Abstract
Background:
The Spinal Cord Injury (SCI) Longitudinal Aging Study was initiated in 1973 and has conducted 8 assessments over the past 40 years. It was designed to help rehabilitation professionals understand the life situation of people with SCI, but it has developed into the most long-standing study of aging and SCI and has resulted in over 50 publications.
Objective:
Our purpose was to provide a detailed history of the study, response patterns, utilization of measures, and a summary of key findings reported in the literature.
Methods:
Five participant samples have been incorporated over the 40 years, with enrollment in 1973, 1984, 1993 (2 samples), and 2003. A total of 2,208 participants have completed 6,001 assessments, with a particularly large number of assessments among those who are more than 40 years post injury (n = 349).
Results:
The overall results have indicated changing patterns of outcomes over time as persons with SCI age, with some notable declines in participation and health. There has been a survivor effect whereby persons who are more active, well-adjusted, and healthier live longer.
Conclusions:
This study has several important features that are required for longitudinal research including (a) consistency of follow-up, (b) consistency of measures over time, (c) addition of new participant samples to counteract attrition, and (d) inclusion of a large number of individuals who have reached aging milestones unparalleled in the literature. Data from this study can inform the literature on the natural course of aging with SCI.
Key words: aging, longitudinal, spinal cord injury
A white paper by a panel of experts from around the United States highlighted the need for ongoing longitudinal studies of the natural course of spinal cord injury (SCI),1 as now more people than ever have lived decades with SCI. Rehabilitation professionals need to understand the natural course of aging after SCI, particularly as related to health, participation in community activities, and quality of life (QOL). This need is reflected in the premature aging observed in several physiological systems (eg, cardiovascular, musculoskeletal, and endocrine).2 We need to understand why aging adversely affects some people, yet others are better able to maintain their health and QOL. The effects of aging are likely to be the most profound among persons who live the majority of their lives with SCI, rather than those who were injured later in life at older ages.1,3
Although discussion has increased regarding aging among people with SCI, relatively few studies have been conducted and research has focused on the medical aspects of aging. The SCI Model Systems (SCIMS), a number of specialty hospitals funded by the National Institute for Disability, Independent Living, and Rehabilitation Research (NIDILRR), have been collectively pooling data, which has been an invaluable resource.4 However, the SCIMS database was not designed to study aging per se and it is currently limited in the number of individuals who have reached aging milestones, so the primary contributions of the database are not directly related to aging.
Other longitudinal studies have made contributions to the study of aging and risk factors for cardiovascular disease (previous National Institute on Disability and Rehabilitation Research [NIDRR]–funded Rehabilitation Research Training Center [RRTC] at Rancho Los Amigos National Rehabilitation Hospital, Downey, CA), secondary conditions study among British participants with long-standing SCI (previous NIDRR-funded RRTC at Craig Hospital, Englewood, CO), and the incidence and prevalence of several health and psychosocial conditions (previous NIDRR-funded collaborative project at Shepherd Center, Rancho Los Amigos, and Craig Hospital). Investigators at the University of Washington are investigating aging longitudinally using multiple disabling conditions and have helped to advance the field, yet they have a limited number of people with SCI.5 These studies have used at least 2 times of measurement for an interval up to 17 years.6
The most long-standing longitudinal study of SCI outcomes is the 40-year SCI Longitudinal Aging Study. It was initiated in 1973 by Dr. Nancy Crewe and her colleagues at the University of Minnesota as a study of the life situation of persons living in the community with SCI.7 At the time, very little was known about individuals living in the community with SCI, as the emphasis was almost exclusively on the importance of inpatient rehabilitation. The study was not designed to be longitudinal or to focus on aging, but it evolved over the years into an invaluable resource for investigating the natural course of aging after SCI. There have now been a total of 8 times of measurement with 5 participant cohorts totaling 2,208 unique participants and 6,001 completed assessments.
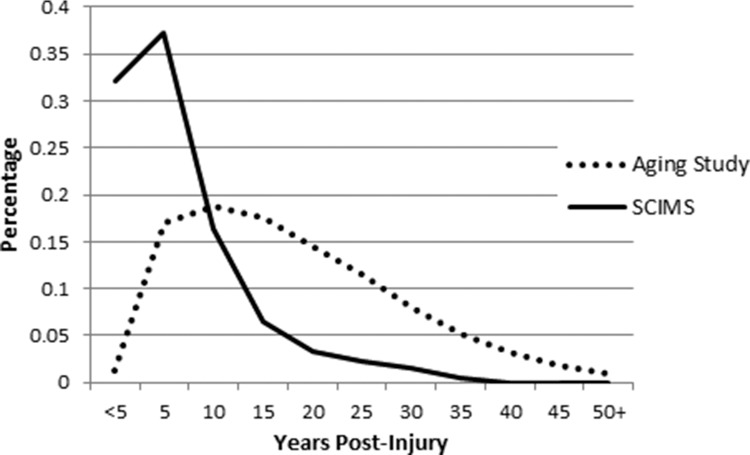
Figure 1 illustrates the fundamental differences between the SCI Longitudinal Aging Study and the SCIMS database, as related to aging, by comparing the portion of assessments as a function of years post injury. Because the SCIMS database started with an inception cohort at the time of injury, the distribution of data collection is highly skewed toward early after SCI onset, with a large number of assessments completed within the first 5 years after injury. In contrast, the distribution of assessments is only modestly skewed in the SCI Longitudinal Aging Study with a peak at 10 years and gradual decline thereafter. There have been 349 assessments completed among cohorts that were 40, 45, and 50+ years post injury (compared with 7 total at 40 years within the SCIMS database).4
Figure 1. Percentage of participants in the Aging Study and Spinal Cord Injury Model System (SCIMS) database by year post injury.
