Abstract
Purpose:
To assess the efficacy of chlorhexidine monotherapy for Acanthamoeba keratitis, and to determine the therapeutic outcomes of concomitant topical corticosteroids.
Methods:
In this prospective interventional case series, 31 eyes of 31 patients with Acanthamoeba keratitis (AK) were treated with chlorhexidine 0.02% as monotherapy, from April 2010 to April 2011. The diagnosis of AK was made based on clinical manifestations and positive confocal microscopic (confoscan 3.4, Nidek Co. Ltd., Gamagori, Japan) results. We report the percentage of a favorable clinical response within two weeks of initiating treatment, worsening of the infection while receiving chlorhexidine, recovery of visual acuity (VA), duration of treatment with chlorhexidine and corticosteroids, necessity for addition of other anti-Acanthamoeba agents, presence of corneal scar at the end of the treatment, and need for penetrating keratoplasty (PK).
Results:
Two weeks after initiation of chlorhexidine, improvement in signs and symptoms was observed in 26 (83.9%) patients but 3 eyes required the addition of propamidine. After initial improvement in one patient, the infection worsened, necessitating the addition of Polyhexamethylene Biguanide (PHMB) and propamidine. A total of 26 (83.9%) patients received topical corticosteroids with mean duration of 65.8 ± 45.1 days. In 22 (71%) eyes, final visual acuity was ≥0.80. Improved VA occurred in 29 eyes (93.5%). Optical PK was considered in 3 (9.7%) eyes and a corneal scar developed in 8 (25.8%) eyes.
Conclusion:
Chlorhexidine is effective for monotherapy in AK and could be a good choice for initiating treatment. After the initial response to anti-Acanthamoeba agents, corticosteroids can be used as adjunctive therapy depending on the clinical condition.
Keywords: Acanthamoeba Keratitis, Chlorhexidine, Topical Corticosteroids
INTRODUCTION
Acanthamoeba keratitis (AK) is a sight-threatening corneal disease caused by free-living amoebae. The majority of patients with AK are contact lens wearers[1] with a predominance of soft contact lens use.[2] AK is considered as a widespread infection. Although it was first described in 1973,[3] many aspects of the infection including its risk factors, diagnosis, outcomes of treatment, and prognosis remain uncertain. Most of the published literature suggests that combination therapy seems to be effective for treatment of AK.[4,5] However, combination therapy may be associated with increased cost, poor compliance and more side effects such as epithelial toxicity.[6,7]
There are few well-designed studies,[8,9] which have investigated the efficacy of chlorhexidine as monotherapy for treatment of AK. Furthermore, the role of corticosteroids for treatment of AK remains controversial. The current study was designed to assess the efficacy of chlorhexidine as monotherapy and clarify the role of corticosteroids for treatment of AK. We also identified other factors that may affect visual outcomes in patients with AK who received treatment with chlorhexidine.
METHODS
Patients
This prospective interventional case series study was performed at Farabi Eye Hospital, Tehran, Iran in accordance with the Declaration of Helsinki and its 1983 revision. Institutional review board approval was obtained and each subject provided informed consent. All cases who presented with AK from April 2010 to April 2011 were enrolled in the study. A detailed questionnaire on demographic characteristics and past medical history including age, gender and previous treatments was completed. Initial best corrected visual acuity (BCVA) was measured by an optometrist. All patients underwent slit lamp examination and were categorized in the following three clinical stages based on the depth of corneal involvement: Stage I: Epitheliopathy; Stage 2, anterior stromal infiltration; stage 3, ring infiltration or deep stromal infiltration.
Confocal microscopy (confoscan 3.4, Nidek Co. Ltd., Gamagori, Japan) was employed for confirming the diagnosis of AK. Only patients who had specific clinical findings suggestive of AK (perineural infiltrates, ring infiltrates and keratitis with disproportionate pain) and simultaneous positive confocal microscopy results for AK were enrolled in the study. Patients with poor compliance during the treatment period were excluded from the study.
