using a geography more tailored to the actual market for care, they discovered effects of community uninsurance that are similar in magnitude to those produced by our models. One explanation for the empirical consistency over different geographies is the emergence of more regional health care systems, facilitated by the gradual consolidation of local systems.83
It is important, too, to emphasize that our data do not allow us to easily distinguish controls from mechanisms. This uncertainty pervades both parts of our analysis, but the implications are less severe than they might appear. At the aggregate level, both the percentage below the poverty line and the unemployment rate are partly functions of the number of former inmates, as earlier research revealed.11 Similarly, whether or not an individual is uninsured may be a function of the number of former inmates in a state, especially if that number is positively correlated with insurance premiums. For these reasons, our results can be regarded as conservative.
Our various dependent variables allowed us to provide a granular assessment of spillover effects, though some of the items are imperfect indicators of quality. For instance, reporting an unmet need for care entails both not receiving services and believing that such services were necessary. As is conventional for studies of this sort, we controlled for the need for services using self-rated health, which, because of its self-reported nature, is strongly related to the perceived need for care and, by extension, to utilization. By this logic, once self-rated health is controlled, the remaining variance in unmet need is more likely to reflect barriers to care than to need for care. Nevertheless, this combination of subjective and objective influences introduces uncertainty. For example, we know that African Americans have less access to care than whites do, but we found in our study—as have others—that African Americans are less likely to report unmet need. A similar uncertainty is apparent in some of the other outcomes. Having a usual source of care, for example, implies needing to visit a physician often enough to report a “usual” source, just as being satisfied with care involves having an illness that is sufficiently complex to allow a reasonable assessment of quality. In these ways, many of the dependent variables admit a mix of countervailing influences. Despite this, the effects of the ex-prisoner population on health care are remarkably consistent. In every case in which the percentage of ex-prisoners is significant, the coefficient is in the direction predicted by the proposition that a larger number of former inmates reduces access to, and the quality of, health care. The only other covariate in our model that showed a similarly robust and consistent pattern is whether the respondent had health insurance, suggesting that both could be characterized as barriers to care.
The Affordable Care Act and the Possibility of Reform
The health care landscape has changed since 2010 (when our aggregate-level analyses ended). The Affordable Care Act (ACA) was passed in 2010, and its rollout is ongoing. The ACA affects ex-prisoners in several ways, including by expanding Medicaid, by requiring most individuals to obtain health insurance, and by creating health insurance exchanges that will enable low-income individuals to purchase insurance. Although these elements might mitigate some of the difficulties that former inmates face, they clearly will not eliminate them. Simulations considering the take-up of Medicaid among former inmates estimate that 22% to 34% of former inmates would enroll in an insurance plan.84 Among those not eligible for Medicaid, 24% would be eligible for insurance tax credits that might allay the cost of buying private, nonemployer coverage through an exchange. The ACA is an improvement over the status quo, but it is not a cure for the problems introduced by incarceration. We should not expect it to eliminate the spillover effects found here, although it might dampen their impact.
The fact that an unusually ambitious reform initiative fails to eliminate the problem does not mean that the spillover effects of incarceration are out of reach of policy. On the contrary, the spillover effects of incarceration on health care are subject to perhaps more points of melioration than are many other spillover effects of incarceration. Furthermore, spillovers with respect to health care may be less subject to the political forces that make other aspects of prison reform difficult. The political effects of incarceration, for instance, ultimately depend on felon disenfranchisement laws. Eliminating these specific institutional effects of incarceration, therefore, depends on eliminating those specific laws. Similarly, reducing the labor market effects of incarceration depends partly on restricting the ability of employers to discriminate on the basis of a criminal record. In the case of health care, however, efforts to reduce spillover effects need not be directed toward only current or former inmates or laws pertaining to criminal justice. The expansion of the already existing health care safety net, including Medicaid, would surely ease many of the financial pressures underlying spillovers. In this regard, some advocates recommend suspending rather than terminating Medicaid benefits for inmates, which would make it easier for them to regain benefits upon release.45 It is also worth emphasizing that the politics of the Affordable Care Act—which are plainly quite strong—may be at least partly related to incarceration, insofar as felon disenfranchisement can tilt elections in favor of politicians less open to Medicaid expansion.85 It is very unlikely that enfranchising former inmates would have been enough to shift elections so that most states accepted the Medicaid expansion.12 Yet felon disenfranchisement represents another mechanism by which political factors can accentuate disadvantage in ways that redound on the health care system.
