Abstract
Objective
The Impact of Events Scale (IES) is one of the most widely used measures of event-specific distress. The IES assesses the frequency with which respondents experience intrusive thoughts and avoidant behaviors over the past week. Our aim is to demonstrate the benefit of a severity-based measurement approach of the IES compared with a frequency-based measurement approach.
Methods
A mixed group of post-treatment cancer survivors (N= 325; M= 31.8 years old) completed measures assessing quality of life (Functional Assessment of Cancer Therapy–General), psychological adjustment (Mental Health Inventory), and cancer-related distress (IES). The IES was keyed to the cancer experience and administered with standard (frequency) and modified (severity) response options.
Results
Classical reliability analyses and bifactor modeling were conducted on both versions of the IES. Reliability estimates suggest that the IES severity items were more highly intercorrelated than the IES frequency items. Both versions of the IES were highly correlated (r = 0.82), showing the presence of a dominant general factor. Bifactor modeling suggested that the severity items generally provided higher levels of discrimination than the frequency items. Validity correlations with the Functional Assessment of Cancer Therapy–General and Mental Health Inventory demonstrated that the IES severity performed as good as or better than the IES frequency.
Conclusions
Given the high correlations and similarity in content, the IES severity items largely assess the same construct as the IES frequency items. However, IES severity items generally showed improved psychometric properties and similar or higher correlations with quality of life and psychological adjustment. The IES severity approach appears to be a more informative method for assessing cancer-specific distress.
Background
Understanding the impact of traumatic experiences on the thoughts and behaviors of patients requires optimal assessment of their subjective responses to their traumatic experience. The Impact of Events Scale (IES) [1], a measure developed to assess the impact of traumatic life events, is one of the most widely used measures of event-specific distress. The IES assesses the frequency with which respondents experience stress-related thoughts and behaviors instead of the severity or the distressing nature of those thoughts and behaviors. Relying on the frequency of stress-related phenomena may be a useful but suboptimal approach for understanding the distress related to a traumatic event because how often someone experiences stress-related phenomena may not be as clinically informative as how bothersome their symptoms are. Our purpose in writing this paper is to evaluate, for the first time, a severity-based measurement approach of the IES compared with the more commonly used frequency-based measurement approach.
The IES was designed to measure the presence of alternating cycles of intrusions such as unwanted thoughts and images of the traumatic event emerging into consciousness and avoidance expressed by efforts to avoid thinking about the traumatic event. The IES is composed of 15 items and has two subscales that assess the frequency of intrusive and avoidant cognitions associated with a specific stressor. Subjects respond using a four-point scale, ranging from ‘not at all’ to ‘often’, regarding how often they experienced specific symptoms during the past week. The IES was revised (IES-R) [2] to include a subscale assessing autonomic arousal in order to mirror the three symptom clusters of post-traumatic stress disorder: intrusions, avoidance, and hyperarousal [3]. In addition, the IES-R instructions were modified to query the severity of distress related to specific symptoms (‘How much were you distressed or bothered by these difficulties?’) instead of the frequency of specific symptoms, a potentially important distinction that could improve measurement of this construct.
The IES is used in a number of clinical populations, including with individuals who have experienced combat [4], natural disasters [5], bereavement [6], substance use [7], and cancer [8], among others. Interestingly, rates of cancer-related traumatic stress, as indicated by structured, clinical diagnostic interviews for posttraumatic stress disorder (PTSD), are relatively low (ranging from 0% to 22%) [9], and the updated DSM-5 criterion for a PTSD diagnosis makes it more difficult for a diagnosis of cancer-related PTSD to be rendered. Criterion A now includes text that says, ‘A life threatening illness or debilitating medical condition is not necessarily considered a traumatic event. Medical incidents that qualify as traumatic events involve sudden, catastrophic events’ (p. 274) [10]. Consequently, being diagnosed or treated for cancer without experiencing concurrent adverse events is not sufficient to merit a diagnosis of PTSD.
Accordingly, a perspective that recognizes a broader range of cancer-related stress reactions is likely more congruent with the experience of a patient with cancer and may be better captured, conceptually, by the perspective of the IES as a measure of cancer-specific distress [11–15]. This characterization of the measure occurs despite the fact the IES instructions ask participants to indicate the frequency of events instead of the severity or distressing nature of these events. On the one hand, the frequency with which participants experience intrusive and avoidant processes about their cancer experience may be a meaningful proxy for their cancer-specific distress. On the other hand, the frequency of cognitive intrusions and avoidance may be a marker of cognitive processing [16]. In the latter scenario, recurrent cognitive intrusions may suggest an adaptive process that allows participants to integrate a stressful event into their lives and may not be indicators of distress per se.
More recently, some studies assessing cancer-specific distress have begun to use the IES-R [17–19]. However, no one has compared the frequency versus severity approaches to identify which strategy is a better gage of the distressing nature of the cancer experience. In this study, we will do the following: (1) examine the benefit of assessing frequency versus severity of cancer-related distress items using the IES and (2) validate the different IES versions against mental health and well-being measures. For the first aim, we will evaluate the strengths of each approach using a combination of classical test theory and item response theory (IRT). We hypothesize that the severity of the items will be a more informative approach to assessing cancer-related distress. For the second aim, we hypothesize that the severity items will show validity correlations that are as high as or higher than those obtained with the frequency items.