Treatment Protocol
After establishing the clinical diagnosis of AK, treatment was initiated with chlorhexidine 0.02% (Sina Darou Company, Tehran, Iran). Chlorhexidine 0.02% was instilled in the affected eye, at a frequency of hourly at day and night, reduced to hourly in the day for the next three days, then reduced to 2 hours in the daytime. According to the clinical response, the regimen was gradually reduced. When failure occurred or infection worsened while receiving chlorhexidine, we added other anti-Acanthamoeba agents in order to induce a favorable clinical response. We used topical corticosteroids for limbitis, uveitis, ocular pain unresponsive to oral analgesics and stromal infiltration following an initial response to anti-Acanthamoeba medication. We started topical corticosteroids at least 2 weeks after treatment with chlorhexidine. Treatment was terminated when all primary ocular complaints, except visual loss, disappeared and there was no sign of active disease on ocular examination and after cessation of any topical steroid therapy.
Outcomes
Outcome measures included a favorable clinical response within two weeks of initiating treatment with chlorhexidine, worsening of the infection while receiving chlorhexidine, recovery of visual acuity (VA), duration of treatment with chlorhexidine and corticosteroids, necessity of adding other anti-Acanthamoeba agents, presence of a corneal scar at the end of the treatment, and the need for penetrating keratoplasty.
Statistical Analysis
Results were reported as mean ± standard deviations (SDs) for quantitative variables and percentage values for categorical variables. Visual acuity was reported in decimal notations. Odds ratios (ORs) and their 95% confidence interval (CIs) derived from logistic regression models were used to evaluate the relation between final VA <20/25 and a set of examined predictors. P values of 0.05 or less were considered as statistically significant. All statistical analyses were performed using SPSS version 13 (SPSS Inc., Chicago, IL, USA) for Microsoft Windows 7.
RESULTS
We enrolled 32 eyes of 32 patients over the period of the study. One patient did not keep her follow-up visits and was thus excluded from the analysis. A total of 31 patients with mean age of 21.5 ± 4.6 (range, 15 to 36) years including a majority of female subjects 27 (87.1%) were treated. Twenty-eight subjects (90.3%) had history of cosmetic contact lens use, 2 wore contact lenses for correction of refractive errors and one had history of ocular trauma with plant material. A total of 14 patients cleaned the lenses or contact lens storage cases with tap water. Before the diagnosis, 12 patients used corticosteroids and the duration of use ranged from 2 to 30 days.
In 20 (64.5%) patients, ocular pain was the main sign at presentation. Stage 1 corneal involvement was present in 13 eyes (41.9%) while 15 (48.4%) and 3 (9.70%) eyes had stage 2 and 3 disease, respectively. After the onset of symptoms, 17 patients (54.8%) were diagnosed within 3 weeks. Mean presenting visual acuity was 0.32 ± 0.22 (range: 0.001-0.80), and was less than 0.50 in 22 patients (71%) [Table 1]. Mean visual acuity at final follow-up was 0.79 (range, 0.001-1.00) and final visual acuity was ≥0.80 in 22 eyes [Table 2].
Table 1.
Demographic characteristics and clinical data (31 patients)
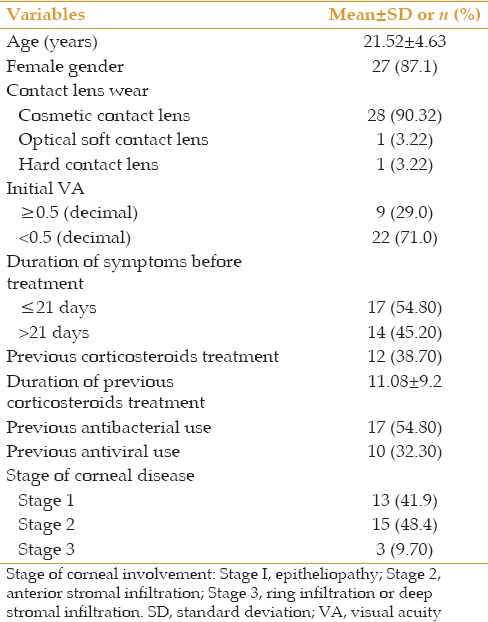
Table 2.
