Abstract
Purpose
Accumulating evidence suggests an important role for psychosocial work factors in injury, but little is known about the interaction between psychosocial factors and previous injury experience on subsequent injury risk. We examined the relationships between psychosocial work factors and new or recurrent injury among hospital workers.
Methods
We studied 492 hospital workers including 116 cases with baseline injury and 376 injury-free referents at baseline over follow-up. Job strain, total support, effort– reward imbalance, overcommitment, and musculoskeletal injury at baseline were examined in logistic regression models as predictors of new or recurrent injury experienced during a 2-year follow-up period.
Results
The overall cumulative incidence of injury over follow-up was 35.6 % (51.7 % for re-injury among baseline injury cases; 30.6 % for new injury among referents). Significantly increased risks with baseline job strain (OR 1.26; 95 % CI 1.02–1.55) and effort–reward imbalance (OR 1.42; 95 % CI 1.12–1.81) were observed for injury only among the referents. Overcommitment was associated with increased risk of injury only among the cases (OR 1.58; 95 % CI 1.05–2.39).
Conclusions
The effects of psychosocial work factors on new or recurrent injury risk appear to differ by previous injury experience, suggesting the need for differing preventive strategies in hospital workers.
Keywords: Work-related injury, Injury recurrence, Psychosocial factors, Overcommitment, Job strain, Effort–reward imbalance, Hospital workers
Introduction
In the USA today, over six million workers are employed in hospital settings (U.S. Bureau of Labor Statistics 2014). The incidence rates for occupational injuries are high among hospital workers, roughly twice the total rate among all US workers: in 2012, 6.1 per 100 full-time workers in private hospitals, 8.5 in state government hospitals, and 5.7 in local government hospitals (U.S. Bureau of Labor Statistics 2013a). Similar patterns of excess injury risk in the health-care industry sector have been reported internationally (European Commission 2011; Workers’ Compensation Board of British Columbia 2013). In general, musculoskeletal disorders are the most prevalent work-related problems, accounting for one-third of all lost-time events, with longer time away from work per event (U.S. Bureau of Labor Statistics 2013b).
Previous studies consistently show that prior musculo-skeletal injury imparts increased risk of subsequent injury. Lipscomb et al. (2008) examined back injury claims among carpenters, finding that the recurrent injury rate was 80 % higher than the new incident injury rate. In another study of a general working population, previous back injury was associated with approximately 50 % greater odds of work-related back re-injury over one-year follow-up (Keeney et al. 2013). Specifically among health-care workers, previous injury was associated with 1.6 times increased odds of back injury at one-year follow-up (Andersen et al. 2014). In another study, one or several episodes of back pain in the preceding year were significantly associated with a greater than twofold odds of sick leave due to back or neck pain during the 18-month follow-up (Bergstrom et al. 2007).
Beyond previous injury as a risk factor for subsequent injury, there also is accumulating evidence that psychosocial work factors can play an important role in injury risk (Leka and Jain 2010). In particular, multiple studies have examined the impact of job strain from high job demand and low job control and imbalance between effort and reward at work, observing a significant association with work-related injuries and musculoskeletal pain in various occupational groups (Burgel et al. 2010; Christensen and Knardahl 2014; Gillen et al. 2007; Hannan et al. 2005; Lee et al. 2014; Rugulies and Krause 2005, 2008; Schoenfisch and Lipscomb 2009). In addition, overcommitment, which is a pattern of excessive work-related commitment and difficulty “unwinding” from work in response to stressful work environments, has been linked to poor health status or increased musculoskeletal pain (Griep et al. 2011; Herin et al. 2011; Huysmans et al. 2012; Joksimovic et al. 2002). On the other hand, support at work from supervisors and coworkers has been suggested to mitigate against the risk of adverse health impact or musculoskeletal pain (Griep et al. 2011; Kraatz et al. 2013; Solidaki et al. 2010).
As such, the impacts of psychosocial work factors and previous injury have been well studied separately, but the question of interactions between those two types of factors has not been integrated into research on subsequent injury risk. We previously followed 582 hospital workers with or without baseline musculoskeletal injury and found that those who had such an injury had improved but nonetheless still manifested significantly lower physical functioning at 2-year follow-up (Gillen et al. 2010). Because workers with a previous injury may be at risk of subsequent injury but also may be differentially vulnerable to various work organization and psychosocial stressors, we further analyzed these data to better elucidate injury risk in light of such potential interactions. Specifically, we aimed to verify the anticipated prospective injury risk associated with psychosocial factors at baseline and additionally to test the associations between selected psychosocial work stressors and subsequent injury, taking into account prior injury.
Methods
Study design and sample
We analyzed data from the Gradients of Occupational Health in Hospital Workers (GROW) study. This investigation was conducted among workers in two hospitals in the San Francisco Bay Area recruited and followed from 2002 to 2004. GROW included 664 hospital workers; 166 cases with work-related musculoskeletal injuries; and 498 referents matched by either job group, shift type or through incidence density (one match from each for a 1:3 case: referent ratio). The GROW study followed the cases and referents for 2 years, including structured interviews and direct observations in a subset of subjects. Detailed information on the study is available elsewhere (Gillen et al. 2007; Hammond et al. 2010; Rugulies et al. 2004), and we have previously reported an analysis of injury recovery based on longitudinal follow-up at 2 years (Gillen et al. 2010). In brief, musculo-skeletal injury cases all had experienced an acute or cumulative work-related musculoskeletal injury that was eligible for workers’ compensation. The injuries had been evaluated by physicians or nurse practitioners at the respective employee health clinics at the two hospital recruitment sites. The types of musculoskeletal injury were classified by the injured body region: back, neck, upper extremity, or lower extremity. The GROW study was approved by the University of California San Francisco's Committee on Human Research.
