Images in Allergy
A 27-year-old man presented 9 years ago with a history of swelling and pruritus of his legs shortly after exiting from a swimming pool and which resolved within an hour. Since then he has had a consistent reaction of painful itch, burning, redness and swelling in response to direct sun exposure, that is limited to the area of exposure, lasts 15–60 minutes and is not associated with systemic symptoms. Treatment with anti-histamines and sunblock provides minimal relief when taken prior to exposure to sunlight. He is otherwise healthy and takes no other medications. He has a normal WBC and blood chemistries with an IgE of 406 IU/mL. Solar challenge testing consisted of direct exposure to UVA (320–400nm wavelength), UVB (290–320 nm) and visible light (380–700 nm) using a range of light energy to determine the minimal threshold to illicit urticaria, i.e. minimal urticarial dose(MUD). Phototesting using a visible light source (GAF 1680 Projector, 500W, Figure 1A) for a 10 minute exposure resulted in acute onset of swelling, severe pruritus and erythema as shown at 15 minutes post-exposure in Figure 1B. Further phototesting to UVB (Figure 1C, Handisol® UVB, National Biological Corp,) induced urticaria with a MUD of 75mJ(testing range 25–200mJ). The patient did not react to UVA light (testing range 1–20J). Thus, the diagnosis is solar urticaria induced by UVB and visible light.
Figure 1.
Solar Urticaria Challenge testing of 27 year old male. A)Visible light exposure (380–700 nm) directed to the lower back with B) development of raised, erythematous wheals 15 min post exposure. C) UVB (290–320 nm) challenge testing and D) positive urticarial reaction at 75, 150 and 200 mJoules of UVB (but not at 25 mJ)
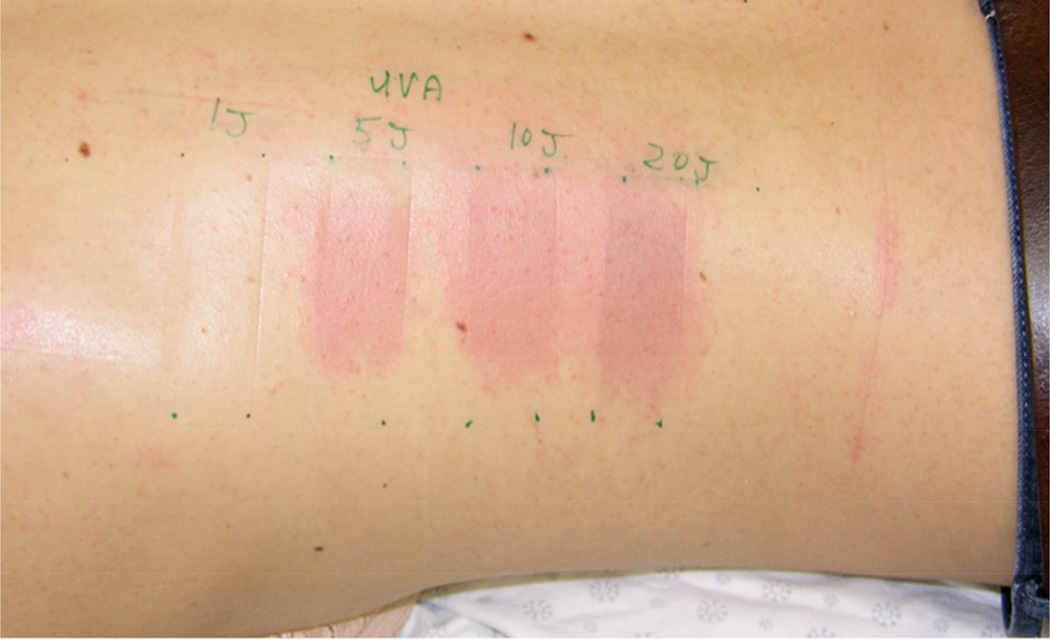
The second case is that of a 29-year-old woman presenting with a 5-year history of sun-induced redness and itch, well demarcated on sun-exposed areas of her chest, neck and arms. Her most severe reaction occurred after prolonged sun exposure at the beach. Scratching the lesions intensifies the urticaria. In general her reactions attenuate toward the end of the summer likely due to repeated exposures. Relief provided by sunblock, and anti-histamines has diminished over the last few years, but repeated UV light tanning was observed to be an effective treatment. Her laboratory studies were within normal limits including an IgE of 85 IU/mL. Phototesting to visible light and UVA exposure triggered urticaria. The MUD of UVA was 5J (testing range 1–20J) as illustrated in Figure 2 with a clear dose affect. Testing to UVB was negative. Her diagnosis is solar urticaria due to UVA and visible light.