Primary and secondary outcomes
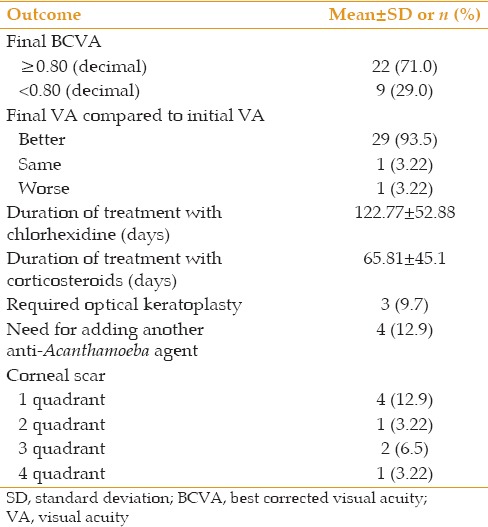
Mean duration of treatment was 122.8 ± 52.9 days. Two weeks after initiation of treatment with chlorhexidine, improvement in signs and symptoms was observed in only 5 patients (16.6%). Keratitis was controlled in 3 eyes by adding propamidine to chlorhexidine and in 2 other eyes without adding any other anti-Acanthamoeba medication. After initial improvement in one patient, worsening of the keratitis occurred. A smear was taken and cultured on a corneal specimen; it was positive for Acanthamoeba but negative for other microorganisms. We added Polyhexamethylene Biguanide (PHMB) and propamidine to this patient’s regimen. This patient developed scleritis that was treated with oral prednisolone. Scleritis was controlled and keratitis healed leaving total corneal scarring. A total of 26 (83.9%) patients received topical corticosteroids with mean duration of 65.81 ± 45.1 days.
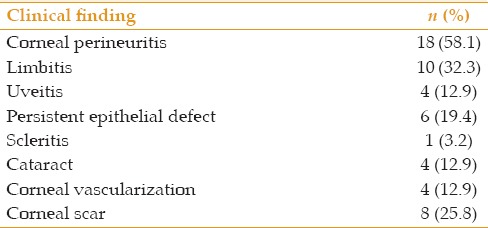
Persistent epithelial defects occurred in 6 (19.4%) patients, and 2 of these patients were treated with amniotic membrane transplantation. Punctate epithelial defects occurred in 9 (29%) eyes; visually significant cataracts developed in 4 (12.9%) eyes; optical penetrating keratoplasty was considered in 3 (9.7%) eyes; hypopyon developed in 3 (9.7%) eyes; and a corneal scar was formed in 8 (25.8%) eyes [Table 3].
Table 3.
Clinical finding initially and during follow-up
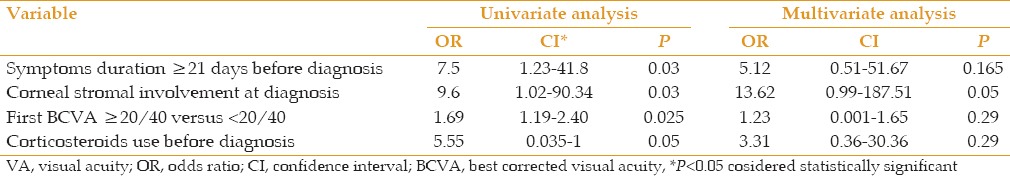
Based on univariate analysis, significant prognostic factors for visual acuity <20/25 included the following: Duration of symptoms 21 days or longer before the diagnosis, stromal involvement at presentation and initial visual acuity <20/40; however steroid use before the diagnosis was not a significant predictor. In multivariate analysis, longer duration of symptoms before the diagnosis and stromal involvement at presentation were associated with worse final visual acuity but were not statistically significant [Table 4].
Table 4.