Our purpose is to describe the 40-year SCI Longitudinal Aging Study, including its history, enrollment of participants, methodology, and key findings that have been reported in the literature. Provided here is an overview of the study and its evolution over the years as a prelude to 2 articles within the current issue (Saunders and Krause, “Injuries and Falls in an Aging Cohort with Spinal Cord Injury: SCI Aging Study,” and Cao et al, “Impact of Marital Status on 20-Year Subjective Well-being Trajectories”).
Methods
Participants
The SCI Longitudinal Aging Study began with a sample of 256 participants, and 4 additional samples have been added over the 40 years. The 5 participant samples are from 2 distinct geographical locations: the Midwest (3 samples) and the Southeast (2 samples). The same 3 inclusion criteria were used for each sample: (1) traumatic SCI with some residual impairment (what currently would be classified as American Spinal Injury Association Impairment Scale [AIS] A-D), (2) at least 1 year since SCI onset, and (3) a minimum age of 18 years at study enrollment.
Participants in the midwestern samples were identified through all possible cases from outpatient records at a university hospital and a rehabilitation hospital in Minnesota who met the selection criteria. Some participants for the third sample were identified from a transitional living facility in the same geographic region. Table 1 summarizes the response pattern across the 8 times of measurement. Sample 1 first participated during the preliminary study in 1973. A total of 256 out of 301 eligible individuals participated (85% response rate). Sample 2 was added during the second stage in 1984, when 193 of 266 eligible (73%) participated. Sample 3 was comprised of 199 participants who were added in 1993 (78% response rate).
Table 1. Number of responses at each time of measurement.
| Follow-up | Year | S1 | S2 | S3 | S4 | S5 | S6 | New | Total | |
| 1973 | 256 | — | — | — | — | — | 256 | 256 | ||
| 11 | 1984 | 154 | 193 | — | — | — | — | 193 | 347 | |
| 15 | 1989 | 135 | 151 | — | — | — | — | 0 | 286 | |
| 20 | 1993 | 114 | 122 | 199 | 597 | — | — | 796 | 1,032 | |
| 25 | 1998 | 95 | 104 | 163 | 398 | — | — | 0 | 760 | |
| 30 | 2003 | 78 | 91 | 136 | 300 | 963 | — | 963 | 1,568 | |
| 35 | 2008 | 63 | 71 | 103 | 219 | 537 | — | 0 | 993 | |
| 40 | 2013 | 48 | 55 | 91 | 181 | 384 | — | 0 | 759 |
Note: Each study data collection typically took place over a 2-year timeframe, but we use 1 year for ease of interpretation.
The initial southeastern sample also first participated in 1993 and was identified from outpatient records of a specialty hospital in Georgia that had been designated as an SCIMS. Using a stratified sampling technique based on gender, race, and age, a total of 597 of a possible 710 individuals with SCI returned usable materials (84% response rate). Using the same selection criteria, a second southeastern sample was added in 2003 from the same specialty hospital; 963 of a possible 1,356 individuals participated in the study (71% response rate).
There have typically been outstanding rates of participation over time, particularly among the samples that have been in the study for the longest time. Table 1 summarizes the number of participants during each of the 8 preliminary stages of data collection (1973, 1984, 1989, 1993, 1998, 2003, 2008, and 2013). Attrition rates include those who were lost to mortality, which is substantially higher in SCI than in the general population,8–10 as well as those lost due to nonresponse and geographic mobility (ie, difficulty identifying current addresses).
The number at the top of each column indicates the number of individuals who were enrolled into the study and the corresponding year during which they were enrolled. For instance, for sample 1 (S1), 256 participants were enrolled in 1973. With minor exceptions, those who did not participate in a given follow-up were not contacted for subsequent follow-ups, such that the number at the bottom of each column represents the number of individuals who completed all previous assessments.
Sample characteristics: 40-year follow-up
At the most recent follow-up (2013), there were 759 active participants: 194 from the midwestern samples and 565 from the southeastern samples. Overall, 71.9% of the participants were male, and 79.1% were White (Table 2). The average age of participants was 27.3 years at time of injury and 54.3 years at the time of the study. An average of 27.0 years had passed since injury, and participants averaged 14.3 years of education. The samples were different in terms of some demographic characteristics, partially due to the region of the country from which they were selected.
