TO THE EDITOR:
One in 13 students has a food allergy that requires individualized health care plans, emergency action plans, and training for school personnel.1 Reactions in schools are common: 16%-18% of school-age children with food allergies experienced a reaction in the school,2 and onset of symptoms in the school setting is a risk factor for fatal reactions.3 Given the prevalence and severity of this issue, the State of Illinois enacted “Guidelines for Managing Life-threatening Food Allergies in Illinois Schools.”4 These guidelines stipulated that food allergy training for all staff with student contact be conducted every other year, and anaphylaxis drills be conducted yearly. In addition, Illinois passed the School Access to Emergency Epinephrine Act.5 This allowed schools to stock undesignated epinephrine for any child with a severe allergic reaction and allowed administration of epinephrine to a child with a written plan for epinephrine but unavailable medication. The assessment of current practices is important in the planning for appropriate resources for school emergency preparedness, including food allergy education and anaphylaxis drills for staff as similar legislation is applied nationally.6 Therefore, we sought to characterize school nurse response to food allergy emergencies in school and the impact recent Illinois State legislation has had on school nurses, including preparedness to manage severe food allergy reactions.
A cross-sectional online survey was administered to school nurses and aides throughout Illinois between October 1, 2012, and January 20, 2013. The Institutional Review Board of Ann & Robert H. Lurie Children’s Hospital of Chicago approved the study protocol. Survey questions were designed to assess school experience with food allergy reactions and school response to recent food allergy legislation in the State of Illinois (see Figure E1 in this article’s Online Repository at www.jaci-inpractice.org). A severe allergic reaction was determined by the nurses’ perception of a severe reaction for which they would normally administer an epinephrine autoinjector. “Unavailability” of epinephrine meant that the nurse would have administered the drug had the student had epinephrine or undesignated epinephrine. A drill was defined as a preplanned exercise conducted by a school (P.A. 94-600, 8-16-05). School community type was based on school nurse response regarding population density that the school covered. A χ2 test of independence was used to compare answers by school community type (eg, rural, suburban, and urban) and school level (preschool/elementary school, middle/junior high, and high school).
Four hundred and sixty personnel (72% of the Illinois Association of School Nurses membership) completed the survey, which represented more than one thousand (1012) Illinois schools. Nurses were responsible for 2.4 schools on average and had a mean of 9.7 years of experience in their present school. Schools were described as suburban (n = 662 schools, 65.8%), rural (n = 225 schools, 22.2%) and urban (n = 125 schools, 12.4%), and were representative of the school makeup in the State of Illinois as categorized by the Illinois State Board of Education. All school levels from preschool to high school were represented (see Table E1 in this article’s Online Repository at www.jaci-inpractice.org).