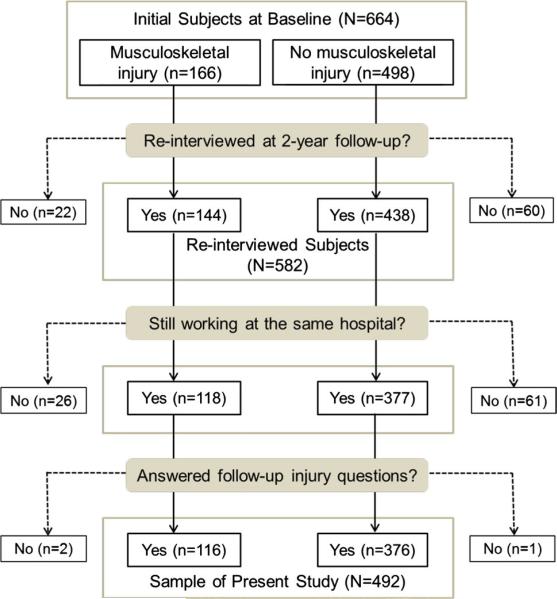
Interview data for cases and referents who were still working at the sample hospitals and were successfully restudied at 2-year follow-up without missing outcome data (n = 492) formed the basis for this analysis. Figure 1 shows the flow of subject inclusion and exclusion for this subsequent evaluation. The mean age of the study sample was 45.9 years at baseline; females comprised 74.2 % of the group. Non-Hispanic whites (42.5 %) and nurses (39.2 %) made up the largest racial/ethnic and job groups within the study, but nonetheless comprised less than half of the participants. Compared to this study sample, those who were not re-studied (n = 172) included significantly fewer non-His panic white subjects (29.3 %) and nurses (30.5 %; p < 0.05).
Fig. 1.
Study sample
Study variables and measures
The primary outcome variable of this study was a work-related subsequent injury, defined as either new or recurrent events during the 2-year follow-up period. New or recurrent injury was defined by an affirmative response to the following question, “Since your last interview, have you experienced any injury on the job, either a new injury or an aggravation of a prior injury?” Those who experienced a new or recurrent subsequent injury were asked: “How many full days of work did you miss for this reason?”; “How many part work days?”; and “Was this injury reported or filed?” For the purposes of this analysis, those who missed any full or part days were defined as having experienced lost-time injury (that is, one full day or more were not required to define such an event). Those who reported or filed the injury were defined as having experienced a reported injury.
Taking into account baseline injury (case status), the predictor variables of primary study interest were psychosocial factors measured at baseline interviews. Psychosocial factors were measured using the Job Content Questionnaire (JCQ) and the Effort–Reward Imbalance (ERI) Questionnaire (Karasek et al. 1998; Siegrist et al. 2004). The JCQ scales of job demand (five items), job control (nine items), supervisor support (four items), and coworker support (four items) measure job stress factors and social support at work using a 4-point Likert scale ranging from “1 = strongly agree” to “4 = strongly disagree.” Job strain was derived as the ratio of job demand to job control. Total support was derived as the sum of supervisor support and coworker support. The ERI scales of effort (6 items) and reward (11 items) measure effort put in work and rewards received in terms of money, esteem, job security, and career opportunities. Effort and reward scales used a two-step process for responses: 1) agree or disagree and 2) a 4-point Likert-type scale ranging from “1 = not at all distressed” to “4 = very distressed.” ERI, the imbalance between effort and reward, was derived as the ratio of effort to reward, multiplied by a correction factor of 11/6 for differences in the numbers of scale items. Over-commitment (six items) was measured using a 4-point Likert scale ranging from “1 = strongly agree” to “4 = strongly disagree.” Validity and reliability of the JCQ and ERI Questionnaires have been well documented in previous studies (Karasek et al. 1998; Siegrist et al. 2004).
Other study variables of interest included age, sex, race and ethnicity, job group, comorbidities, and depression at baseline. Comorbidities were asked by the following question, “Has a medical doctor ever told you that you have any of the following medical conditions: asthma, diabetes, high blood pressure, coronary artery disease or heart attack, arthritis, back or neck condition such as a slipped disc, carpal tunnel syndrome, and tendonitis?” Based on the answers, dichotomous variables of musculoskeletal comorbidity and other medical comorbidity were created. Depressive symptoms were measured by the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff 1977). The CES-D scale consists of 20 items measuring depressive symptoms over the past 7 days using a 4-point Likert-type scale ranging from “1 = rarely or none of the time (<1 day)” to “4 = most or all of the time (5–7 days).” The psychometric properties of CES-D have been widely tested in previous studies (Carleton et al. 2013).