Conclusion
The case for providing additional resources to former inmates is often made in light of the harm done by a criminal record: incarceration undermines employment, wages, and health, and, by extension, the well-being of children, families, and communities. We found this case compelling on its own merits, but our study adds to the debate by expanding the ledger. We showed that incarceration affects those institutions directly responsible for health and well-being and that individuals far removed from the criminal justice system are affected as well. We also showed that the institutional effects of incarceration are not limited to a finite set of pathways and, indeed, that it is worth considering a more expansive framework for understanding institutional effects. While the effects of incarceration on unemployment rates are premised on keeping inmates out of the labor market, the effects of incarceration on health care are premised on the fact that inmates will always be in the market for health services. Similarly, whereas the institutional effects of incarceration on voting might increase inequality, the effects of incarceration on health care lower its quality for everyone. Finally, whereas neighborhood segregation ordinarily deepens the impact of incarceration, the effects of incarceration on health care spread well beyond local boundaries.
Although we did not emphasize health outcomes, the pathways we documented with respect to health care likely undermine health as well. Reducing access to care compromises the health of former inmates in the first instance, but in the long run it may affect the health of others too. These results thus suggest a corollary to Dostoyevsky’s famous admonition.86 Just as a society’s degree of civilization may be judged by its prisons, so too may its number of prisoners affect its capacity to provide a civilized level of care.
Acknowledgments:
The authors thank audiences at Rutgers University, the University of Wisconsin, and the International Sociological Association for helpful comments.
Funding/Support:
This research was funded in part by a Robert Wood Johnson Foundation Health Investigator Award to Jason Schnittker and Christopher Uggen.
Conflict of Interest Disclosures:
All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. No disclosures were reported.
References
- 1.Western B. Punishment and Inequality in America. New York, NY: Russell Sage; 2006. [Google Scholar]
- 2.Wakefield S, Uggen C. Incarceration and stratification. Ann Rev Sociol. 2010;36:387‐406. [Google Scholar]
- 3.Wildeman C. Parental imprisonment, the prison boom, and the concentration of childhood disadvantage. Demography. 2009;6:265‐281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Comfort M. Punishment beyond the legal offender. Ann Rev Law Soc Sci. 2007;3:271‐296. [Google Scholar]
- 5.Hagan J, Dinovitzer R. Collateral consequences of imprisonment for children, communities, and prisoners. In: Tonry M, Petersilia J, eds. Crime and Justice: A Review of Research. Vol 26 Chicago, IL: University of Chicago Press; 1999:121‐162. [Google Scholar]
- 6.Pettit B. Invisible Men: Mass Incarceration and the Myth of Black Progress. New York, NY: Russell Sage; 2012. [Google Scholar]
- 7.Pettit B, Western B. Mass imprisonment and the life course: race and class inequality in U.S. incarceration. Am Sociol Rev. 2004;69:151‐169. [Google Scholar]
- 8.Clear TR. Imprisoning Communities: How Mass Incarceration Makes Disadvantaged Places Worse. New York, NY: Oxford University Press; 2007. [Google Scholar]
- 9.Roberts DE. The social and moral cost of mass incarceration in African American communities. Stanford Law Rev. 2004;56:1271‐1305. [Google Scholar]
- 10.Sampson RJ, Loeffler C. Punishment’s place: the local concentration of mass incarceration. Daedalus. 2010;139:20‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Western B, Beckett K. How unregulated is the U.S. labor market? The penal system as a labor market institution. Am J Sociol. 1999;104:1030‐1060. [Google Scholar]
- 12.Uggen C, Manza J. Democratic contraction? Political consequences of felon disenfranchisement in the United States. Am Sociol Rev. 2002;67:777‐803. [Google Scholar]
- 13.National Research Council. The Growth of Incarceration in the United States: Exploring Causes and Consequences. Washington, DC: National Academies Press; 2014. [Google Scholar]
- 14.Mayer SE, Jencks C. Growing up in poor neighborhoods: how much does it matter? Science. 1989;243:1441‐1445. [DOI] [PubMed] [Google Scholar]