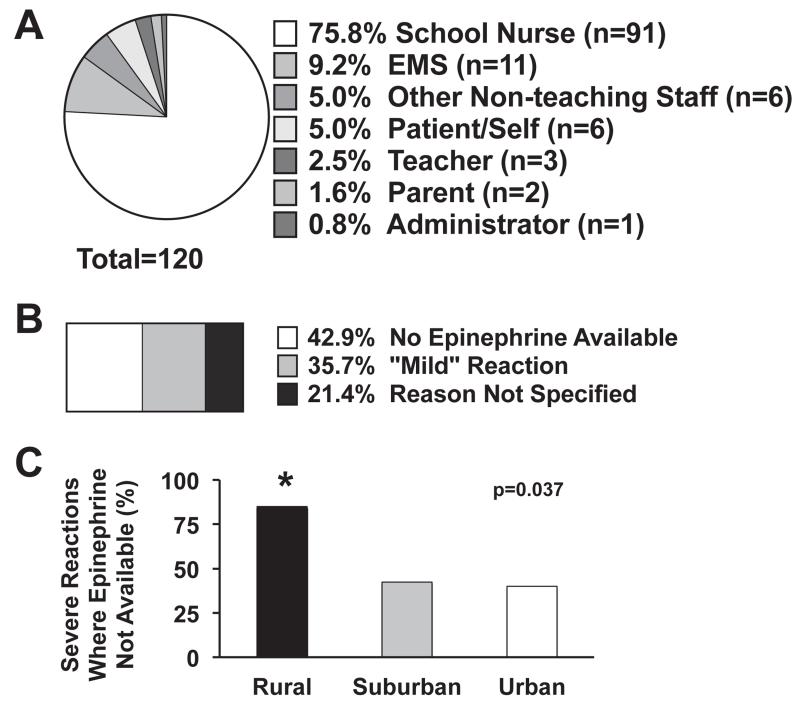
More than one-third (35.2%) of respondents reported an experience with a severe allergic reaction, although nurses from rural communities were least likely to report this experience (n = 161 emergencies, 18.9% rural vs 38.5% suburban vs 46% urban, P = .001). High school nurses were most likely to report this experience (29.7% preschool/elementary vs 32.3% middle/junior high vs 47.4% high school, P = .002). Importantly, 21.6% (n = 35/161) of the severe reactions were from a previously unknown allergen and were independent of school location (35.3% rural vs 21.6% suburban, 13.0% urban, P = .25) and school level. Epinephrine was administered a total of 120 times (79.5%) but was not given in 28 of 161 severe reactions (17.4%; see Table E2 in this article’s Online Repository at www.jaci-inpractice.org). When epinephrine was given, the school nurse administered epinephrine the overwhelming majority (75.8%) of the time (Figure 1, A). When epinephrine was not given, unavailability of the drug was the most frequently cited reason (Figure 1, B), and this was most common in rural schools (85.7% vs 50% vs 47%, P = .037, Figure 1, C). There was no difference based on school level.
FIGURE 1.
Treatment of severe allergic reactions at schools. A, School personnel responding to severe allergic reactions. Although they were not always available, school nurses responded to severe allergic reactions an overwhelmingly majority of the time. There was no difference between community types. B, Reasons specified for not giving epinephrine for a severe reaction. C, Rural communities reported epinephrine unavailability more often than urban and suburban communities (85.7% vs 42.4% vs 40%, *P = .037).
In compliance with State Guidelines, the majority of nurses (79.4%) and school health aides (53.6%) provided food allergy training to the school staff within the past year (Figure E1, A); this did not differ by community type or school level. However, anaphylaxis drills were rarely conducted (6.6%) despite the recommendation in state guidelines (see Figure E2 in this article’s Online Repository at www.jaci-inpractice.org). Barriers to conducting anaphylaxis drills are shown (Figure E2). When asked what would help the nurse conduct anaphylaxis drills, the most frequent suggestions were training (materials and training for nurses), support from administration and staff, and mandated anaphylaxis drills by Illinois State Board of Education (drills currently “recommended,” but not “mandated”). These responses were similar between community types and school levels.
Nearly all respondents (99.1%) reported feeling either fairly confident or confident in their ability to manage a food allergy reaction, and 75.5% attributed most or some of their confidence to their district’s food allergy policy. Interestingly, confidence in management varied widely depending on the location of the reaction (Table E3 in this article’s Online Repository at www.jaci-inpractice.org). School buses, playgrounds, and field trips remain areas of concern. Perceived readiness did not differ between community types or school levels.
