Abstract
Production of extended-spectrum β-lactamases (ESBLs) producing E. coli in animals and different methods of identifications from Ado Ekiti, Ekiti State, Nigeria, were investigated. Three hundred and fifty fecal samples, collected from apparently healthy cattle and pigs, were cultured and identified following standard procedures. ESBL phenotypic detection was carried out using combination disc test, double disc synergism test, and ESBL brilliance agar screening. Molecular detection of TEM, SHV, and CTX-M genes was carried out using standard molecular method. One hundred and fourteen E. coli isolates were recovered from the 350 samples processed, out of which 72 (63.2%) isolates were positive for ESBLs with multiple resistance to the antibiotics used. Eighty-one (71%) isolates were positive for ESBL by combination disc test, 90 (78.9%) were positive for double disc synergism test, and 93 (81.6%) were positive for ESBL brilliance agar. TEM and CTX-M genes were detected in 48 (42.1%) and 51 (44.7%) isolates, respectively. SHV gene was not detected in any of the isolates while TEM and CTX-M were detected in 33 (28.9%) isolates. This study showed high resistance of E. coli to antibiotics, particularly to the third generation cephalosporins. Regular monitoring and regulated use of antibiotics in livestock should be encouraged.
1. Introduction
Production of extended-spectrum β-lactamases (ESBLs) is the most common mechanism of resistance to third-generation cephalosporins among Enterobacteriaceae including Klebsiella pneumoniae and Escherichia coli [1, 2]. ESBL determinants have been detected not only in clinical isolates but also in commensal bacteria from humans and animals and in isolates from products of the food chain and sewage, revealing distribution and suggesting the presence of environmental reservoirs for these resistance determinants [3, 4].
The increase in antimicrobial-resistant bacteria of animal origin resembles the process in humans about two decades ago [5]. Since the late 1990s, extended-spectrum β-lactamase (ESBL) producing Enterobacteriaceae, in particular E. coli, have emerged globally. Initially, ESBL producing bacteria were only observed in human medical practice [6, 7] but the recent observation of these bacteria, first in companion animals and increasingly in livestock, has initiated monitoring studies focused on livestock [8]. ESBL producing E. coli isolates are now being found in increasing numbers of food-producing animals leading to the hypothesis that animals might become infection sources or even reservoirs (the natural persistent source of infection) contributing to the spread of these bacteria [9].
Currently, there is paucity of information on ESBL producing E. coli from animals and the possible contribution of these resistant species to the ever growing antimicrobial resistance observed in humans. The broad objective of this study was to determine the occurrence of ESBL producing Escherichia coli in cattle and pigs in Ado Ekiti, South Western Nigeria.
2. Materials and Methods
2.1. Sample Collection
Three hundred and fifty fecal samples were collected from cattle (n = 200) and pigs (n = 150). Samples from apparently healthy cattle were collected from the colon immediately after slaughtering the animal at the abattoirs aseptically. Freshly passed feces from apparently healthy pigs were collected into sterile capped universal bottles with sterile spatula and were transported to the laboratory immediately.
2.2. Isolation and Identification
Isolates were recovered from the samples after culturing on modified selenite F and incubated for 18–24 hours at 37°C. The overnight incubated liquid selective media were inoculated on Sorbitol Macconkey Agar, Eosin Methylene Blue Agar, and Macconkey Agar and incubated for 18–24 hours at 37°C. Presumptive characteristic E. coli isolates were identified and confirmed using arrays of biochemical tests and API 20 E multitest systems (bioMérieux, France). The study was carried out in the Department of Medical Laboratory Science, ABUAD, Ado Ekiti, and the Department of Medical Microbiology and Parasitology LAUTECH, Osogbo, between February and November 2014.
2.3. Susceptibility Test
Antimicrobial susceptibility of pure colonies to Ampicillin (10 μg), Amoxicillin (25 μg), Augmentin (AUG) (30 μg), Cefotaxime (CTX) (30 μg), Ceftazidime (CAZ) (30 μg), Cefuroxime (CXM) (30 μg), Ciprofloxacin (CPX) (10 μg), Cefixime (CXM) (5 μg), Cefpodoxime (CP) (10 μg), Ofloxacin (5 μg), Imipenem (10 μg), Tetracycline (30 μ), Gentamicin (GEN) (10 μg), Streptomycin (STR) (10 μg), Erythromycin (ERY) (10 μg), Chloramphenicol (CHL) (25 μg), Cloxacillin (5 μg), Nitrofurantoin (NIT), and Cotrimoxazole (STX) (25 μg) was determined and interpreted by the disc diffusion method following the guidelines of Clinical Laboratory Standard Institute [10].
