Abstract
Background:
Medication reconciliation is one of the more challenging aspects of inpatient care, and its accuracy is paramount to safe transitions of care. Studies have shown that pharmacists have a role in medication reconciliation through improving patient safety and avoiding costs associated with medication errors. The wide-scale use of pharmacists in this process has been limited by time constraints, cost, and lack of resources.
Objective:
This study evaluates the impact of pharmacists in resolving medication errors, decreasing readmission rates, and reducing institutional costs during the discharge medication reconciliation process.
Methods:
Pharmacists evaluated discharge medication reconciliation documentation for patients to determine its accuracy, the accuracy of the admission reconciliation documentation, and any potential issues unrelated to accuracy. Analysis of these data determined the time required for pharmacist involvement, the number of errors identified by pharmacists, the quality of pharmacist interventions, the cost avoidance for each error, and the overall impact on hospital readmission.
Results:
During the 7-week study period, pharmacists performed 67 discharge medication reviews and identified 84 errors. Seventy-five percent were considered to be significant and 6% were considered to be serious. The 30-day readmission rate in the study cohort was 18% compared with 20% in the control group. Based on the clinical severity scale and pharmacist salaries, pharmacist interventions resulted in $42,300 in cost avoidance.
Conclusion:
Pharmacists involved in this pilot discharge process identified and resolved significant errors on medication reconciliation orders that resulted in a financial benefit to the institution.
Keywords: cost avoidance, discharge, medication errors, medication reconciliation, readmissions
Performing medication reconciliation at the time of hospital admission and discharge is one of the more challenging aspects of inpatient care, but it is paramount to safe transitions of care. Inaccurate medication reconciliation is the source of many medication-related misadventures leading to hospital admissions and patient morbidity and mortality.1–3
Because of the emphasis on increasing patient safety and reducing health care dollars spent, medication reconciliation is the focus of many health systems. Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) surveys and Centers for Medicare & Medicaid Services (CMS) now highlight the importance of proper medication reconciliation and use it to help determine reimbursement rates.4–6 However, many patient and provider barriers can prevent clinicians from obtaining a proper medication history, which leads to unsafe transitions of care, specifically at discharge. Patients, for example, may lack the cognitive skills to understand instructions for medication use and to accurately communicate to providers how they are using medications.1 Providers have limited time and may not have sufficient drug therapy knowledge to perform accurate medication reconciliation.1
Previous studies have shown that pharmacists can play an important role in the medication reconciliation process. By completing medication histories upon admission, pharmacists have decreased the number of errors and increased the accuracy of admission orders.7,8 Pharmacist involvement in discharge medication reconciliation has been shown to increase the accuracy of discharge orders and home medication regimens.7–10 Pharmacists can identify significant medication discrepancies at the time of discharge including missing medications, improper doses, and incomplete orders.7–10 However, the wide-scale use of pharmacists in the admission and discharge process has been limited by the time and the cost needed to incorporate pharmacists into the process. Furthermore, the impact of pharmacist medication reconciliation at discharge on hospital readmission rates has yet to be determined.
The aim of this pilot study was to evaluate the accuracy of current admission medication reconciliation practices as well as the clinical and financial impact of a pharmacist verification of discharge medication reconciliation after completion by the discharge provider.
Methods
This prospective, cross-sectional pilot study was conducted on 2 adult medical/surgical patient care units (unit) of a 700-bed academic medical center. All medical and surgical patients over the age of 18 who were discharged from these units Monday through Friday for a 7-week period from September to October 2013 were included. There were no additional inclusion and exclusion criteria. All methods and procedures were in accordance with the ethical standards set by the institutional review board. Results were analyzed and characterized by the discharge service (medicine or surgery).