Statistical analysis
Descriptive statistics were used to summarize the characteristics of the sample and injury outcome variables. The proportion of subsequent new or recurrent injury over follow-up indicates cumulative incidence. Baseline characteristics were compared by injury experience over follow-up using Chi-square test or t test. The associations of subsequent new or recurrent injury with baseline musculoskeletal injury and psychosocial factors were examined using logistic regression. Odds ratios (ORs) and 95 % confidence intervals (CI) were obtained. In the analysis of psychosocial factors, hierarchical multivariable analyses were conducted by adding the following covariates step by step: unadjusted model (Model 1); plus age, sex, race/ethnicity (non-Hispanic white vs. other), and job group (nurse vs. other) (Model 2); plus musculoskeletal comorbidity (Model 3); and plus CES-D measured depression (Model 4). Continuous scale scores of psychosocial factors were divided by their observed standard deviation (SD) to yield comparative units of analysis across measures. Thus, the estimated ORs indicate the likelihood of outcome experience expressed per 1 SD increment.
We hypothesized that the associations between psychosocial factors and subsequent new or recurrent injury would differ by case versus referent status. To test this, we conducted analyses stratified by baseline musculoskeletal injury status for job strain, ERI, total support, and overcommitment. For statistical testing of potential interactions, the product terms of baseline musculoskeletal injury and psychosocial variables were added to the multivariable models. Because nurses were the largest occupational group in this study, we also examined the associations and interactions separately in the subgroups of nurses and all others.
Analyses used a standard statistical package SAS 9.4 (SAS Institute, Inc., Cary, NC). Statistical significance was set at p < 0.05.
Results
Subsequent new or recurrent injury outcomes reported at 2-year follow-up interview are presented in Table 1. Of 492 hospital workers, 175 (35.6 %) reported experiencing a new or recurrent injury since the baseline interview. While the cases with baseline injury at study entry accounted for 23.6 % of the sample, these cases accounted for 34.3 % (n = 60) of those who reported subsequent injury at follow-up. Cumulative incidence of new or recurrent injury was significantly higher among cases than referents (51.7 vs. 30.6 %; p < 0.0001). Of 175 workers with a subsequent new or recurrent injury, 112 (64.0 %) reported the injury to a supervisor, while the remainder (36.0 %) of injury events went un-reported. Ninety-three (53.1 %) lost work time due to the injury; of these, 79 (85.0 %) reported the injury, while 14 (15.0 %) did not report the event despite lost work time. In terms of new or recurrent injury incidence by the body part of baseline injury, there was no consistent pattern across the three injury types of any injury, reported injury, and lost-time injury.
Table 1.
Subsequent injury experience over 2-year follow-up by baseline musculoskeletal injury status among 492 hospital workers
| Injury status at baseline interview | Subsequent injury events over 2-year follow-up |
|||||
|---|---|---|---|---|---|---|
| Any injury |
Reported injury |
Reported lost-time injury |
||||
| N | % | N | % | N | % | |
| All cases and referents (N = 492) | 175 | 35.6 | 112 | 22.8 | 79 | 16.1 |
| Cases (any injury; N = 116) | 60 | 51.7 | 36 | 31.0 | 25 | 21.6 |
| Upper extremity injury (N = 53) | 29 | 54.7 | 17 | 32.1 | 12 | 22.6 |
| Back injury (N = 33) | 15 | 45.5 | 10 | 30.3 | 8 | 24.2 |
| Neck injury (N = 13) | 7 | 53.8 | 3 | 23.1 | 3 | 23.1 |
| Lower extremity injury (N = 17) | 9 | 52.9 | 6 | 35.3 | 2 | 11.8 |
| Referents (no injury; N = 376) | 115 | 30.6 | 76 | 20.2 | 54 | 14.4 |
Injury status at baseline interview based on employee health clinic report. Subsequent injury events based on participant responses at follow-up interview
New or recurrent injury experiences by the sample characteristics are presented in Table 2. Injuries were significantly more common among female compared to male workers (p < 0.01). Non-Hispanic white workers were less likely to have a new or recurrent injury than other racial/ ethnic groups combined (p = 0.02). Injuries were also more common among those who ever had a musculoskeletal comorbidity compared to others (p < 0.001). The mean baseline CES-D score was significantly higher (indicating more depressive symptoms) among those who went on to experience a new or recurrent injury than their counterparts (p = 0.01).
Table 2.