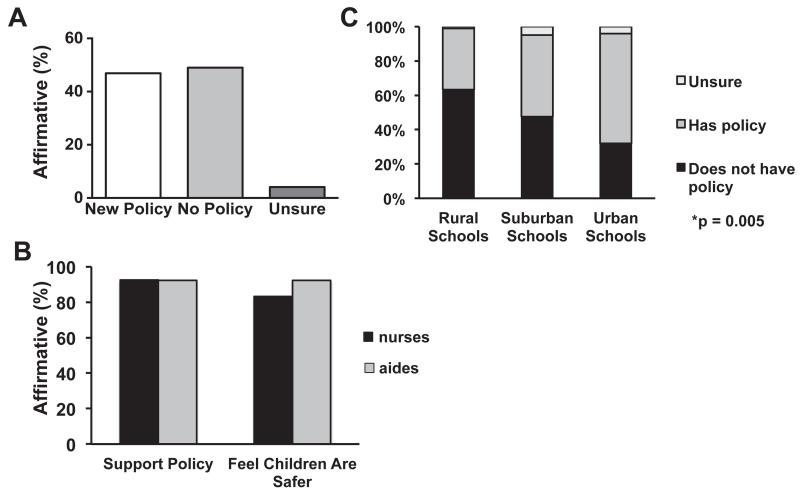
Rural schools were least likely to have a written plan or protocol to outline staff procedure in the event of a severe allergic reaction (59.4% of respondents working at rural schools were aware of a written plan or protocol vs 81.7% for suburban vs 71.9% for urban, P = .0019). This did not differ between school levels. Additionally, rural schools were least likely to report undesignated epinephrine policies (35.6% of rural, 47.5% of suburban, and 64.0% of urban schools, Figure 2, P = .005). Among those schools with undesignated epinephrine autoinjectors, nearly all nurses and aides supported the new policy (92.4% nurses, 92.3% aides, Figure 2, C) and the majority of nurses (83.2%) and aides (92.3%) indicated that they felt children with food allergy were now safer in school.
FIGURE 2.
Undesignated epinephrine in schools. A, As a result of the Illinois State Food Allergy Guidelines, 46.9% of nurses reported a new school policy for the use of undesignated epinephrine in their school. However, the plurality of schools did not have undesignated epinephrine. B, School nurses and aids overwhelmingly supported the policy for undesignated epinephrine and indicated that it has made children safer in schools (black bars = nurses, gray bars = health aides). C, Nurses from rural schools were least likely to report a policy for undesignated epinephrine; urban schools were most likely. *P = .005.
Together, these data emphasize that all school personnel are called upon to administer injectable epinephrine, and that school nurses support expanded legislation regarding food allergy education, training, and availability of injectable epinephrine. Additionally, we report a previously unrecognized rural disparity in implementation of food allergy guidelines and access to undesignated epinephrine. Our study indicates that nurses provide 76% of the injectable epinephrine, despite being in the school less than 50% of the time. This leads to the question of why epinephrine is given much less frequently by other personnel. Is this due to lack of recognition of symptoms or lack of confidence in providing the treatment? This is of great concern because a delay in administration of epinephrine is an identified risk factor for death from food-induced anaphylaxis.2,3 As mentioned earlier, 21.6% of the severe reactions were from a previously unknown allergen, supporting access to undesignated epinephrine even for students not previously diagnosed. Additionally, lack of anaphylaxis drills despite a desire to conduct these drills suggests that additional resources such as a module outlining steps to conduct, record, and evaluate an anaphylaxis drill would be helpful. Thus, this study highlights the need for food allergy training in the schools and areas where training can be improved.
Previously unrecognized, this study illustrates an important health disparity and an opportunity for improved implementation and advocacy. Nurses from rural schools reported the least experience with food allergy reactions, were least likely to recall a written policy for handling of food allergy emergencies in their school, and were least likely to report a new policy for undesignated epinephrine. Of note, rural schools were defined by nurse response regarding population density. Additionally, we report percentages of school nurses from these areas that have responded to the policy. Therefore, the rural disparity compared with urban or suburban counterparts illustrate that rural schools were least likely to respond to legislation, are not easily explained by the possibility of fewer students. Geographic health disparity is well recognized, and rural health disparity with regard to access to care and health outcome has been described particularly in cardiac and cancer care.7 With regard to food allergy, although previous studies have reported disparities with regard to geography in the United States8 and socio-economic status,9 disparity based on community type has not yet been described. The presence of food allergy guidelines was associated with increased emergency health plan compliance in a smaller study of 124 schools.10
Limitations include a potential reporting bias in that nurses most interested in this topic may have completed the survey and, therefore, were most enthusiastic about food allergy education and training. A “severe allergic reaction” was used in the survey without a prespecified definition; the nurses’ perception of a severe reaction, and not an objective definition, was used. Finally, as differences in school response by population density were an unexpected finding, data regarding outcomes due to the lack of new policies or decreased access to epinephrine were not collected. Rather, the survey focused on school nurse implementation and attitudes toward the State Guidelines.
