Abstract
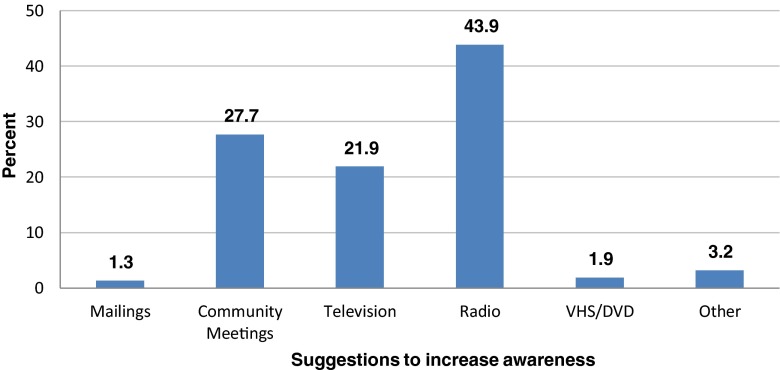
Sickle cell trait (SCT; HbAS), the heterozygous state for the sickle cell allele of the beta globin gene, is carried by as many as 100 million individuals worldwide. Nigeria has the highest prevalence of SCT, impacting an estimated 25 % of adult population. This study was designed to assess timing of awareness, knowledge of SCT status and preferred method of education among parents of children with sickle cell disease (SCD). We conducted a cross-sectional survey of parents of children with SCD from June 2013–March 2014. Participants completed a 20-item questionnaire to assess (1) awareness of personal sickle cell genotype, (2) timing of awareness of personal sickle cell genotype, and (3) knowledge of SCT. One hundred and fifty-five participants completed the survey. Seventy-eight percent were females, and 87 % (135/155) were aware of their own sickle cell genotype. Timing of awareness varied as follows: following birth of a child with sickle cell disease (45 %); during marriage (21.5 %); school admission (9.6 %); during pregnancy (9.6 %); and other times (14 %). Approximately 35.5 % of participants thought that sickle cell trait was a mild form of sickle cell disease. Radio (43.9 %), informational community meetings (27.7 %), and television (21.9 %) were identified by participants as the most effective method of increasing sickle cell trait awareness. Innovative approaches are needed to increase the proportion of individuals who are aware of their own sickle cell genotype prior to having a child with sickle cell anemia in line with the Healthy People 2020 objective.
Electronic supplementary material
The online version of this article (doi:10.1007/s12687-015-0225-5) contains supplementary material, which is available to authorized users.
Keywords: Sickle cell genotype, Sickle cell awareness, Sickle cell knowledge, Nigeria, Cross-sectional survey, Healthy People 2020
Introduction
Sickle cell disease includes a variety of pathologic conditions resulting from inheritance of sickle hemoglobin (Hb) either in a homozygous state (SS) or in a heterozygous state with another abnormal hemoglobin such as SC, Sβthal, SOArab, SD, and SG (Aken’ova 2013). The most common and most severe type is the homozygous state (SS) known as sickle cell anemia (SCA) associated with chronic severe hemolytic anemia and vaso-occlusion (Adekile and Adeodu 2007; Hoffbrand et al. 2001; Martin and Pearson 1997). In addition to medical complications associated with SCA, it is also associated with psychosocial complications (Ola et al. 2013). Globally, it is estimated that about 305,000 newborns are born annually with SCA, and the global burden has been shown to be on the increase (Piel et al. 2013). The increasing number of SCA will continue to have a major impact particularly on healthcare services and financing (Piel et al. 2013).
Sickle cell trait (SCT; HbAS), the heterozygous state for the sickle cell allele of the beta globin gene, is carried by as many as 100 million individuals worldwide including an estimated 2.5 million Americans (National Heart 2012). Although found among all racial groups, individuals of African descent has the highest prevalence (Serjeant 2013; WHO 2006). SCT confers a survival advantage relative to individuals with normal Hb in malaria endemic region where the largest number of individuals with SCT reside (Serjeant 2013). On the other hand, SCT also improves life expectancy relative to SCA (WHO 2006). The prevalence of SCT varies widely from region to region and reaches up to 40 % in parts of West Africa (Serjeant 2013; WHO 2006). In Nigeria, the prevalence SCT is estimated at 24 % (Taiwo et al. 2011; WHO 2006). It is estimated that there are more than 40 million individuals who carry the sickle cell trait in Nigeria and more than 150,000 children born each year with SCA (Galadanci et al. 2014).
