Abstract
Purpose:
To evaluate foveal microstructural changes and to determine its association with visual outcomes after reattachment of rhegmatogenous retinal detachments (RRDs) by scleral buckling (SB) or pars plana vitrectomy (PPV).
Methods:
Using spectral domain optical coherence tomography (SD-OCT), foveal microstructure in eyes with macula-off RRD were studied 1, 3, 6, 9, 12 and 15 months after PPV or SB and correlated with visual outcomes.
Results:
Forty-two eyes were included in the final analysis. Even with improved microstructural changes and normalization of retinal structures on OCT, final visual acuity was not correlated with microstructural changes in eyes undergoing PPV. In the SB group, final visual acuity was significantly correlated with an intact inner segment/outer segment (IS/OS) junction (P = 0.013). There was no significant correlation between final visual acuity and presence of subretinal fluid (SRF) in either group.
Conclusion:
After SB, eyes with an intact IS/OS junction had better final visual acuity. In the PPV group, there was no significant correlation between microstructural changes and visual acuity. The presence of SRF did not influence final visual acuity in both groups.
Keywords: Pars Plana Vitrectomy, Rhegmatogenous Retinal Detachment, Scleral Buckling, Spectral Domain Optical Coherence Tomography, Subretinal Fluid
INTRODUCTION
Anatomical distortion of the retina by rhegmatogenous retinal detachment (RRD) leads to visual impairment. Despite excellent surgical results with current modalities of treatment, visual recovery may still be disappointing in patients with macula-off rhegmatogenous retinal detachment (RRD). Nevertheless, incomplete visual recovery can often occur in clinically normal-looking retinas due to subtle changes in foveal microstructure. Reduced postoperative visual acuity has been reported to be related to preoperative visual acuity, duration of detachment, cystoid macular edema, epiretinal membrane, retinal folds and retinal pigment epithelium migration.[1,2,3,4,5]
The advent of optical coherence tomography (OCT) enables the detection of ultrastructural changes, which may not be clinically evident. High resolution spectral domain OCT (SD-OCT), enables the evaluation of macular microstructural changes comparable to histologic details in vivo. It gives important insights about morphological and structural changes occurring at the level of the external limiting membrane and photoreceptor inner segment/outer segment (IS/OS) junction which may relate to the integrity of the photoreceptor layer.[6,7,8,9,10] It has been shown that there are some associations between various postoperative morphological changes such as the disruption of the IS/OS junction and poor visual outcome, after successful RRD repair.[6,7,9] Using SD-OCT, Smith and associates reported a correlation between microperimetric abnormalities and the presence of photoreceptor disruption or subretinal fluid (SRF) after macula-off retinal detachment surgery.[11]
Some prospective studies using SD-OCT have evaluated foveal structure after RRD repair, in eyes successfully treated for macula-off RRD after pars plana vitrectomy (PPV) or scleral buckling (SB). In the present study, microstructural changes of the fovea using SD-OCT and postoperative visual acuity were evaluated in the course of follow up for RRD repair using PPV or SB.
METHODS
Between January 2010 and September 2010, all consecutive patients fulfilling the criteria of having a macula-off primary RRD, no pre-existing ocular disease affecting central vision and no history of retinal surgery, were enrolled in this observational case series. Redetachment cases were excluded from the study. This study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board and Ethics Committee of Tehran University of Medical Sciences. Informed consent was obtained from all patients.
All patients underwent a comprehensive ophthalmological examination, including determination of best corrected visual acuity (BCVA) using the ETDRS chart converted into LogMAR scale, dilated indirect and non-contact biomicroscopy, and OCT to confirm macular detachment.
The patients underwent standard 20 gauge PPV with or without encircling band or SB surgery alone, based on the physicians’ discretion. BCVA measurement and OCT examination were repeated 1, 3, 6, 9, 12 and 15 months, post-operatively. All OCT examinations were performed after pupillary dilation using the Cirrus SD-OCT (Carl Zeiss Meditec, Inc., Dublin, CA, USA) with the protocol of the HDIA; 5 Line Raster and Macular Cube 512 × 128.