2.4. Detection of Extended-Spectrum β-Lactamase (ESBL)
2.4.1. Cefpodoxime and Cefpodoxime-Clavulanate (Combination Disc Screening)
Cefpodoxime and Cefpodoxime-clavulanate (Oxoid, Basingstoke, UK) discs were applied on freshly prepared Muller Hinton agar and the plates were incubated aerobically at 37°C. A final measurement of the zone of inhibition was made after overnight incubation. ESBL producers were defined as having a differential zone diameter of ≥+5 mm (Cefpodoxime-clavulanate zone − Cefpodoxime zone).
2.5. Double Disc Diffusion Test
A Ceftazidime 30 μg disc and Cefotaxime 30 μg disc with Amoxicillin/clavulanic acid 20/10 μg (Oxoid, UK) were placed in the center 20 mm apart and incubated at 37°C for 18–20 hours [11]. ESBL production was inferred when the zone of inhibition around the Ceftazidime and Cefotaxime discs was expanded by the presence of clavulanate by ≥5 mm.
2.6. ESBL Brilliance Agar
Oxoid ESBL brilliance agar was inoculated according to manufacturer's instructions. Plates were inoculated with 1 μL (a standard loopful) of a 0.5 McFarland standard suspension of E. coli. Subsequently they were incubated aerobically at 35 to 37°C for 18 to 24 hours in an inverted position and presumptive ESBL E. coli were identified based on color production. Escherichia coli produced blue/pink coloration following 24–48 hours of incubation. The reference E. coli strain ATCC25922 was inhibited and was used as negative control.
2.7. Polymerase Chain Reaction to Detect bla Genes
The DNA of the ESBL confirmed isolates was extracted separately using a DNA extraction kit (Biospin plasmid extraction, Bioflux, Japan). According to previously published work, PCR was used to detect bla TEM, bla CTX-M, and bla SHV genes using specific primers [12]. Routine reactions were performed using the PCR master mix containing 3 μL deoxynucleoside triphosphate (dNTPs), 4 μL ×10 Tris EDTA buffer, 0.2 μL Thermus aquaticus (Taq) polymerase, 0.5 μL MgCl2, 5 μL DNA lysates, 15.3 μL of PCR water, and 1 μL of forward and reverse primers in a 30 μL final reaction volume. Electrophoresis was done using 1% Agarose.
2.8. Statistical Analysis
The sensitivities and specificities of the tests were determined. Differences in sensitivity and specificity of the tests were analyzed with the chi square test and log linear analysis using the Statistical Package for Social Sciences software (SPSS version 21).
3. Results
Table 1 shows the highest prevalence of Klebsiella spp. both in cattle and in pigs showing 125 and 70, respectively, while the least bacterial isolate was Proteus spp. with a prevalence of 21 and 10 for cattle and pigs, respectively, and Escherichia coli and Pseudomonas spp. were 114 and 129, respectively.
Table 1.
Distribution of gram negative organisms isolated from cattle and pigs.
| Number of samples | Proteus spp. | E. coli | Pseudomonas spp. | Klebsiella spp. |
|---|---|---|---|---|
| Cattle | 21 | 79 | 84 | 125 |
| Pigs | 10 | 35 | 45 | 70 |
| Total | 31 | 114 | 129 | 195 |
Table 2 shows the distribution and sources of fecal samples; female cow investigated was 73, while bull male was 127 and 10 large pigs were the least collected.
Table 2.