- 15.Uggen C, Manza J, Thompson M. Citizenship, democracy, and the civic reintegration of criminal offenders. Ann Am Acad Polit Soc Sci. 2006;605:281‐310. [Google Scholar]
- 16.Bonczar TP. Prevalence of Imprisonment in the U.S. Population, 1974–2001. Washington, DC: US Department of Justice, Bureau of Justice Statistics; 2003. [Google Scholar]
- 17.Carson EA, Golinelli D. Prisoners in 2012: Trends in Admissions and Releases, 1991–2012. Washington, DC: U.S. Department of Justice; 2013. [Google Scholar]
- 18.Maruschak LM, Bonczar TP. Probation and Parole in the United States, 2012. Washington, DC: US Department of Justice, Bureau of Justice Statistics; 2013. [Google Scholar]
- 19.Carson EA. Prisoners in 2013. Washington, DC: US Department of Justice, Bureau of Justice Statistics; 2014. [Google Scholar]
- 20.Warren J, Gelb A, Horowitz J, Riordan J. One in 100: Behind Bars in America 2008. Washington, DC: Pew Center on the States, Pew Charitable Trusts; 2008. [Google Scholar]
- 21.Glaze LE, Maruschak LM. Parents in Prison and Their Minor Children. Washington, DC: US Department of Justice, Bureau of Justice Statistics; 2008. [Google Scholar]
- 22.Guerino P, Harrison PM, Sabol WJ. Prisoners in the United States. Washington, DC: US Department of Justice, Bureau of Justice Statistics; 2011. [Google Scholar]
- 23.Institute of Medicine. A Shared Destiny: Community Effects of Uninsurance. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 24.Pagán JA, Pauly MV. Community‐level uninsurance and the unmet medical needs of insured and uninsured adults. Health Serv Res. 2006;41:788‐803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pagán JA, Asch DA, Brown CJ, Guerra CE, Armstrong K. Lack of community insurance and mammography screening rates among insured and uninsured women. J Clin Oncol. 2008;26:1865‐1870. [DOI] [PubMed] [Google Scholar]
- 26.Institute of Medicine. Coverage Matters: Insurance and Health Care. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 27.Schoen C, DesRoches C. Uninsured and unstably insured: the importance of continuous insurance coverage. Health Serv Res. 2000;35:187‐206. [PMC free article] [PubMed] [Google Scholar]
- 28.Fields WW, Asplin BR, Larkin GL, et al. The Emergency Medical Treatment and Labor Act as a federal health care safety net program. Acad Emerg Med. 2001;8:1064‐1069. [DOI] [PubMed] [Google Scholar]
- 29.Wilper AP, Woolhandler S, Boyd JW, et al. The health and health care of US prisoners: results of a nationwide survey. Am J Public Health. 2009;99:666‐672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mallik‐Kane K, Visher CA. Health and Prisoner Reentry: How Physical, Mental, and Substance Abuse Conditions Shape the Process of Reintegration. Washington, DC: Urban Institute Press; 2008. [Google Scholar]
- 31.Patterson E. Incarcerating death: mortality in the U.S. state correctional facilities, 1985–1998. Demography. 2010;47:587‐607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosen DL, Wohl DA, Schoenbach VJ. All‐cause and cause‐specific mortality among black and white North Carolina state prisoners, 1995–2005. Ann Epidemiol. 2011;21:719‐726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schnittker J, John A. Enduring stigma: the long‐term effects of incarceration on health. J Health Soc Behav. 2007;16:115‐130. [DOI] [PubMed] [Google Scholar]
- 34.Massoglia M. Incarceration as exposure: the prison, infectious disease, and other stress‐related illnesses. J Health Soc Behav. 2008;16:56‐71. [DOI] [PubMed] [Google Scholar]
- 35.Andrus JK, Fleming DW, Knox C, et al. HIV testing in prisoners: is mandatory testing mandatory? Am J Public Health. 1989;79:840‐842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dixon PS, Flanigan TP, DeBuono BA, et al. Infection with the human immunodeficiency virus in prisoners: meeting the health care challenge. Am J Med. 1993;95:629‐635. [DOI] [PubMed] [Google Scholar]
- 37.Rosen DL, Schoenbach VJ, Wohl DA, White BL, Stewart PW, Golin CE. An evaluation of HIV testing among inmates in the North Carolina prison system. Am J Public Health. 2009;99:S452‐S459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hammett TM. HIV/AIDS and other infectious diseases among correctional inmates: transmission, burden, and an appropriate response. Am J Public Health. 2006;96:974‐978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gaes GG, Kendig N. The skill sets and health care needs of release offenders. In: Travis J, Waul M, eds. Prisoners Once Removed: The Impact of Incarceration and Reentry on Children, Families, and Communities. Washington, DC: Urban Institute Press; 2003:105‐153. [Google Scholar]