Subject characteristics at baseline interview in relation to subsequent injury experience over 2-year follow-up among 492 hospital workers
| Subject characteristics at baseline interview | All subjects (N = 492) |
New or recurrent injury status reported at 2-year follow-up |
|||||
|---|---|---|---|---|---|---|---|
| Yes (N = 175) |
No (N = 317) |
p value | |||||
| N | % | N | % | N | % | ||
| Sex: female | 365 | 74.2 | 142 | 81.1 | 223 | 70.4 | <0.01 |
| Race/ethnicity | 0.02 | ||||||
| White, non-Hispanic | 209 | 42.5 | 62 | 35.4 | 147 | 46.4 | |
| Hispanic | 80 | 16.3 | 27 | 15.4 | 53 | 16.7 | |
| Asian/Pacific Islander | 128 | 26.0 | 48 | 27.4 | 80 | 25.2 | |
| African-American | 46 | 9.4 | 25 | 14.3 | 21 | 6.6 | |
| Other | 29 | 5.9 | 13 | 7.4 | 16 | 5.1 | |
| Job group | 0.23 | ||||||
| Nurse | 193 | 39.2 | 74 | 42.3 | 119 | 37.5 | |
| Other clinical | 70 | 14.2 | 28 | 16.0 | 42 | 13.3 | |
| Clerical | 96 | 19.5 | 38 | 21.7 | 58 | 18.3 | |
| Administrative/professional | 55 | 11.2 | 15 | 8.6 | 40 | 12.6 | |
| Technical | 42 | 8.5 | 11 | 6.3 | 31 | 9.8 | |
| Support staff | 36 | 7.3 | 9 | 5.1 | 27 | 8.5 | |
| Musculoskeletal comorbidity | 225 | 46.0 | 101 | 57.7 | 124 | 39.5 | <0.001 |
| Other medical comorbidity | 183 | 37.3 | 70 | 40.0 | 113 | 35.8 | 0.23 |
| Mean | SD | Mean | SD | Mean | SD | p value | |
|---|---|---|---|---|---|---|---|
| Age (years) | 45.9 | 9.6 | 45.8 | 9.2 | 46.0 | 9.9 | 0.82 |
| Depression (CES-D) | 20.5 | 8.1 | 21.7 | 8.2 | 19.8 | 8.0 | 0.01 |
Musculoskeletal comorbidity includes arthritis, back or neck condition, carpal tunnel syndrome, tendonitis; other medical comorbidity includes asthma, diabetes, high blood pressure, heart disease
CES-D Center for Epidemiologic Studies Depression Scale
Table 3 presents psychosocial factors measured at baseline and their associations with subsequent new or recurrent injury experiences over follow-up examined by multivariable analyses using hierarchical models (see “Methods”). In all models, job control, effort, reward, and ERI consistently showed significant associations with subsequent injury. In Model 4 (controlling for all the studied covariates including age, sex, race/ethnicity, job group, musculoskeletal comorbidity, and CES-D), increased risks of subsequent new or recurrent injury were associated with baseline lower job control (OR 0.78; 95 % CI 0.64–0.96), higher effort (OR 1.24; 95 % CI 1.01–1.51), lower reward (OR 0.80; 95 % CI 0.64–0.98), and higher ERI (OR 1.25; 95 % CI 1.02–1.53). These findings are scaled to indicate that odds of a new or recurrent injury increase about 1.3 times per 1 SD increment of effort and ERI and per 1 SD decrement of job control and reward. Job strain manifested a significant association only in Model 2 controlling for age, sex, race/ethnicity, and job group (OR 1.22; 95 % CI 1.02–1.47).
Table 3.
Psychosocial factors at baseline and subsequent new or recurrent injury experience over 2-year follow-up among hospital workers
| Variable at baseline (range) | New or recurrent injury status reported at 2-year follow-up |
Model 1 | Model 2 | Model 3 | Model 4 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes (n = 175) |
No (n = 317) |
|||||||||||
| Mean | SD | Mean | SD | OR | 95 % CIs | OR | 95 % CIs | OR | 95 % CIs | OR | 95 % CIs | |
| Job demand (12-48) | 35.7 | 6.4 | 35.4 | 6.0 | 1.05 | 0.87-1.27 | 1.10 | 0.91-1.34 | 1.06 | 0.87-1.29 | 1.02 | 0.84-1.25 |
| Job control (24-96) | 68.8 | 9.4 | 72.0 | 10.6 | 0.73** | 0.60-0.88 | 0.74** | 0.61-0.90 | 0.76** | 0.62-0.93 | 0.78* | 0.64-0.96 |
| Job strain (0.125-2.0) | 0.53 | 0.12 | 0.50 | 0.13 | 1.20 | 0.99-1.44 | 1.22* | 1.02-1.47 | 1.17 | 0.97-1.42 | 1.13 | 0.93-1.38 |
| Supervisor support (4-16) | 11.8 | 2.8 | 12.0 | 2.7 | 0.93 | 0.77-1.12 | 0.93 | 0.77-1.13 | 0.95 | 0.78-1.16 | 0.98 | 0.80-1.19 |
| Coworker support (4-16) | 12.3 | 2.2 | 12.5 | 1.9 | 0.93 | 0.78-1.13 | 0.96 | 0.79-1.16 | 0.96 | 0.79-1.17 | 1.00 | 0.82-1.22 |
| Total support (8-32) | 24.1 | 4.3 | 24.4 | 3.9 | 0.92 | 0.76-1.12 | 0.93 | 0.77-1.13 | 0.95 | 0.78-1.16 | 0.99 | 0.81-1.22 |
| Effort (6-30) | 15.9 | 5.0 | 14.7 | 5.1 | 1.27* | 1.05-1.53 | 1.33** | 1.10-1.61 | 1.29* | 1.06-1.56 | 1.24* | 1.01-1.51 |
| Reward (11-55) | 46.7 | 8.4 | 48.8 | 7.2 | 0.77** | 0.64-0.92 | 0.73** | 0.60-0.89 | 0.76** | 0.62-0.92 | 0.80* | 0.64-0.98 |
| Effort-reward ratio (0.2-5.0) | 0.68 | 0.41 | 0.58 | 0.31 | 1.29** | 1.07-1.56 | 1.35** | 1.11-1.64 | 1.31** | 1.07-1.58 | 1.25* | 1.02-1.53 |
| Overcommitment (6-24) | 13.6 | 3.3 | 13.2 | 3.0 | 1.12 | 0.93-1.34 | 1.13 | 0.94-1.37 | 1.11 | 0.91-1.34 | 1.02 | 0.83-1.25 |
To standardize the OR estimates, scores for each scale were divided by its standard deviation (SD) so that the ORs estimate the likelihood of outcome experienced per 1 SD change (see “Methods”)
Model 1: No covariates included in model
Model 2: adjusted for age, sex, race/ethnicity (non-Hispanic white vs. other), and job group (nurse vs. other)
Model 3: adjusted for age, sex, race/ethnicity (non-Hispanic white vs. other), job group (nurse vs. other), and musculoskeletal comorbidity
Model 4: adjusted for age, sex, race/ethnicity (non-Hispanic white vs. other), job group (nurse vs. other), musculoskeletal comorbidity, and CES-D score
p < 0.05
p < 0.01
The associations between baseline musculoskeletal injury and subsequent injury experience also were examined. After controlling for all covariates in Model 4, odds of a new or recurrent injury were two times higher among cases with baseline injury than among referents without baseline injury (OR 1.96; 95 % CI 1.25–3.05, data not shown in table).