Distribution and sources of the fecal samples.
| Cattle | Pigs |
|---|---|
| Cow (female) 73 | Soar (female) 135 (10 piglets) |
| Large white 65 | |
| Large black 10 | |
| Hampshire 45 | |
| Duroc 15 | |
|
| |
| Bull (male) 127 | Boar (male) 15 |
3.1. Antibiotic Susceptibility Patterns of E. coli Isolates
Table 3 shows the results of all the 114 E. coli isolates that were subjected to antimicrobial testing and interpreted as resistant, intermediate, and sensitive following the guidelines of Clinical Laboratory Standard Institute [10]. The overall resistance of the isolates to antibiotics shows that resistance to Penicillin (PEN) (96%), Ampicillin (AMC) (89%), Amoxicillin (AMX) (88%), Augmentin (AUG) (96%), Cefotaxime (CTX) (92%), Cefuroxime (CPX) (83%), Cloxacillin (CXC) (84%), and Cotrimoxazole (STX) (90%) was high while resistance to Ciprofloxacin and Ofloxacin was low with 5% resistance to these antibiotics. The isolates also showed considerable resistance to Ampicillin, Tetracycline, Cotrimoxazole, and Cephalosporins as shown in Table 3.
Table 3.
Antimicrobial sensitivity patterns of E. coli isolates based on the classes of antibiotics tested.
| Class/antibiotics | Number of resistant isolates (%) | Number of intermediate isolates (%) | Number of sensitive isolates (%) |
|---|---|---|---|
| β-lactams | |||
| Penicillin | 110 (96%) | 04 (4%) | — |
| Amoxicillin | 100 (88%) | 14 (12%) | — |
| Ampicillin | 102 (89%) | 12 (11%) | — |
| Augmentin | 110 (96%) | 04 (4%) | — |
| Ceftazidime | 66 (58%) | 27 (24%) | 21 (18%) |
| Cefotaxime | 105 (92%) | 9 (8%) | — |
| Cefixime | 45 (39%) | 42 (37%) | 27 (24%) |
| Cefuroxime | 95 (83%) | 10 (9%) | 8 (7%) |
| Cefpodoxime | 66 (58%) | 06 (5%) | 42 (37%) |
| Tetracycline | 100 (88%) | 9 (8%) | 4 (4%) |
| Erythromycin | 94 (82%) | 15 (13%) | 5 (4%) |
| Streptomycin | 90 (79%) | 15 (13%) | 9 (8%) |
| Gentamicin | 56 (49%) | 03 (3%) | 55 (48%) |
| Ciprofloxacin | 6 (5%) | 6 (5%) | 102 (90%) |
| Ofloxacin | 6 (5%) | 5 (4%) | 103 (90%) |
| Cloxacillin | 96 (84%) | 18 (16%) | — |
| Cotrimoxazole | 102 (90%) | 12 (10%) | — |
| Nitrofurantoin | — | 12 (11%) | 102 (89%) |
| Chloramphenicol | 105 (92%) | 9 (8%) | — |
| Carbapenem | |||
| Imipenem | — | 5 (4%) | 109 (96%) |
The number of isolates that showed resistance simultaneously to twelve (12) different antibiotics was 42 (37.8%) and was highest among those isolates that demonstrated multiple antibiotic resistance while only 6 (5.6%) isolates showed resistance simultaneously to fifteen out of the 20 antibiotics tested. All the 114 E. coli isolates showed resistance to at least nine antibiotics. All isolates that were resistant to more than two classes were identified as multidrug resistant (MDR) isolates and were selected for possible ESBL production screening (Table 4).
Table 4.
The frequency distribution of antibiotics and resistant isolates.
| Number of antibiotics | Number of resistant isolates (%) |
|---|---|
| 09 | 03 (2.6%) |
| 10 | 12 (10.5%) |
| 11 | 06 (5.6%) |
| 12 | 42 (37.8%) |
| 13 | 24 (21%) |
| 14 | 18 (15.8%) |
| 15 | 09 (7.9%) |
3.2. Phenotypic Test
Figure 1 shows the results of the phenotypic tests used. Eighty-one (71%) isolates out of the 114 isolates were positive for combination disc test (Cefpodoxime/clavulanic acid) as shown in the figure. There was a significant association (p = 0.026) between Cefpodoxime/clavulanic acid and the detection of ESBL genes (CTX, SHV, and TEM). The sensitivity of the test was calculated using molecular detection as the gold standard was 89% while specificity was 82%. The rate of false positive prediction (1 − specificity) was 0.18 (18%). Double disc synergism test using Cefotaxime/Ceftazidime/clavulanate substrate was positive in 90 (78.9%) isolates out of the 114 isolates. There was an association between this phenotypic test and the detection of CTX-M genes (p = 0.025) and TEM genes (p < 0.001) (Table 5). The sensitivity of the test was 80% while specificity was 70%. The rate of false positive prediction (1 − specificity) was 30%. ESBL brilliance agar was positive in 93 (81.57%) isolates. There was a significant association (p < 0.001) in the result obtained by Cefpodoxime/clavulanic acid and ESBL brilliance agar. The sensitivity of the test was 79% and specificity was 67% while rate of false positive prediction was 33%.
