Abstracts
Sickle cell disease (SCD), a genetic disorder often reported late, can be identified early in life, and hot-spot areas may be identified to conduct genetic epidemiology studies. This study was undertaken to estimate prevalence and to identify hot spot area for SCD in Kalahandi district, by screening cord blood of neonates delivered at the district hospital as first-hand information. Kalahandi District Hospital selected for the study is predominated by tribal population with higher prevalence of SCD as compared to other parts of Odisha. Cord blood screening of SCD was carried out on 761 newborn samples of which 13 were screened to be homozygous for SCD. Information on area of parent’s residence was also collected. Madanpur Rampur area was found to be with the highest prevalence of SCD (10.52 %) and the gene distribution did not follow Hardy-Weinberg Equation indicating un-natural selection. The approach of conducting neonatal screening in a district hospital for identification of SCD is feasible and appropriate for prioritizing area for the implementation of large-scale screening and planning control measures thereof.
Keywords: Cord blood screening, Sickle cell, Area specific, District hospital
Introduction
Study of genetic epidemiology has been a great challenge specifically in India with huge amount of genetic heterogeneity (Bittles 2002). Reason for this heterogeneity is diverse population structures, culture, and traditions in urban, rural, and tribal populations. This leads to differences in area-specific prevalence of genetic diseases. At the same time, the diverse Indian terrain makes it difficult to study and conduct a screening activity specifically in tribal populations residing at hard-to-reach areas and with variable traditions.
The inherited disorders of hemoglobin like sickle cell and β-thalassemia are the commonest monogenic disorders causing major health problem. With a population of over 1.25 billion individuals, it is estimated that India is home to over 50 % of the world’s sickle cell disease (SCD) patients (Shrikhande et al 2014; Kate and Lingojwar 2002). As per the hospital data, the prevalence of sickle gene is found to be 0–18 % in north eastern India, 0–33.5 % in western India, 22.5–44.4 % in central India, and 1–40 % in southern India (Gorakshakar 2006). Sickle cell is specifically prevalent in some ethnic groups because they have practiced or are practicing endogamy (Shrikhande et al 2014).
The prevalence of sickle cell disease in a community survey was found to be 3.03 % in the State of Odisha (Purohit et al. 2014) and is reported to vary among different populations within Odisha (Balgir 2000; Balgir 2005). This could be due to difference in founder effect, genetic drift, and practice of endogamy (Rudan et al. 2006). Therefore, it is important to identify the population and region of disease prevalence and to study associated risk factors in these regions. The present study is an effort towards this in Kalahandi district where we have tried to make use of “Janani Suraksha Yojana” program run by the Indian government, under which institutional deliveries are promoted, for obtaining information on SCD disease prevalence and to identify nearby hot spots for the disease via cord blood screening method.
Methodology
Selection of study area
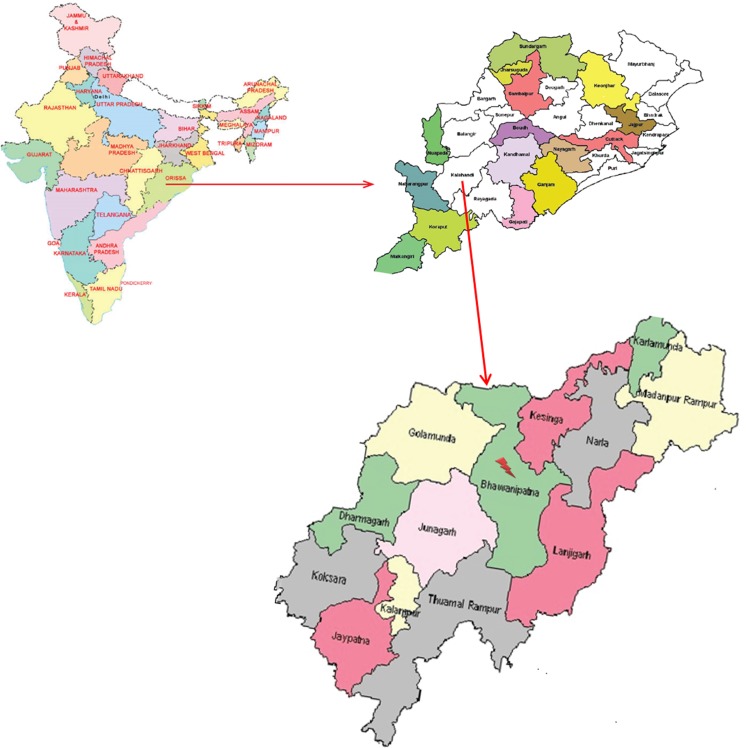
Kalahandi District Hospital was selected for screening of neonates for SCD for two reasons: (1) Kalahandi is a tribal-dominated district with area-specific variation in marriage practices and (2) the district hospital is located at Bhawanipatna town which is the center of Kalahandi district and gets delivery cases from about all the areas (13 different areas) of the district (Fig. 1), although in variable proportions. The district is also under Janani Suraksha Yojana program of the Government of India. The program has been met with successful implementation leading to an increase in district hospital deliveries. This provides us with large sample collection for neonatal screening.
