Abstract
Background
The adjustment of plantarflexion resistive moment of an articulated ankle-foot orthosis is considered important in patients post stroke, but the evidence is still limited. Therefore, the aim of this study was to investigate the effect of changing the plantarflexion resistive moment of an articulated ankle-foot orthosis on ankle and knee joint angles and moments in patients post stroke.
Methods
Gait analysis was performed on 10 subjects post stroke under four different plantarflexion resistive moment conditions using a newly designed articulated ankle-foot orthosis. Data were recorded using a Bertec split-belt instrumented treadmill in a 3-dimensional motion analysis laboratory.
Findings
The ankle and knee sagittal joint angles and moments were significantly affected by the amount of plantarflexion resistive moment of the ankle-foot orthosis. Increasing the plantarflexion resistive moment of the ankle-foot orthosis induced significant decreases both in the peak ankle plantarflexion angle (P<0.01) and the peak knee extension angle (P<0.05). Also, the increase induced significant increases in the internal dorsiflexion moment of the ankle joint (P<0.01) and significantly decreased the internal flexion moment of the knee joint (P<0.01).
Interpretation
These results suggest an important link between the kinematic/kinetic parameters of the lower-limb joints and the plantarflexion resistive moment of an articulated ankle-foot orthosis. A future study should be performed to clarify their relationship further so that the practitioners may be able to use these parameters as objective data to determine an optimal plantarflexion resistive moment of an articulated ankle-foot orthosis for improved orthotic care in individual patients.
Keywords: AFO, gait disorders, orthotic devices, stiffness, kinetics, kinematics
Introduction
Stroke is a major cause of gait disabilities and ankle-foot orthoses (AFOs) are commonly prescribed to address issues related to hemiplegic gait, such as foot-drop and medio-lateral instability (de Wit et al., 2004; Gok et al., 2003). Gait disabilities in patients with a history of stroke may result from impairment in motor coordination, muscle strength, restriction in joint range of motion, spasticity and/or deterioration in sensitivity. Increased dorsiflexion resistive moment of the affected ankle joint due to spastic hypertonia is common in this group of patients (Kobayashi et al., 2010). Thus, the mechanical properties of AFOs, such as the resistive moment and alignment (i.e. initial angle), need to accommodate these impairments and be customizable for each patient based on objective clinical data. Currently, AFOs are provided to the patients based on subjective physical exam data and visual observations of gait deficits by practitioners in the clinical setting. This could potentially lead to improper fit, malalignment, discomfort, and ultimately diminished mobility.
The resistive moment of an AFO plays an important role in assisting gait in patients with stroke. Various measurement techniques have been developed to quantify the resistive moments of AFOs (Kobayashi et al., 2011b). Plantarflexion resistive moment resists an ankle moving in a plantarflexion direction, while dorsiflexion resistive moment resists the ankle moving in a dorsiflexion direction. The plantarflexion resistive moment plays an important role to achieve heel strike in the first rocker of stance (Yamamoto et al., 2009), and preservation of the first rocker is an import function for an AFO (Nolan and Yarossi, 2011). However, limited evidence exists regarding the effect of changing the magnitude of the plantarflexion resistive moment of an articulated AFO on hemiplegic gait in individuals post stroke.
It has been suggested that varying the plantarflexion resistive moment of articulated AFOs will affect kinematics and kinetics of lower-limb joints while walking in patients with stroke (Singer et al., 2014; Yamamoto et al., 2013). These studies implied the importance of tuning the plantarflexion resistive moments for individual patients. To achieve this, the plantarflexion resistive moment may need to be adjustable without affecting dorsiflexion resistive moment. This is only possible with an articulated AFO with a special joint, such as an oil-damper joint (Yamamoto et al., 2005). Findings from the studies using non-articulated AFOs may not be directly applicable to articulated AFOs. Some studies suggested that the effect of non-articulated AFO’s resistive moment on overall walking performance might be minimal in patients with ankle muscle weakness due to various limb salvage procedures (Harper et al., 2014; Russell Esposito et al., 2014). However, the resistive moment of a non-articulated AFO is generally adjusted by trimming its material or exchanging its component. As a result, both dorsiflexion and plantarflexion resistive moments are affected, and it is impossible to adjust them independently. Therefore, it may be ideal to investigate the effect of plantarflexion resistive moment using an articulated AFO in which the plantarflexion resistive moment can be changed independent of the dorsiflexion resistive moment.