Pharmacist Intervention
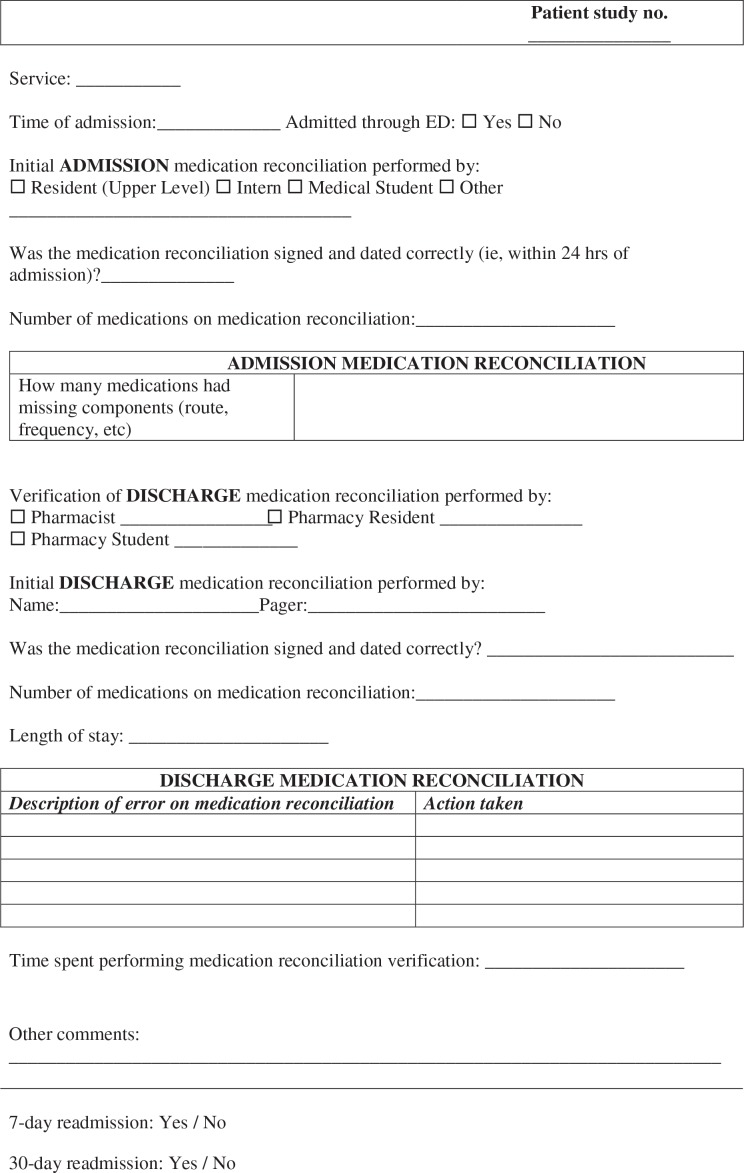
Once discharge orders were completed for an individual patient, the charge nurse for the unit contacted a designated pharmacist to begin the discharge medications review. The pharmacist would then review the patient’s profile, specifically the admission medication reconciliation documentation, all inpatient medication orders, and the discharge medication orders and prescriptions. The pharmacist clarified discrepancies by speaking to the patient and calling outpatient pharmacies to confirm medication lists. This comprehensive review allowed the pharmacist to examine the entire hospital course and determine the reason for discrepancies in the admission and discharge medication orders and any specific safety concerns (eg, identification of allergies, changes in vital signs, or changes in home medications). Using a data collection sheet (Figure 1), the pharmacist compared the medication lists and documented any potential errors. An error could include an omission of a medication; extra medications; inappropriate medications based on age, weight, or antibiotic susceptibilities; or discrepancies in dose, frequency, or dosage form. Based on the findings, the pharmacist would contact the patient’s nurse or prescriber as necessary to clarify and rectify any discrepancies. The time to complete the entire medication review process was recorded. If a pharmacist was unavailable to perform the review due to staffing patterns, this barrier was also documented. Figure 2 depicts the workflow for this process.
Figure 1.
Medication reconciliation data collection form.
Figure 2.

Workflow for discharge medication review process.
The admission medication reconciliation was considered to be complete if it was signed and dated within 24 hours and if no medications were missing a strength, dose, or frequency. Errors were categorized by relevant disease state or medication class, including diabetes mellitus, hypertension, antimicrobials, analgesics, anticoagulants, and chronic disease state management.
Outcomes
The primary outcome was the number and severity of errors identified by the pharmacist per patient per service. Secondary outcomes included a comparison of the 7- and 30-day readmission rates for study patients to rates for a historical cohort of patients admitted and discharged from the same units from July and August 2013.