Table 2. Participant characteristics by sample and region in 2013 (most recent follow-up).
| Midwest | Southeast | |||||
| S1 | S2 | S3 | S4 | S5 | Total | |
| Gender | ||||||
| Male | 85.4 | 89.1 | 73.6 | 54.1 | 74.8 | 71.9 |
| Female | 14.6 | 10.9 | 26.4 | 45.9 | 24.2 | 28.1 |
| Race | ||||||
| White | 100.0 | 96.4 | 96.7 | 61.9 | 77.9 | 79.1 |
| Black | 0.0 | 1.8 | 2.2 | 34.8 | 19.5 | 18.6 |
| Other | 0.0 | 1.8 | 1.1 | 3.3 | 2.6 | 2.3 |
| Injury severity | ||||||
| C1-C4, Non-A | 18.8 | 14.6 | 11.0 | 7.7 | 6.8 | 8.9 |
| C5-C8, Non-A | 37.5 | 41.8 | 35.2 | 29.3 | 22.8 | 28.1 |
| Non-C, Non-A | 33.3 | 23.6 | 37.4 | 44.8 | 35.9 | 37.1 |
| Ambulatory | 10.4 | 20.0 | 16.5 | 18.2 | 34.6 | 25.9 |
| Age at survey | 64.9 (5.0) | 59.3 (8.2) | 56.1 (10.1) | 54.2 (11.5) | 52.0 (12.5) | 54.3 (11.9) |
| Years post injury | 45.9 (4.1) | 36.1 (5.4) | 29.8 (7.2) | 26.5 (5.8) | 22.9 (9.9) | 27.0 (10.2) |
Note: Values given as % or mean (SD). Non-A = nonambulatory; S = sample.
Relevance to aging: Historical participation
Because of the longitudinal nature of the study and its relevance to aging, we break down the number of historical responses as related to years post injury, dating back to the preliminary assessment in 1973. We emphasize years post injury as it reflects aging after SCI onset, whereas age at injury onset reflects aging prior to SCI onset and chronologic age reflects the linear combination of both preinjury and postinjury aging. Table 3 breaks down the number of respondents according to years post injury at the time of assessment, presented in 5-year intervals, with 2.5-year windows on each side of the midpoint. For example, those at 40 years post injury include all persons assessed between 37.5 years and 42.4 years post injury. There have been 5,942 completed assessments, among those with data on injury year, with a total of 349 assessments in the categories of 40 years (n = 187), 45 years (n = 104), and 50+ years post injury (n = 58).
Table 3. Number of assessments completed as a function of years post injury at the time of assessment and total assessments across all years as compared with the SCIMS database.
| Years post injury | ||||||||||||
| ≤5 | 5 | 10 | 15 | 20 | 25 | 30 | 35 | 40 | 45 | 50+ | Total | |
| 1973 | 37 | 105 | 49 | 37 | 19 | 4 | 1 | 2 | 2 | — | — | 256 |
| 1985 | 2 | 78 | 80 | 84 | 55 | 25 | 15 | 8 | — | — | — | 347 |
| 1989 | — | 8 | 67 | 59 | 78 | 32 | 24 | 13 | 4 | 1 | — | 286 |
| 1994 | 14 | 343 | 227 | 156 | 102 | 100 | 40 | 23 | 15 | 5 | 1 | 1,026 |
| 1998 | — | 43 | 235 | 138 | 110 | 77 | 78 | 30 | 15 | 9 | 2 | 737 |
| 2002 | 28 | 443 | 232 | 280 | 176 | 141 | 116 | 68 | 28 | 19 | 7 | 1,538 |
| 2008 | — | — | 225 | 114 | 216 | 141 | 102 | 79 | 68 | 30 | 18 | 993 |
| 2013 | — | — | 1 | 170 | 107 | 170 | 102 | 84 | 55 | 40 | 30 | 759 |
| Total | 81 | 1,020 | 1,116 | 1,038 | 863 | 690 | 478 | 307 | 187 | 104 | 58 | 5,942a |
| SCIMS total as of 2013 | 35,106 | 40,562 | 17,967 | 7,147 | 3,698 | 2,500 | 1,597 | 598 | 7 | 0 | 0 | 109,182 |
Note: Years post injury is the midpoint of the grouping with 2.5 years on either side of the midpoint (eg, the 10-year interval assessments were completed between 7.6 and 12.4 years post injury). SCIMS = Spinal Cord Injury Model Systems.
While there have been 6,001 assessments conducted, there were 59 participants with missing data on year of injury that are not represented in this table.
Data collection procedures
Self-report measures have been obtained by mail during each of the 8 times of measurement. The data collection protocol has been relatively constant over the years, with only minor deviation. Cover letters that explain the study have routinely been sent prior to sending a full packet of materials. Two follow-up mailings have been implemented for nonrespondents, along with a follow-up phone call. Additional mailings have sometimes been utilized if the person has lost or discarded their materials but continue to express an interest in participating or as 1 follow-up loop near the end of the study.
Extensive efforts have been made to locate participants upon follow-up. During the early stages of the study, many participants were located through old addresses, relatives, and directory assistance. However, tracking has been more difficult over time, which is at least partially due to the proliferation of cell phones. Currently, participants are tracked through online search mechanisms. Participant remuneration was provided beginning in 1989 and has ranged from $5 to $40. Although no remuneration was provided in 1985, participants were offered copies of a handbook on employment that was developed from information gathered during the first assessment.7
Qualitative interviews were also conducted as part of the preliminary study in 197411 and the 20-year follow-up.12 The preliminary interviews conducted with 131 participants were used as a basis for the handbook for counselors on employment after SCI.7 The follow-up interviews 20 years later were conducted on a subsample of 50 of the original participants.12
Measures
The Life Situation Questionnaire (LSQ) was designed specifically for the study in 1973 to obtain mostly objectively verifiable information about the overall psychosocial, vocational, and medical outcomes of people with SCI. The initial version of the LSQ included the following content areas: (1) demographic and injury characteristics, (2) educational status and employment, (3) community participation, (4) activities of daily living and instrumental activities of daily living, (5) life satisfaction, (6) adjustment, and (7) recent medical history.