Studies that investigated the effects of AFOs on hemiplegic gait generally overlooked “resistive moment” characteristics of the AFOs. Characterizing resistive moment of AFOs is important to interpret their effects on gait (Bregman et al., 2010; Kobayashi et al., 2011a; Yamamoto et al., 1993). One way to investigate the effect of plantarflexion resistive moment of AFOs on hemiplegic gait is to change the resistive moment. Therefore, the aim of this study was to investigate the effect of systematically changing the plantarflexion resistive moment of an articulated AFO on ankle and knee joint angles and moments in patients post stroke presenting with hemiplegic gait. To accomplish this, a new articulated AFO was developed that could provide varying levels of plantarflexion resistive moment. We hypothesized that both ankle and knee joint angles and moments would be significantly affected by changing the plantarflexion resistive moments of the AFO. The hypothesis focused on the ankle and knee joints because they were expected to be the two main lower-limb joints being affected by the AFO.
Methods
Participants
Ten subjects (2 females/8 males) with a history of stroke participated in this study. Their mean age was 56 (11) years old and mean time since stroke incidence was 6 (3) years. The mean body height was 1.76 (0.11) m and mean body mass was 99 (17) kg. All subjects had unilateral limb involvement (6 right/4 left). To be included in the study each subject had to be a minimum of 6-month post-stroke with hemiplegia and have the ability to walk safely on an instrumented treadmill with the use of an AFO and without a walking aid. Subjects were excluded if they had confounding injury or any musculoskeletal or cognitive problems that would limit the ability to walk on the instrumented treadmill. After informed consent was obtained for this Institutional Review Board approved study, the following clinical tests were performed on each subject: 1) Modified Ashworth Scale (MAS) (Bohannon and Smith, 1987), 2) Timed-up and Go Test (TUG) (Podsiadlo and Richardson, 1991), 3) Manual muscle testing (MMT) of ankle and knee joints (Kendall et al., 1993), and 4) Measurement of manual passive peak dorsiflexion angle (i.e. range of motion: ROM) while the knee joint kept in extension in the supine position.
New articulated ankle-foot orthosis
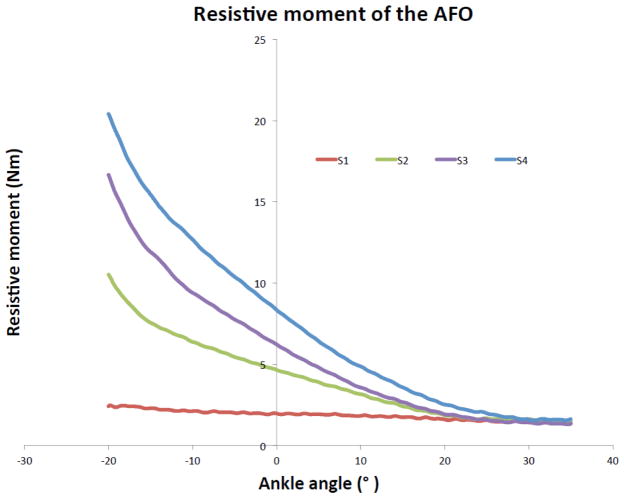
The new articulated AFO developed for this study had an adjustable plantarflexion resistive moment. Adjustments were accomplished by exchanging a steel spring resulting in different spring rates (Figure 1). The mass of the AFO including the sandal was 1 kg. The spring only generated plantarflexion resistive moment at the ankle, and the AFO did not have any spring induced dorsiflexion resistive moment. Thus, the AFO was classified as an articulated AFO with adjustable plantarflexion resistive moment. The resistive moment of the AFO was measured under 4 different spring conditions (S1, S2, S3 and S4) with a custom automated device used in an earlier study (Gao et al., 2011). The S1 was a baseline condition where no steel spring was installed on the AFO, and it represented an AFO with a minimum resistive moment. The resistive moment was measured at an angular velocity of 3°/s with a sampling frequency of 100Hz. The resistive moment and angular position data were filtered using a fourth-order zero-lag low pass Butterworth filter with a cutoff frequency of 5Hz. The ankle angle – resistive moment relationship while the AFO being plantarflexed from 35° of dorsiflexion to 20° of plantarflexion (i.e. an ascending limb of a hysteresis curve) was plotted (Figure 2). The mean plantarflexion resistive moment of 4 measurements was calculated for the different spring conditions at 0°, 5°, 10°, 15° and 20° of plantarflexion angles (Table 1).
Figure 1.
The new articulated ankle-foot orthosis.
Figure 2.
The ankle angle – resistive moment relationship of the articulated ankle-foot orthosis measured by a custom automated device (Gao et al., 2011).
Table 1.