- 40.Freudenberg N. Jails, prisons, and the health of urban populations: a review of the impact of the correctional system on community health. J Urban Health. 2001;78:214‐235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hammett T. Making the case for health interventions in correctional facilities. J Urban Health. 2001;78:236‐240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baillargeon J, Giordano TP, Rich JD, et al. Accessing antiretroviral therapy following release from prison. JAMA. 2009;301:848‐857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pager D, Western B, Bonikowski B. Discrimination in a low‐wage labor market: a field experiment. Am Sociol Rev. 2009;74:777‐799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lutzsky AW, Holahan J, Wiener JM. Health Policy for Low‐Income People: Profiles of 13 States. Washington, DC: Urban Institute Press; 2002. [Google Scholar]
- 45.Wakeman S, McKinney M, Rich J. Filling the gap: the importance of Medicaid continuity for former inmates. J Gen Intern Med. 2009;24:860‐862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Morrissey JP, Dalton KM, Steadman HJ, Cuddeback GS, Haynes D, Cuellar A. Assessing gaps between policy and practice in Medicaid disenrollment of jail detainees with severe mental illness. Psychiatr Serv. 2006;57:803‐808. [DOI] [PubMed] [Google Scholar]
- 47.Rosen DL, Dumont DM, Cislo AM, Brockmann BW, Traver A, Rich JD. Medicaid policies and practices in US state prison systems. Am J Public Health. 2014;104:418‐420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mallik‐Kane K. Returning Home Illinois Policy Brief: Health and Prisoner Reentry. Washington, DC: Urban Institute Justice Policy Center; 2005. [Google Scholar]
- 49.Wang EA, Hong CS, Shavit S, Sanders R, Kessell E, Kushel MB. Engaging individuals recently released from prison into primary care: a randomized trial. Am J Public Health. 2012;102:e22‐e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Conklin T, Lincoln T, Tuthill R. Self‐reported health and prior health behaviors of newly admitted correctional inmates. Am J Public Health. 2000;90:1939‐1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Meyer JP, Qiu J, Chen NE, Larkin GL, Altice FL. Emergency department use by released prisoners with HIV: an observational longitudinal study. PLoS ONE. 2012;7:e42416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.LaCalle E, Rabin E. Frequent users of emergency departments: the myths, the data, and the policy implications. Ann Emerg Med. 2010;56:42‐48. [DOI] [PubMed] [Google Scholar]
- 53.Jha A, Orav J, Li Z, Epstein AM. Concentration and quality of hospitals that care for elderly black patients. Archives Intern Med. 2007;167:1177‐1182. [DOI] [PubMed] [Google Scholar]
- 54.Smith DB. The racial segregation of hospital care revisited: Medicare discharge patterns and their implications. Am J Public Health. 1998;88:461‐463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stevens R. In Sickness and in Wealth: Amerca’s Hospitals in the Twentieth Century. New York, NY: Basic Books; 1989. [Google Scholar]
- 56.Cunningham PJ, Tu HT. A changing picture of uncompensated care. Health Aff. 1997;16:167‐175. [DOI] [PubMed] [Google Scholar]
- 57.Needleman J. Nonprofit to for‐profit conversions by hospitals, health insurers, and health plans. Public Health Rep. 1999;114:108‐119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Derlet RW. Overcrowding in emergency departments: increased demand and decreased capacity. Ann Emerg Med. 2002;39:430‐432. [DOI] [PubMed] [Google Scholar]
- 59.Lipscomb J. Managed care market penetration, spillover effects, and the quality of cancer care. J Natl Cancer Inst. 2005;97:242‐244. [DOI] [PubMed] [Google Scholar]
- 60.Joy JE, Penhoet EE, Pettiti DB. Saving Women’s Lives: Strategies for Improving Breast Cancer Detection and Diagnosis. Washington, DC: Institute of Medicine and National Research Council; 2005. [PubMed] [Google Scholar]
- 61.Eberth JM, Eschbach K, Morris JS, Nguyen HT, Hossain MM, Elting LS. Geographic disparities in mammography capacity in the South: a longitudinal assessment of supply and demand. Health Serv Res. 2014;49:171‐185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Center for Studying Health System Change. Community Tracking Study Household Survey, 1996–2003 (computer file). Washington, DC: Center for Studying Health System Change (producer); Ann Arbor, MI: Interuniversity Consortium for Political and Social Research (distributor); 2003.