Methods
Subjects and procedures
As part of a larger study, participants were recruited from the US general population by an Internet survey company, Toluna (http://www.toluna-group.com). Data collection from online research panels is increasingly common and can be a valid, cost-effective, and efficient means of recruiting clinical samples as demonstrated by our recent experience with two, large-scale National Institutes of Health (NIH)-funded initiatives [20,21].
To be eligible for this study, participants had to have a prior diagnosis of cancer (excluding basal cell skin carcinoma), be between the ages of 18–39 years, within 0–60 months post-treatment, and provide informed consent. Participants were excluded from this study if they had a recurrent diagnosis of cancer, had history of multiple primary cancers, or received palliative or hospice care. Potential participants were sent recruitment emails from Toluna and asked to log on to a secure study website. After screening for eligibility, participants were consented electronically and then administered the study questionnaires. Participants completed demographic and medical information items (history of acute and chronic health conditions) along with other study measures. Participants who completed the survey were eligible for prize or incentive-based compensation through Toluna. Study procedures were approved by the local institutional review board. Additional details about subject recruitment are described elsewhere [22].
Measures
Participants completed a variety of self-report questionnaires assessing the following: (a) demographic and clinical information; (b) quality of life; (c) psychological adjustment; and (d) cancer-specific distress.
Demographic and clinical information
Demographic information obtained included age, race, marital status, education, and annual household income. Clinical information obtained included cancer type, stage of cancer at diagnosis, time since active treatment, performance status [23], and self-report of other medical comorbidities.
Quality of life
The Functional Assessment of Cancer Therapy—General (FACT-G) is a 27-item measure of health-related quality of life in cancer [24]. The FACT-G yields four subscale scores: physical well-being (seven items), functional well-being (seven items), social/family well-being (seven items), and emotional well-being (six items). The physical well-being subscale assesses physical concerns, the functional well-being subscale measures an individual’s ability to engage in various tasks, the social/family well-being subscale questions assess social support and communication, and the emotional well-being subscale measures mood and emotional response to illness. Higher scores indicate better health-related quality of life.
Psychological adjustment
Mental health was assessed using the 18-item short form of the Mental Health Inventory (MHI) [25]. This scale yields four subscale scores: depression (four items), anxiety (five items), behavioral control (four items), and positive affect (four items). Higher scores indicate better mental health and more positive psychological adjustment.
Cancer-specific distress
The IES [1] was used as our index of cancer-specific distress. As already mentioned, the IES is a 15-item self-report measure of intrusive and avoidant cognitions and is frequently used in evaluating stress reactions after traumatic experiences. The IES was keyed to the experience of having cancer: ‘Please read each item, and then indicate how frequently those comments were true for you during the past 7 days with respect to your experience with cancer…’ In addition to the standard items that assess frequency, a subsequent set of items was constructed assessing the severity of the intrusive and avoidant cognitions. In other words, we first assessed how frequent a particular cognition occurred and then assessed how distressed individuals were by the cognition. For example, participants were asked to indicate how frequently the statement ‘I thought about it when I didn’t mean to’ was true for them and then asked ‘How much did this distress or bother you?’ This format was used for all item pairs with the original IES item administered first and the modified IES item administered second. A four-point scale was used for both IES versions with response options of 0 (not at all), 1 (rarely), 3 (sometimes), and 5 (often). While such numerical assignments are not relevant when estimating polychoric correlations and parameters of latent trait models (discussed later), this scoring was applied to descriptive statistics, item correlations, and validity correlations.
Analyses
Analyses proceeded in three steps. First, we computed the reliability statistics of each of the frequency and severity scales separately. As part of this analysis, we computed an estimate of each item set’s unidimensionality, omega hierarchical (ωh) [26], using the psych package in r [27,28]. Second, we used a bifactor IRT model of both item sets to compare the relative contribution of each set (frequency versus severity) to capture the general factor variance. Consistent with our first aim’s hypothesis, we anticipated that the discrimination parameters (or general factor loadings) would be higher for the severity items. To do this, we used irtpro 2.1 [29] and selected the default Bock–Aitkin expectation–maximization algorithm to compute the maximum-likelihood estimates of the bifactor model parameters [30]. Third, as a test of our second aim’s hypothesis, we compared how well the sum scores of frequency and severity item sets correlated with criterion mental health variables.
Results
Descriptive characteristics of sample
Study participants (N=335) had a mean age of 31.8 years (SD= 5.4), were primarily female (68.4%), Caucasian (83.9%), and currently married/partnered (63.0%), had a college education (40.3%), were employed full time (57.3%), and reported an annual income of $50,000 to $99,999 (28.7%). In terms of cancer diagnosis, study participants reported a mix of cancer types including breast (23.9%), gynecologic (16.1%), melanoma (11.0%), lung (6.9%), colorectal (6.3%), thyroid (6.3%), testicular (6.0%), and hematologic malignancies (5.1%). The majority of participants had local stage disease (67.2%), were 20.9 (SD= 16.5) months post-treatment (i.e., conclusion of surgery, chemotherapy, or radiation), and reported normal activity, without symptoms (54.0%). Item means and standard deviations as well as total score means and standard deviations for both the frequency and severity versions of the IES are provided in Table 1.