Fig. 1.
Areas of Kalahandi district in the State of Odisha, India
Ethical issues
The study was approved by the institutional ethical committee and was conducted in collaboration with the State Government of Odisha, India. Informed written consent was taken from the parents of all the neonates.
Sample collection
A total of 761 full-term newborns delivered in Kalahandi District Hospital, Bhawanipatna, Kalahandi, from March 2013 to June 2013 were included in this cross-sectional study. From each newborn, 5 ml of venous cord blood was collected under aseptic condition in EDTA vials; cord blood screening was used as it is noninvasive to the newborn. Information on neonate’s sex, weight, and parent’s place of residence, which included complete address with details of area and district, was collected.
Hb variant analysis
Cord blood samples were analyzed for quantification of Hb type by using Hb Variant Classic (Bio-Rad, USA), β-thal short program. Based on the time of elution (retention time), normal or variant hemoglobin was identified.
Results
Overall prevalence of SCD in neonates born at Kalahandi District Hospital
Out of 761 cases, 83.44 % (n = 635) without any abnormal Hb, 14.71 % (n = 112) heterozygous, and 1.7 % (n = 13) homozygous for sickle cell gene were observed among those neonates delivered at Kalahandi District Hospital. Only one (0.13 %) was heterozygous for Hb D. It had been observed that proportion of sickle cell gene was equal in both the sexes.
Identification of hot spots for SCD
Kalahandi district is surrounded by 13 areas, out of which maximum deliveries were from Bhawanipatna area where the hospital is situated followed by Jhunagarh. The rest of the areas received more or less equal number of delivery cases. Ksinga, Narla, and Madanpur Rampur (also known as M. Rampur) was found to have almost equal number of heterozygous cases; however, unlike M. Rampur, there was no case of homozygous SCD in Ksinga and Narla. Homozygous for sickle cell gene was found in three (Bhawanipatna, Jhunagarh, M. Rampur) out of 13 areas studied, and the prevalence was highest in M. Rampur (10.52 %) (Table 1). On calculation of Hardy-Weinberg equilibrium (HWE), it was found that out of all the areas, the sickling gene does not follow HWE inheritance pattern only in M. Rampur. Prevalence of sickle cell disorder varies from 1.71 to 10.52 % in different areas of Kalahandi district (Table 1).
Table 1.