Plantarflexion resistive moments (Nm) of the articulated AFO derived from a custom automated device (Gao et al., 2011) across five plantarflexed positions of the AFO.
| Spring condition | Ankle angle position | ||||
|---|---|---|---|---|---|
| 0° | 5° PF | 10° PF | 15° PF | 20° PF | |
|
| |||||
| Mean (SD) (Nm) | |||||
| S1 | 1.98 (0.05) | 2.01 (0.02) | 2.12 (0.01) | 2.32 (0.11) | 2.41 (0.01) |
| S2 | 4.67 (0.06) | 5.46 (0.06) | 6.39 (0.07) | 7.58 (0.06) | 10.49 (0.04) |
| S3 | 6.25 (0.04) | 7.79 (0.05) | 9.44 (0.05) | 11.97 (0.11) | 16.81 (0.23) |
| S4 | 8.29 (0.12) | 10.30 (0.15) | 12.61 (0.16) | 15.39 (0.17) | 20.35 (0.13) |
Abbreviations: PF, plantarflexion; SD, standard deviation
Gait analysis
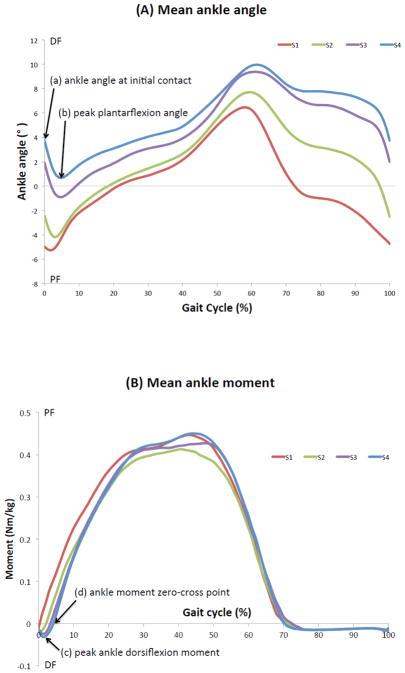
Each subject was fit with the articulated AFO, and reflective markers were placed based on a modified Cleveland Clinic Marker Set defining 8 segments (2 feet, 2 shanks, 2 thighs, 1 pelvis, and 1 HAT (head, arm, and trunk)). The anatomical landmarks where the markers were placed included: acromion processes, sternum, 10th thoracic vertebrae, anterior and posterior superior iliac spines, medial and lateral epicondyle of the femur, medial and lateral malleoli, calcaneus and head of the 2nd and 5th metatarsals. For the limb with the AFO, markers were placed directly on the AFO to prevent them from being obscured by the straps and bars of the AFO. The ankle joint of the AFO was aligned with the anatomical ankle joint. Because the AFO was securely attached to the shank, dynamic tracking was accomplished using a rigid cluster that was attached directly to the AFO above the ankle joint (Figure 1). The initial angular position of the AFO (i.e. an angular position at which the steel spring starts to be engaged to generate a plantarflexion resistive moment) as well as the heel height of the sandal were kept constant across the subjects (Figures 1 and 2). Therefore, this study was solely aimed to investigate the effect of the changes in the plantarflexion resistive moment of the AFO on gait parameters of interest. Each subject was secured in a harness and walked at a comfortable walking speed, which ranged from 0.15 m/s to 0.27 m/s [Mean: 0.22 (0.04) m/s], on a Bertec split-belt instrumented treadmill (Bertec corporation, Columbus, OH, USA). Data were recorded during 4 separate trials using 4 different spring conditions. For the same subject the identical speed was set on the treadmill for all spring conditions. The order of spring conditions (S1, S2, S3 and S4) was randomized for the walking trials. Gait data were acquired using a Vicon 10-camera motion analysis system (Vicon Motion Systems, Oxford, UK) and the instrumented treadmill at a rate of 200Hz for 5 successful steps of the leg with AFO. Each subject was given a short acclimatization period to walk on the treadmill under each spring condition before the data collection. Data were recorded and synchronized using Vicon Nexus (Vicon Motion Systems, Oxford, UK) and postprocessed using Visual3D (CMotion, Germantown, MD, USA). Marker and force platform data were filtered using a low pass, zero-phase shift Butterworth filter at 6 Hz and 20 Hz, respectively (Winter, 2005). The ankle and knee joint moments were normalized to each subject’s body mass (Nm/kg). The ankle and knee joint angles and moments of 5 steps of the leg with AFO were averaged and normalized to a gait cycle for each spring condition in each subject and they were subsequently averaged for the 10 subjects and were plotted (Figures 3 and 4).
Figure 3.
The effect of the changes in plantarflexion resistive moments of the articulated ankle-foot orthosis on the (A) mean ankle joint angles and (B) mean ankle joint moments in a gait cycle. Dorsiflexion angles and plantarflexion moments were defined as positive for the ankle joint.
Abbreviations: DF, dorsiflexion; PF, plantarflexion
Figure 4.