Table 1.
Item means and standard deviations for the Impact of Events Scale, frequency and severity versions
| Frequency | Severity | |||
|---|---|---|---|---|
| IES item | Mean | SD | Mean | SD |
| 1. I thought about it when I didn’t mean to. | 2.56 | 1.67 | 2.43 | 1.67 |
| 2. I avoided letting myself get upset when I thought about it or was reminded of it. | 2.69 | 1.74 | 2.20 | 1.68 |
| 3. I tried to remove it from memory. | 2.16 | 1.91 | 2.02 | 1.77 |
| 4. I had trouble falling asleep or staying asleep because of pictures or thoughts about it that came into my mind. | 1.79 | 1.81 | 1.98 | 1.87 |
| 5. I had waves of strong feelings about it. | 2.28 | 1.75 | 2.19 | 1.76 |
| 6. I had dreams about it. | 1.36 | 1.63 | 1.49 | 1.74 |
| 7. I stayed away from reminders of it. | 1.79 | 1.84 | 1.56 | 1.69 |
| 8. I felt as if it hadn’t happened or wasn’t real. | 1.88 | 1.77 | 1.65 | 1.68 |
| 9. I tried not to talk about it. | 2.11 | 1.95 | 1.75 | 1.74 |
| 10. Pictures about it popped into my mind. | 1.90 | 1.68 | 1.77 | 1.75 |
| 11. Other things kept making me think about it. | 2.05 | 1.65 | 1.78 | 1.66 |
| 12. I was aware I still had a lot of feelings about it but I didn’t deal with them. | 1.90 | 1.79 | 1.95 | 1.85 |
| 13. I tried not to think about it. | 2.41 | 1.88 | 1.86 | 1.62 |
| 14. Any reminder brought back feelings about it. | 2.20 | 1.75 | 2.00 | 1.73 |
| 15. My feelings about it were kind of numb. | 2.06 | 1.75 | 1.76 | 1.70 |
| Total score | 31.15 | 17.76 | 28.38 | 20.49 |
The obtained range of values for individual items for both the frequency and distress/bother response options was 0 to 5.
IES, Impact of Events Scale; SD, standard deviation.
Reliability analyses
Computing reliability analyses, we first estimated the polychoric correlations of the data. Because items may be endorsed according to thresholds in addition to content, analytic procedures that depend on interitem correlations may overestimate multidimensionality. Estimating polychoric correlations represents one way to counter this bias [31,32]. Table 1 shows the reliability statistics based on the polychoric matrix (nonpolychorics are in parentheses).
As Table 2 shows, both IES frequency and severity scales show high values for Cronbach’s alpha. The estimates of general factor saturation (ωh) are likewise high; for both IES scales, the proportion of test variance attributable to a general factor was above 70%. Both estimates were greater than the lower-bound cut-off of 0.70 for the presence of smaller group factors suggested by Reise et al. [33].
Table 2.
Classical reliability statistics for the Impact of Events Scale, frequency and severity versions
| Corrected item–total correlations | ||||||
|---|---|---|---|---|---|---|
| Scale | Cronbach’s α | ωh | AIC | Mean | Min | Max |
| IES frequency | 0.93 (0.91) | 0.77 (0.75) | 0.49 (0.41) | 0.74 (0.61) | 0.42 (0.34) | 0.81 (0.71) |
| IES severity | 0.97 (0.95) | 0.89 (0.76) | 0.69 (0.60) | 0.83 (0.76) | 0.76 (0.66) | 0.87 (0.80) |
Item–total correlations corrected for item overlap. Item statistics are based on polychoric correlations (non-polychoric statistics are in parentheses).
AIC, average interitem correlation; IES, Impact of Events Scale.
However, the severity items were more highly intercorrelated compared with the frequency items. In particular, the average interitem correlation was considerably higher for the severity items (0.69) compared with the frequency items (0.49). In addition, using the polychoric estimate, the omega (h) was higher for the severity items than for the frequency items. These data suggest that the severity items showed higher values for some indicators of reliability. Although high reliability can suggest redundancy in some cases, in this study, the item stems are the same for both item sets, and only the directions for responding differ.
Because the IES severity items assess the same construct slightly differently, we would expect frequency and severity to be highly correlated. This was in fact the case, with a raw score correlation of 0.82. Nevertheless, the frequency and severity items were not interchangeable psychometrically. For example, the IES severity items were more highly correlated with each other than with the frequency items. Thus, while the corrected mean item–total correlation for the severity items was 0.76 (range 0.66–0.80), the mean item correlation of the severity items with the frequency total score was lower, 0.65 (range 0.56–0.69), underscoring the fact that they are assessing the construct in slightly different ways.