There are inherent, sometimes conflicting, challenges in longitudinal studies to utilize state-of-the-art measures that are constantly changing, while maintaining consistency for longitudinal comparisons. We have attempted to balance competing demands by maintaining the core content while adding additional measures to substantially increase the scope of measurement of key constructs, with a specific focus often added to a particular follow-up. We provide only relatively brief summaries of each area of variables, emphasizing those that have been part of the development of the LSQ and measured throughout the study, as well as key additions that have also been measured longitudinally. The timeline for the measures is summarized in Table 4.
Table 4. Timeline for measures.
| Data collections | ||||||||
| Variable | 1973 | 1984 | 1989 | 1993 | 1998 | 2003 | 2008 | 2013 |
| Demographic/Injury characteristics | ||||||||
| Gender/Age/Marital status | X | X | X | X | X | X | X | X |
| Race/Ethnicity | X | X | X | X | X | X | X | |
| Injury level/Date of injury/ Neurologic | X | X | X | X | X | X | X | X |
| completeness | ||||||||
| Etiology/Proxy for Frankel grade | X | X | X | X | ||||
| Educational status/ Employment/Socio-environmental | ||||||||
| Educational status | X | X | X | X | X | X | X | X |
| Employment history | X | X | X | X | X | X | X | X |
| Income | X | X | X | X | ||||
| Environmental factors - CHIEF | X | X | ||||||
| Social Support - BSSS | X | |||||||
| Social Support - PROMIS | X | |||||||
| Community participation | ||||||||
| Sitting tolerance | X | X | X | X | X | X | X | X |
| Frequency of social outings | X | X | X | X | X | X | X | X |
| Frequency of weekly visitors | X | X | X | X | X | X | X | X |
| Fitness ratings | X | X | X | X | X | X | ||
| Fitness activities | X | X | X | X | ||||
| CHART | X | X | X | X | ||||
| Recreational activities | X | X | ||||||
| Health behaviors | ||||||||
| Prescription medications | X | X | X | X | ||||
| Smoking/alcohol use | X | X | X | X | ||||
| Alcohol abuse - CAGE | X | X | ||||||
| Immunizations/vaccinations | X | |||||||
| Function | ||||||||
| Activities of daily living | X | X | X | X | X | X | X | X |
| Instrumental activities of daily living | X | X | X | X | X | X | X | X |
| Life satisfaction | ||||||||
| Life Satisfaction (6-item) | X | X | X | X | X | X | X | X |
| 11-item | X | X | X | X | X | X | X | |
| 20-item | X | X | X | X | X | |||
| Problems (15-item) | X | X | X | X | X | X | X | |
| 30-item | X | X | X | X | X | |||
| Adjustment | ||||||||
| Self-rated adjustment | X | X | X | X | X | X | X | X |
| Quality of life | X | X | X | X | ||||
| Personality - MPQ | X | |||||||
| Recent medical history | ||||||||
| General health | X | X | X | X | X | X | X | X |
| Pressure ulcers | X | X | X | X | ||||
| Subsequent Injuries | X | X | X | X | ||||
| Depression - OAHMQ | X | X | X | X | ||||
| Depression - PHQ-9 | X | X | ||||||
| Secondary conditions checklist | X | |||||||
| Pain | X | X | X | |||||
| Fatigue | X | X | X | |||||
| PTSD | X | |||||||
| Pneumonia | X | |||||||
| Chronic conditions | X | |||||||
Note: BSSS = Berlin Social Support Scales; CAGE = cut down on drinking, annoyed by criticism, guilty about drinking, eye opener in the morning; CHART = Craig Handicap Assessment Reporting Technique; CHIEF = Craig Handicap Inventory of Environmental Factors; MPQ = Multidimensional Personality Questionnaire; OAHMQ = Older Adult Health and Mood Questionnaire; PHQ-9 = Patient Health Questionnaire – 9-item version; PTSD = posttraumatic stress disorder.
Demographic characteristics including gender, age, and marital status were collected, with race and ethnicity added during subsequent follow-ups.
Injury characteristics in the original LSQ were limited to injury level, date of injury, and neurologic completeness of injury; etiology and a proxy measure for Frankel grade were added beginning in 1998.
Educational status was measured by the number of years of education during the preliminary assessments but was expanded to include passing of educational milestones, such as completion of diplomas and degrees, and whether this occurred prior to or after SCI onset.
Employment history was measured by current employment status, hours worked per week, and job type. Measurement of employment was significantly expanded over time to include more details regarding the timing of employment related to the onset of SCI, barriers to employment, and job accommodations.
Measurement of participation was limited in the LSQ to 3 general items including sitting tolerance, frequency of weekly social outings, and frequency of weekly visitors. Five fitness items were assessed as proxy variables for healthy lifestyle within the revised LSQ, beginning with the third stage of the study in 1989.
Activities of daily living (ADL) and instrumental activities of daily living (IADL) were measured with 15 items with 3 categories: independent, partially dependent, and dependent.
Psychosocial adjustment was measured initially with 2 sets of items, including 6 life satisfaction items measured using a 5-point Likert scale and 2 self-rated adjustment scales, each measured on a 10-point scale. The number of satisfaction items increased to 11 on the first follow-up in 1984 and to 20 items beginning in the data collection in 1993. A set of 15 problems items was added in 1984, also using a 5-point Likert scale, and was expanded to 30 items in 1993.