Association between clinical manifestations and final VA <20/25
DISCUSSION
Acanthamoeba keratitis is a sight-threatening corneal disease and many aspects of its treatment remain controversial. Oldenburg et al performed a survey on opinions and practice patterns for treatment of AK; in their study, 93.9% of respondents preferred combination therapy over monotherapy for treatment of AK. Of the 82 respondents, 90.2% used combination therapy most of the time or always, while only 6.1% used monotherapy.[6] Combination therapy increases cost, and usually results in poor compliance and more side effects such as epithelial toxicity.[6,7] This preference for combination therapy may have resulted from the case series that described combination treatment for AK.[10,11]
On the other hand, there are case reports and series that suggested monotherapy with chlorhexidine,[9,12] or PHMB[13,14] may be successful in AK. However, well-designed studies have investigating the efficacy of monotherapy for treatment of AK are limited. This may cause a tendency for some clinicians to use combination therapy rather than monotherapy. There are reports suggesting that the in vitro anti-Acanthamoeba activity of chlorhexidine is similar or higher than PHMB.[15,16] Moreover, PHMB seems to be more toxic to keratocytes than chlorhexidine.[16] Wysenbeek and associates, assessed the efficacy of three agents in different concentrations against different strains of Acanthamoeba (0.1% and 0.02% polyhexamethylenebiguanide, 0.1% and 0.02% chlorhexidine, and propamidine isethionate). Only chlorhexidine at concentrations of 0.02% and 0.1% was effective against all five strains of Acanthamoeba and only 0.1% chlorhexidine destroyed all cysts. However, because higher concentrations of chlorhexidine are toxic to the cornea, they recommended that 0.02% chlorhexidine is a good initial choice for treatment of AK.[17] When Oldenburg et al asked respondents to choose an ideal medication as monotherapy for AK, they first choice was PHMB, followed by chlorhexidine.[6] A well-designed study is needed to demonstrated that changing from combination therapy to monotherapy with chlorhexidine in vitro is more effective than PHMB.
We used chlorhexidine monotherapy for treatment of our patients in a prospective manner. Chlorhexidine is an effective anti-Acanthamoeba agent.[9,18,19] In a prospective, nonrandomized study, Kosrirukvongs and associates reported that chlorhexidine was an effective amoebicidal agent in 5 patients with AK.[9] In a randomized controlled trial by Lim et al[8] treatment was successful in 85.7% of patients who received chlorhexidine compared with 78.3% successful treatment in patients who received PHMB. They defined treatment failure as failure to achieve a favorable clinical response within two weeks of initiating treatment with PHMB or chlorhexidine alone, or patients whose infection worsened while receiving monotherapy. In our study, a favorable clinical response was not achieved in 5 patients (16.1%) after two weeks of treatment with chlorhexidine, and keratitis worsened in one patient (3.2%). This is comparable to the results reported by Lim et al[8] Interval form onset of symptoms to diagnosis and anti-Acanthamoeba treatment and risk factors for AK were similar in two studies, but median duration of treatment in our study (122.78 days) was longer than that by Lim et al[8] (92 days). Vision was also improved in 93.5% of eyes in our study versus 71.4% in the mentioned report. The incidence of corneal scarring was significantly lower in our patients. Similar to the current series, BCVA of 6/12 or better was achieved in 78% of eyes in both groups of Lim’s study, albeit mean VA at initial visit in their patients was 0.3 (LogMAR). These authors did not report the stage of keratitis at initial visit and how they used corticosteroids, but our patients had worse VA at initial visit and higher stages of corneal involvement at presentation. It seems that both of these factors mandated a longer duration of treatment in our patients, however the greater use of corticosteroids led to better visual outcomes as compared to the study by Lim et al[8]
When chlorhexidine was used as monotherapy in our study, it revealed a good therapeutic efficacy against Acanthamoeba; BCVA of 0.50 or better was achieved in 25 of 31 eyes (81%). This success rate is comparable to that achieved by three other major studies that used combination therapy, and reported the same level of BCVA in 75%[20] and 79%[7,10] of their patients. They often used PHMB and propamidine. Seal et al used chlorhexidine and propamidine for treatment of AK; with one exception, 11 patients recovered 6/9 vision. In this study, one patient who presented with ring infiltration underwent keratoplasty as a result of secondary bacterial infection, with graft survival and visual acuity of 6/6 after 2 years. Of 11 patients, only 2 patients had stromal infiltration, which is not comparable with 18 patients in our study that presented with stromal involvement with or without ring infiltration.[19] In the current series, only 4 (12.9%) patients required another anti-Acanthamoeba agent; furthermore, monotherapy with chlorhexidine without adding other drugs could treat most cases of AK.