Though the frequency of sickle cell trait predicts the prevalence of SCA, awareness and knowledge of sickle cell trait status may help reduce the prevalence of SCA (Ezechukwu and Chukwuka 2004; Nnaji et al. 2013; WHO 2006). It is estimated that a significant proportion of individuals in Nigeria are unaware of their sickle cell genotype prior to marriage (Ezechukwu and Chukwuka 2004). A recent study on the attitudes and awareness of youths in the Yaba Development Area found that 55 % of youths in the age group of 15–19 years old had no exposure to SCA premarital counseling (Oludare and Ogili 2013). This same group also scored lowest in SCA knowledge and had the highest rate of negative attitudes towards SCA (Oludare and Ogili 2013).
Despite the high prevalence of both SCT and SCA in Nigeria, there is no universal newborn screening program and no uniform premarital testing for sickle cell genotype, which results in children with sickle cell disease being identified during an illness when their genotype is performed based on clinical suspicion. In most cases, this is also the time when the genotype of their parents is obtained. There is a paucity of data on the awareness of SCT status in parents of children with SCA. Studies from Nigeria assessed the SCT awareness in unmarried general population (Nnaji et al. 2013; Oludare and Ogili 2013).
Increasing the proportion of individuals who are aware of their sickle cell genotype is a stated priority of the Healthy People 2020 objectives and the World Health Organization’s 2006 sickle cell resolution (USDHHS 2013; WHO 2006). Current modeling projects a 50 % increase over present levels of annual SCA births in Nigeria by the year 2050 (Piel et al. 2013). This dramatic projection indicates the need to identify methods to increase awareness and education levels related to SCT and SCA. The most appropriate time for individuals to become aware of their sickle cell genotype is not well described. Although universal newborn screening for sickle cell genotype has been in place in the USA, a recent study showed that a significant proportion of adolescents are unaware of their sickle cell genotype (Chandnani et al. 2013). A recent survey of Nigerian physicians living in the USA indicates that most would recommend individuals become aware of their own genotype prior to marriage (Shahani et al. 2013). This same cohort of participants indicates that individuals with sickle cell anemia should be identified as soon after birth as possible. This study was designed to assess the knowledge, timing of awareness of SCT status among parents of children with SCA and determine preference among participants on the best method of sickle cell education. We hypothesize that a majority of participants would become aware of their own genotype only following the birth of their child with sickle cell anemia.
Subjects and methods
Setting, design, and study population
A cross-sectional survey of parents attending the sickle cell clinic at the University of Nigeria Teaching Hospital (UNTH), Enugu.
Participant recruitment, inclusion, and exclusion criteria
All parents of children with SCA attending the Sickle Cell Clinic of UNTH over the study period and who consented to study were recruited consecutively. Non-biologic parents or caregivers of children with sickle cell anemia were excluded.
Study procedure
Parents attending clinic were approached to participate in the study. Study purpose was explained to parents in their preferred language of English or local Nigerian language. Following explanations, written informed consent was obtained from all participants prior to completing survey. The investigators then administered a structured questionnaire designed to obtain demographic information including parental education, occupation, and religion. Questionnaire also sought sickle cell-specific information including awareness of genotype, time of awareness, and perception of SCT and SCA.
Statistical analysis
Statistical analysis was performed using SPSS statistical program version 22 (IBM Corp Released 2013). Chi-square test was used to compare frequencies and to test the association between differences in proportion, whereas Pearson’s correlation coefficient was employed to test the relationship between two numerical variables. The level of significance was set as p < 0.05. The knowledge scores were summed on a binary basis with 1 point being assigned for a correct answer and 0 being given for an incorrect response. Scores of 3–6 was considered a low to average sickle cell trait knowledge, while scores of 7 and 8 were considered to be an indicator of high sickle cell trait knowledge. Multivariate analysis was performed to identify predictors of knowledge. The study protocol was approved by the UNTH Health Research Ethics Committee.