Figure 1.
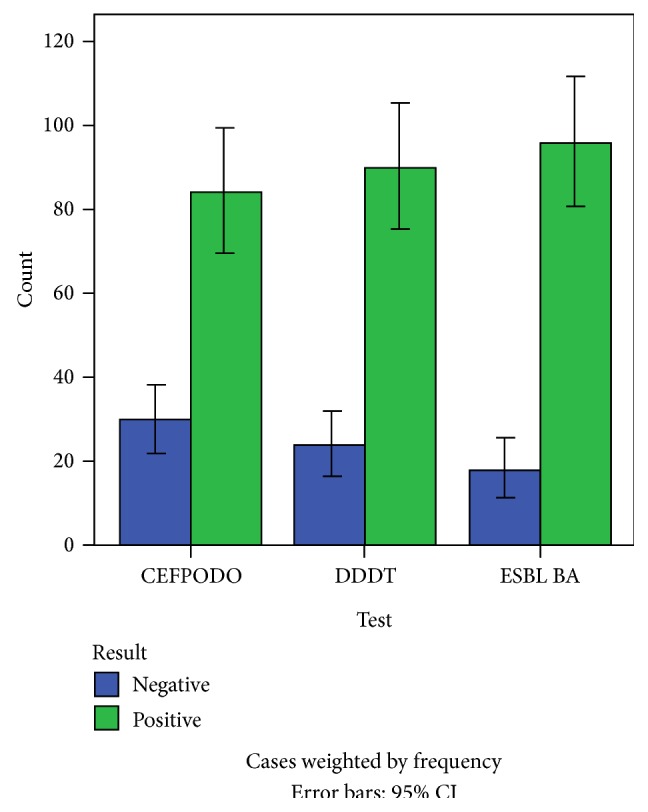
Representation of phenotypic detection of ESBL.
Table 5.
Association of phenotypic tests and molecular characterization of E. coli isolates from animals.
| Interactions | Chi square (χ 2) | Significance | Degree of freedom |
|---|---|---|---|
| CEFPODOXIME/ESBL BA/DDDT/GENE | 0.000 | 1.00 | 1 |
| ESBL BA/GENES | 0.000 | 1.000 | 1 |
| CEFPODOXIME/DDST/GENE | 4.961 | 0.026∗ | 1 |
| CEFPODOXIME/ESBL BA | 17.540 | <0.001∗ | 1 |
| ESBL BA/DDST | 24.466 | <0.001∗ | 1 |
| ESBL BA/CTX_M | 0.000 | 1.000 | 2 |
| CEFPODOXIME/DDST/CTX | 5.009 | 0.025∗ | 1 |
| ESBL BA/TEM | 0.000 | 1.000 | 2 |
| CEPODOXIME/TEM | 0.165 | 0.684 | 2 |
| DDST/TEM | 22.407 | <0.001∗ | 1 |
| ESBL BA/SHV | 0.000 | 1.000 | 2 |
| DDST/SHV | 0.000 | 1.000 | 2 |
| CEFPODOXIME/SHV | 0.000 | 1.000 | 2 |
∗Statistically significant.
CEFPODOXIME: Cefpodoxime screening test.
DDST: double disc synergism test.
ESBL BA: ESBL brilliance agar screening test.
SHV: detection of SHV genes.
TEM: detection of TEM genes.
CTX-M: detection of CTX-M genes.