Five series of OCT images were read by two experienced vitreoretinal surgeons and accepted only when they were in agreement; otherwise a third vitreoretinal surgeon reviewed controversial cases. All OCT readers were masked to all characteristics of the patients. The thickness of the outer nuclear layer (ONL) was evaluated as “decreased,” “increased,” “normal” and “not evaluable” compared with the ONL of the normal fellow eye. The integrity of the IS/OS junction and external limiting membrane (ELM) were classified as “disrupted,” “fused,” “intact” and “not evaluable.” They were assumed to be “intact” when at least 50% of their length in the central 1500 micron zone around the fovea was continuous and clearly visible, otherwise they were assumed to be “disrupted.” They were named “fused” when a thick hyper-reflective band prevented accurate discrimination of the IS/OS junction from the ELM. “not evaluable” was adopted when detection of the IS/OS junction and ELM status was not possible. Three patterns of SRF in OCT were classified as: “Single localized,” “multiple localized,” “low-lying extensive.” The main outcome measures was normalization of all OCT changes retinal layers after the operation and resorption of subretinal fluid.
Statistical analysis was performed using SPSS 12 software (SPSS Inc., Chicago, Illinois, USA). The level of statistical significance was set at P < 0.05. T-test was used to determine the effect of the IS/OS junction, ELM integrity and ONL thickness on BCVA, and to evaluate the effect of SRF on BCVA. Continuous data are presented as means ± standard deviations. Pearson Chi-square test was used to evaluate the association between categorical variables. The spearman correlation coefficient was used to evaluate the correlation between symptom duration, preoperative BCVA and BCVA at the first post-operative visit, with final BCVA. Due to the relatively smaller sample size of the PPV group compared to the SB group, the results of the two groups were not compared with each other.
RESULTS
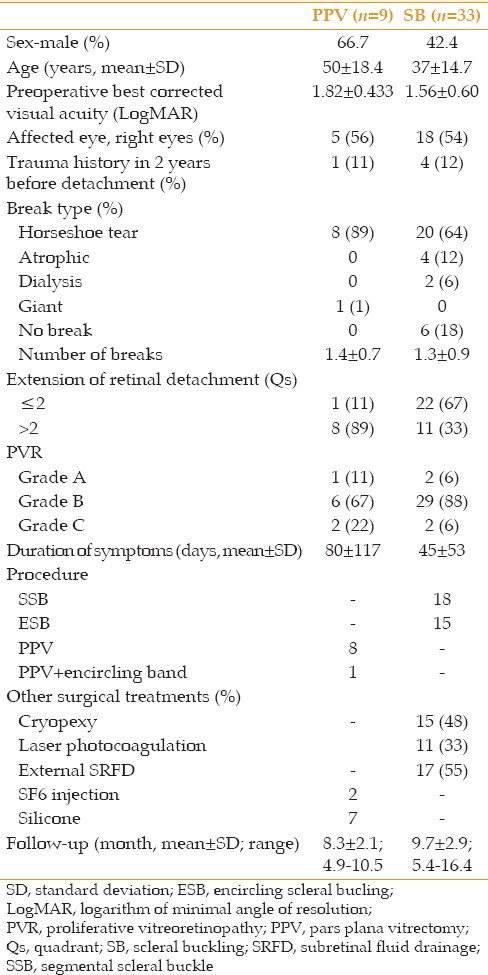
Of the 93 patients who were initially enrolled for the study, 51 patients were excluded because of redetachment (15 cases) or incomplete follow-up (36 cases). Finally, 42 eyes were included in the final analysis (9 eyes in the PPV group and 33 eyes in the SB group). No bilateral cases were included. Demographic and clinical characteristics and follow up of patients are shown in Table 1. Outcome measures were evaluated in both groups at 1, 3, 6, 9, 12 and 15 months after surgery. In the PPV group, central foveal thickness (CFT) was 280 ± 60 μm at the first postoperative visit and 250 ± 52 μm at final visit. In the SB group corresponding figures were 275 ± 73 μm and 248 ± 50 μm.
Table 1.
Demographic and clinical characteristics of study participants
Visual Acuity
BCVA of the study groups are shown detailed Table 2. The frequency of patients in each subgroup and their relation with BCVA is shown in Table 3. In the PPV group and SB groups, there was a significant correlation between BCVA at the first postoperative visit and final BCVA (correlation coefficient: 0.73, P = 0.025 and correlation coefficient: 0.73, P < 0.001). The correlation between preoperative VA and final BCVA was not significant in both groups. In SB and PPV groups, a correlation was found between the duration of symptoms and final BCVA (correlation coefficient: 0.45, P = 0.008; and correlation coefficient: 0.40, P = 0.01, respectively).