Economic Analysis
An independent pharmacist not involved with the medication reconciliation process (W.B.) reviewed and graded the interventions based on clinical severity using a validated scale first reported by Overhage and Lukes in 1999.11 This scale stratifies the severity of an error in a medication order as potentially lethal, serious, significant, minor, or no error. The cost avoidance associated with each error was determined using methods described by Nesbit et al in 2000.12 To summarize, the probability of an adverse drug event (ADE) occurring in the absence of pharmacist intervention was estimated as 60% for potentially lethal errors, 40% for serious, 10% for significant, 1% minor, or 0% for no error, respectively. The average cost of a preventable ADE described in previous trials and adjusted for inflation using the Consumer Price Index to 2014 dollars was estimated to be $5,000. The assumption was made that the likelihood of an ADE would resemble estimates in the literature in the absence of pharmacist intervention; thus, the cost avoidance was calculated as the product of the likelihood of ADE and the average cost of each ADE for each level of error severity. The labor cost to the institution was calculated as the hourly salary and benefits wage for each of the practitioners involved (ie, pharmacists and pharmacy residents) multiplied by time spent performing this service. The perspective of the cost analysis was societal; although the institution was bearing the labor costs for the pharmacists to perform this service, the reduced number of ADEs and related health care encounters would confer a benefit to society.
A sensitivity analysis was performed to determine whether this service would still confer cost-savings potential if both ADE cost and probability of harm based on ADE severity were varied from the original estimates. Estimates for ADE cost and likelihood of ADE occurring were decreased proportionally to provide a more conservative cost impact amount as well as to determine the point at which providing this service would be cost neutral (ie, when pharmacy expenses equaled cost avoidance) to society.
Categorical data were evaluated using Fisher’s exact and chi-square tests; continuous data were evaluated using t tests. P values of less than .05 were considered significant.
Results
During the study period, the pharmacists were contacted for 77 patients. Ten patients (13%) were not able to have discharge verification secondary to incomplete or absent orders or the pharmacist being unable to verify orders prior to the patient leaving the hospital. For the remaining 67 patients, admission and discharge medication verification was performed by pharmacy residents the majority of the time (76%), while clinical pharmacists performed or supervised the remaining 24%. Out of these, 84 errors were identified, with a mean 1.25 ± 2.04 errors per patient. A range of 0 to 6 errors were identified per patient. Fifty-five of these errors were corrected with a phone call to the provider prior to the patient’s discharge. The remaining errors were resolved by communication with the nurse or with a for-your-information (FYI) page to the provider, which did not require a call back. Tables 1 and 2 display the admission and discharge medication reconciliation characteristics, respectively. As noted in Table 1, admission medication reconciliation documentation was complete for 40% (27/67) of patients. Table 3 further describes the errors identified.
Table 1. Admission medication reconciliation patient characteristics.
| Characteristics | Surgery patients (n = 34) | Medicine patients (n = 33) | P |
| Patient admitted via emergency department | 7 (21) | 22 (67) | .0002 |
| Medication history and reconciliation documented by prescriber | 29 (85) | 30 (91) | .71 |
| MREC form signed by prescriber within 24 hours | 19 (66) | 24 (80) | .2 |
| MREC complete (not missing strength, frequency, or route) | 13 (38) | 14 (46) | .81 |
| MREC performed by prescriber in Epic | 3 (10) | 7 (23) | .19 |
| Home medication list available in Epic | 21 (72) | 24 (80) | .44 |
| Home medication list in Epic matches MREC documentation | 7 (33) | 5 (17) | .75 |
| No. of home medications, mean ± SD | 7.8 ± 6.2 | 8.7 ± 5.4 | .53 |
| Patients with >10 home medications | 11 (38) | 16 (53) | 1.00 |
| Errors identified by pharmacists at discharge | 57 | 42 | 1.00 |
Note: Results reported as n (%) unless otherwise noted. Categorical data was evaluated using Fisher’s exact and chi-square tests and continuous data was evaluated using t tests. MREC = medication reconciliation.
Table 2. Discharge medication reconciliation patient characteristics.
| Characteristics | Surgery patients (n = 34) | Medicine patients (n = 33) | P |
| MREC form signed and dated | 30 (88) | 30 (91) | 1.00 |
| Number of discharge medications, mean ± SD | 10 ± 6 | 9.6 ± 5 | .77 |
| Patients with >10 discharge medications | 16 (47) | 16 (47) | 1.00 |
| Patients with errors on MREC | 22 (65) | 15 (45) | .14 |
| Errors identified by pharmacists | 48 | 36 | |
| No. of errors per patient, mean ± SD | 1.4 ± 1.4 | 1.1 ± 2.6 | .53 |
| Phone call to provider required to resolve errors | 16 (47) | 13 (39) | .47 |
| Errors corrected following phone call | 30 (63) | 25 (69) | .18 |
| Time in minutes required for MREC verification, mean ± SD | 20 ± 12 | 14 ± 14 | .06 |
Note: Results reported as n (%) unless otherwise noted. Categorical data was evaluated using Fisher’s exact and chi-square tests and continuous data was evaluated using t tests. MREC = medication reconciliation.