Bifactor modeling to distinguish between severity and frequency
To determine whether the severity items are an improvement over the frequency items, we modeled the items together and estimated the IRT parameters of a general factor, representing the variance common to all 30 items. In this bifactor model, we specified two group factors: one for the frequency items and one for the severity items. Although the shared variance between the two measures was large (r= 0.82), the bifactor model was the more robust model for these analyses. In a unidimensional model of all 30 items, we suspected that the repeated item wording of the severity items might form a large local dependence, which would inflate their discrimination parameters/loadings relative to the frequency items. In a bifactor model, however, the variance specific to each factor would not distort the large amount of (general factor) variance assumed to underlie most of the IES construct.
Our bifactor model parameters were estimated using a common IRT estimation technique, the Bock–Aitkin expectation–maximization algorithm [30]. Parameter estimates (or loadings) derived from such full-information techniques may be more accurate compared with limited-information factor analyses, because they use information from all of the response options available for each item [34]. Because of this, full-information techniques minimized the possibility that response bias or ‘difficulty’ factors might distort the factor structure in limited information models [32].
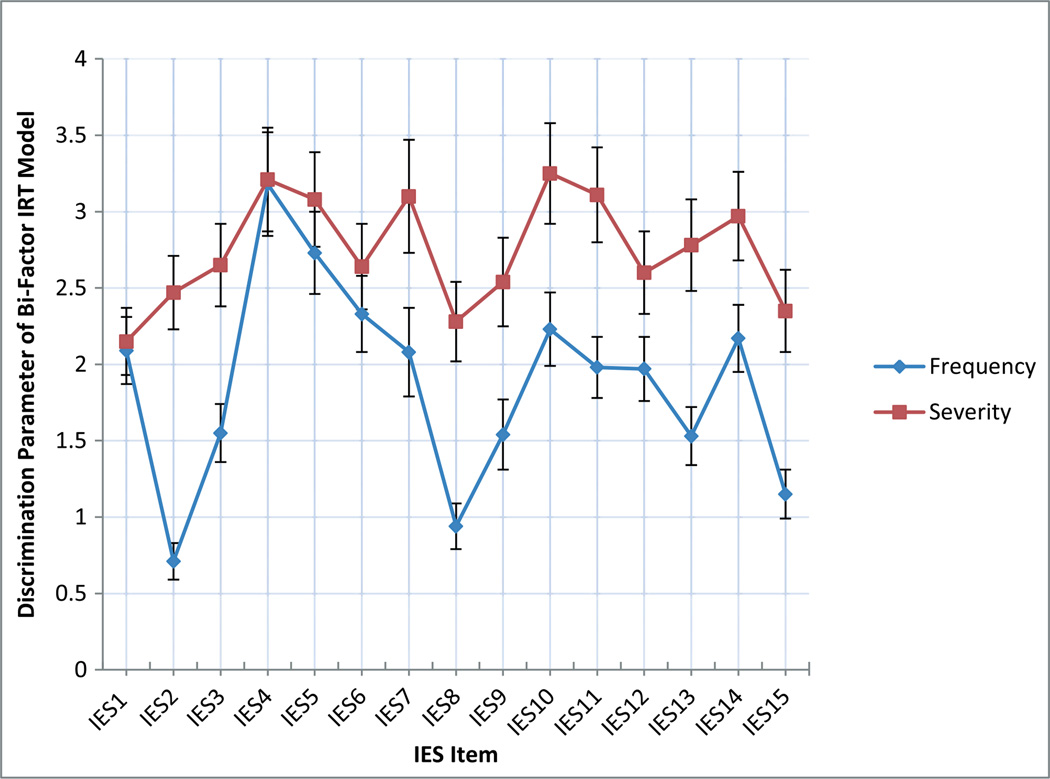
Because both frequency and severity items were in the model, we could directly compare how well each set of items captured the general factor variance. Figure 1 shows each item’s discrimination parameter for each frequency and severity item. The discrimination parameter is an index of an item’s association with the general trait. Typical scales show item values ranging from 0.5 to 2.5 [35], but carefully constructed item banks may show higher values [36]. As Figure 1 shows, the discrimination parameters of the severity items were as high or, in many cases, higher than the matched parameter of the frequency items. The discrimination parameters of the severity items were, on average, 0.86 higher than the frequency items (the differences ranged from 0.03 to 1.76). These results suggest that the severity items do a better job than the frequency items of capturing the psychological impact of traumatic events.
Figure 1.