Table 2.
BCVA in study groups in consecutive visits
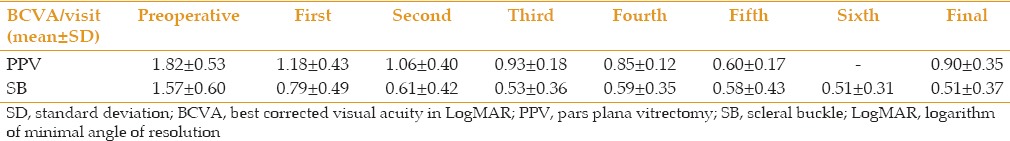
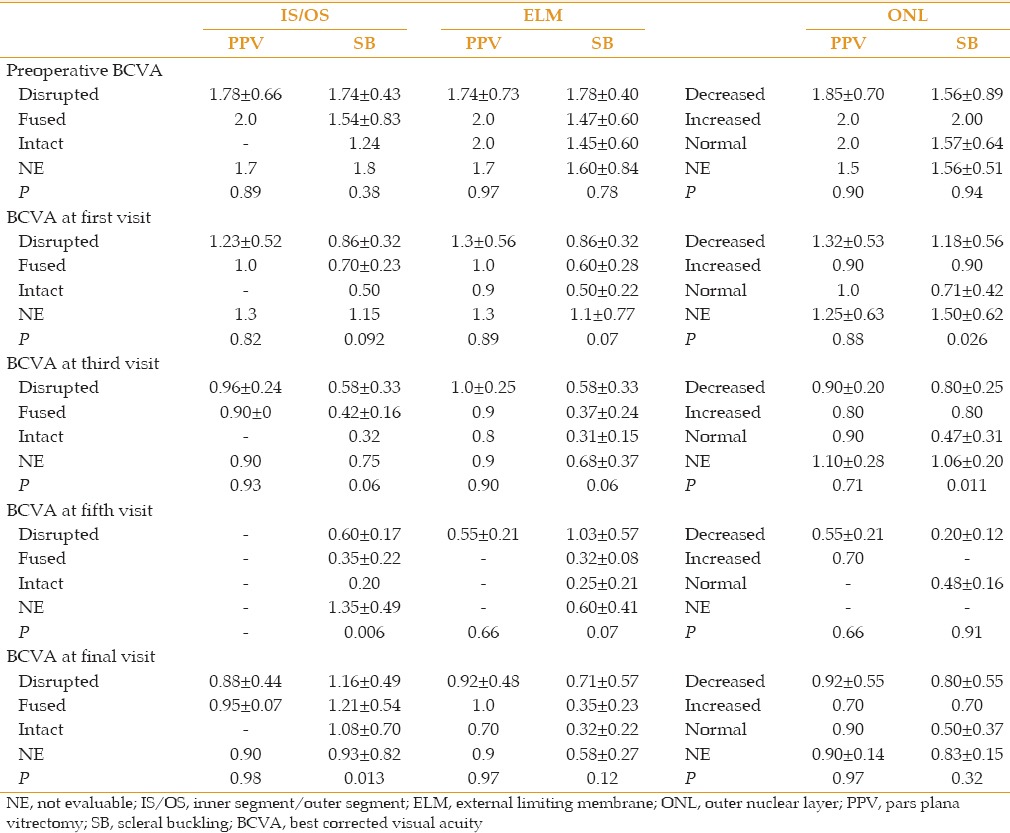
Table 3.
BCVA in subgroups at consecutive visits
In the SB group, out of variables such as age, type of retinal break, duration of symptoms, SRF draiange, only the duration of symptoms (P = 0.01) and cryotherapy (P = 0.046) had a significant effect on final BCVA.
IS/OS Junction Status
In the PPV group, mean preoperative BCVA in different subgroups of IS/OS status was similar (P = 0. 89) and although the mean BCVA of these patients improved at the final visit, there was no correlation between final visual acuity and different subgroups of IS/OS junction [P = 0. 98, Table 3].
In the SB group, the correlation between different IS/OS junction subgroups and mean preoperative BCVA (P = 0.38) and first postoperative examination was not significant (P = 0.3), but at 12 months and the final visit (15 months), the correlation between lower BCVA and disrupted IS/OS junction was significant [P = 0.006 and 0.013, respectively, Table 3].