Measurement of medical history included nonroutine physician visits, hospitalizations, and days hospitalized within the 12 months prior to the assessment. Beginning in 1998, several additional indicators of secondary health conditions were added over time, emphasizing pressure ulcers and subsequent injuries.
Several measures have been added. In 1998, we added select items from the Craig Handicap Assessment Reporting Technique (CHART),13 a set of items regarding the frequency of use of prescription medications to treat 4 types of conditions (pain, spasticity, sleep, depression/ anxiety),14,15 and several questions regarding smoking and alcohol use from the Behavioral Risk Factor Surveillance System (BRFSS).16
Several socio-environmental measures have been used, including portions of the Berlin Social Support Scales (BSSS) (Perceived Support, Need for Support, and Support Seeking).17 In the most recent time of measurement, these items were replaced with items from the PROMIS Social Support Scale.18 The Craig Handicap Inventory of Environmental Factors (CHIEF) Short Form was used on 2 occasions to assess the amount which environmental factors acted as barriers.13
We began measuring depressive symptoms in 1998 using the Older Adult Health and Mood Questionnaire19 (OAHMQ) and subsequently added the Patient Health Questionnaire – 9-item version (PHQ-9).20 Other psychometric measures have been introduced to the study but not used consistently throughout. For instance, the Multidimensional Personality Questionnaire21 was used on a single occasion in 1988,22 and the Purdue PTSD was used in 2003.23
Health items from the BRFSS were added in 2003, along with measurement of pain and pain interference with the Brief Pain Inventory (BPI)24 and fatigue using the Modified Fatigue Impact Scale (MFIS).25,26 A measure of secondary health conditions, the Secondary Health Conditions Checklist, was assessed 1 time only in 1993.27 This measure asked about 50 secondary conditions in the past year and also since SCI onset.
Summary of Published Studies
What have we learned? Although it is beyond the scope of this article to review all published studies, we note important trends in 4 areas related to the natural course of SCI: (1) the survivor effect; (2) changing trends in activities, satisfaction, and health over time; (3) the multifaceted nature of subjective well-being (SWB); and (4) multiple indicators of outcomes reflecting successful employment. Our review is not an attempt to be comprehensive but rather to reflect upon some of the most important considerations with SCI that have been the focus of the investigation from the inception of the study.
Survivor Effect
One of the most important findings has been the survivor effect, whereby those individuals who were more active, employed, and had better overall psychosocial adjustment were more likely to live to subsequent follow-ups. The first longitudinal analysis indicated that those who had greater psychosocial and vocational adjustment, more so than medical adjustment, were more likely to have survived over the 11-year interval.28 This trend continued in subsequent analyses.29,30 Participation in social activities outside the home and sitting tolerance were important protective factors for mortality, whereas self-reported physical and psychological health problems, dependency, and economic barriers represented significant risk factors.28–30
The survivor effect is not only important from the methodologic standpoint of understanding that survivors are not representative of the full population of people with SCI, but is also important from the clinical and rehabilitative perspective for the need to intervene to promote longevity. These findings have been exceedingly important to the field, as they drew an explicit link between psychosocial and vocational factors with longevity, at a time where other research was focusing almost exclusively on demographic and injury-related predictors of mortality.31,32 Individuals with SCI face significant challenges in maintaining longevity; therefore it is important to promote their psychological well-being, gainful employment, and active participation to reduce their risk of mortality related with SCI. The findings also underscore the importance of involving interdisciplinary professionals in SCI patient care, as factors related to mortality are highly diverse and multiple intervention strategies are needed to promote longevity. Without question, persons with SCI are vulnerable to mortality and require greater vigilance in health behaviors compared with the general population.
Natural course of SCI
Perhaps the most striking immediate observation was that the participants appeared to be relatively well-adjusted overall, and nearly all outcomes improved over the first 11 years.33 The improved outcomes among the longitudinal participants were paralleled by those observed among new participants, suggesting a significant global environmental effect between 1973 and 1984.34,35 There were significant enhancements to education and employment outcomes over time, and this remained apparent at the 20-year follow-up.36 However, beginning with the 25-year follow-up,37 some important changes were identified where social participation and satisfaction with social activities and health decreased. Satisfaction with employment and employment indicators were maintained. A more complete analysis of the 30-year data further documented these changes, indicating that favorable outcomes plateaued somewhere between 15 and 20 years after the preliminary follow-up38; these changes were also identified at 35 years.39 The effects of aging and the passage of time appeared to have the greatest impact on social and medical outcomes, whereas employment outcomes were typically maintained. Without question, there is pressure to maintain employment and financial resources among persons who have worked into later adulthood. It will be important for further research to evaluate whether the pressure to maintain employment may affect an individual’s ability to sustain other aspects of life, including health, participation, and SWB.
Subjective well-being
SWB is measured from the perspective of the individual. SWB has proven to be a multidimensional construct, with various aspects changing over time after SCI. We initially captured SWB through life satisfaction only, measuring both general satisfaction and economic satisfaction.