Discrimination parameters of the severity items versus frequency items of the Impact of Events Scale (IES) in a bifactor item response theory (IRT) model
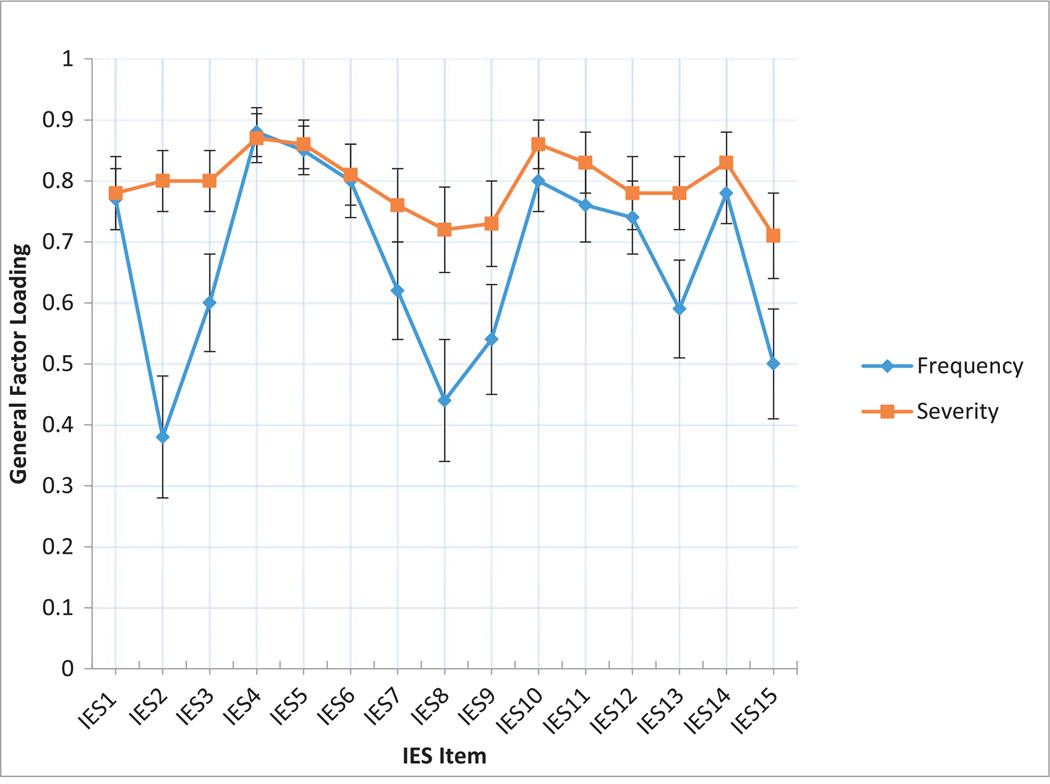
Note: When the discrimination parameters are transformed to general factor loadings (Wirth & Edwards, 2007), the picture is much the same. The Severity items had, on average, a loading that was .12 higher (range, .01 to .42) than the Frequency items. Error bars represent standard errors of measurement. Appendix A shows the Figure for the general factor loadings
Correlation with criterion mental health variables
Next, we correlated both the IES frequency items and the IES severity items with criterion validity variables. These variables included mental health (MHI-depression, MHIanxiety, MHI-behavioral control, and MHI-positive affect subscale scores), as well as quality of life (FACT-G functional, physical, social, and emotional well-being subscale scores). We hypothesized that both IES scales would be associated with the measures in the direction of poorer mental health and poorer health-related quality of life. In addition, we hypothesized IES severity would show stronger correlations with the criterion variables compared with the IES frequency.
Table 3 shows that, as expected, the IES frequency and severity scores were inversely related to better mental health and more positive health-related quality of life. In all cases, the correlation coefficients between the IES severity and the criterion variable were higher than the corresponding IES frequency correlation. Moreover, in all but one case, the differences were significantly higher (as indicated by dependent t-tests).
Table 3.
Pearson correlations between Impact of Events Scale frequency/Impact of Events Scale severity and convergent validity variables
| IES frequency | IES severity | |||||
|---|---|---|---|---|---|---|
| r | 95% CI | r | 95% CI | t-test | p | |
| MHI: anxiety | −0.41** | [−0.50, −0.32] | −0.52** | [−0.59, −0.44] | −3.85 | <0.001 |
| MHI: depression | −0.39** | [−0.48, −0.30] | −0.55** | [−0.62, −0.47] | −5.77 | <0.001 |
| MHI: behavioral control | −0.41** | [−0.50, −0.32] | −0.56** | [−0.63, −0.48] | −5.44 | <0.001 |
| MHI: positive affect | −0.33** | [−0.42, −0.23] | −0.34** | [−0.43, −0.24] | −0.32 | 0.75 |
| FACT-G: physical well-being | −0.44** | [−0.52, −0.35] | −0.60** | [−0.66, −0.53] | −6.01 | <0.001 |
| FACT-G: social/family well-being | −0.11* | [−0.22, −0.003] | −0.20** | [−0.30, −0.10] | −2.76 | 0.01 |
| FACT-G: emotional well-being | −0.54** | [−0.61, −0.46] | −0.70** | [−0.75, −0.64] | −6.71 | <0.001 |
| FACT-G: functional well-being | −0.31** | [−0.40, −0.21] | −0.42** | [−0.50, −0.33] | −3.63 | <0.001 |
Higher Mental Health Inventory and Functional Assessment of Cancer Therapy—General scores are indicative of better mental health and better quality of life, respectively. The t-tests for the differences between correlation coefficients were dependent on the correlation between the Impact of Events Scale severity and the Impact of Events Scale frequency.
IES, Impact of Events Scale; MHI, Mental Health Inventory; FACT-G, Functional Assessment of Cancer Therapy—General.
p < 0.05.
p < 0.01.