ELM Status
In PPV group, at the first post-operation visit mean preoperative BCVA was not correlated to the ELM condition (P = 0. 97). Although the mean BCVA of these patients was improved at the final visit, no difference in the subgroups was noted (P = 0.97) [Table 3]. In the SB group, the mean preoperative BCVA of subgroups were not correlated to changes of and IS/OS junction. At 15 month, the correlation between BCVA and disrupted IS/OS was significant (P = 0.039) [Table 3].
BCVA at 15 months was better in eyes with intact ELM (P = 0. 039). There was no patient with disrupted ELM but intact IS/OS junction in both groups. On the other hand, there were two patients in the PPV group and one in the SB group with intact ELM and disrupted IS/OS junction. Of the three patients with combined disrupted IS/OS junction and ELM in the PPV group, in two patients the IS/OS junction was restored at the final visit. Of four patients with combined disrupted IS/OS junction and ELM in the SB group, all eyes were restored at the final visit.
ONL Status
In both study groups, mean preoperative and final BCVA were not significantly different according to ONL thickness [compared with the fellow eye, Table 3].
Subretinal Fluid
Preoperative BCVA was not different in eyes with and without SRF (P = 0.96); similarly final BCVA was also not different (0.36 ± 0.30 vs. 0.61 ± 0.40, P = 0.09). To evaluate the effect of the duration of SRF persistence on final visual acuity, patients with SRF in the first postoperative visit were divided into two groups, those with SRF resolution before 6 months (4 cases) and those with SRF resolution afterwards (11 cases). Mean preoperative BCVA in the first group was not different from the second group (1.67 ± 0.47 vs. 1.44 ± 0.56, P = 0.48). Final visual acuity was also not different between these two groups (0.20 ± 0.11 vs. 0.46 ± 0.32, P = 0.14).
Complications
In the PPV group, an epiretinal membrane (ERM) was formed in 3 (13%) patients at a mean time of 5 ± 0.5 (range: 4.5-5.5) months after surgery. Intraretinal microcysts were found in one patient. In the SB group, ERM was formed in 4 (12%) patients at a mean time of 7.4 ± 2.9 (range: 4-10.5) months after surgery. Central foveal microcysts were found in 2 patients. Cataract progression was found in two patients after PPV and SB after 6 and 10 months; both cases were excluded from the study.
DISCUSSION
This study showed that in both the PPV and SB groups, there was a significant correlation between the first post-operation visit BCVA and final BCVA. In the SB group, there was a strong correlation between better final visual acuity and intact IS/OS junction and an intact ELM. Surprisingly, patients in the fused subgroup (fused IS/OS to ELM) had better final visual acuity than those with disrupted IS/OS junction. In the PPV group, retinal layer integrity status was not correlated with final BCVA. Visual outcomes correlated strongly with integrity of the IS/OS line in previous reports, both with scleral buckle and PPV.[7,6,11,12,13,14,15] At the proximal portion of the photoreceptor outer segment, a persistently disrupted IS/OS line suggests the absence of photoreceptor cells which is the source of visual transduction.
The association between the integrity of the ELM and postoperative visual outcome, was shown in a study by Wakabayashi et al.[7] They suggested that disruption of the IS/OS junction and the ELM at the fovea after successful RRD repair, could indicate that morphological changes in the photoreceptor layer are not limited to the photoreceptor's IS/OS level, but extended toward the photoreceptor's cell bodies and Muller cells. In our series, no eye showed disrupted ELM with an intact IS/OS junction, suggesting that the first retinal insult resulting from RRD may occur in the photoreceptor OS, and that the OS was not restored completely in any eye with disrupted ELM. The repair of photoreceptors also appears to have an in–out pattern. As with Wakabayashi et al and Gharbiya et al, the postoperative preservation of the ELM, seems to be important in restoration of the photoreceptor layer in preoperative macula-off eyes.[7,12,14] This may account for some of the variations observed in visual recovery after successful RRD repair.