3.3. Detection of ESBL Genes
The molecular characterization of resistant gene of the E. coli isolates using PCR was analysed. SHV showed no specific amplification and thus was not detected in any of the samples. A total of 51 (44.7%) isolates showed detectable CTX-M genes while TEM genes were present in 48 (42%) E. coli isolates.
4. Discussion and Conclusion
Antibiotic resistance has continued to constitute serious problems not only in human medicine but also in animal husbandry, livestock management, and veterinary medicine [13, 14].
In this study, several methods of detection were employed as previously reported methods of ESBLs detection. The major finding in the present study is the presence of multiple drug resistant commensal E. coli in animals to commonly used antibiotics such as Penicillin (96%), Augmentin (96%), Cefotaxime (92%), Ceftazidime (58%), Cefuroxime (83%), and Cotrimoxazole (STX) (90%). This observation reiterates the finding in other studies that have reported antibiotic resistance among bacteria especially E. coli isolated from cattle and other animals is increasing at an alarming rate [15–18]. In this study, susceptibility of all the isolates that showed multiple resistance to a minimum of nine antibiotics was 3 (2.6%). 12 (10.5%) isolates were resistant to ten antibiotics, 6 (5.6%) isolates were resistant to 13 different antibiotics, and 42 (36.8%) isolates were resistant to twelve antibiotics, while 9 (7.9%) isolates were resistant to fifteen antibiotics. This finding correlates with similar results obtained from other studies that have reported some levels of multiple antibiotic resistance by E. coli from cattle, meat products, and other animals [19, 20]. Ajayi et al. [17] determined the antibiotic susceptibility patterns of commensal E. coli from feces of apparently healthy cattle in Ado Ekiti, Nigeria, from ready to slaughter cattle. Their result revealed E. coli isolates which showed resistance to at least 3 of the eight antibiotics tested [17]. All the isolates showing multiple antimicrobial resistance in this study were screened for possible ESBL production. Extended-spectrum β-lactamase indeed is a superbug of trouble to clinicians and microbiologists and is creating environmental stress to pharmaceutical pipeline in the development of new antibiotics.
The Health Protection Agency of the United Kingdom recommends testing Cefpodoxime or both Cefotaxime and Ceftazidime as a first screening test [21]. This study revealed the combination of the two latter drugs separated at 20 mm distance achieves 80% sensitivity to adequately detect ESBL production, meaning that only 20% of the isolates would need further testing. This conforms to some other studies. Garrec et al. [22] reported a sensitivity of 77% using this same method. Generally, evaluations of the double disc diffusion test have revealed sensitivities of the method ranging from 79% to 97% and specificities ranging from 94% to 100% [23, 24]. The sensitivity of Cefpodoxime in this study was 89% while specificity was 82%. The rate of false positive prediction (1 − specificity) was 0.18 (18%). Cefpodoxime was found to have the highest sensitivity in this study and is thus in agreement with a study by Jain and Mondal [25] who concluded their report using the standard disc diffusion as screening test for identifying ESBL producers that Cefpodoxime was found to be the most efficient antimicrobial agent having a sensitivity of 93% and a specificity of 85.7% in screening isolates as potential ESBL producers followed by Ceftazidime with a sensitivity of 89.6% and specificity of 80.9% and Cefotaxime having sensitivity of 81.6% and specificity 85.7% [25]. However, it has been reported that it is adequate to use Cefotaxime, which is consistently susceptible to CTX-M, and Ceftazidime, which is a consistently good substrate for TEM and SHV variants but if only one drug is to be used, then the single best indicator for ESBL producer has been found to be Cefpodoxime [11, 26].
Using the Oxoid ESBL brilliance Agar, the sensitivity was 79% and specificity was 67%, while rate of false positive prediction (1 − specificity) was 33%. This was in contrast to a study published by Huang et al. [27], who reported a sensitivity of 94.9% and specificity of 95.7%. According to data on file at Oxoid (http://www.oxoid.com/), the performance of this product was rated as sensitivity having 95% and specificity having 94%. The differences observed in this study could be due to the use of already well characterized (known) ESBL producing isolates in the evaluation as well published that any results obtained by this method are presumptive and should be confirmed by other methods.