Discussion
This manuscript demonstrates, for the first time, the benefit of using a severity-based approach with the IES compared with a frequency-based approach to assessing the psychological impact of the cancer experience. Using a combination of classical test and item response theories, we provided evidence supporting the comparability of the IES severity items relative to the IES frequency items and suggesting that the IES severity items may even be psychometrically superior. By employing an approach that assesses the severity or distressing nature of intrusive or avoidant cognitions, the modified IES was a more reliable, informative, and valid measure than the standard IES that employs a frequency-based approach to assessing the impact of stressful life events.
Our hypothesis that the severity items would be a more informative approach to assessing cancer-related distress was supported. In this sample, the severity items captured the general trait of distress more accurately than the frequency items, evidenced by the higher discrimination parameters. In other words, most of the severity items did a better job than the frequency items at discriminating between low and high levels of cancer-specific distress. Moreover, the severity items demonstrated greater reliability, suggesting better measurement precision and reduced error. The frequency rating scale provides an index of the number of times an event is experienced, but it indicates nothing about the valence or whether or not that particular event was distressing. The frequency with which individuals experience specific stress-related phenomena, in this case, intrusive and avoidant thoughts about cancer, is only one dimension of the impact of the cancer experience, and it is not necessarily the most important dimension of that experience [37]. Although it is likely, given the nature of the item content for the IES, that higher frequency events are also distressing, it is also possible that as individuals begin to adapt to the cancer experience and integrate it into their lives, the frequency with which they experience certain intrusive and avoidant cognitions may remain relatively high but the distressing nature of those events may begin to decline as patients experience longer periods of disease-free survivorship.
The weakening of the connection between high frequency and high distressing events can be seen in clinical approaches to certain types of psychological disorders. Indeed, empirically supported therapies for managing anxiety disorders rely on behavioral approaches such as systematic graduated exposures to help clients begin to reduce their anxious responses to repeated confrontations with the anxiety-provoking stimuli [38,39]. In this case, high frequency events begin to lose their potency and have a progressively weaker impact on the client. Patients with cancer or other significantly stressful life experiences may also experience the same phenomenon over time, and this helps underscore why frequency assessments of cancer-specific (or trauma-specific) distress may not be the most meaningful approach to measuring these experiences for patients.
Our hypothesis that the severity items would show validity correlations that are as high as or higher than those obtained with the frequency items was also supported. IES severity items were more strongly correlated with poorer mental health and quality of life outcomes than frequency items. As already noted, this may be due to the fact that the frequency items may not necessarily indicate maladaptive processes. In fact, some models of cognitive processing [16] suggest that a high level of intrusions is indicative of fear network activation and may be necessary to foster network resolution through the integration of the cancer experience into one’s life. In other words, this perspective posits that high levels of intrusive thoughts may be a marker of an adaptive psychological process and not a maladaptive one. In contrast, for severity items, these are invariably negative or maladaptive in nature. Indeed, if a question asks about how ‘distressed or bothered’ someone was by intrusive or avoidant cognitions, it makes sense that these items would be more strongly correlated with higher levels of depression and anxiety and lower levels of behavioral control and emotional, physical, functional, and social well-being. The important finding here is not that the severity items were strongly associated with poorer mental health and quality of life outcomes, which is not particularly surprising, but that the severity items were more strongly associated with these outcomes than the standard IES frequency items. This underscores the importance of psychosocial screening for clinical stress reactions in cancer patients beyond traumatic stress, such as other anxiety or mood disorders as well as adjustment disorders [40].
This study has a few limitations. While the IES severity items showed higher reliability estimates than IES frequency items, it is possible that the severity question format introduced redundancy [41]. It is possible, for example, that when participants were asked about severity, they focused more on the ‘bother’ aspect relative to the specific item content, thereby glossing over the distinctions among the items. Following this logic, one might suggest that the stronger relationship between IES severity items and psychological adjustment measures reflects some loss of the distinctive IES construct validity. This would seem unlikely, however, given the high correlation we found between the IES measures (0.82). Nevertheless, further study with both item types with criterion validity variables should explore this alternative hypothesis.
Additionally, our sample was a predominantly White, highly educated sample recruited from an Internet panel company. This may raise concerns about the generalizability of our findings. However, recent research has supported the viability of web-based data collection by demonstrating that samples recruited from the Internet are comparable with data from probability-based general population samples [42]. Moreover, to effectively explore the psychological impact of the cancer experience, it is important to have a sufficiently distressed sample. Prior work from this dataset has demonstrated that these cancer survivors are reporting clinically significant levels of distress [11] and are, thus, an appropriate sample for addressing these research questions. Our sample was composed of cancer survivors, and the generalizability of these findings to other patient populations who have experienced significant life threats is not known. It is reasonable to expect that our findings would generalize to other patient populations, but this is an assumption that warrants additional empirical studies with other patients who have experienced different types of stressful and traumatic events.