Results
Participant characteristics
A total of 273 children with SCA attended the sickle cell clinic during the study period. One hundred fifty-five (155) parents were approached to participate in the study, and all completed the survey for a response rate of 100 %. The remaining 118 were non-biologic parents, caregivers, or adolescents who attended alone and these were all excluded. Table 1 details the characteristics of the study population. Each survey was completed by one member of a married couple with over three-quarters (78.1 %) of the responses coming from females and 21.9 % were completed by males. The mean age of the respondents was 39.2 years with a median of 38 years. Approximately three-fourths (76.1 %) of the subjects had a secondary or higher education. Participants completing the survey were generally working adults with 85.2 % reporting their status as employed or self-employed. The vast majority (98.7 %) of respondents identified their faith as being of Christian denomination.
Table 1.
Participant characteristics
| Characteristic | Informant N = 155 | Spouse N = 155 | ||
|---|---|---|---|---|
| Number | Percent | Number | Percent | |
| Sex | ||||
| Male | 34 | 21.9 | 121 | 78.1 |
| Female | 121 | 78.1 | 34 | 21.9 |
| Age | ||||
| 23–29 | 21 | 13.5 | 9 | 5.8 |
| 30–39 | 68 | 43.9 | 45 | 29.0 |
| 40–49 | 46 | 29.7 | 55 | 35.5 |
| 50–59 | 14 | 9.0 | 40 | 25.8 |
| 60–69 | 6 | 3.9 | 6 | 3.9 |
| Education level | ||||
| None | 2 | 1.3 | 3 | 1.9 |
| Primary | 35 | 22.6 | 40 | 25.8 |
| Secondary | 63 | 40.6 | 62 | 40.0 |
| Tertiary | 55 | 35.5 | 50 | 32.3 |
| Employment status | ||||
| Employed | 66 | 42.6 | 60 | 38.7 |
| Self-employed | 66 | 42.6 | 85 | 54.8 |
| Unemployed | 21 | 13.5 | 9 | 5.8 |
| Retired | 2 | 1.3 | 1 | 0.6 |
| Religion | ||||
| Christian | 153 | 98.7 | 152 | 98.1 |
| Muslim | 2 | 1.3 | 3 | 1.9 |
Awareness of SCT genotype
Among the 155 respondents, 135 (87.1 %) were aware of their sickle cell trait. Participants that were aware of their trait status had two follow-up questions as shown on Table 2. The first asked respondents to identify their trait. While no subject self-identified as having sickle cell disease, the overwhelming majority (99.3 %) reported having an AS genotype. A majority of respondents (45.2 %) became aware of their own sickle cell genotype following the birth of a child with sickle cell disease. Marriage (21.5 %) was the next most common response. Marriage, pregnancy, and birth of a child with SCA combined for over three-quarters (76.3 %) of the events at which respondents became aware of their genotype.
Table 2.
Awareness of SCT genotype
| Characteristic | Informant N = 155 | Spouse N = 155 | ||
|---|---|---|---|---|
| Number | Percent | Number | Percent | |
| Aware | ||||
| Yes | 135 | 87.1 | 128 | 82.3 |
| No | 20 | 12.9 | 27 | 17.4 |
| If yes, what | ||||
| AA | 1 | 0.7 | 5 | 3.9 |
| AS | 134 | 99.3 | 122 | 95.3 |
| SS | 0 | 0.0 | 1 | 0.8 |
| Time of awareness | ||||
| Knowledge sake | 17 | 12.6 | 11 | 8.6 |
| School admission | 13 | 9.6 | 3 | 2.3 |
| Employment | 1 | 0.7 | 4 | 3.1 |
| Marriage | 29 | 21.5 | 33 | 25.8 |
| Child with SS | 61 | 45.2 | 72 | 56.3 |
| Pregnancy | 13 | 9.6 | 4 | 3.1 |
| Other | 1 | 0.7 | 1 | 0.8 |
SCT knowledge scores
Responses to specific knowledge on sickle cell are shown on Table 3. A significant proportion of respondents (35.5 %) thought sickle cell trait is a mild form of sickle cell disease. Almost 40 % of respondents misidentified the proportion of Nigerians with sickle cell trait and the probability of having a child with sickle cell anemia when two parents have the sickle cell trait. Participants with tertiary education were significantly more likely to score high on the knowledge score (74.5 %) compared to individuals with lower education (53 %). Men also had significantly higher knowledge score (74.5 %) compared to women (56.2 %).