Economic satisfaction improved over time and general satisfaction (social life, sex life, and health) declined over time.37,40 After expanding the measurement to additional items and including self-reported problems, the multifaceted nature of SWB after SCI became readily apparent; we identified 7 factor scales when performing factor analysis jointly using the 2 sets of items (life satisfaction, problems)41 and 9 separate scales when performing distinct analyses.42 The impact of aging on SWB suggests that persons who were older at injury onset and chronologically older had lower levels of SWB and lower self-reported adjustment.35,43 White participants reported higher SWB across several indices, and males had lower scores than women on satisfaction interpersonal relations.44 The trajectory of employment satisfaction contradicts somewhat the patterns seen in other life satisfaction areas. Longitudinal examinations have indicated an increase in employment satisfaction over time, with an indication that employment satisfaction may increase in the years shortly after onset of injury but then decline thereafter.38
Other SWB outcomes related to psychological distress are important to consider given the relationship with outcomes such as mortality and functioning.30 A longitudinal examination of depression across 5 years indicated that 22.1% and 20.2% of participants met criteria for probable major depression at baseline and follow-up, respectively.45 Of those with probable major depression at baseline, 55.7% met criteria at follow-up; this suggests that the risk of probable major depression increases substantially among those who previously had significant depressive symptomatology. Although this is not surprising, the strength of the relationship is particularly noteworthy, as it indicates the degree to which it is difficult for persons with SCI to overcome depressive disorders.
Predictors of probable major depression included being nonambulatory, being a non-White male, being female, greater time since injury, more frequent pain medication use, and less activity. A cross-sectional analysis using the aging database indicated that only 7.2% of participants experienced post-traumatic stress disorder (PTSD), and PTSD was found to be greatly related to the experience of depressive symptomatology. It is noteworthy that all participants had lived several years with SCI at a minimum at the time of first assessment, so PTSD could have been present earlier; however, it clearly decreased over the decades after SCI onset and did not appear to be a major issue for study participants. Taken together, the findings suggest there is an increased risk of depressive disorder among persons with SCI, even though the overall level of SWB across the participants remains relatively high.
Trends in employment
Some of the most important analyses of the data have come from the analysis of employment outcomes, particularly as related to the diversity of potential outcomes compared with the nearly singular focus on current employment within the literature. We found that postinjury employment rates, reflective as to whether the individual has worked at any time since SCI onset, exceed 50%. This is due to an approximate 2 to 1 ratio of those who remain employed at a given point in time compared to those who lose employment, highlighting the importance of improving job retention.46 This may be partially related to premature departure from the workforce as individuals age with SCI.47
Other findings help to differentiate the relationship of predictive factors with postinjury employment from their relationship with other quality indicators such as job retention and earnings. Whereas persons with less severe SCI are more likely to obtain employment, they are not more likely to retain it. Similarly, we did not find injury severity to be related to earnings among those who had postinjury employment.48,49 We also found that persons who are non-White or Hispanic (race/ethnicity), female (gender), and have lower education levels are less likely to become employed after SCI onset and they also make less income when employed. So, whereas injury severity variables lead to employment disadvantage due to the inability of individuals to obtain employment, gender, race, and education are related to disparities in multiple quality indicators of employment as well.
Another important employment outcome is the amount of time between SCI onset and the first employment post injury. The average time from SCI onset to first postinjury job was 4.8 years, with both a fast track and a slow track to employment.50 The fast track is marked by higher education, having worked in a professional occupation prior to SCI onset, and having the opportunity to return to the preinjury employer. The earlier findings on postinjury employment indicated the importance of job retention, but these findings emphasize the importance of a speedy return to work whenever possible (ie, before the opportunity is lost). In a longitudinal analysis of barriers to employment, we found that health barriers, such as pressure ulcers, were the most significant barriers to future employment.51 Even though medical and financial disincentives were indicated as barriers by many unemployed participants, they were unrelated to the probability of future employment.
Summary and Future Directions
The foresight and initiative taken by Dr. Crewe and her colleagues to identify the life situation of persons with SCI in 1973 has paid outstanding dividends. With the evolution of the initial research into a 40-year longitudinal study, it has had particular relevance to aging and to our understanding of the natural course of SCI in psychosocial and vocational areas. We have presented a summary of the history, methodology, and some of the findings to provide an overview of the complicated picture related to the natural course of SCI. Additional analyses with varying subsets of participants from the overall study extend our knowledge. It is only through steadfast commitment to longitudinal research in a partnership between research participants and investigators that we will successfully unravel the effects of aging after SCI and identify diverse intervention strategies to improve all outcomes, including longevity.
Acknowledgments
The authors have no conflicts of interest to disclose.
This article is dedicated to the memory of Nancy M. Crewe, PhD, and Sarah B. Lottes. Dr. Crewe had the foresight to initiate the SCI Longitudinal Aging Study in 1973. Without her mentorship, this would never have developed into a longitudinal study, much less a 40-year study. Sarah was devoted to this study since her involvement in 1993 as a Research Coordinator until the day of her death at age 72. Their memory and spirit are constant motivation for the continuation of this work.
Financial support/disclosures: The contents of this presentation were developed under grants from the US Department of Health and Human Services Administration for Community Living, NIDILRR grant numbers H133G110157, H133G060126, H133G020239, H133G010009, H133G70111, and H133G20200. However, those contents do not necessarily represent the policy of the US Department of Health and Human Services and endorsement by the Federal Government should not be assumed.