This study demonstrates positive effects of recent state legislation mandating food allergy education and the allowance of undesignated epinephrine in schools and highlights the need for school-wide food allergy preparedness and training. Our findings also reveal opportunities for improvement in food allergy policy implementation, including securing additional time and resources for food allergy training and anaphylaxis drills, and addressing geographic health disparities by increasing efforts in rural communities.
Supplementary Material
Clinical Implications.
Legislation mandating food allergy education and allowing undesignated epinephrine in schools has had a positive impact. Opportunities for improvement include additional time and resources for food allergy training and increasing efforts in rural communities to address geographic health disparities.
Acknowledgment
The authors kindly acknowledge Miao Cai for her assistance in statistical analysis.
Funding was provided by Food Allergy Research and Education (FARE) Organization, Blowitz-Ridgeway Respiratory Health Association, Thrasher Research Fund, National Institute of Allergy and Infectious Diseases (NIAID) (K23 AI100995-01).
K. A. Schmeissing has received research support from FARE. C. Szychlinski has received research support from FARE; and has received lecture fees from Mylan. A. M. Singh has received research support from the National Institutes of Health (KL2 5KL2RR025740-04)/NIAID, Thrasher Research Fund, and Blowitz-Ridgeway Respiratory Health Association. J. A. Pongracic has received research support from DBV Technologies, FARE, and Boston Children’s Hospital; and has received travel support from Food Allergy Project.
Footnotes
Conflicts of interest: The rest of the authors declare that they have no relevant conflicts.
REFERENCES
- 1.Gupta RS, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. 2011;128:e9–17. doi: 10.1542/peds.2011-0204. [DOI] [PubMed] [Google Scholar]
- 2.Nowak-Wegrzyn A, Conover-Walker MK, Wood RA. Food-allergic reactions in schools and preschools. Arch Pediatr Adolesc Med. 2001;155:790–5. doi: 10.1001/archpedi.155.7.790. [DOI] [PubMed] [Google Scholar]
- 3.Sampson HA, Mendelson L, Rosen JP. Fatal and near-fatal anaphylactic reactions to food in children and adolescents. N Engl J Med. 1992;327:380–4. doi: 10.1056/NEJM199208063270603. [DOI] [PubMed] [Google Scholar]
- 4. [June 2, 2015];Illinois State Board of Education Food Allergy Guidelines. Available from: http://www.isbe.net/nutrition/pdf/food_allergy_guidelines.pdf.
- 5. [April 17, 2015];Illinois General Assembly Public Act 097-0361. Available from: http://www.ilga.gov/legislation/publicacts/fulltext.asp?Name=097-0361.
- 6. [June 2, 2015];School Access to Emergency Epinephrine Act. Available from: https://www.congress.gov/bill/113th-congress/house-bill/2094/text.
- 7.Meilleur A, Subramanian SV, Plascak JJ, Fisher JL, Paskett ED, Lamont EB. Rural residence and cancer outcomes in the United States: issues and challenges. Cancer Epidemiol Biomarkers Prev. 2013;22:1657–67. doi: 10.1158/1055-9965.EPI-13-0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta RS, Springston EE, Smith B, Warrier MR, Pongracic J, Holl JL. Geographic variability of childhood food allergy in the United States. Clin Pediatr (Phila) 2012;51:856–61. doi: 10.1177/0009922812448526. [DOI] [PubMed] [Google Scholar]
- 9.Shah SS, Parker CL, O’Brian Smith E, Davis CM. Disparity in the availability of injectable epinephrine in a large, diverse US school district. J Allergy Clin Immunol Pract. 2014;2:288–293. e1. doi: 10.1016/j.jaip.2013.09.016. [DOI] [PubMed] [Google Scholar]
- 10.Eldredge C, Patterson L, White B, Schellhase K. Assessing the readiness of a school system to adopt food allergy management guidelines. WMJ. 2014;113:155–61. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.