Table 3.
Sickle cell trait knowledge scores
| Question | Correct | Incorrect | Percentage correct |
|---|---|---|---|
| How does someone get SCT | 193 | 16 | 89.7 |
| To inherit sickle cell disease, both parents must have at least one sickle cell gene | 152 | 3 | 98.1 |
| Blood testing can confirm sickle cell trait | 153 | 2 | 98.7 |
| It is important to know if you have sickle cell trait even if asymptomatic | 153 | 2 | 98.7 |
| Sickle cell trait is a mild form of sickle cell disease | 100 | 55 | 64.5 |
| People with sickle cell trait have symptoms of sickle cell disease | 128 | 27 | 82.6 |
| 1 in 4 Nigerians have sickle cell trait | 94 | 61 | 60.6 |
| If both parents have sickle cell trait, there is a 25 % chance the child will have sickle cell disease | 94 | 61 | 60.6 |
Predictors of knowledge score
The timing of the awareness was a statistically significant (p = 0.012) predictor of a respondent having a high knowledge score, in that individuals who discovered their sickle cell trait after the birth of a child with sickle cell disease were almost two and a half times (odds ratio (OR) 2.493) as likely to have a score indicating high knowledge in comparison to individuals who discovered their sickle cell trait prior to the birth of a child (Table 4).
Table 4.
Predictors of knowledge score
| Low to average knowledge score (3–6) | High knowledge score (7–8) | Total | Pearson’s (p value) | Odds ratio | 95 % CI lower | 95 % CI upper | |||
|---|---|---|---|---|---|---|---|---|---|
| Number | Percent | Number | Percent | ||||||
| Sex | |||||||||
| Male | 13 | 38.2 | 21 | 61.8 | 34 | 0.336 | 1.198 | 0.648 | 2.214 |
| Female | 53 | 43.8 | 68 | 56.2 | 121 | (0.695) | 0.951 | 0.806 | 1.123 |
| Age | |||||||||
| <40 | 37 | 41.6 | 52 | 58.4 | 89 | 0.087 | 1.042 | 0.791 | 1.374 |
| ≥40 | 29 | 43.9 | 37 | 56.1 | 66 | (0.870) | 0.946 | 0.655 | 1.366 |
| Education | |||||||||
| Less than university | 48 | 48.0 | 52 | 52.0 | 100 | 3.385 | 0.803 | 0.639 | 1.010 |
| University or 1 greater | 18 | 32.7 | 37 | 67.3 | 55 | (0.089) | 1.524 | 0.958 | 2.426 |
| Timing of awareness | 2.493 | 1.259 | 4.934 | ||||||
| After birth of SS child | 18 | 29.5 | 43 | 70.5 | 61 | 7.030 | 1.772 | 1.131 | 2.775 |
| Pregnancy or before | 48 | 51.1 | 46 | 48.9 | 94 | (0.012) | 0.711 | 0.554 | 0.912 |
SCT increasing awareness
Figure 1 describes the responses given by respondents when asked to identify the best outreach method for increasing sickle cell trait awareness in the population. A majority of respondents (44 %) suggested that public education using radios would be the most effective method of education followed by 27.7 % who identified community meetings as a potential effective method of education.
Fig. 1.
Suggestions for increasing SCT awareness
Discussion
Findings from this study indicate that a majority of parents in this cohort became aware of their own sickle cell genotype following the birth of a child with sickle cell anemia. The mean age of 39.2 years is higher than the mean age of 23.35 years documented in another study in Nigeria (Oludare and Ogili 2013). This was not unexpected as the study participants were unmarried youths compared to current study among married adults.