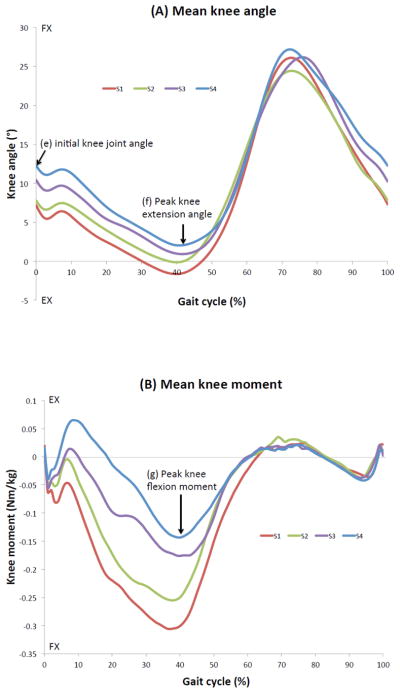
The effect of the changes in plantarflexion resistive moments of the articulated ankle-foot orthosis on the (A) mean knee joint angles and (B) mean knee joint moments in a gait cycle. Knee flexion angles and knee extension moments were defined as positive for the knee joint.
Abbreviations: EX, extension; FX, flexion
The following gait parameters of the affected lower-limb were extracted from the post-processed data (Figures 3 and 4): 1) (a) ankle angle at initial contact, (b) peak ankle plantarflexion angle, (c) (internal) peak ankle dorsiflexion moment, (d) ankle moment zero-crossing point [i.e. % of gait cycle when (internal) dorsiflexion moments change to (internal) plantarflexion moments] and (e) initial knee joint angle in the first rocker of stance, and 2) (f) peak knee extension angle and (g) (internal) peak knee flexion moment in the second rocker of stance. The moment parameters are described as “internal” moments throughout this work.
Statistical analysis
The baseline condition (S1) was compared to each of the other spring conditions (S2, S3 and S4) for the joint angle and moment parameters utilizing 2-tailed paired t-tests with Stata/IC 11.1 (STATA Corp, College Station, USA). No statistical comparisons were performed among spring conditions: S2, S3, and S4 because the hypothesis test focused on the changes from the baseline (S1) condition. Means, standard deviations and 95% confidence intervals of each joint angle and moment parameter of the 10 subjects were calculated. Statistical significance was set at P = 0.05. P-values were adjusted for multiple comparisons using the Tukey-Ciminera-Heyse procedure (Sankoh et al., 1997; Tukey et al., 1985).
Results
Clinical assessment outcomes
The outcome of each clinical assessment for this cohort of 10 subjects was as follows: 1) The MAS ranged from 1+ to 3; 2) The TUG ranged from 10.62 to 27.00 seconds and its mean (standard deviations) was 17.72 (5.13) seconds; 3) The MMT of the ankle plantarflexors ranged from 0 to 4, the MMT of the ankle dorsiflexors ranged from 0 to 4, the MMT of the knee extensors ranged from 3+ to 5, and the MMT of the knee flexors ranged from 2+ to 5; 4) The manual passive peak dorsiflexion angle while the knee joint kept in extension ranged from −11 to 10° of dorsiflexion.
Plantarflexion resistive moment of the AFO
For each spring condition, the ankle angle-resistive moment relationship is presented in Figure 2. The plantarflexion resistive moment from 0 to 20° of plantarflexion with 5° of increments is presented in Table 1. The plantarflexion resistive moment of the AFO ranged from 1.98 to 8.29 Nm at 0° and from 2.41 to 20.35 Nm at 20° of plantarflexion.
Ankle joint angles and moments
The mean ankle joint angles and moments of the 10 subjects under each spring condition in a gait cycle are presented in Figure 3A and B, respectively. The mean and 95% confidence interval of each extracted ankle joint parameter are presented in Table 2. Significant differences were found in all the ankle joint parameters. Each ankle joint parameter generally demonstrated a systematic response to the changes in the spring conditions of the AFO. The mean peak ankle plantarflexion angle at each spring condition was as follows: −5.25 (4.82) ° at S1, −4.18 (4.51) ° at S2, −0.89 (6.17) ° at S3 (P<0.01) and 0.69 (5.28) ° at S4 (P<0.01), while the mean ankle moment zero-cross point at each spring condition was as follows: 1.60 (1.58) % at S1, 3.50 (2.37) % at S2 (P<0.05), 5.30 (3.50) % at S3 (P<0.01), and 6.60 (4.43) % at S4 (P<0.01).
Table 2.