One in vitro study suggested that corticosteroids inhibit encystment of Acanthamoeba trophozoites, making them more susceptible to anti-Acanthamoeba agents.[21,22] The role of corticosteroids in treatment of AK remains controversial. Some reports have shown that corticosteroids increase the rate of treatment failure in AK, while others have demonstrated good outcomes with topical corticosteroids use.[22,23,24] Park et al reported that mean treatment duration was longer in the group using corticosteroids as compared to the group not treated with steroids; however, visual outcomes were not significantly different between the two groups.[24] As discussed earlier in our study, it seems that greater use of corticosteroids necessitates a longer duration of treatment but entails a better visual outcome. Univariate analysis revealed that treatment with corticosteroids was not a significant factor for worse visual outcomes (OR = 1.29, CI = 1.03-1.62, P = 0.155 for visual acuity <20/25).
In a study by Kelley et al six eyes out of 20 (30%) with AK developed secondary glaucoma and the authors stated that development of secondary elevated intraocular pressure is not uncommon in AK and a predictor for poor prognosis. Histopathologic findings suggest an apparent inflammatory angle-closure mechanism for glaucoma, without direct infiltration of the organism.[25] In our study, no patient developed elevated intraocular pressure, which might be due to better control of inflammation with the use of corticosteroids.
Corneal confocal microscopy in patients with both clinical features of Acanthamoeba keratitis has shown high sensitivity and specificity.[26,27,28] Clarke et al considered that confocal microscopy is a very useful adjunct to clinical examination and suggested it could be used as a first-line test for diagnosis of AK.[29]
In our study, 28 patients had a history of wearing cosmetic contact lens including 2 patients using contact lenses for refractive error correction. Fourteen patients cleaned their lenses or contact lens storage cases with tap water. Tap water may contain Acanthamoeba and serve as a source of contamination for contact lenses or cases.[30] Often, cosmetic contact lenses are freely available without professional education. Education of contact lens wearers about disinfection and risks associated with tap water can reduce the incidence of AK.[31]
Chew et al, in univariate analysis, reported that stromal involvement and initial visual acuity <20/50 were significantly correlated with the need for penetrating keratoplasty and final visual acuity <20/25; in multivariate analysis, only initial VA <20/50 had a significant association.[32] In our study, longer duration of disease before the diagnosis, initial VA <20/40 and stromal involvement were significantly correlated with final VA <20/25 in univariate analysis, but none of these factors retained a significant correlation in multivariate analysis.
In conclusion, chlorhexidine seems to be an effective agent for monotherapy in AK and could be a good choice for initial treatment. After an initial response to anti-Acanthamoeba agents, corticosteroids can be used as adjunctive therapy depending on clinical condition. Regarding the different levels of presenting VA and variable stage of corneal involvement in different studies on AK, randomized clinical trials comparing combination therapy with monotherapy will be necessary to firmly establish treatment efficacy and visual outcomes in this grave corneal infection.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Seal DV. Acanthamoeba keratitis update-incidence, molecular epidemiology and new drugs for treatment. Eye (Lond) 2003;17:893–905. doi: 10.1038/sj.eye.6700563. [DOI] [PubMed] [Google Scholar]