Table 3. Discharge medication errors identified.
| Medication error categories | Errors in surgery patients (n = 48) | Errors in medicine patients (n = 36) |
| Chronic disease state management | 21 (43) | 15 (42) |
| Antimicrobial | 10 (21) | 3 (8) |
| Analgesic | 7 (15) | 3 (8) |
| Hypertension agent | 6 (13) | 6 (17) |
| Anticoagulant | 2 (4) | 2 (6) |
| Diabetes agent | 2 (4) | 4 (11) |
| Discharge MREC unavailable | 0 | 3 (8) |
Note: Results reported as n (%). MREC = medication reconciliation.
The medication reconciliations required a median of 15 minutes to perform, with a range of 5 to 60 minutes. Table 4 shows the types of discharge medication errors identified by pharmacists during the study. The majority of these errors were related to failure to restart or inappropriate initiation of medications for chronic disease state management or antimicrobial choice or dose.
Table 4. Severity of errors identified at discharge.
| Severity (cost avoidance estimate a) | Errors in surgery patients (n = 48) | Errors in medicine patients (n = 36) |
| Lethal ($3,000/error) | 0 | 0 |
| Serious ($2,000/error) | 3 | 2 |
| Significant ($500/error) | 39 | 24 |
| Minor ($50/error) | 6 | 10 |
| No harm to patient | 0 | 0 |
Calculated as product of average cost of adverse drug event (ADE) ($5,000) and likelihood of ADE occurring based on error severity.
Six percent of the errors (5/84) were deemed to be serious; 75% (63/84) and 19% (16/84) were considered to be significant and minor, respectively (Table 4). No errors were considered to be potentially lethal or to cause no harm to the patient. Based on error severity and potential to cause ADEs, cost avoidance for this study was estimated to be $42,300. By extrapolating these results for the entire adult population at this institution (estimated 26,000 adult discharges annually), cost avoidance was estimated to be $16,415,000 due to a hypothetical reduction in medication errors.
Seven-day readmission rates in the study cohort were similar to the historical control group (P = 1.00). The 30-day readmission rates were numerically lower in the study cohort (P = .86) (Table 5).
Table 5. Readmission rates.
| Readmission | Control cohort (n = 259) July – August 2013 | Study cohort (n = 67) September – October 2013 | P value |
| 7-day | 19 (7.4%) | 5 (7.5%) | 1.00 |
| 30-day | 51 (19.8%) | 12 (18%) | .86 |
Note: Categorical data was evaluated using Fisher’s exact and chi-square tests and continuous data was evaluated using t tests.
In total, the pharmacist discharge medication verification for the study cohort took 21.6 hours. Based on institutional salaries for clinical pharmacy specialists and pharmacy residents in 2013, the cost to the pharmacy department was a mean of $9 for each verification. Therefore, total annual salary cost based on estimated 26,000 adult discharges is $234,000, resulting in a net savings of $16,181,000 annually based on error avoidance.
Results of the sensitivity analysis (Table 6) suggest that this service would be financially advantageous to the institution even when average costs of an ADE and estimates of error probability were decreased considerably from the base case estimate. Given the salary cost of approximately $9 per patient during the pilot phase, both estimated costs of an ADE and the likelihood of an ADE occurring for each of the various error severity categories would have to be approximately 12% of base case estimates for this service to be cost-neutral (ie, a cost:benefit ratio of 1:1).
Table 6. Cost sensitivity analysis.
| Likelihood of ADE occurring based on error severity | ||||||
| Cost of ADE | Lethal | Serious | Significant | Minor | Total savings | Savings per patient |
| $5,000 | 60% | 40% | 10% | 1% | $42,300 | $631 |
| $4,000 | 48% | 32% | 8% | 0.8% | $32,112 | $479 |
| $3,000 | 36% | 24% | 6% | 0.6% | $15,228 | $227 |
| $2,000 | 24% | 16% | 4% | 0.4% | $6768 | $101 |
| $1,000 | 12% | 8% | 2% | 0.2% | $1692 | $25 |
| $600 | 7.2% | 4.8% | 1.2% | 0.12% | $610 | $9 |
Note: ADE = adverse drug event.