Area-wise distribution of sickle cell gene in Kalahandi district, Odisha, India
| Sl no. | Area | Total (n = 761) | % Normal (n = 635) | % sickle cell trait (n = 112) | % sickle cell disease (n = 13) | 95 % CI of sickle cell trait proportion | 95 % CI of sickle cell disease proportion |
|---|---|---|---|---|---|---|---|
| 1 | Lanjigarh | 8 | 87.5 (n = 7) | 12.5 (n = 1) | 0.02–0.47 | ||
| 2 | Bhawanipatna | 292 | 83.2 (n = 243) | 15.07 (n = 44) | 1.71 (n = 5) | 0.11–0.19 | 0.01–0.03 |
| 3 | Golmunda | 42 | 73.8 (n = 31) | 26.19 (n = 11) | 0.15–0.41 | ||
| 4 | Jhunagarh | 175 | 86.8 (n = 152) | 11.43 (n = 20) | 1.71 (n = 3) | 0.07–0.16 | 0.01–0.04 |
| 5 | Kesinga | 36 | 86.11 (n = 31) | 13.89 (n = 5) | 0.06–0.03 | ||
| 6 | Narla | 27 | 85.18 (n = 23) | 14.81 (n = 4) | 0.05–0.32 | ||
| 7 | Dharmagarh | 20 | 90 (n = 18) | 10.00 (n = 2) | 0.02–0.30 | ||
| 8 | Jaypatna | 42 | 88.09 (n = 37) | 11.90 (n = 5) | 0.05–0.42 | ||
| 9 | Koksara | 28 | 89.28 (n = 25) | 10.71 (n = 3) | 0.03–0.27 | ||
| 10 | Madanpur Rampur | 19 | 68.42 (n = 13) | 15.79 (n = 3) | 10.52 (n = 2) | 0.05–0.37 | 0.02–0.31 |
| 11 | Kalampur | 2 | 100 (n = 2) | ||||
| 12 | Thuamul Rampur | 7 | 85.71 (n = 6) | 14.29 (n = 1) | 0.02–0.51 | ||
| 13 | Karlamunda | 2 | 100 (n = 2) | ||||
| 14 | Other nearby districts | 61 | 73.77 (n = 45) | 21.31 (n = 13) | 4.916 (n = 3) | 0.12–0.33 | 0.01–0.13 |
One sample was positive for Hb D trait and is not included in the table
Discussion
Cord blood screening serves as a good tool to capture genetic disease and its carriers at an early stage and help in prevention and control of disease and morbidity and mortality due to such diseases. Moreover, number of institutional deliveries at Kalahandi District Hospital has tremendously increased with the implementation of Indian Government program of Janani Suraksha Yojana. Wide public acceptance of the program has made it possible to conduct such screening activities.
The present study is carried out in Kalahandi District Hospital of Odisha. The hospital is situated at Bhawanipatana which is placed at the center of the Kalahandi district and is surrounded by six nearest areas (Kesinga, Golmunda, Jhunagarh, Thuamalrampur, Lanjigaarh, Narla). Therefore, hospital delivery cases are usually from these regions and some also from other nearby areas, like Dharmagarh, Jaypatna, Koksara, Madanpur Rampur, Kalampur, and Karlamunda. Since institutional delivery among pregnant women, by Janani Suraksha Yojana program, which aims at reducing maternal and neonatal mortality by promoting institutional deliveries among poor pregnant women, has been promoted and successfully implemented, an increase in institutional delivery cases has been observed (Gupta et al. 2012; Randive et al. 2014). Across region variation in culture, tradition, education level, and marriage practices even within the district has been observed (Ota and Mohanty 2010), which could be the main source and cause for differences in genetic epidemiology. In order to prioritize area for the implementation of genetic disease management and control program, cord blood screening at a district hospital is a good source to get first-hand information on hot-spot areas. Implementation of program in hot-spot areas with known associated risk factors would result in higher impact of control measures. This study was conducted to get overall prevalence and to identify hot-spot regions for SCD gene in tribal-dominated Kalahandi district of Odisha. This knowledge would assist in prioritizing intervention studies like genetic counseling and parental education about disease in these hot-spot areas in order to reduce the morbidity and mortality due to SCD.
In our study, it was found that M. Rampur is the probable hot spot for SCD with 10.52 % homozygous cases. The SCD gene distribution in this region does not follow HWE. This suggests founder effect or endogamy in this region. M. Rampur has a specific tribal population, namely Mirdhas, which prefers marriage between maternal cousins. This tribal population is not found in other areas like Bhawanipatna, Jhunagarh, Golmunda, Narla, Dharmagarh, Kesinga, Koksara, and Jaypatna (Ota and Mohanty 2010). Cross-cousin marriage along with within caste and within community marriage, prominent in Indian culture, could be the reasons for the low rate of gene flow in this population leading to departure from HWE and could be the reason for higher rate of SCD homozygous cases. However, a study on a larger sample is warranted to confirm the findings. This region could, therefore, be prioritized for the implementation of control measures like marriage counseling and prenatal screening for SCD in Odisha. Even though proportion of deliveries at the district hospital from M. Rampur is fewer due to comparatively other closer community health centers (CHC), low manpower and inadequate infrastructure would be an issue for cord blood collection and storage at the CHCs (http://planningcommission.nic.in/aboutus/committee/strgrp/…/sgfw_ch8.pdf/), whereas screening at the district hospital would be possible with available manpower, due to their central location, better infrastructure, and sufficient and trained staff. All these make it more feasible and cost effective to conduct cord blood screening at a district hospital for identifying SCD hot-spot regions.