In sum, these results suggest that the IES severity items, perhaps because of the improvements in reliability, are better able to capture negative mental health aspects of the IES. The high correlation between the IES severity and IES frequency items (0.82) suggests that the IES severity items still mostly measure the same construct. Future studies of the impact of traumatic events would likely benefit from using the IES-R because of its severity-based response options instead of the IES. Alternatively, the IES and the IES-R measures could feasibly be ‘linked’ psychometrically [43,44] such that a table equating the summed score of each measure could be constructed. This would allow researchers to directly compare scores obtained with IES frequency to IES severity items and allow for the creation of an equivalent clinical cut-off score to help guide provision of services. In turn, this will enhance our understanding of the experiences of patients with cancer and other significant life stressors and identify the most vulnerable subgroups in need of psychosocial care.
Acknowledgements
Research reported in this publication was supported by the American Cancer Society—Illinois Division under award number PSB-08-15 and the National Cancer Institute of the NIH under award number K07CA158008. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Appendix A
General factor loadings of the severity items versus frequency items of the Impact of Events Scale (IES) in a full-information bifactor model
Note: Error bars represent standard errors of measurement.
Footnotes
The authors have no financial disclosures or conflicts of interest to report.
References
- 1.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;413:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Weiss DS, Marmar CR. The Impact of Event Scale-revised. In: Wilson JP, Martin KT, editors. Assessing Psychological Trauma and PTSD: A Handbook for Practitioners. New York: Guilford; 1996. pp. 399–411. [Google Scholar]
- 3.Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association; 2000. [Google Scholar]
- 4.Schwarzwald J, Solomon Z, Weisenberg M, Mikulincer M. Validation of the Impact of Event Scale for psychological sequelae of combat. J Consult Clin Psychol. 1987;552:251–256. doi: 10.1037//0022-006x.55.2.251. [DOI] [PubMed] [Google Scholar]
- 5.Kenardy J, Webster R, Lewin T, Carr V, Hazell P, Carter G. Stress debriefing and patterns of recovery following a natural disaster. J Trauma Stress. 1996;91:37–49. doi: 10.1007/BF02116832. [DOI] [PubMed] [Google Scholar]
- 6.Horowitz MJ. Stress Response Syndromes. Northvale, NJ: Jason Aronson Press; 1986. [Google Scholar]
- 7.Brady KT, Dansky BS, Back SE, Foa EB, Carroll KM. Exposure therapy in the treatment of PTSD among cocaine-dependent individuals: preliminary findings. J Subst Abuse Treat. 2001;211:47–54. doi: 10.1016/s0740-5472(01)00182-9. [DOI] [PubMed] [Google Scholar]
- 8.Cordova MJ, Andrykowski MA, Kenady DE, McGrath PC, Sloan DA. Frequency and correlates of post-traumatic-stress-disorder like symptoms after treatment for breast cancer. J Consult Clin Psychol. 1995;63:6–981. doi: 10.1037//0022-006x.63.6.981. [DOI] [PubMed] [Google Scholar]
- 9.Kangas M, Henry JL, Bryant RA. Posttraumatic stress disorder following cancer. A conceptual and empirical review. Clin Psychol Rev. 2002;224:499–524. doi: 10.1016/s0272-7358(01)00118-0. [DOI] [PubMed] [Google Scholar]
- 10.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5 ed. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 11.Yanez B, Garcia S, Victorson D, Salsman JM. Distress among young adult cancer survivors: a cohort study. Support Care Cancer. 2013;219:2403–2408. doi: 10.1007/s00520-013-1793-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwartz MD, Lerman C, Audrain J, et al. The impact of a brief problem-solving training intervention for relatives of recently diagnosed breast cancer patients. Ann Behav Med. 1998;201:7–12. doi: 10.1007/BF02893803. [DOI] [PubMed] [Google Scholar]
- 13.Zakowski SG, Valdimarsdottir HB, Bovbjerg DH, et al. Predictors of intrusive thoughts and avoidance in women with family histories of breast cancer. Ann Behav Med. 1997;194:362–369. doi: 10.1007/BF02895155. [DOI] [PubMed] [Google Scholar]
- 14.Koopman C, Butler LD, Classen C, et al. Traumatic stress symptoms among women with recently diagnosed primary breast cancer. J Trauma Stress. 2002;154:277–287. doi: 10.1023/A:1016295610660. [DOI] [PubMed] [Google Scholar]
- 15.Myers SB, Manne SL, Kissane DW, et al. Social–cognitive processes associated with fear of recurrence among women newly diagnosed with gynecological cancers. Gynecol Oncol. 2013;1281:120–127. doi: 10.1016/j.ygyno.2012.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Creamer M, Burgess P, Pattison P. Reaction to trauma: a cognitive processing model. J Abnorm Psychol. 1992;1013:452–459. doi: 10.1037//0021-843x.101.3.452. [DOI] [PubMed] [Google Scholar]