Table 4 shows multivariable associations between psychosocial factors and subsequent injury experience, stratified by baseline musculoskeletal injury status in the entire cohort and the two subgroups of nurses and all others. The stratified analyses revealed different patterns of associations by baseline injury status as well as new findings not identified in the main effect analysis presented in Table 3. Job strain and ERI were significantly associated with injury risk only among referents: job strain (OR 1.26; 95 % CI 1.02–1.55) and ERI (OR 1.42; 95 % CI 1.12–1.81). In the subgroup analysis, the point estimates for risk among referents were quite similar to the entire cohort, albeit with wider CIs, statistical significance was observed for ERI among the non-nurse referents (OR 1.42; 95 % CI 1.09– 1.83). More notable differences were observed for total support and overcommitment, which were not significant in the main effect models. For total support, no association was observed in either cases or referents in the entire cohort; however, among the nurse subgroup, increased risk was suggested with greater total support, and the association was significant among referents (OR 1.59; 95 % CI 1.03–2.44). For overcommitment, significant associations with subsequent new or recurrent injury were observed only among cases: The association was nearly double in the nurse subgroup (OR 2.98; 95 % CI 1.01–8.77) than in the entire cohort (OR 1.58; 95 % CI 1.05–2.39), although the estimates had overlapping CIs. In significance testing for interactions between the predictor variables and baseline injury status, only overcommitment demonstrated a marginally significant interaction effect in the entire cohort (p = 0.06) and a significant interaction in the nurse sub group (p = 0.035). None of the other factors tested manifested significant statistical interactions.
Table 4.
Stratified analysis by baseline musculoskeletal injury status (cases vs. referents) and job group (nurses vs. others): multivariable associations of psychosocial factors at baseline interview with subsequent new or recurrent injury over 2-year follow-up among 492 hospital workers
| Variable at baseline | All employees (n = 492) |
Nurses (n = 193) |
Others (n = 299) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases at baseline (N = 174) |
Referents (N = 317) |
Cases at baseline (N = 43) |
Referents (N = 150) |
Cases at baseline (N = 73) |
Referents (N = 226) |
|||||||
| OR | 95 % CI | OR | 95 % CI | OR | 95 % CI | OR | 95 % CI | OR | 95 % CI | OR | 95 % CI | |
| Job strain | 0.89 | 0.56-1.41 | 1.26* | 1.02-1.55 | 1.17 | 0.48-2.81 | 1.26 | 0.81-1.97 | 0.81 | 0.46-1.41 | 1.27 | 0.99-1.61 |
| Effort-reward imbalance | 1.04 | 0.72-1.50 | 1.42** | 1.12-1.81 | 0.80 | 0.42-1.52 | 1.67 | 0.91-3.08 | 1.23 | 0.76-1.98 | 1.42** | 1.09-1.83 |
| Total support | 0.95 | 0.66-1.37 | 0.97 | 0.77-1.22 | 1.36 | 0.63-2.93 | 1.59* | 1.03-2.44 | 0.86 | 0.55-1.33 | 0.76 | 0.57-1.03 |
| Overcommitment | 1.58* | 1.05-2.39 | 1.01 | 0.81-1.26 | 2.98* | 1.01-8.77 | 0.91 | 0.61-1.36 | 1.38 | 0.88-2.16 | 1.08 | 0.82-1.42 |
All multiple logistic regression models include age, sex, and race/ethnicity (non-Hispanic white vs. other); to standardize the OR estimates, scores for job strain, effort-reward imbalance, total support, and overcommitment were divided by its standard deviation (SD) so that the ORs estimate the likelihood of outcome experienced per 1 SD change (see “Methods”). Due to missing data, the sample size for each data analysis varies
p < 0.05
p < 0.01
Discussion
This study examined the effects of psychosocial factors on subsequent injury experience at work and the interactions of such factors with previous musculoskeletal injury in a prospective sample of hospital workers. As anticipated, we found that having a musculoskeletal injury and experiencing negative psychosocial factors at baseline were both significantly associated with increased risk of subsequent new or recurrent injury over follow-up. We also observed variable associations between psychosocial factors and prospective injury risk depending on the presence or absence of previous injury. Job strain and ERI were significant risk factors for new injuries only among workers without a previous injury. Overcommitment emerged as a signifi-cant risk factor only among workers with a previous injury, especially among nurses.