Although in the present study the population screened varies from one area to another due to the difference in distance from the district hospital, nevertheless, the results suggest that the district hospital cord blood screening can still serve as a good source to identify local hot spots for genetic epidemiology studies.
Acknowledgments
We are grateful to the State Government of Odisha, India, for their permission and unconditional support to conduct the study at Kalahandi District Hospital. Our gratitude also goes to the staff from the Department of Gynecology and Obstetric, District Hospital of Bhawanipatna, Kalahandi, and parents of neonates. We extend our gratitude to Mr. Krushna Chandra Choudhary from Regional Medical Research Centre Field unit, Kalahandi, for coordinating in cord blood collection and transport. This study was funded by the Indian Council of Medical Research, New Delhi, India.
Conflict of interest
The authors have no conflict of interests.
References
- Balgir RS. The spectrum of haemoglobin variants in two scheduled tribes of Sundargarh district in north-western Orissa. India Ann Hum Biol. 2000;32:560–573. doi: 10.1080/03014460500228741. [DOI] [PubMed] [Google Scholar]
- Balgir RS. Spectrum of hemoglobinopathies in the state of Orissa, India: a ten years cohort study. J Assoc Physicians India. 2005;53:1021–1026. [PubMed] [Google Scholar]
- Bittles AH. Endogamy, consanguinity and community genetics. J Genet. 2002;81:91–98. doi: 10.1007/BF02715905. [DOI] [PubMed] [Google Scholar]
- Gorakshakar AC (2006) Epidemiology of sickle hemoglobin in India. Proceedings of the National Symposium on Tribal Health, held at Jabalpur, India, October 19-20. 2006:103–108 (http://www.rmrct.org/files_rmrc_web/centre’s_publications/NSTH_06/NSTH06_14.AC.Gorakshakar.pdf) Accessed 26 December 2014
- Gupta SK, Pal DK, Tiwari R, et al. Impact of Janani Suraksha Yojana on institutional delivery rate and maternal morbidity and mortality: an observational study in India. J Health Popul Nutr. 2012;30:464–471. doi: 10.3329/jhpn.v30i4.13416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kate SL, Lingojwar DP. Epidemiology of sickle cell disorder in the State of Maharashtra. Int J Hum Genet. 2002;2(3):161–167. [Google Scholar]
- Ota AB, Mohanty BN. Population profile of schedule tribes in Odisha. Schedule Caste and Schedule Tribes Research and Training Institute. Bhubaneswar: Government of Odisha; 2010. [Google Scholar]
- Purohit P, Dehury S, Patel S, Patel DK. Prevalence of deletional alpha thalassemia and sickle gene in a tribal dominated malaria endemic area of eastern India. ISRN Hematol. 2014;2014:745245. doi: 10.1155/2014/745245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randive B, San Sebastian M, De Costa A, Lindholm L. Inequalities in institutional delivery uptake and maternal mortality reduction in the context of cash incentive program, Janani Suraksha Yojana: results from nine states in India. Soc Sci Med. 2014;123:1–6. doi: 10.1016/j.socscimed.2014.10.042. [DOI] [PubMed] [Google Scholar]
- Rudan I, Biloglav Z, Vorko-Jović A, Kujundzić-Tiljak M, Stevanović R, Ropac D, Puntarić D, Cucević B, Salzer B, Campbell H. Effects of inbreeding, endogamy, genetic admixture, and outbreeding on human health: a (1001 Dalmatians) study. Croat Med J. 2006;47:601–610. [PMC free article] [PubMed] [Google Scholar]
- Shrikhande AV, Arjunan A, Agarwal A, Dani A, Tijare J, Gettig E, Krishnamurti L. Prevalence of the β(S) gene among scheduled castes, scheduled tribes and other backward class groups in Central India. Hemoglobin. 2014;38(4):230–235. doi: 10.3109/03630269.2014.931287. [DOI] [PubMed] [Google Scholar]