- 2.Stehr-Green JK, Bailey TM, Brandt FH, Carr JH, Bond WW, Visvesvara GS. Acanthamoeba keratitis in soft contact lens wearers. A case-control study. JAMA. 1987;258:57–60. [PubMed] [Google Scholar]
- 3.Naginton J, Watson PG, Playfair TJ, McGill J, Jones BR, Steele AD. Amoebic infection of the eye. Lancet. 1974;2:1537–1540. doi: 10.1016/s0140-6736(74)90285-2. [DOI] [PubMed] [Google Scholar]
- 4.Lam DS, Lyon D, Poon AS, Rao SK, Fan DS. Polyhexamethylene biguanide (0.02%) alone is not adequate for treating chronic Acanthameoba keratitis. Eye (Lond) 2000;14(Pt 4):678–679. doi: 10.1038/eye.2000.174. [DOI] [PubMed] [Google Scholar]
- 5.Kitagawa K, Nakamura T, Takahashi N, Oikawa Y, Ikeda T. A novel combination treatment of chlorhexidine gluconate, natamycin (pimaricin) and debridement for a Acanthamoeba keratitis. Jpn J Ophthalmol. 2003;47:616–617. doi: 10.1016/j.jjo.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 6.Oldenburg CE, Acharya NR, Tu EY, Zegans ME, Mannis MJ, Gaynor BD, et al. Practice patterns and opinions in the treatment of Acanthamoeba keratitis. Cornea. 2011;30:1363–1368. doi: 10.1097/ICO.0b013e31820f7763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bacon AS, Frazer DG, Dart JK, Matheson M, Ficker LA, Wright P. A review of 72 consecutive cases of Acanthamoeba keratitis, 1984-1992. Eye (Lond) 1993;7(Pt 6):719–725. doi: 10.1038/eye.1993.168. [DOI] [PubMed] [Google Scholar]
- 8.Lim N, Goh D, Bunce C, Xing W, Fraenkel G, Poole TR, et al. Comparison of polyhexamethylene biguanide and chlorhexidine as monotherapy agents in the treatment of Acanthamoeba keratitis. Am J Ophthalmol. 2008;145:130–135. doi: 10.1016/j.ajo.2007.08.040. [DOI] [PubMed] [Google Scholar]
- 9.Kosrirukvongs P, Wanachiwanawin D, Visvesvara GS. Treatment of Acanthamoeba keratitis with chlorhexidine. Ophthalmology. 1999;106:798–802. doi: 10.1016/S0161-6420(99)90169-0. [DOI] [PubMed] [Google Scholar]
- 10.Butler TK, Males JJ, Robinson LP, Wechsler AW, Sutton GL, Cheng J, et al. Six-year review of Acanthamoeba keratitis in New South Wales, Australia: 1997-2002. Clin Experiment Ophthalmol. 2005;33:41–46. doi: 10.1111/j.1442-9071.2004.00911.x. [DOI] [PubMed] [Google Scholar]
- 11.Sun X, Zhang Y, Li R, Wang Z, Luo S, Gao M, et al. Acanthamoeba keratitis: Clinical characteristics and management. Ophthalmology. 2006;113:412–416. doi: 10.1016/j.ophtha.2005.10.041. [DOI] [PubMed] [Google Scholar]
- 12.Mathers W. Use of higher medication concentrations in the treatment of Acanthamoeba keratitis. Arch Ophthalmol. 2006;124:923. doi: 10.1001/archopht.124.6.923. [DOI] [PubMed] [Google Scholar]
- 13.Sharma S, Garg P, Rao GN. Patient characteristics, diagnosis, and treatment of non-contact lens related Acanthamoeba keratitis. Br J Ophthalmol. 2000;84:1103–1108. doi: 10.1136/bjo.84.10.1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gray TB, Gross KA, Cursons RT, Shewan JF. Acanthamoeba keratitis: A sobering case and a promising new treatment. Aust N Z J Ophthalmol. 1994;22:73–76. doi: 10.1111/j.1442-9071.1994.tb01700.x. [DOI] [PubMed] [Google Scholar]
- 15.Narasimhan S, Madhavan HN, Therese KL. Development and application of an in vitro susceptibility test for Acanthamoeba species isolated from keratitis to polyhexamethylene biguanide and chlorhexidine. Cornea. 2002;21:203–205. doi: 10.1097/00003226-200203000-00016. [DOI] [PubMed] [Google Scholar]
- 16.Lee JE, Oum BS, Choi HY, Yu HS, Lee JS. Cysticidal effect on Acanthamoeba and toxicity on human keratocytes by polyhexamethylene biguanide and chlorhexidine. Cornea. 2007;26:736–741. doi: 10.1097/ICO.0b013e31805b7e8e. [DOI] [PubMed] [Google Scholar]