Discussion
The pharmacist’s ability to decrease medication errors through medication reconciliation has been well documented in previous studies.1,7–14 However, it is still debated whether the pharmacist intervention is more effective at admission or discharge, and it is not certain which patients should receive pharmacist assessment. Additionally, the role of pharmacy students, residents, and technicians in making significant interventions during medication reconciliation has yet to be fully determined.
Because of time constraints, pharmacists may not be able to review or perform medication reconciliation on both admission and discharge. This prospective study focused on discharge reconciliation, because this transition of care allows for a comprehensive review of the entire hospital course in a timely manner and errors at discharge can be one of the most concerning aspects of incorrect medication reconciliation.7–10 Few studies have examined the role of pharmacists in performing medication reconciliation at the time of discharge. Vira et al9 conducted a study reviewing the role of pharmacists completing reconciliation at admission and then counseling patients on discharge. On admission, pharmacists found a median of 1 variance per patient (n = 60) with 20 clinically significant variances that could have led to patient harm. However, at the time of discharge, pharmacists found that 43% still had variances on their discharge orders, 10 of which were clinically significant. Newman et al10 also conducted a study reviewing the role of pharmacist medication reconciliation at the time of discharge. In that study, pharmacists were integrated into a preexisting discharge process in which they could review the entire hospital course for patients with psychosis or mood disorders. Pharmacists performed a chart review and physically examined any medications brought in by the patients. They contacted physicians to correct any errors and counseled all patients prior to discharge. Pharmacists found a mean of 2.14 variances per patient, though the investigators did not comment on the significance of the interventions. Furthermore, patient counseling was included in the interventions, along with the identification of medication discrepancies. The largest constraint of this study was the time to complete the entire discharge process, which was 57 minutes.
Unlike the previous studies, pharmacists in our study made clinically significant and serious interventions that were rated based on a validated severity scale. These interventions were made after conducting medication reconciliation only at the time of discharge and without interviewing all patients. Physicians are primarily responsible for the medication reconciliation process at our institution, so pharmacists were able to contribute to the process without repeating the physician’s work. The median time of medication reconciliation was 15 minutes (range, 5-60 minutes), which demonstrates the pharmacist’s ability to ensure that patients were leaving on the appropriate regimens in a time efficient manner. Discharge errors that lead to patient harm are one of the largest concerns with inaccurate medication reconciliation. However, pharmacist interventions in this study could have contributed to increased patient safety, although the results did not show a significant difference in readmission rates.
Larger studies have found that pharmacist interventions in the postdischarge setting have led to a decrease in readmission rates. Jack et al13 conducted one of the only prospective randomized trials to evaluate a discharge process that included postdischarge medication reconciliation by pharmacists. In that study, a nurse facilitated the discharge, and pharmacists followed up with patients 2 to 4 days after discharge by phone call. Investigators found that the discharge process decreased hospital utilization in the following 30 days, which resulted in an estimated $149,995 in cost savings secondary to this decrease in readmission. Similarly, a retrospective study reviewed the role of pharmacists in decreasing costs and readmission rates by performing medication reconciliations after discharge.14 Pharmacists in an ambulatory setting contacted high-risk patients 3 to 7 days after discharge to discuss medication changes and determine discrepancies. If any variances existed, the pharmacists would contact the primary care provider to address the concerns. Similar to our study, investigators performed a cost analysis based on the severity of interventions and found a potential cost savings of $35,478 for 243 medication reconciliations. Although these studies produced promising results, there are some limitations in the postdischarge setting. Pharmacists may not be able to contact patients without telephone access, and depending on the severity of the medication error, the time lapse between discharge and pharmacist intervention could potentially lead to serious adverse effects. Therefore, our study supports the inclusion of pharmacists in the discharge process through their review of patient records.