- 63.Cunningham PJ, Kemper P. Ability to obtain medical care for the uninsured: how much does it vary across communities? JAMA. 1998;280:921‐927. [DOI] [PubMed] [Google Scholar]
- 64.Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Q. 1973;51:95‐124. [PubMed] [Google Scholar]
- 65.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36:1‐10. [PubMed] [Google Scholar]
- 66.Miilunpalo S, Vuori I, Oja P, Pasanen M, Urponen H. Self‐rated health status as a health measure: the predictive value of self‐reported health status on the use of physician services and on mortality in the working‐age population. J Clin Epidemiol. 1997;50:517‐528. [DOI] [PubMed] [Google Scholar]
- 67.State Health Access Data Assistance Center. Comparing state unisurance estimates: SHADAC‐enhanced CPS and CPS (issue brief no. 21). Minneapolis, MN: University of Minnesota; 2010. [Google Scholar]
- 68.Kaiser Family Foundation. The Kaiser Family Foundation state health facts. Menlo Park, CA: Kaiser Family Foundation; 2013. http://kff.org/statedata/. Accessed August 2013. [Google Scholar]
- 69.Barker V. The politics of punishing: building a state governance theory of American imprisonment variation. Punishment & Society. 2006;8:5‐33. [Google Scholar]
- 70.Beckett K, Western B. Governing social marginality: welfare, incarceration, and the transformation of state policy. Punishment Soc. 2001;3:43‐59. [Google Scholar]
- 71.Sugie NF. Punishment and welfare: paternal incarceration and families’ receipt of public assistance. Soci Forces. 2012;90(4):1403‐1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.University of Kentucky Center for Poverty Research. UKCPR national welfare data, 1980–2013. Lexington, KY: Gatton College of Business and Economics, University of Kentucky; 2014. http://www.ukcpr.org/data. Accessed November 5, 2014. [Google Scholar]
- 73.Beck N, Katz JN. Modeling dynamics in time‐series cross‐sectional political economy data. Social science working paper no. 1304. Pasadena, CA: California Institute of Technology; 2009. [Google Scholar]
- 74.Binswanger IA, Stern MF, Deyo RA, et al. Release from prison—a high risk of death for former inmates. N Engl J Med. 2007;356:157‐165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Garcia TC, Bernstein AB, Bush MA. Emergency department visits and visitors: who used the emergency room in 2007? NCHS data brief no. 38. Hyattsville, MD: National Center for Health Statistics; 2010. [PubMed] [Google Scholar]
- 76.Rose DR, Clear TR. Incarceration, reentry, and social capital: social networks in the balance. In: Travis J, Waul M, eds. Prisoners Once Removed: The Impact of Incarceration and Reentry on Children, Families, and Communities. Washington, DC: Urban Institute Press; 2003:313‐341. [Google Scholar]
- 77.Wacquant L. Punishing the Poor: The Neoliberal Government of Social Insecurity. Durham, NC: Duke University Press; 2009. [Google Scholar]
- 78.Sarrazin MV, Campbell M, Rosenthal GE. Racial differences in hospital use after acute myocardial infarction: does residential segregation play a role? Health Aff. 2009;28:w368‐w378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Abraham LK. Mama Might Be Better off Dead: The Failure of Health Care in Urban America. Chicago, IL: University of Chicago Press; 1993. [Google Scholar]
- 80.Stephenson BL, Wohl DA, Golin CE, Tien H‐C, Stewart P, Kaplan AH. Effect of release from prison and re‐incarceration on the viral loads of HIV‐infected individuals. Public Health Rep. 2005;120:84‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Varghese B, Peterman T. Cost‐effectiveness of HIV counseling and testing in US prisons. J Urban Health. 2001;78:304‐312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wennberg JE, Cooper MM. The Dartmouth Atlas of Health Care in the United States. Chicago, IL: American Hospital Publishing, 1996. [PubMed] [Google Scholar]
- 83.Cuellar AE, Gertler PJ. Trends in hospital consolidation: the formation of local systems. Health Aff. 2003;22:77‐87. [DOI] [PubMed] [Google Scholar]
- 84.Cuellar AE, Cheema J. As roughly 700,000 prisoners are released annually, about half will gain health coverage and care under federal laws. Health Aff. 2012;31:931‐938. [DOI] [PubMed] [Google Scholar]
- 85.Manza J, Uggen C. Locked Out: Felon Disenfranchisement and American Democracy. New York, NY: Oxford University Press; 2006. [Google Scholar]
- 86.Dostoyevsky F. The House of the Dead (1862). London: Penguin; 1985. [Google Scholar]