Following the screening of the E. coli isolates for ESBL genes using Polymerase Chain Reaction (PCR), bla TEM was detected in 48 (42.1%) and bla CTX-M was detected in 51 (44.7%) and bla SHV1 was not detected in any of the isolates. These findings suggest that bla CTX-M was more common among the ESBL genes in these isolates which conforms to other studies [11, 28]. In this study, the occurrence of ESBL producing E. coli was as high as 63.2% as ESBL genes were detected in 72 out of 114 isolates screened. This is alarming and worrisome and higher than reports from clinical isolates in Nigeria, class A and D ESBLs and p-AmpC were found in hospital settings, and the prevalence ranged from 10.3 to 27.5% [6, 29–32].
Although most of these studies were done using E. coli isolates from humans, ESBLs have been reported to be plasmid encoded implying that these resistance determinants are found in our environment and can be transferred from one organism to another. The high prevalence of these ESBL producers in fecal samples of animal further buttresses the hypothesis that animals might become infection sources or even reservoirs (the natural persistent source of infection) contributing to the spread of these bacteria [9]. These resistant traits call for gross surveillance in community settings because ESBLs gene is a world growing treat for available antibiotics but its epidemiological effect and evaluation are still underestimated with low awareness.
In conclusion, to the best of our knowledge this is the first report of phenotypic and molecular investigation of bla genes (CTX, SHV, and TEM) from animal fecal samples and epidemiological relevance of different phenotypic and molecular methods. Multiple drug resistant ESBL producing E. coli is present in fecal samples of cattle and pigs in Ado Ekiti. The differences observed in the detection of ESBL positive isolates by the three different methods may be justified by the lower sensitivity of the phenotypic methods and the influence of environmental factors on the incidence of resistance.
Acknowledgments
The authors sincerely thank all the medical laboratory scientists at the LAUTECH Teaching Hospital and Medical Laboratory Complex College of Health Sciences, Isale Osun, Osogbo, for their help, support, and contribution to the success of this project. They thank Mrs. Adefioye S and Mrs. Olowe RA for reading the paper.
Conflict of Interests
The authors declared that they have no conflict of interests.
References
- 1.Paterson D. L., Bonomo R. A. Extended-spectrum β-lactamases: a clinical update. Clinical Microbiology Reviews. 2005;18(4):657–686. doi: 10.1128/cmr.18.4.657-686.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pitout J. D., Laupland K. B. Extended-spectrum beta-lactamase-producing Enterobacteriaceae: an emerging public-health concern. The Lancet Infectious Diseases. 2008;8(3):159–166. doi: 10.1016/s1473-3099(08)70041-0. [DOI] [PubMed] [Google Scholar]
- 3.Briñas L., Moreno M. A., Zarazaga M., et al. Detection of CMY-2, CTX-M-14, and SHV-12 β-lactamases in Escherichia coli fecal-sample isolates from healthy chickens. Antimicrobial Agents and Chemotherapy. 2003;47(6):2056–2058. doi: 10.1128/aac.47.6.2056-2058.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Briñas L., Zarazaga M., Sáenz Y., Ruiz-Larrea F., Torres C. β-Lactamases in ampicillin-resistant Escherichia coli isolates from foods, humans, and healthy animals. Antimicrobial Agents and Chemotherapy. 2002;46(10):3156–3163. doi: 10.1128/aac.46.10.3156-3163.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ewers C., Grobbel M., Bethe A., Wieler L. H., Guenther S. Extended-spectrum beta-lactamases-producing gram-negative bacteria in companion animals: action is clearly warranted! Berliner und Münchener Tierärztliche Wochenschrift. 2011;124:10–17. [PubMed] [Google Scholar]