Our cohort manifested a high incidence of work-related injury, particularly among workers with a musculoskeletal injury at baseline, with over 50 % experiencing a subsequent injury over the 2-year follow-up period. Such workers had twofold increased odds of subsequent injury compared to workers without a baseline musculoskeletal injury. We found that such increased risk was independent of a history of musculoskeletal comorbidity, which was also a signifi-cant independent risk factor for injury. Our findings are consistent with reports from previous studies, indicating that the risk of work-related injury can be augmented by an earlier injury (Bergstrom et al. 2007; Keeney et al. 2013; Lipscomb et al. 2008). Our findings also suggest that normal and healthy musculoskeletal functioning is important in preventing injury. They further indicate the need for concentrated case management for workers with musculoskeletal injury and comorbidities to reduce the risk of subsequent injury.
In terms of psychosocial factors and their interactions with previous injury, job strain and ERI were particularly noteworthy for new injury risk among workers without a baseline injury. Also, for job strain, we found that job control may play a more important role in injury risk. Our findings indicating the negative impact of job stress are consistent with evidence from recent systemic review reports (Koch et al. 2014; Kraatz et al. 2013). Kraatz et al. (2013) reviewed 18 prospective studies and reported that strong evidence was found for an incremental effect of job strain on the development of neck or shoulder disorders. Koch et al. (2014) reviewed studies on ERI and musculoskeletal pain and reported finding a moderate level of evidence supporting their significant association; these researchers particularly addressed the need for more longitudinal studies, noting that evidence largely relied on cross-sectional studies (15 out of 19 in total). Our findings from the prospective design contribute to this existing literature.
On the other hand, for workers with a previous injury, we found that job strain and ERI were not significant risk factors for subsequent injury. Of note, however, overcommitment was associated with increased risk of subsequent injury for those workers. Moreover, among psychosocial factors examined, overcommitment presented the largest detrimental effect (OR 2.98) in the nurse subgroup with a previous injury. These findings suggest that an individual's overcommitted work style or overcommitting responses to stressful job conditions may play an important role in increasing the risk of new or recurrent injury particularly for workers with previous injuries. In the review by Koch et al. (2014) previously cited, four out of eight cross-sectional studies found significant associations between over-commitment and musculoskeletal pain, leading the authors to conclude that the evidence was inconclusive. In a prospective study by Huysmans et al. (2012), overcommitment was shown to be significantly associated with increased risk of musculoskeletal pain among office workers. Our prospective study adds evidence supporting increased risk of subsequent injury associated with overcommitment in certain subgroups that may be especially vulnerable.
Interestingly, total support from supervisors and coworkers was not significant in the total sample, but a significant association with this factor in an unexpected direction was observed in the nurse subgroup. This differs from overall evidence in the literature, which otherwise argues that higher support is a protective factor for general or musculoskeletal health (Griep et al. 2011; Kraatz et al. 2013; Solidaki et al. 2010, 2013). Our finding for nurses might be a chance observation, but it may be that nurses who feel more support at work may take more risks or may be more willing to do physically challenging tasks. For example, when patient lift equipment is not readily available but coworkers are friendly and available to help perform a patient handling task, a nurse may not wait for the equipment but rather perform manual handling, especially when working under time pressure or motivated to help a patient in discomfort. This mechanism of perceived support, if operative, could put these workers at risk of injury. If this is indeed the case, this finding may indicate the importance of nursing-targeted safety training to ensure safe work practices.
Our study has the strength of a prospective analysis. It also has limitations that should be acknowledged when interpreting its findings. First, this study relied on self-report for subsequent injury (although baseline injury was based on clinical case reports), and thus, the findings are subject to potential reporting and recall biases. Second, for the outcome variable, we do not have specific information on the type and body part of subsequent injuries. Further, subsequent injury among the previously injured subsumes aggravation of the previous event or, potentially, an entirely new trauma. Thus, this is likely to include a heterogeneous range of injury mechanisms and outcomes including different types of injuries as well as symptoms. Third, more severe injuries that might have led to work cessation would not have been included in this analysis of those still working at the same hospitals at follow-up. This could lead to underestimation of risk of subsequent injury. Finally, our sample size is relatively small, limiting study power to identify certain associations, particularly within substrata of the cohort.
In conclusion, our findings highlight the impacts of negative psychosocial work factors on injury risk among hospital workers, taking into account previous musculoskeletal injuries that carry risk of their own. Moreover, the effects of psychosocial work factors on subsequent new or recurrent injury risk appear to differ by previous injury experience. Workplace injury prevention programs should consider both organizational and individual factors that affect the psychosocial work environment of hospital staff, in particular job strain, effort–reward imbalance, and overcommitment. Different preventive strategies may be necessary depending on the previous injury status of injured hospital employees.