References
- 1. Groah SL, Charlifue S, Tate D, et al. Spinal cord injury and aging: Challenges and recommendations for future research. Am J Phys Med Rehabil. 2012;91(1):80–93. [DOI] [PubMed] [Google Scholar]
- 2. Hitzig SL, Eng JJ, Miller WC, Sakakibara BM. An evidence-based review of aging of the body systems following spinal cord injury. Spinal Cord. 2011;49(6):684–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jensen MP, Truitt AR, Schomer KG, Yorkston KM, Baylor C, Molton IR. Frequency and age effects of secondary health conditions in individuals with spinal cord injury: A scoping review. Spinal Cord. 2013;51(12):882–892. [DOI] [PubMed] [Google Scholar]
- 4. National Spinal Cord Injury Statistical Center. The 2013 Annual Statistical Report for the Spinal Cord Injury Model Systems. 2013. [Google Scholar]
- 5. Matsuda PN, Verrall AM, Finlayson ML, Molton IR, Jensen MP. Falls among adults aging with disability. Arch Phys Med Rehabil. 2015;96(3):464–471. [DOI] [PubMed] [Google Scholar]
- 6. Adkins RH, Szlachcic Y, Govindarajan S. Metabolic syndrome and spinal cord injury: A 17-year longitudinal study. Top Spinal Cord Inj Rehabil. 2010;16(2):40–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Crewe NM, Athelstan GT, Bower A. Employent After Spinal Cord Injury: A Handbook for Counselors. Minneapolis: University of Minnesota, Department of Physical Medicine and Rehabilitation; 1978. [Google Scholar]
- 8. DeVivo MJ, Krause JS, Lammertse DP. Recent trends in mortality and causes of death among persons with spinal cord injury. Arch Phys Med Rehabil. 1999;80(11):1411–1419. [DOI] [PubMed] [Google Scholar]
- 9. Devivo MJ, Chen Y, Krause JS, Saunders LL, Cao Y. Causes of death in an aging spinal cord injury population. Paper presented at: Academy of Spinal Cord Injury Professionals; 2013; Las Vegas, NV. [Google Scholar]
- 10. Strauss DJ, DeVivo MJ, Paculdo DR, Shavelle RM. Trends in life expectancy after spinal cord injury. Arch Phys Med Rehabil. 2006;87(8):1079–1085. [DOI] [PubMed] [Google Scholar]
- 11. Athelstan GT, Crewe NM. Psychological adjustment to spinal cord injury as related to manner of onset of disability. Rehabil Couns Bull. 1979;22:311–319. [Google Scholar]
- 12. Crewe NM. Life stories of people with long term spinal cord injury. Rehabil Couns Bull. 1997;41(1):26–42. [Google Scholar]
- 13. Whiteneck GG, Charlifue SW, Gerhart KA, Overholser JD, Richardson GN. The Craig Handicap Assessment and Reporting Technique. Englewood, CO: Craig Hospital;1992. [Google Scholar]
- 14. Krause JS, Vines CL, Farley TL, Sniezek J, Coker J. An exploratory study of pressure ulcers after spinal cord injury: Relationship to protective behaviors and risk factors. Arch Phys Med Rehabil. 2001;82(1):107–113. [DOI] [PubMed] [Google Scholar]
- 15. Krause JS. Factors associated with risk for subsequent injuries after the onset of traumatic spinal cord injury. Arch Phys Med Rehabil. 2004;85:1503–1508. [DOI] [PubMed] [Google Scholar]
- 16. Center for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Questionnaire. 1996. http://www.cdc.gov/brfss/questionnaires/pdf-ques/96brfss.pdf.
- 17. Schwarzer R, Schulz U. Berlin Social Support Scales (BSSS). 2000. http://userpage.fu-berlin.de/~health/bsss.htm. Accessed January 22, 2007.
- 18. National Institute of Health. PROMIS instrument development and psychometric evaluation, scientific standards. 2012. http://www.nihpromis.org/Documents/PROMIS_Standards_050212.pdf. Accessed October, 2012.
- 19. Kemp BJ, Adams BM. The Older Adult Health and Mood Questionnaire: A measure of geriatric depressive disorder. J Geriatr Psychiatry Neurol. 1995;8(3):162–167. [DOI] [PubMed] [Google Scholar]
- 20. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tellegen A. Multidimensional Personality Questionnaire. Minnesota: University of Minnesota Press; 1982. [Google Scholar]
- 22. Krause JS. Personality and traumatic spinal cord injury: Relationship to participation in productive activities. J Appl Rehabil Couns. 1997;28(2):15–20. [Google Scholar]
- 23. Lauterbach D, Vrana SR. Three studies on the reliablity and validity of a self-report measure of posttraumatic stress disorder. Assessment. 1996;3:17–25. [Google Scholar]
- 24. Cleeland CS. The Brief Pain Inventory: User guide. 2009. http://www.mdanderson.org/education-and-research/departments-programs-and-labs/departments-and-divisions/symptom-research/symptom-assessment-tools/BPI_UserGuide.pdf.