- 6.Ogbolu D. O., Alli O. A. T., Olanipekun L. B., Ojo O. I., Makinde O. O. Faecal carriage of extended-spectrum beta-lactamase (ESBL)-producing commensal Klebsiella pneumoniae and Escherichia coli from hospital out-patients in Southern Nigeria. International Journal of Medicine and Medical Sciences. 2013;5(3):97–105. doi: 10.5897/IJMMS12.0005. [DOI] [Google Scholar]
- 7.Olowe O. A., Oladipo G. O., Makanjuola O. A., Olaitan J. O. Prevalence of extended spectrum beta-lactamases (esbls) carrying genes in Klebsiella spp from clinical samples at ile-ife, south western Nigeria. International Journal of Pharma & Bio Sciences. 2012;1(2) [Google Scholar]
- 8.Smet A., van Nieuwerburgh F., Vandekerckhove T. T. M., et al. Complete nucleotide sequence of CTX-M-15-plasmids from clinical Escherichia coli isolates: insertional events of transposons and insertion sequences. PLoS ONE. 2010;5(6) doi: 10.1371/journal.pone.0011202.e11202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carattoli A. Animal reservoirs for extended spectrum β-lactamase producers. Clinical Microbiology and Infection. 2008;14(1):117–123. doi: 10.1111/j.1469-0691.2007.01851.x. [DOI] [PubMed] [Google Scholar]
- 10.Clinical and Laboratory Standards Institute (CLSI) Document. M100-S21s. Wayne, Pa, USA: Clinical and Laboratory Standards Institute; 2011. Performance standards for antimicrobial susceptibility testing: twenty-first informational supplement. [Google Scholar]
- 11.Jarlier V., Nicolas M. H., Fournier G., Philippon A. ESBLs conferring transferable resistance to newer-lactam agents in Enterobacteriaceae: hospital prevalence and susceptibility patterns. Reviews of Infectious Diseases. 1988;10:867–878. doi: 10.1093/clinids/10.4.867. [DOI] [PubMed] [Google Scholar]
- 12.Chen H., Shu W., Chang X., Chen J.-A., Guo Y., Tan Y. The profile of antibiotics resistance and integrons of extended-spectrum β-lactamase producing thermotolerant coliforms isolated from the Yangtze River basin in Chongqing. Environmental Pollution. 2010;158(7):2459–2464. doi: 10.1016/j.envpol.2010.03.023. [DOI] [PubMed] [Google Scholar]
- 13.Witte W. Medical consequences of antibiotic use in agriculture. Science. 1998;279(5353):996–997. doi: 10.1126/science.279.5353.996. [DOI] [PubMed] [Google Scholar]
- 14.Lawson M. A. The antibiotic resistance problem revisited. American Biology Teacher. 2008;70(7):405–410. doi: 10.1662/0002-7685(2008)70[405:tarpr]2.0.co;2. [DOI] [Google Scholar]
- 15.Aibinu I., Aednipekun E., Odugbemi T. Emergence of quinolone resistance amongst Escherichia coli strains isolated from clinical infections in some Lagos state hospitals, in Nigeria. Nigerian Journal of Health and Biomedical Sciences. 2004;3(2):73–78. doi: 10.4314/njhbs.v3i2.11513. [DOI] [Google Scholar]
- 16.Kozak G. K., Boerlin P., Janecko N., Reid-Smith R. J., Jardine C. Antimicrobial resistance in Escherichia coli isolates from Swine and wild small mammals in the proximity of swine farms and in natural environments in Ontario, Canada. Applied and Environmental Microbiology. 2009;75(3):559–566. doi: 10.1128/aem.01821-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ajayi A. O., Oluyege A. O., Olowe O. A., Famurewa O. Antibiotic resistance among commensal Escherichia coli isolated from faeces of cattle in Ado-Ekiti, Nigeria. Journal of Animal and Veterinary Advances. 2011;10(2):174–179. doi: 10.3923/javaa.2011.174.179. [DOI] [Google Scholar]
- 18.Ogunleye A. O., Oyekunle M. A., Sonibare A. O. Multidrug resistant Escherichia coli isolates of poultry origin in Abeokuta, South Western Nigeria. Veterinarski Arhiv. 2008;78(6):501–509. [Google Scholar]
- 19.Sáenz Y., Zarazaga M., Brias L., Lantero M., Ruiz-Larrea F., Torres C. Antibiotic resistance in Escherichia coli isolates obtained from animals, foods and humans in Spain. International Journal of Antimicrobial Agents. 2001;18(4):353–358. doi: 10.1016/s0924-8579(01)00422-8. [DOI] [PubMed] [Google Scholar]