A higher proportion of respondents in this study was aware and correctly identified their genotype in comparison to only 55 % awareness among respondents in a recent study in the same population (Galadanci et al. 2014). However, the study was conducted among all mothers and not specifically mothers who have a child with sickle cell anemia. It is not surprising that mothers without children with SCA are less likely to know their genotype than those with such children. As we hypothesized, the birth of a child was the most common event at which participants became aware of their own sickle cell trait carrier status. Earlier awareness of the sickle cell genotype could provide information to make decisions about potential partners who also have the sickle cell trait and could prevent the birth of a child with SCA following the modeling proposed by Piel et al. (2013). Although no specific time has been identified for individuals to become aware of their sickle cell genotype, consensus seems to be that this should occur before marriage (Ezechukwu and Chukwuka 2004; Nnaji et al. 2013; Taiwo et al. 2011). Some investigators advocate that this should occur during adolescent to provide information early enough in relationship to make procreational descisions (Oludare and Ogili 2013). Studies have shown that latter awareness of genotype has led to cancellation of marriages with associated societal consequences (Nnaji et al. 2013; Taiwo et al. 2011).
A recent study found that participants recommended more public enlightenment campaign on sickle cell using processes such as media, social media, internet, schools, churches, outreaches, and seminars (Oludare and Ogili 2013). This is similar to findings in this study where respondents identified radio as the most effective method of increasing sickle cell trait awareness. Other suggested modes were informational meetings in the community and television.
A significant proportion of respondents (35.5 %) in this study thought sickle cell trait is a mild form of sickle cell disease which is similar to other studies that has identified significant misunderstanding about sickle cell trait indicating the need for identification of innovative and effective approaches to increase public awareness and knowledge of sickle cell trait and anemia (Acharya et al. 2009).
Findings from this study also identified educational level (tertiary education) and gender (male sex) as predictors for higher knowledge of sickle cell trait. It is noteworthy in this study that parents who discovered their sickle cell trait status after the birth of a child with SCA were more likely to exhibit high knowledge compared to those who discovered their trait prior to the birth of a child with SCA. A plausible explanation could be that individuals who became aware of their sickle cell trait after their child was born had this discovery made at a medical facility (probably during child’s ill health or admission) where educators/healthcare givers were able to sit down with the family and provide a detailed explanation of sickle cell trait and SCA. This underscores the importance of education and genetic counseling in improving knowledge of sickle cell trait and SCA. This improved knowledge following education and genetic counseling has been demonstrated in other studies (WHO 2006).
Our study has limitations. It is a single site study and as such has limited generalizability although other studies have shown similar low awareness and knowledge of sickle cell in Nigeria (Alao et al. 2009; Ezechukwu and Chukwuka 2004; Olakunle et al. 2013; Owolabi et al. 2011). It is plausible that community-based interventions as recommended by participants will increase awareness and knowledge of sickle cell, the feasibility, effectiveness and cost-effectiveness of such interventions have not been proven.
A majority of parents of children with sickle cell disease became aware of their own genotype after the birth of their child. Innovative approaches are needed to translate available evidence-based interventions to sustainable community-based programs in order to realize the Healthy People 2020 goal of increased awareness and knowledge among individuals with hemoglobinopathies.
Electronic supplementary material
(DOCX 14 kb)
(DOCX 16 kb)
Acknowledgments
The study was partially supported by the HealthySunrise Foundation. The funding agency played no role in the study conception, design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author, Dr. Ezeanolue, had full access to all the data in the study and had final responsibility for the decision to submit for publication. The authors are grateful to staff members at the Pediatrics Clinic, University of Nigeria College of Medicine, who assisted with the identification of potential participants.
Compliance with ethics guidelines
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all patients for being included in the study.