Ankle and knee joint angle and moment parameters under each spring condition
| Gait parameters | S1 Mean (SD) |
95% CI | S2 Mean (SD) |
95% CI | S3 Mean (SD) |
95% CI | S4 Mean (SD) |
95% CI |
|---|---|---|---|---|---|---|---|---|
| (a) Ankle angle at initial contact (°) | −4.97 (4.64) | −8.29, −1.65 | −2.43 (3.59)* | −5.00, 0.14 | 1.92 (4.65)† | −1.41, 5.24 | 3.74 (3.69)† | 1.10, 6.38 |
| (b) Peak ankle plantarflexion angle (°) | −5.25 (4.82) | −8.70, −1.80 | −4.18 (4.51) | −7.41, −0.96 | −0.89 (6.17)† | −5.30, 3.52 | 0.69 (5.28)† | −3.08, 4.47 |
| (c) Peak ankle dorsiflexion moment (Nm/kg) | −0.01 (0.01) | −0.02, 0.00 | −0.02 (0.01) | −0.03, −0.01 | −0.02 (0.02) | −0.04, −0.01 | −0.03 (0.02)† | −0.04, −0.02 |
| (d) Ankle moment zero-cross point (% GC) | 1.60 (1.58) | 0.47, 2.73 | 3.50 (2.37)* | 1.81, 5.19 | 5.30 (3.50)† | 2.80, 7.80 | 6.60 (4.43)† | 3.43, 9.77 |
| (e) Knee angle at initial contact (°) | 7.20 (5.52) | 3.25, 11.15 | 7.79 (5.88) | 3.58, 12.00 | 10.43 (5.98)* | 6.15, 14.71 | 12.27 (5.10)† | 8.62, 15.92 |
| (f) Peak knee extension angle (°) | −1.64 (11.51) | −9.87, 6.60 | −0.12 (11.43)* | −8.30, 8.05 | 0.92 (11.13)* | −7.04, 8.88 | 2.03 (11.39) | −6.11, 10.18 |
| (g) Peak knee flexion moment (Nm/kg) | −0.31 (0.41) | −0.60, −0.01 | −0.26 (0.40) | −0.54, 0.03 | −0.18 (0.36)† | −0.44, 0.08 | −0.14 (0.39)* | −0.43, 0.14 |
An asterisk (*) indicates significant difference at P<0.05 from the S1 condition, while a cross (†) indicates significant difference at P<0.01 from the S1 condition. Dorsiflexion angles and plantarflexion moments were defined as positive for the ankle joint, while knee flexion angles and knee extension moments were defined as positive for the knee joint.
Abbreviations: 95% CI, 95% confidence interval; GC, gait cycle; SD, standard deviation
Knee joint angles and moments
The mean knee joint angles and moments of the 10 subjects under each spring condition in a gait cycle are presented in Figure 4A and B, respectively. The mean and 95% confidence interval of each extracted knee joint parameter are presented in Table 2. Significant differences were found in all the knee joint parameters. Each knee joint parameter generally demonstrated a systematic response to the changes in the spring conditions of the AFO. The mean peak knee extension angle at each spring condition was as follows: −1.64 (11.51) ° at S1, −0.12 (11.43) ° at S2 (P<0.05), 0.92 (11.13) ° at S3 (P<0.05) and 2.03 (11.39) ° at S4, while the mean peak knee flexion moment at each spring condition was as follows: −0.31 (0.41) Nm/kg at S1, −0.26 (0.40) Nm/kg at S2, −0.18 (0.36) Nm/kg at S3 (P<0.01), and −0.14 (0.39) Nm/kg at S4 (P<0.05).
Discussion
This study investigated the effect of the plantarflexion resistive moment of an articulated AFO on ankle and knee joint angles and moments in patients with a history of stroke. All of the examined ankle and knee parameters were significantly affected by changing the plantarflexion resistive moment of the AFO (Table 2). In addition, the ankle and knee joint angles and moments were, in general, affected very systematically (Figures 3 and 4). These results suggest an important relationship between these kinematic/kinetic parameters and the plantarflexion resistive moment of the AFO. Our previous work were either case series (Singer et al., 2014) or focused only on kinematics (Kobayashi et al., 2011a, 2013) using somewhat bulky experimental AFOs. This study is novel and important because both kinematic and kinetic parameters demonstrated statistically significant effects due to changes in the plantarflexion resistive moments using the new and compact articulated AFO in a group of 10 individuals post stroke. Once the relationship between the kinematic and kinetic parameters is more clearly defined in future studies, practitioners may be able to use these parameters as objective data to individualize the plantarflexion resistive moment of an articulated AFO to each patient.
AFOs are primarily provided to correct impairments related to the ankle joint. Ankle joint angles and moments are directly affected by the relationship between the strength of the individual’s ankle dorsiflexors/plantarflexors, their spasticity, the presence of a contracture, and the plantarflexion resistive moment of the AFO. Increases in the plantarflexion resistive moment of the AFO enabled the subjects to keep their ankle joint in a more dorsiflexed positions in early stance. This explains systematic changes in (a) the ankle angle at initial contact and (b) the peak ankle plantarflexion angle (Table 2; Figure 3A). The ankle joint moment presented in this study has contributions from 1) the anatomical ankle joint and 2) the plantarflexion resistive moment of the AFO. The plantarflexion resistive moments of the AFO complement the function of impaired dorsiflexors. Because the speed of the treadmill was kept constant under each spring condition for each subject, the change in (c) the peak ankle dorsiflexion moment is most likely from the changes in the magnitude of the plantarflexion resistive moment of the AFO (Table 2: Figure 3B). The higher the plantarflexion resistive moment of the AFO, the later the timing of foot-flat is expected in the first rocker of stance. The timing of foot-flat is related to (d) the ankle moment zero-crossing point. The foot-flat generally occurs just after the ankle moment zero-crossing point. This study demonstrated that increases in plantarflexion resistive moment could delay the timing of foot-flat in stance (Table 2: Figure 3B). This delay may reflect a more defined heel strike in the first rocker of stance.