- 25. Fisk JD, Ritvo PG, Ross L, Haase DA, Marrie TJ, Schlech WF. Measuring the functional impact of fatigue: Initial validation of the fatigue impact scale. Clin Infect Dis. 1994;19:S79–S83. [DOI] [PubMed] [Google Scholar]
- 26. Multiple Sclerosis Council for Clinical Practice Guidelines; Fatigue and Multiple Sclerosis: Evidence-Based Management of Strategies for Fatigue in Multiple Sclerosis. Washington, DC: Paralyzed Veterans of America; 1998. [Google Scholar]
- 27. Krause JS. Skin sores after spinal cord injury: Relationship to life adjustment. Spinal Cord. 1998;36:51–56. [DOI] [PubMed] [Google Scholar]
- 28. Krause JS, Crewe NM. Prediction of long-term survival of persons with spinal cord injury: An 11 year prospective study. Rehabil Psychol. 1987;32:205–213. [Google Scholar]
- 29. Krause JS. Survival following spinal cord injury: A fifteen-year prospective study. Rehabil Psychol. 1991;36(2):89–98. [Google Scholar]
- 30. Krause JS, Kjorsvig JM. Mortality after spinal cord injury: A four-year prospective study. Arch Phys Med Rehabil. 1992;73(6):558–563. [PubMed] [Google Scholar]
- 31. DeVivo MJ, Stover SL, Black KJ. Prognostic factors for 12-year survival after spinal cord injury. Arch Phys Med Rehabil. 1992;73(2):156–162. [PubMed] [Google Scholar]
- 32. DeVivo MJ, Stover SL. Long term survival and causes of death In: Stover SL, DeLisa JA, Whiteneck GG, eds. Spinal Cord Injury: Clinical Outcomes from the Model Systems. Gaithersburg, MD: Aspen, Publishers; 1995:289–316. [Google Scholar]
- 33. Crewe N, Krause J. An eleven-year follow-up of adjustment to spinal cord injury. Rehabil Psychol. 1990;35(4):205–210. [Google Scholar]
- 34. Krause JS, Crewe NM. Chronologic age, time since injury, and time of measurement: Effect on adjustment after spinal cord injury. Arch Phys Med Rehabil. 1991;72:91–100. [PubMed] [Google Scholar]
- 35. Krause JS, Sternberg M. Aging and adjustment after spinal cord injury: The roles of chronologic age, time since injury, and environmental change. Rehabil Psychol. 1997;42(4):287–302. [Google Scholar]
- 36. Krause JS. Changes in adjustment after spinal cord injury: A 20-year longitudinal study. Rehabil Psychol. 1998;43(1):41–55. [Google Scholar]
- 37. Krause JS, Broderick L. A 25-year longitudinal study of the natural course of aging after spinal cord injury. Spinal Cord. 2005:1–8. [DOI] [PubMed] [Google Scholar]
- 38. Krause JS, Coker JL. Aging after spinal cord injury: A 30-year longitudinal study. J Spinal Cord Med. 2006;29(4):371–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Krause JS, Bozard JL. Natural course of life changes after spinal cord injury: A 35-year longitudinal study. Spinal Cord. 2012;50(3):227–231. [DOI] [PubMed] [Google Scholar]
- 40. Krause JS. Adjustment after spinal cord injury: A 9-year longitudinal study. Arch Phys Med Rehabil. 1997;78(6):651–657. [DOI] [PubMed] [Google Scholar]
- 41. Krause JS. Dimensions of subjective well-being after spinal cord injury: An empirical analysis by gender and race/ethnicity. Arch Phys Med Rehabil. 1998;79(8):900–909. [DOI] [PubMed] [Google Scholar]
- 42. Krause JS, Reed KS. Life satisfaction and self-reported problems after spinal cord injury: Measurement of underlying dimensions. Rehabil Psychol. 2009;54(3):343–350. [DOI] [PubMed] [Google Scholar]
- 43. Krause JS. Aging and life adjustment after spinal cord injury. Spinal Cord. 1998;36(5):320–328. [DOI] [PubMed] [Google Scholar]
- 44. Krause JS. Subjective well-being after spinal cord injur y: Relationship to gender, race-ethnicity, and chronologic age. Rehabil Psychol. 1998;43(4):282–296. [Google Scholar]
- 45. Saunders LL, Krause JS, Focht KL. A longitudinal study of depression in survivors of spinal cord injury. Spinal Cord. 2012;50(1):72–77. [DOI] [PubMed] [Google Scholar]
- 46. Krause JS, Terza JV, Dismuke C. Factors associated with labor force participation after spinal cord injury. J Vocational Rehabil. 2010;33(2):89–99. [Google Scholar]
- 47. Krause JS. Employment after spinal cord injury: Relation to selected participant characteristics. Arch Phys Med Rehabil. 1996;77:737–743. [DOI] [PubMed] [Google Scholar]
- 48. Krause JS, Terza JV. Injury and demographic factors predictive of disparities in earnings after spinal cord injury. Arch Phys Med Rehabil. 2006;87(10):1318–1326. [DOI] [PubMed] [Google Scholar]
- 49. Krause JS, Terza JV, Dismuke C. Earnings among people with spinal cord injury. Arch Phys Med Rehabil. 2008;89(8):1474–1481. [DOI] [PubMed] [Google Scholar]
- 50. Krause JS. Years to employment after spinal cord injury. Arch Phys Med Rehabil. 2003;84(9):1282–1289. [DOI] [PubMed] [Google Scholar]
- 51. Krause JS, Reed KS. Barriers and facilitators to employment after spinal cord injury: Underlying dimensions and their relationship to labor force participation. Spinal Cord. 2011;49(2):285–291. [DOI] [PubMed] [Google Scholar]