Conflict of interest
Osita Ezenwosu, Bartholomew Chukwu, Anthony Ikefuna, Aaron Hunt, Justin Keane, Ifeoma Emodi, and Echezona Ezeanolue declare that they have no conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Acharya K, Lang CW, Ross LF. A pilot study to explore knowledge, attitudes, and beliefs about sickle cell trait and disease. J Natl Med Assoc. 2009;101:1163–1172. doi: 10.1016/s0027-9684(15)31113-5. [DOI] [PubMed] [Google Scholar]
- Adekile A, Adeodu O. Haemoglobinopathies. In: Azubuike J, Nkanginieme K, editors. Textbook of paediatrics and child health in a tropical region. 2. Owerri: African Educational Services; 2007. pp. 373–390. [Google Scholar]
- Aken’ova Y (2013) Distribution of sickle cell disease in Africa. Dokita, University College Hospital, Ibadan, Nigeria
- Alao OO, Araoye M, Ojabo C. Knowledge of sickle cell disease and haemoglobin electrophoresis: a survey of students of a tertiary institution. Niger J Med. 2009;18:326–329. doi: 10.4314/njm.v18i3.51208. [DOI] [PubMed] [Google Scholar]
- Chandnani HK, Zargar S, Ezeanolue EE (2013) Adolescent Sickle Cell Awareness and Knowledge. Poster presentation at the Pediatric Academic Societies meeting, May 4–7, Washington, DC
- Ezechukwu C, Chukwuka J. Pre-marriage counseling as a tool for sickle cell disease awareness in Nigerians. Sahel Med J. 2004;7:54–57. doi: 10.4314/smj2.v7i2.12868. [DOI] [Google Scholar]
- Galadanci N, et al. Current sickle cell disease management practices in Nigeria. Int Health. 2014;6:23–28. doi: 10.1093/inthealth/iht022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffbrand A, Petit J, Moss P. Essential haematology. 4. Massachusetts: Blackwell Science; 2001. [Google Scholar]
- IBM Corp (Released 2013) IBM SPSS Statistics for Macintosh, Version 22.0. IBM Corp, Armonk, NY
- Martin P, Pearson H. Hemoglobinopathies and thalassemias. In: Kenn B, Oski F, editors. Oski’s essential paediatrics. 3. Philadelphia: Lippincott-Raven Publishers; 1997. pp. 347–350. [Google Scholar]
- National Heart Lung, and Blood Institute, National Institute of Health (2012) Sickle cell disease research & care. http://www.nhlbi.nih.gov/news/spotlight/fact-sheet/sickle-cell-disease-research-care.html. Accessed 12 Aug 2014
- Nnaji GA, Ezeagwuna DA, Nnaji I, Osakwe JO, Nwigwe AC, Onwurah OW. Prevalence and pattern of sickle cell disease in premarital couples in Southeastern Nigeria. Niger J Clin Pract. 2013;16:309–314. doi: 10.4103/1119-3077.113452. [DOI] [PubMed] [Google Scholar]
- Ola B, Coker R, Ani C. Stigmatising attitudes towards peers with sickle cell disease among secondary school students in Nigeria. Int J Child Youth Fam Stud. 2013;4:391–402. [Google Scholar]
- Olakunle OS, Kenneth E, Olakekan AW, Adenike OB. Knowledge and attitude of secondary school students in Jos, Nigeria on sickle cell disease. Pan Afr Med J. 2013;15:127. doi: 10.11604/pamj.2013.15.127.2712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oludare GO, Ogili MC (2013) Knowledge, attitude and practice of premarital counseling for sickle cell disease among youth in Yaba. Nigeria Afr J Reprod Health 17:175–182 [PubMed]
- Owolabi RS, Alabi P, Olusoji D, Ajayi S, Otu T, Ogundiran A. Knowledge and attitudes of secondary school students in Federal Capital Territory (FCT), Abuja, Nigeria towards sickle cell disease. Niger J Med. 2011;20:479–485. [PubMed] [Google Scholar]
- Piel FB, Hay SI, Gupta S, Weatherall DJ, Williams TN. Global burden of sickle cell anaemia in children under five, 2010–2050: modelling based on demographics, excess mortality, and interventions. PLoS Med. 2013;10:e1001484. doi: 10.1371/journal.pmed.1001484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serjeant GR. The natural history of sickle cell disease. Cold Spring Harb Perspect Med. 2013;3:a011783. doi: 10.1101/cshperspect.a011783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahani S, Obaro S, Ezeanolue E. Awareness of sickle cell genotype among Nigerians in the United States. J Investig Med. 2013;61:58. [Google Scholar]
- Taiwo IA, Oloyede OA, Dosumu AO. Frequency of sickle cell genotype among the Yorubas in Lagos: implications for the level of awareness and genetic counseling for sickle cell disease in Nigeria. J Community Genet. 2011;2:13–18. doi: 10.1007/s12687-010-0033-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services (2013) Healthy People 2020. http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=4.
- World Health Organization (2006) Sickle cell anemia: Report by the Secretariat. Fifty-ninth World Health Assembly
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 14 kb)
(DOCX 16 kb)