Knee joint angles and moments are indirectly affected by the AFOs. Increased plantarflexion resistive moment of the AFO allowed the ankle joint to be kept in a more dorsiflexed position. This position caused the knee to be more flexed and anterior to the ground reaction force, resulting in a decreased (f) peak knee extension angle and (g) peak knee flexion moment. Among the 10 subjects, 6 subjects walked with their knee hyperextended during stance. This is why the mean knee angles and moments showed the characteristics of those with a hyperextended knee (Figure 4A and B). The excessive knee flexion moment is related to knee hyperextension and the development of knee recurvatum during gait, which can be a devastating sequelae post stroke. By increasing the plantarflexion resistive moment of the AFO, the amount of hyperextension at the knee was decreased, accompanied with deceases in the knee flexion moment. We also speculated that the increases in the flexion angles in (e) the initial knee joint angle was linked to the decreases in (f) the peak knee extension angle. These results strongly suggest that the AFOs would affect kinematics and kinetics of the knee joint in patients with stroke, and would reinforce the findings of the previous studies (Kobayashi et al., 2013; Singer et al., 2014).
When comparing to other literature, the common characteristic of our articulated AFO and the AFO with the oil-damper joint (Yamamoto et al., 2005) is that they both can provide adjustable plantarflexion resistive moments. However, some distinctive differences exist between the two AFO designs. The differences are as follows: 1) The resistive moments of our articulated AFO are induced by springs, while those of the oil-damper joints are by dampers that have velocity-dependent characteristics. 2) The initial angular position where the spring starts to get engaged to generate the plantarflexion resistive moment for our articulated AFO is approximately 30° of dorsiflexion (Figure 2) and this angle was kept constant across subjects in this study, while that of the oil-damper joint is about 0–8° of dorsiflexion. This means that our articulated AFO’s spring starts to engage much earlier than the oil-damper joint. 3) Both AFOs can generate about the same plantarflexion resistive moment (about 13 Nm) at 10° of plantarflexion. However, our AFO provides the plantarflexion moments gradually throughout the range, while the oil-damper joint provides them abruptly from the initial position. This means that the slope of angle-moment curve (i.e. stiffness) is steeper in the oil-damper joint. How these differences in the AFO designs may affect gait will be a topic of future work.
In addition to the laboratory assessment and results, clinical assessments were performed to understand the characteristics of the subjects who participated in this study. The outcomes of the modified Ashworth scale (MAS) and the peak dorsiflexion angles (i.e. range of motion: ROM) suggested that this group of subjects generally had increased tone in the ankle joint. The manual muscle testing (MMT) showed that the range of muscle strength at ankle and knee joints was not homogeneous. However, all the subjects could voluntarily flex and extend their knee joint. The Timed Up & Go test (TUG) assesses functional mobility and is able to detect changes in mobility over time in patients with stroke (Persson et al., 2014). The mean TUG was 17.72 (5.13) seconds in this study. The TUG score of less than 20 is generally considered as independent for basic transfers (Podsiadlo and Richardson, 1991). How the clinical assessment outcomes could contribute to AFO prescriptions for patients with stroke requires further research.
The limitations of this study are as follows: 1) The number of subjects who participated in this study was small (10 subjects). These subjects may not necessarily represent the general population of stroke patients. The clinical characteristics of this group of subjects were also not homogenous. However, the fact that significant and systematic effects were found in this non-homogeneous group of subjects is also the strength of this study as it suggests that ankle and knee joints kinetic and kinematic parameters are commonly responsive to the plantarflexion resistive moments of an AFO. 2) There is some evidence that the adjustment of the shank to vertical angle through AFO-footwear combination is important to optimize an AFO prescription (Owen, 2010). It is our intention to include this aspect in our future study. 3) While every effort was made to fit the articulated AFO comfortably to each subject, it was not custom-made. Therefore, the results of the present study represent “off-the-shelf” AFOs rather than “custom-made” AFOs. 4) This study investigated the immediate effects of the changes in the plantarflexion resistive moments of the AFO. The long-term effects should also be investigated in future studies. 5) While treadmill gait was suggested to be similar to overground gait in healthy subjects (Riley et al., 2007), walking on the treadmill appeared to have affected a comfortable walking speed of the subjects in this study. 6) This study focused on the ankle and knee joints as we hypothesized that they were the primary and secondary joints being affected by the AFO. However, the potential effects of the AFO on hip joints, pelvis, trunk and center of mass are acknowledged (Cruz and Dhaher, 2009; Kobayashi et al., 2012; Wang et al., 2007). 7) The effect of dorsiflexion resistive moments of the AFO was not investigated. Its effect should also be explored systematically in future studies. Finally, 8) it was expected that there were some errors associated with 3-dimensional gait analysis and inverse dynamics (Cappozzo et al., 1996).