Acknowledgments
The parent GROW study was funded by the US National Institute of Health, National Institute for Arthritis, Musculo-skeletal and Skin Diseases (R01 AR47798). This study of secondary data analysis had no funding sources.
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
Contributor Information
Soo-Jeong Lee, University of California, San Francisco, San Francisco, CA, USA.
Doohee You, University of California, Berkeley, Berkeley, CA, USA.
Marion Gillen, University of California, San Francisco, San Francisco, CA, USA.
Paul D. Blanc, University of California, San Francisco, San Francisco, CA, USA
References
- Andersen LL, Burdorf A, Fallentin N, Persson R, Jakobsen MD, Mortensen OS, Clausen T, Holtermann A. Patient transfers and assistive devices: prospective cohort study on the risk for occupational back injury among healthcare workers. Scand J Work Environ Health. 2014;40:74–81. doi: 10.5271/sjweh.3382. doi:10.5271/sjweh.3382. [DOI] [PubMed] [Google Scholar]
- Bergstrom G, Bodin L, Bertilsson H, Jensen IB. Risk factors for new episodes of sick leave due to neck or back pain in a working population. A prospective study with an 18-month and a three-year follow-up. Occup Environ Med. 2007;64:279–287. doi: 10.1136/oem.2006.026583. doi:10.1136/oem.2006.026583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgel BJ, White MC, Gillen M, Krause N. Psychosocial work factors and shoulder pain in hotel room cleaners. Am J Ind Med. 2010;53:743–756. doi: 10.1002/ajim.20832. doi:10.1002/ajim.20832. [DOI] [PubMed] [Google Scholar]
- Carleton RN, Thibodeau MA, Teale MJ, Welch PG, Abrams MP, Robinson T, Asmundson GJ. The center for epidemiologic studies depression scale: a review with a theoretical and empirical examination of item content and factor structure. PLoS One. 2013;8:e58067. doi: 10.1371/journal.pone.0058067. doi:10.1371/journal.pone.0058067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen JO, Knardahl S. Time-course of occupational psychological and social factors as predictors of new-onset and persistent neck pain: a three-wave prospective study over 4 years. Pain. 2014;155:1262–1271. doi: 10.1016/j.pain.2014.03.021. doi:10.1016/j.pain.2014.03.021. [DOI] [PubMed] [Google Scholar]
- European Commission Occupational health and safety risks in the healthcare sector—guide to prevention and good practice. [18 Aug 2014];Publications Office of the European Union. 2011 https://osha.europa.eu/en/legislation/guidelines/sector_specific/occupational-health-and-safety-risks-in-the-healthcare-sector-guide-to-prevention-and-good-practice.
- Gillen M, Yen IH, Trupin L, Swig L, Rugulies R, Mullen K, et al. The association of socioeconomic status and psychosocial and physical workplace factors with musculoskeletal injury in hospital workers. Am J Ind Med. 2007;50:245–260. doi: 10.1002/ajim.20429. doi:10.1002/ajim.20429. [DOI] [PubMed] [Google Scholar]
- Gillen M, Cisternas MG, Yen IH, Swig L, Rugulies R, Frank J, Blanc PD. Functional recovery following musculoskeletal injury in hospital workers. Occup Med (Lond) 2010;60:532–539. doi: 10.1093/occmed/kqq110. doi:10.1093/occmed/kqq110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griep RH, Rotenberg L, Landsbergis P, Vasconcellos-Silva PR. Combined use of job stress models and self-rated health in nursing. Revista de Saúde Pública. 2011;45:145–152. doi: 10.1590/s0034-89102011000100017. [DOI] [PubMed] [Google Scholar]
- Hammond WP, Gillen M, Yen IH. Workplace discrimination and depressive symptoms: a study of multi-ethnic hospital employees. Race Soc Probl. 2010;2(1):19–30. doi: 10.1007/s12552-010-9024-0. doi:10.1007/s12552-010-9024-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannan LM, Monteilh CP, Gerr F, Kleinbaum DG, Marcus M. Job strain and risk of musculoskeletal symptoms among a prospective cohort of occupational computer users. Scand J Work Environ Health. 2005;31:375–386. doi: 10.5271/sjweh.921. [DOI] [PubMed] [Google Scholar]
- Herin F, Paris C, Levant A, Vignaud MC, Sobaszek A, Soulat JM, Orsosa group Links between nurses’ organisational work environment and upper limb musculoskeletal symptoms: independently of effort–reward imbalance! The ORSOSA study. Pain. 2011;152:2006–2015. doi: 10.1016/j.pain.2011.04.018. doi:10.1016/j.pain.2011.04.018. [DOI] [PubMed] [Google Scholar]
- Huysmans MA, Ijmker S, Blatter BM, Knol DL, van Mechelen W, Bongers PM, van der Beek AJ. The relative contribution of work exposure, leisure time exposure, and individual characteristics in the onset of arm-wrist-hand and neck-shoulder symptoms among office workers. Int Arch Occup Environ Health. 2012;85:651–666. doi: 10.1007/s00420-011-0717-5. doi:10.1007/s00420-011-0717-5. [DOI] [PubMed] [Google Scholar]