- 17.Wysenbeek YS, Blank-Porat D, Harizman N, Wygnanski-Jaffe T, Keller N, Avni I. The reculture technique: Individualizing the treatment of Acanthamoeba keratitis. Cornea. 2000;19:464–467. doi: 10.1097/00003226-200007000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Tirado-Angel J, Gabriel MM, Wilson LA, Ahearn DG. Effects of polyhexamethylene biguanide and chlorhexidine on four species of Acanthamoeba in vitro. Curr Eye Res. 1996;15:225–228. doi: 10.3109/02713689608997418. [DOI] [PubMed] [Google Scholar]
- 19.Seal D, Hay J, Kirkness C, Morrell A, Booth A, Tullo A, et al. Successful medical therapy of Acanthamoeba keratitis with topical chlorhexidine and propamidine. Eye (Lond) 1996;10(Pt 4):413–421. doi: 10.1038/eye.1996.92. [DOI] [PubMed] [Google Scholar]
- 20.Duguid IG, Dart JK, Morlet N, Allan BD, Matheson M, Ficker L, et al. Outcome of Acanthamoeba keratitis treated with polyhexamethyl biguanide and propamidine. Ophthalmology. 1997;104:1587–1592. doi: 10.1016/s0161-6420(97)30092-x. [DOI] [PubMed] [Google Scholar]
- 21.Osato M, Robinson N, Wilhelmus K, Jones D. Morphogenesis of Acanthamoeba castellanii: Titration of the steroid effect. Invest Ophthalmol Vis Sci. 1986;27:37. [Google Scholar]
- 22.O’Day DM, Head WS. Advances in the management of keratomycosis and Acanthamoeba keratitis. Cornea. 2000;19:681–687. doi: 10.1097/00003226-200009000-00013. [DOI] [PubMed] [Google Scholar]
- 23.Dart JK, Saw VP, Kilvington S. Acanthamoeba keratitis: Diagnosis and treatment update 2009. Am J Ophthalmol. 2009;148:487–499.e2. doi: 10.1016/j.ajo.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 24.Park DH, Palay DA, Daya SM, Stulting RD, Krachmer JH, Holland EJ. The role of topical corticosteroids in the management of Acanthamoeba keratitis. Cornea. 1997;16:277–283. [PubMed] [Google Scholar]
- 25.Kelley PS, Dossey AP, Patel D, Whitson JT, Hogan RN, Cavanagh HD. Secondary glaucoma associated with advanced Acanthamoeba keratitis. Eye Contact Lens. 2006;32:178–182. doi: 10.1097/01.icl.0000189039.68782.fe. [DOI] [PubMed] [Google Scholar]
- 26.Tu EY, Joslin CE, Sugar J, Booton GC, Shoff ME, Fuerst PA. The relative value of confocal microscopy and superficial corneal scrapings in the diagnosis of Acanthamoeba keratitis. Cornea. 2008;27:764–772. doi: 10.1097/ICO.0b013e31816f27bf. [DOI] [PubMed] [Google Scholar]
- 27.Pfister DR, Cameron JD, Krachmer JH, Holland EJ. Confocal microscopy findings of Acanthamoeba keratitis. Am J Ophthalmol. 1996;121:119–128. doi: 10.1016/s0002-9394(14)70576-8. [DOI] [PubMed] [Google Scholar]
- 28.Kanavi MR, Javadi M, Yazdani S, Mirdehghanm S. Sensitivity and specificity of confocal scan in the diagnosis of infectious keratitis. Cornea. 2007;26:782–786. doi: 10.1097/ICO.0b013e318064582d. [DOI] [PubMed] [Google Scholar]
- 29.Clarke B, Sinha A, Parmar DN, Sykakis E. Advances in the diagnosis and treatment of Acanthamoeba keratitis. J Ophthalmol. 2012;2012:1110–1115. doi: 10.1155/2012/484892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jeong HJ, Lee SJ, Kim JH, Xuan YH, Lee KH, Park SK, et al. Acanthamoeba: Keratopathogenicity of isolates from domestic tap water in Korea. Exp Parasitol. 2007;117:357–367. doi: 10.1016/j.exppara.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 31.Radford CF, Minassian DC, Dart JK. Acanthamoeba keratitis in England and Wales: Incidence, outcome, and risk factors. Br J Ophthalmol. 2002;86:536–542. doi: 10.1136/bjo.86.5.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chew HF, Yildiz EH, Hammersmith KM, Eagle RC, Jr, Rapuano CJ, Laibson PR, et al. Clinical outcomes and prognostic factors associated with Acanthamoeba keratitis. Cornea. 2011;30:435–441. doi: 10.1097/ICO.0b013e3181ec905f. [DOI] [PubMed] [Google Scholar]