Conclusions
This study showed that the ankle and knee joint angles and moments were significantly and systematically affected by the amount of plantarflexion resistive moment of the articulated AFO. This indicates the importance of tuning the plantarflexion resistive moment of articulated AFOs for individual patients. Future studies should investigate how this kinematic and kinetic data can contribute to better orthotic care in the clinical setting by building on the findings of the current study.
Highlights.
A new articulated ankle-foot orthosis was developed for stroke patients.
The effect of its plantarflexion resistive moment on gait was investigated.
Ankle angles and moments demonstrated a significant and systematic response.
Knee angles and moments demonstrated a significant and systematic response.
The plantarflexion resistive moment should be tuned for each patient.
Acknowledgments
This study was supported by the National Institutes of Health, Eunice Kennedy Shriver National Institute of Child Health & Human Development, Grant Number 2R44HD069095. We would like to thank Mr. David E. Hensley of Seattle O&P for his technical support in designing the articulated AFO.
Footnotes
Conflict of interest statement
Kobayashi T, Orendurff MS and Daly WK are employees of Orthocare Innovations and designed the articulated AFO used in this study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bohannon RW, Smith MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Physical therapy. 1987;67:206–207. doi: 10.1093/ptj/67.2.206. [DOI] [PubMed] [Google Scholar]
- Bregman DJ, De Groot V, Van Diggele P, Meulman H, Houdijk H, Harlaar J. Polypropylene ankle foot orthoses to overcome drop-foot gait in central neurological patients: a mechanical and functional evaluation. Prosthet Orthot Int. 2010;34:293–304. doi: 10.3109/03093646.2010.495969. [DOI] [PubMed] [Google Scholar]
- Cappozzo A, Catani F, Leardini A, Benedetti MG, Croce UD. Position and orientation in space of bones during movement: experimental artefacts. Clin Biomech (Bristol, Avon) 1996;11:90–100. doi: 10.1016/0268-0033(95)00046-1. [DOI] [PubMed] [Google Scholar]
- Cruz TH, Dhaher YY. Impact of ankle-foot-orthosis on frontal plane behaviors post-stroke. Gait Posture. 2009;30:312–316. doi: 10.1016/j.gaitpost.2009.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit DC, Buurke JH, Nijlant JM, Ijzerman MJ, Hermens HJ. The effect of an ankle-foot orthosis on walking ability in chronic stroke patients: a randomized controlled trial. Clin Rehabil. 2004;18:550–557. doi: 10.1191/0269215504cr770oa. [DOI] [PubMed] [Google Scholar]
- Gao F, Carlton W, Kapp S. Effects of joint alignment and type on mechanical properties of thermoplastic articulated ankle-foot orthosis. Prosthet Orthot Int. 2011;35:181–189. doi: 10.1177/0309364611409617. [DOI] [PubMed] [Google Scholar]
- Gok H, Kucukdeveci A, Altinkaynak H, Yavuzer G, Ergin S. Effects of ankle-foot orthoses on hemiparetic gait. Clin Rehabil. 2003;17:137–139. doi: 10.1191/0269215503cr605oa. [DOI] [PubMed] [Google Scholar]
- Harper NG, Esposito ER, Wilken JM, Neptune RR. The influence of ankle-foot orthosis stiffness on walking performance in individuals with lower-limb impairments. Clin Biomech (Bristol, Avon) 2014;29:877–884. doi: 10.1016/j.clinbiomech.2014.07.005. [DOI] [PubMed] [Google Scholar]
- Kendall FP, McCreary EK, Provance PG. Muscles Testing and Function with Posture and Pain. 4. Williams & Wilkins; Baltimore, Maryland: 1993. [Google Scholar]
- Kobayashi T, Leung AK, Akazawa Y, Hutchins SW. Design of a stiffness-adjustable ankle-foot orthosis and its effect on ankle joint kinematics in patients with stroke. Gait Posture. 2011a;33:721–723. doi: 10.1016/j.gaitpost.2011.02.005. [DOI] [PubMed] [Google Scholar]
- Kobayashi T, Leung AK, Akazawa Y, Hutchins SW. Effect of ankle-foot orthoses on the sagittal plane displacement of the center of mass in patients with stroke hemiplegia: a pilot study. Topics in stroke rehabilitation. 2012;19:338–344. doi: 10.1310/tsr1904-338. [DOI] [PubMed] [Google Scholar]