In addition to the uncertainty about the timing of the pharmacist intervention, it can be difficult to determine which patients should receive pharmacist screening. Many studies have limited pharmacist intervention to high-risk populations that could have more difficult regimens and be at higher risk for medication errors. Buckley et al1 limited pharmacist intervention to patients with a 30-day readmission; diagnosis of acute myocardial infarction, heart failure, or anticoagulation; concomitant clopidogrel and aspirin; or greater than 2 of the following disease states: end-stage renal disease diabetes mellitus, hypertension, or chronic obstructive pulmonary disease (though this criteria was arbitrarily defined). In a study by Vira et al,9 pharmacist intervention was performed if specifically requested by a physician. Clinical pharmacists chose additional patients, if time permitted, from discharges involving patients with extended lengths of stay, multiple co-morbidities, and/or multiple medications or medication changes. Finally, Kilcup14 allowed physicians to assess which patients could benefit from pharmacist review and counseling. All of these studies believed that pharmacists would be of most benefit in a high-risk patient population, because time to perform reconciliation would be a constraint. In contrast, our study reviewed all patients discharged within the day shift regardless of service or type of admission. This pilot project showed that surgery patients who would not have met inclusion criteria in prior studies still had complicated medication regimens and just as many errors as patients on the medicine service. The lack of difference between the 2 services suggests that pharmacist medication reconciliation provides value for all types of admissions, even those patients scheduled for a routine procedure or a simple admission. Therefore, pharmacist review should be considered for all patients and not solely those deemed as high risk.
A potential barrier to the implementation of a pharmacist discharge medication reconciliation process for all patients is the time required by a pharmacist. In previous studies, pharmacist medication reconciliation at discharge or immediately following discharge took a mean time of 42 to 57 minutes.10,13 In this study, the median time to complete a medication review was 15 minutes. The difference in median time spent could be due to the differences in the actual process; in our study, pharmacists were supplementing the medication reconciliation process instead of performing it as in other studies.1,9,10 By simply reviewing the 3 medication lists (admission, inpatient, and discharge), pharmacists made significant interventions in a more timely manner. However, it is important to note that some medication reconciliations took up to 60 minutes. Although these are outliers, this time commitment could still have a significant impact on a pharmacist’s daily workflow. Although re-allocation of pharmacist’s time and duties may be inconvenient, the benefit of improved patient care should not be ignored. Pharmacists have a unique role as medication experts, and improved patient care has been demonstrated through pharmacist interventions.1, 8–14 Of note, although the pharmacists performing the audits in this study were not familiar with the entire hospital course for the patients of interest, they were still able to identify many significant interventions. Other studies reviewing pharmacist postdischarge reconciliation show that pharmacists without full knowledge of the hospital course can still make significant safety impacts and decrease hospital utilization.13,14 Even though a pharmacist who is more familiar with the patient’s history would be much more likely to detect meaningful discrepancies, pharmacists who do not have this knowledge can make meaningful interventions based solely on their abilities as medication experts. Therefore, medication reconciliation should not be limited to rounding pharmacists associated with care teams.
Another possible challenge to the initiation of a discharge medication reconciliation process could be the costs involved with the model. There was a mean cost of $9 per medication reconciliation verification based on the time to complete verifications and the institutional salaries for clinical pharmacy specialists and pharmacy residents involved. Prior studies have shown similar costs with an estimated $11 per medication reconciliation.9 Based on an estimated 26,000 annual discharges, implementation of medication reconciliation verification institutionally would lead to an annualized cost estimate of $234,000. This equates to several full-time equivalent (FTE) employees at our institution and likely at most institutions. However, the net cost avoidance of this study, based on the estimates for avoidable adverse medication events and labor costs, resulted in a financial benefit of $42,300 with a projected annual cost avoidance of $16,181,000. To help further offset costs, the role of pharmacy residents, students, and even technicians should be considered. In our study, residents and students were able to recognize potential errors and increase patient safety. Furthermore, Buckley et al1 showed that technicians with adequate training could perform patient interviews to determine discrepancies, which allowed pharmacists to focus on resolving the errors. By utilizing all members of the pharmacy department, institutions could implement an extensive cost-savings project. Further, as there was a numerically lower readmission rate in the study group, the medication reconciliation interventions may represent an important development in reimbursement based on clinical outcomes, patient satisfaction, and value-based purchasing.