- Joksimovic L, Starke D, vd Knesebeck O, Siegrist J. Perceived work stress, overcommitment, and self-reported musculoskeletal pain: a cross-sectional investigation. Int J Behav Med. 2002;9:122–138. doi: 10.1207/s15327558ijbm0902_04. [DOI] [PubMed] [Google Scholar]
- Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3:322–355. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- Keeney BJ, Turner JA, Fulton-Kehoe D, Wickizer TM, Chan KC, Franklin GM. Early predictors of occupational back reinjury: results from a prospective study of workers in Washington State. Spine (Phila Pa 1976) 2013;38:178–187. doi: 10.1097/BRS.0b013e318266187d. doi:10.1097/BRS.0b013e318266187d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koch P, Schablon A, Latza U, Nienhaus A. Musculoskeletal pain and effort–reward imbalance: a systematic review. BMC Public Health. 2014;14:37. doi: 10.1186/1471-2458-14-37. doi:10.1186/1471-2458-14-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraatz S, Lang J, Kraus T, Munster E, Ochsmann E. The incremental effect of psychosocial workplace factors on the development of neck and shoulder disorders: a systematic review of longitudinal studies. Int Arch Occup Environ Health. 2013;86:375–395. doi: 10.1007/s00420-013-0848-y. doi:10.1007/s00420-013-0848-y. [DOI] [PubMed] [Google Scholar]
- Lee SJ, Lee JH, Gillen M, Krause N. Job stress and work-related musculoskeletal symptoms among intensive care unit nurses: a comparison between job demand-control and effort–reward imbalance models. Am J Ind Med. 2014;57:214–221. doi: 10.1002/ajim.22274. doi:10.1002/ajim.22274. [DOI] [PubMed] [Google Scholar]
- Leka S, Jain A. Health impact of psychosocial hazards at work: an overview. World Health Organization; Geneva: 2010. [18 Aug 2014]. http://www.who.int/occupational_health/publications/hazardpsychosocial/en/. [Google Scholar]
- Lipscomb HJ, Cameron W, Silverstein B. Incident and recurrent back injuries among union carpenters. Occup Environ Med. 2008;65:827–834. doi: 10.1136/oem.2008.039222. doi:10.1136/oem.2008.039222. [DOI] [PubMed] [Google Scholar]
- Radloff LS. A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- Rugulies R, Krause N. Job strain, iso-strain, and the incidence of low back and neck injuries. A 7.5-year prospective study of San Francisco transit operators. Soc Sci Med. 2005;61:27–39. doi: 10.1016/j.socscimed.2004.11.042. doi:10.1016/j.socscimed.2004.11.042. [DOI] [PubMed] [Google Scholar]
- Rugulies R, Krause N. Effort–reward imbalance and incidence of low back and neck injuries in San Francisco transit operators. Occup Environ Med. 2008;65:525–533. doi: 10.1136/oem.2007.035188. doi:10.1136/oem.2007.035188. [DOI] [PubMed] [Google Scholar]
- Rugulies R, Braff J, Frank JW, Aust B, Gillen M, Yen IH, et al. The psychosocial work environment and musculoskeletal disorders: design of a comprehensive interviewer-administered questionnaire. Am J Ind Med. 2004;45(5):428–439. doi: 10.1002/ajim.20009. doi:10.1002/ajim.20009. [DOI] [PubMed] [Google Scholar]
- Schoenfisch AL, Lipscomb HJ. Job characteristics and work organization factors associated with patient-handling injury among nursing personnel. Work. 2009;33:117–128. doi: 10.3233/WOR-2009-0847. doi:10.3233/WOR-2009-0847. [DOI] [PubMed] [Google Scholar]
- Siegrist J, Starke D, Chandola T, Godin I, Marmot M, Niedhammer I, Peter R. The measurement of effort–reward imbalance at work: European comparisons. Soc Sci Med. 2004;58:1483–1499. doi: 10.1016/S0277-9536(03)00351-4. doi:10.1016/S0277-9536(03)00351-4. [DOI] [PubMed] [Google Scholar]
- Solidaki E, Chatzi L, Bitsios P, Markatzi I, Plana E, Castro F, et al. Work-related and psychological determinants of multisite musculoskeletal pain. Scand J Work Environ Health. 2010;36:54–61. doi: 10.5271/sjweh.2884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solidaki E, Chatzi L, Bitsios P, Coggon D, Palmer KT, Kogevinas M. Risk factors for new onset and persistence of multi-site musculoskeletal pain in a longitudinal study of workers in Crete. Occup Environ Med. 2013;70:29–34. doi: 10.1136/oemed-2012-100689. doi:10.1136/oemed-2012-100689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Bureau of Labor Statistics [18 Aug 2014];Incidence rates and numbers of nonfatal occupational injuries by selected industries and ownership, 2012. 2013a http://www.bls.gov/news.release/osh.t05.htm.
- U.S. Bureau of Labor Statistics [18 Aug 2014];Nonfatal occupational injuries and illnesses requiring days away from work, 2012. 2013b http://www.bls.gov/news.release/osh2.nr0.htm.
- U.S. Bureau of Labor Statistics [18 Aug 2014];Quarterly census of employment and wages. 2014 http://www.bls.gov/cew/apps/data_views/data_views.htm.
- Workers’ Compensation Board of British Columbia [18 Aug 2014];WorkSafe BC 2012 statistics. 2013 http://www.worksafebc.com/publications/reports/statistics_reports/.