- 17.Carpenter K, Fowler J, Maxwell GL, Andersen B. Direct and buffering effects of social support among gynecologic cancer survivors. Ann Behav Med. 2010;391:79–90. doi: 10.1007/s12160-010-9160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chambers SK, Zajdlewicz L, Youlden DR, Holland JC, Dunn J. The validity of the distress thermometer in prostate cancer populations. Psycho-Oncology. 2014;232:195–203. doi: 10.1002/pon.3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yanez B, Edmondson D, Stanton AL, et al. Facets of spirituality as predictors of adjustment to cancer: relative contributions of having faith and finding meaning. J Consult Clin Psychol. 2009;774:730–741. doi: 10.1037/a0015820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cella D, Riley W, Stone A, et al. The Patient-reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;6311:1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gershon R, Lai J, Bode R, et al. Neuro-QOL: quality of life item banks for adults with neurological disorders: item development and calibrations based upon clinical and general population testing. Qual Life Res. 2012;213:475–486. doi: 10.1007/s11136-011-9958-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salsman JM, Garcia SF, Yanez B, Sanford SD, Snyder MA, Victorson D. Physical, emotional, and social health differences between post-treatment young adults with cancer and matched healthy controls. Cancer. 2014;12015:2247–2254. doi: 10.1002/cncr.28739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–655. [PubMed] [Google Scholar]
- 24.Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol. 1993;113:570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 25.Veit CT, Ware JE., Jr The structure of psychological distress and well-being in general populations. J Consult Clin Psychol. 1983;515:730–742. doi: 10.1037//0022-006x.51.5.730. [DOI] [PubMed] [Google Scholar]
- 26.McDonald RP. Test Theory: A Unified Treatment. Mahwah, NJ: Lawrence Earlbaum Associates, Inc.; 1999. [Google Scholar]
- 27.psych: procedures for personality and psychological research. Evanston, Illinois, USA: Northwestern University; 2013. (R package version 1.2-1), [computer program]. [Google Scholar]
- 28.R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2011. [computer program]. [Google Scholar]
- 29.IRTPRO 2.1 for Windows. Lincolnwood, IL: Scientific Software International, Inc.; 2011. [computer program]. [Google Scholar]
- 30.Bock RD, Aitkin M. Marginal maximum likelihood estimation of item parameters: application of an EM algorithm. Psychometrika. 1981;464:443–459. [Google Scholar]
- 31.Divgi DR. Calculation of the tetrachoric correlation coefficient. Psychometrika. 1979;442:169–172. [Google Scholar]
- 32.Woods C. Factor analysis of scales composed of binary items: illustration with the Maudsley Obsessional Compulsive Inventory. J Psychopathol Behav Assess. 2002;244:215–223. [Google Scholar]
- 33.Reise SP, Scheines R, Widaman KF, Haviland MG. Multidimensionality and structural coefficient bias in structural equation modeling: a bifactor perspective. Educ Psychol Meas. 2013;731:5–26. [Google Scholar]
- 34.Wirth RJ, Edwards MC. Item factor analysis: current approaches and future directions. Psychol Methods. 2007;121:58–79. doi: 10.1037/1082-989X.12.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Edelen MO, Reeve BB. Applying item response theory (IRT) modeling to questionnaire development, evaluation, and refinement. Qual Life Res. 2007;16(Suppl 1):5–18. doi: 10.1007/s11136-007-9198-0. [DOI] [PubMed] [Google Scholar]
- 36.Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D. Item banks for measuring emotional distress from the Patient-reported Outcomes Measurement Information System (PROMIS): depression, anxiety, and anger. Assessment. 2011;183:263–283. doi: 10.1177/1073191111411667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Salsman JM, Segerstrom SC, Brechting EH, Carlson CR, Andrykowski MA. Posttraumatic growth and PTSD symptomatology among colorectal cancer survivors: a three-month longitudinal examination of the cognitive processing. Psycho-Oncology. 2009;18:30–41. doi: 10.1002/pon.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Foa EB, Kozak MJ. Emotional processing of fear: exposure to corrective information. Psychol Bull. 1986;991:20–35. [PubMed] [Google Scholar]
- 39.Wolpe J. The systematic desensitization treatment of neuroses. J Nerv Ment Dis. 1961;1323:189–203. doi: 10.1097/00005053-196103000-00001. [DOI] [PubMed] [Google Scholar]
- 40.Kangas M. DSM-5 trauma and stress-related disorders: implications for screening for cancer-related stress. Front Psychiatry. 2013;4122:1–3. doi: 10.3389/fpsyt.2013.00122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Clark LA, Watson D. Constructing validity: basic issues in objective scale development. Psychol Assess. 1995;73:309. doi: 10.1037/pas0000626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu H, Cella D, Gershon R, et al. Representativeness of the PROMIS Internet panel. J Clin Epidemiol. 2010;6311:1169–1178. doi: 10.1016/j.jclinepi.2009.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dorans NJ. Linking scores from multiple health outcome instruments. Qual Life Res. 2007;16(Supplement 1):85–94. doi: 10.1007/s11136-006-9155-3. [DOI] [PubMed] [Google Scholar]
- 44.Schalet BD, Cook KF, Choi SW, Cella D. Establishing a common metric for self-reported anxiety: linking the MASQ, PANAS, and GAD-7 to PROMIS anxiety. J Anxiety Disord. 2014;281:88–96. doi: 10.1016/j.janxdis.2013.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]