As this was a nonrandomized pilot study, there are a few limitations. Due to the nature of the study, we were only able to perform medication reconciliations on 2 inpatient units and this was only done on weekdays. This pilot design limited our duration and sample size, which may have led to type II error, particularly in regard to differences in readmission rates. There were fewer readmissions in the pharmacist discharge group and larger studies from a postdischarge perspective have shown a significant decrease in hospital utilization, so it is our belief that enrolling more patients could potentially lead to a significant decrease in readmissions. Therefore, the lack of significance between the 2 groups could have been a false negative result. Additionally, investigator bias could have played a role, as different investigators may have interpreted the severity of errors differently. However, the pharmacist who scored the interventions was independent from the medication reconciliation verifications and used a validated severity scale that therefore helped to minimize bias.11 The use of a validated scale to help fully assess the benefits provided by pharmacist intervention is only one of the many strengths of this study. This prospective study directly assessed pharmacist interventions on both clinical and financial outcomes based on validated scales. This allows for appropriate evaluation of the clinical and financial implications of implementation of a pharmacist discharge reconciliation program.
Conclusion
Pharmacists involved in the discharge process identified numerous errors on both the admission medication reconciliation and discharge orders. Many of these interventions were significant and could have prevented a readmission, particularly those related to antimicrobials, anticoagulation, and chronic disease state management. Pharmacist involvement in the discharge process can improve patient safety and result in cost avoidance for institutions. Broader implementation of this or similar interventions may significantly impact 7- and 30-day readmission rates.
Acknowledgments
The authors declare no conflicts of interest.
References
- 1.Buckley MS, Harinstein LM, Clark KB, et al. Impact of a clinical pharmacy admission medication reconciliation program on medication errors in “high-risk” patients. Ann Pharmacother. 2013; 47(12):1599–1610. [DOI] [PubMed] [Google Scholar]
- 2.Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: A systematic review. CMAJ. 2005;173(5):510–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomsen LA, Winterstein AG, Søndergaard B, Haugbølle LS, Melander A. Systematic review of the incidence and characteristics of preventable adverse drug events in ambulatory care. Ann Pharmacother. 2007;41:1411–1426. [DOI] [PubMed] [Google Scholar]
- 4.Hospital consumer assessment of healthcare providers and systems. Hospital survey. http://www.hcahpsonline.org Accessed September16, 2013.
- 5.Centers for Medicare & Medicaid Services. Hospital consumer assessment of healthcare providers and systems. http://www.cms.gov/Regulations-and-Guidance/Legislation/CFCsAndCoPs/Hospitals.html Accessed September16, 2013. [DOI] [PMC free article] [PubMed]
- 6.The Joint Commission. National patient safety goals. 2013. http://www.jointcommission.org/assets/1/18/NPSG_Chapter_Jan2013_HAP.pdf Accessed September16, 2013.
- 7.Forster AJ, Murff HJ, Peterson JF, et al. Incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161–167. [DOI] [PubMed] [Google Scholar]
- 8.Cornu P, Steubaut S, Leysen T, et al. Effect of medication reconciliation at hospital admission on medication discrepancies during hospitalization and at discharge for geriatric patients. Ann Pharmacother. 2012;46:484–494. [DOI] [PubMed] [Google Scholar]
- 9.Vira T, Colquhoun M, Etchells E. Reconcilable differences: Correcting medication errors at hospital admission and discharge. Qual Saf Health Care. 2006;15:122–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Newman D, Haight R, Hoeft D. Implementation and impact of pharmacists led medication reconciliation and patient education at discharge from an inpatient behavior health unit. Ment Health Clin. 2013;3(1):96. [Google Scholar]
- 11.Overhage JM, Lukes A. Practical, reliable, comprehensive method for characterizing pharmacists’ clinical activities. Am J Health Syst Pharm. 1999;56:2444–2450. [DOI] [PubMed] [Google Scholar]
- 12.Nesbit TW, Shermock KM, Bobek MB, et al. Implementation and pharmacoeconomic analysis of a clinical staff pharmacist practice model. Am J Health Syst Pharm. 2001;58:784–790. [DOI] [PubMed] [Google Scholar]
- 13.Jack BW, Chetty VK, Anthony D, et al. Reengineered hospital discharge program to decrease rehospitalization. Ann Intern Med. 2009;150(3):178–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kilcup M, Schultz D, Carlson J, et al. Postdischarge pharmacist medication reconciliation: Impact on readmission rates and financial savings. J Am Pharm Assoc. 2013;53:78–84. [DOI] [PubMed] [Google Scholar]