- Kobayashi T, Leung AK, Akazawa Y, Hutchins SW. The effect of varying the plantarflexion resistance of an ankle-foot orthosis on knee joint kinematics in patients with stroke. Gait Posture. 2013;37:457–459. doi: 10.1016/j.gaitpost.2012.07.028. [DOI] [PubMed] [Google Scholar]
- Kobayashi T, Leung AK, Akazawa Y, Tanaka M, Hutchins SW. Quantitative measurement of spastic ankle joint stiffness using a manual device: a preliminary study. J Biomech. 2010;43:1831–1834. doi: 10.1016/j.jbiomech.2010.02.024. [DOI] [PubMed] [Google Scholar]
- Kobayashi T, Leung AK, Hutchins SW. Techniques to measure rigidity of ankle-foot orthosis: a review. J Rehabil Res Dev. 2011b;48:565–576. doi: 10.1682/jrrd.2010.10.0193. [DOI] [PubMed] [Google Scholar]
- Nolan KJ, Yarossi M. Preservation of the first rocker is related to increases in gait speed in individuals with hemiplegia and AFO. Clin Biomech (Bristol, Avon) 2011;26:655–660. doi: 10.1016/j.clinbiomech.2011.03.011. [DOI] [PubMed] [Google Scholar]
- Owen E. The importance of being earnest about shank and thigh kinematics especially when using ankle-foot orthoses. Prosthet Orthot Int. 2010;34:254–269. doi: 10.3109/03093646.2010.485597. [DOI] [PubMed] [Google Scholar]
- Persson CU, Danielsson A, Sunnerhagen KS, Grimby-Ekman A, Hansson PO. Timed Up & Go as a measure for longitudinal change in mobility after stroke - Postural Stroke Study in Gothenburg (POSTGOT) Journal of neuroengineering and rehabilitation. 2014;11:83. doi: 10.1186/1743-0003-11-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. Journal of the American Geriatrics Society. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- Riley PO, Paolini G, Della Croce U, Paylo KW, Kerrigan DC. A kinematic and kinetic comparison of overground and treadmill walking in healthy subjects. Gait Posture. 2007;26:17–24. doi: 10.1016/j.gaitpost.2006.07.003. [DOI] [PubMed] [Google Scholar]
- Russell Esposito E, Blanck RV, Harper NG, Hsu JR, Wilken JM. How does ankle-foot orthosis stiffness affect gait in patients with lower limb salvage? Clinical orthopaedics and related research. 2014;472:3026–3035. doi: 10.1007/s11999-014-3661-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sankoh AJ, Huque MF, Dubey SD. Some comments on frequently used multiple endpoint adjustment methods in clinical trials. Stat Med. 1997;16:2529–2542. doi: 10.1002/(sici)1097-0258(19971130)16:22<2529::aid-sim692>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- Singer ML, Kobayashi T, Lincoln LS, Orendurff MS, Foreman KB. The effect of ankle–foot orthosis plantarflexion stiffness on ankle and knee joint kinematics and kinetics during first and second rockers of gait in individuals with stroke. Clin Biomech (Bristol, Avon) 2014;29:1077–1080. doi: 10.1016/j.clinbiomech.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tukey JW, Ciminera JL, Heyse JF. Testing the statistical certainty of a response to increasing doses of a drug. Biometrics. 1985;41:295–301. [PubMed] [Google Scholar]
- Wang RY, Lin PY, Lee CC, Yang YR. Gait and balance performance improvements attributable to ankle-foot orthosis in subjects with hemiparesis. Am J Phys Med Rehabil. 2007;86:556–562. doi: 10.1097/PHM.0b013e31806dd0d3. [DOI] [PubMed] [Google Scholar]
- Winter DA. Biomechanics and motor control of human movement. 3. Wiley; Hoboken, New Jersey: 2005. [Google Scholar]
- Yamamoto S, Hagiwara A, Mizobe T, Yokoyama O, Yasui T. Development of an ankle-foot orthosis with an oil damper. Prosthet Orthot Int. 2005;29:209–219. doi: 10.1080/03093640500199455. [DOI] [PubMed] [Google Scholar]
- Yamamoto S, Hagiwara A, Mizobe T, Yokoyama O, Yasui T. Gait improvement of hemiplegic patients using an ankle-foot orthosis with assistance of heel rocker function. Prosthet Orthot Int. 2009;33:307–323. doi: 10.3109/03093640903176563. [DOI] [PubMed] [Google Scholar]
- Yamamoto S, Miyazaki S, Kubota T. Quantification of the effect of the mechanical property of ankle-foot orthoses on hemiplegic gait. Gait Posture. 1993;1:27–34. [Google Scholar]
- Yamamoto S, Tomokiyo N, Yasui T, Kawaguchi T. Effects of plantar flexion resistive moment generated by an ankle-foot orthosis with an oil damper on the gait of stroke patients: a pilot study. Prosthet Orthot Int. 2013;37:212–221. doi: 10.1177/0309364612460266. [DOI] [PubMed] [Google Scholar]