- 20.Umolu PI., Omigie O., Tatfeng Y., Omorogbe FI., Aisabokhale F., Ugbodagah OP. Antimicrobial susceptibility and plasmid profiles of Escherichia coli isolates obtained from different human clinical specimens in Lagos-Nigeria. The Journal of American Science. 2006;2(4):1931–1956. [Google Scholar]
- 21.Health Protection Agency. Laboratory Detection and Reporting of Bacteria with Extended Spectrum β-Lactamases. National Standard Method QSOP 51. Issue 2.2. London, UK: Health Protection Agency; 2008. [Google Scholar]
- 22.Garrec H., Drieux-Rouzet L., Golmard J.-L., Jarlier V., Robert J. Comparison of nine phenotypic methods for detection of extended-spectrum β-lactamase production by Enterobacteriaceae . Journal of Clinical Microbiology. 2011;49(3):1048–1057. doi: 10.1128/jcm.02130-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vercauteren E., Descheemaeker P., Ieven M., Sanders C. C., Goossens H. Comparison of screening methods for detection of extended-spectrum β- lactamases and their prevalence among blood isolates of Escherichia coli and Klebsiella spp. in a Belgian teaching hospital. Journal of Clinical Microbiology. 1997;35(9):2191–2197. doi: 10.1128/jcm.35.9.2191-2197.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bedenic B., Randegger C., Boras A., Haechler H. Comparison of five different methods for detection of SHV extended-spectrum β-lactamases. Journal of Chemotherapy. 2001;13(1):24–33. doi: 10.1179/joc.2001.13.1.24. [DOI] [PubMed] [Google Scholar]
- 25.Jain A., Mondal R. Detection of extended spetrum beta-lactamase production in clinical isolates of Klebsiella spp . Indian Journal of Medical Research. 2008;127(4):344–346. [PubMed] [Google Scholar]
- 26.Steward C. D., Rasheed J. K., Hubert S. K., et al. Characterization of clinical isolates of Klebsiella pneumoniae from 19 laboratories using the National Committee for Clinical Laboratory Standards extended-spectrum beta-lactamase detection methods. Journal of Clinical Microbiology. 2001;39(8):2864–2872. doi: 10.1128/jcm.39.8.2864-2872.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang T.-D., Bogaerts P., Berhin C., Guisset A., Glupczynski Y. Evaluation of brilliance ESBL agar, a novel chromogenic medium for detection of extended-spectrum-beta- lactamase-producing Enterobacteriaceae . Journal of Clinical Microbiology. 2010;48(6):2091–2096. doi: 10.1128/jcm.02342-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carattoli A., Bertini A., Villa L., Falbo V., Hopkins K. L., Threlfall E. J. Identification of plasmids by PCR-based replicon typing. Journal of Microbiological Methods. 2005;63(3):219–228. doi: 10.1016/j.mimet.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 29.Kasap M., Fashae K., Torol S., Kolayli F., Budak F., Vahaboglu H. Characterization of ESBL (SHV-12) producing clinical isolate of Enterobacter aerogenes from a tertiary care hospital in Nigeria. Annals of Clinical Microbiology and Antimicrobials. 2010;9, article 1 doi: 10.1186/1476-0711-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Olowe O. A., Grobbel M., Büchter B., Lübke-Becker A., Fruth A., Wieler L. H. Detection of bla CTX-M-15 extended-spectrum β-lactamase genes in Escherichia coli from hospital patients in Nigeria. International Journal of Antimicrobial Agents. 2010;35(2):206–207. doi: 10.1016/j.ijantimicag.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 31.Aibinu I., Odugbemi T., Koenig W., Ghebremedhin B. Sequence Type ST131 and ST10 Complex (ST617) predominant among CTX-M-15-producing Escherichia coli isolates from Nigeria. Clinical Microbiology and Infection. 2012;18(3):E49–E51. doi: 10.1111/j.1469-0691.2011.03730.x. [DOI] [PubMed] [Google Scholar]
- 32.Iroha I. R., Esimone C. O., Neumann S., et al. First description of Escherichia coli producing CTX-M-15- extended spectrum beta lactamase (ESBL) in out-patients from south eastern Nigeria. Annals of Clinical Microbiology and Antimicrobials. 2012;11, article 19 doi: 10.1186/1476-0711-11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]