Figure 2.
29-year-old female with Solar Urticaria. Urticarial reaction to 5–20 Joules of UVA light with dose effect.
Solar urticaria is a rare mast cell mediated photodermatosis(1) likely attributable to a photoantigen that is activated by light of a particular spectrum.(2) Symptoms generally begin with a sensation of burning and itch within 5–10 min of sun exposure and are occasionally associated with systemic manifestation(3)and rarely anaphylaxis. Solar urticaria should be distinguished from local heat urticaria and polymorphous light eruption (PLE), the latter of which is a more delayed(hours vs. minutes) and prolonged(days vs. hours). Phototesting as performed in the above cases at the bedside, aids in the identification of the wavelength that elicits solar manifestations and helps to characterize the nature and intensity of the reaction, which is helpful for selecting treatment. Treatment modalities include avoidance to exposure, sunblock, antihistamines(4), phototherapy, and in recalcitrant cases cyclosporine A, IVIG(5) and omalizmab.(6)
Acknowledgments
This work was supported by the Division of Intramural Research, NIAID, NIH. Support by M.Y. for this project was funded in whole or in part with federal funds from the National Cancer Institute, National Institutes of Health, under Contract No. HHSN261200800001E and [in part] by the National Institute of Allergy and Infectious Diseases. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Authors state no conflict of interest.
References
- 1.Hawk JL, Eady RA, Challoner AV, Kobza-Black A, Keahey TM, Greaves MW. Elevated blood histamine levels and mast cell degranulation in solar urticaria. British journal of clinical pharmacology. 1980;9(2):183–186. doi: 10.1111/j.1365-2125.1980.tb05831.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Botto NC, Warshaw EM. Solar urticaria. Journal of the American Academy of Dermatology. 2008;59(6):909–920. doi: 10.1016/j.jaad.2008.08.020. quiz 21-2. [DOI] [PubMed] [Google Scholar]
- 3.Ramsay CA. Solar urticaria. International journal of dermatology. 1980;19(5):233–236. doi: 10.1111/j.1365-4362.1980.tb00314.x. [DOI] [PubMed] [Google Scholar]
- 4.Beattie PE, Dawe RS, Ibbotson SH, Ferguson J. Characteristics and prognosis of idiopathic solar urticaria: a cohort of 87 cases. Archives of dermatology. 2003;139(9):1149–1154. doi: 10.1001/archderm.139.9.1149. [DOI] [PubMed] [Google Scholar]
- 5.Aubin F, Porcher R, Jeanmougin M, Leonard F, Bedane C, Moreau A, et al. Severe and refractory solar urticaria treated with intravenous immunoglobulins: a phase II multicenter study. Journal of the American Academy of Dermatology. 2014;71(5):948–953 e1. doi: 10.1016/j.jaad.2014.07.023. [DOI] [PubMed] [Google Scholar]
- 6.Baliu-Pique C, Aguilera Peiro P. Three cases of solar urticaria successfully treated with omalizumab. Journal of the European Academy of Dermatology and Venereology : JEADV. 2015 doi: 10.1111/jdv.13001. [DOI] [PubMed] [Google Scholar]