It was noticed that the first post-operative visit BCVA is important in predicting the final visual outcome in both the PPV and SB groups. Gharbiya et al reported that not only the status of the ELM and the IS/OS junction, but also integrity of the intermediate line and the outer nuclear layer thickness changes, may be important predictors of postoperative visual outcome, after anatomically successful RRD repair.[12] In our series, ELM disruption was observed in 62.5% of eyes (in the PPV group) and 22% of eyes (in the SB group). Gharbiya reported ELM disruption in 30% of cases after PPV. ELM disruption has been reported in 24-33% of eyes after PPV or SB[7,16] and in some reports it was stated as of no importance for visual recovery.[16]
In this study, the percentage of eyes with disrupted IS/OS junction decreased from 66.6% to 22% at final visit (9 month) in the PPV group. In the SB group, the percentage of eyes with disrupted IS/OS junction was 16.7% which was restored in all patients at 10 months. Shimoda et al reported that after PPV, the frequency of IS/OS junction disruption decreased from 55% in the first month to 17% in the sixth month.[15] They reported that mean BCVA was lower in eyes with a disrupted IS/OS line compared with other configurations at 6 months. Schocket et al in a mixed group of patients after PPV/SB/pneumatic retinopexy, reported that IS/OS junction disruption was present in 82% of cases[6] and Smith, in a similar but prospective study, reported IS/OS disruption in 76% of cases.[11] Gharbiya et al in a study on macula-off eyes after SB, reported IS/OS junction disruption in 52% of cases and reported that postoperative BCVA was lower in eyes with photoreceptor layer abnormalities than those without it.[12] Wakabayashi et al reported IS/OS junction disruption in 43% of eyes after PPV and SB, which was restored in 64% of eyes.[7]
In the present study, final visual acuity was not affected by ONL thickness unlike earlier reports stating it as an important predictor of visual outcome in central serous retinopathy.[12,17] Experimental studies, in both animal models and human eyes have shown that RD caused photoreceptor cell death by apoptosis, as early as 1-3 days.[18,19,20,21] A steady decline in the thickness of the ONL and a decrease in the number of photoreceptor nuclei has been shown to occur in the detached retina.[18,22]
SRF was observed in 22% of eyes in the PPV group which was partially resolved at the final visit, and 47% of eyes in the SB group which was resolved in 78% of eyes at a mean time of 10 months. Final BCVA was not affected by the presence of SRF or duration of SRF persistence. Wakabayashi et al reported SRF in 13% of their cases, which resolved in 6 months.[7] SRF was reported not to be critical in prolonged visual impairment in patients with anatomically successful RD repair. Benson et al reported SRF in 15% of PPV cases, of which 47% of them resolved at six months, and showed that the presence of SRF is associated with worse visual acuity recorded at six weeks.[5] Shimoda et al reported SRF in 40% of eyes even at 6 months, but the visual outcomes were as good as eyes with an intact IS/OS line.[15] Gharbiya et al, in SB cases, reported SRF at a mean time of 14.5 months in 13% and showed that mean BCVA was not different between eyes with SRF and those without it.[12]
The current study has some limitations such as small sample size, especially in the PPV group precluding accurate comparison of the results in both groups. Some patients with good visual outcome did not complete their final visits, thereby reducing the rates of visual recovery and structural improvement in this study. Other causes of incomplete recovery of vision, such as that caused by cataracts especially in the vitrectomy group and also photo-toxicity due to the illumination system of vitrectomy, could undermine the results of this study. Additionally, the longer mean duration of symptoms in the PPV group, could also be a reason for failure in finding a significant correlation between microstructural changes and visual acuity in this group.
In summary, using SD-OCT we observed that in eyes undergoing PPV and SB for RRD, there was a significant correlation between the first postoperative BCVA and final BCVA. It was found that after SB surgery, patients with intact IS/OS junction and ELM had better visual recovery 12-15 months after surgery. At the final visit, such a correlation was absent in the PPV group. Incomplete visual acuity recovery, after anatomically successful RRD repair, could be attributed to several pre- and post-operative factors influencing foveal microstructure. Studies with a larger sample size are required in this field.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Oshima Y, Yamanishi S, Sawa M, Motokura M, Harino S, Emi K. Two-year follow-up study comparing primary vitrectomy with scleral buckling for macula-off rhegmatogenous retinal detachment. Jpn J Ophthalmol. 2000;44:538–549. doi: 10.1016/s0021-5155(00)00205-7. [DOI] [PubMed] [Google Scholar]
- 2.Salicone A, Smiddy WE, Venkatraman A, Feuer W. Visual recovery after scleral buckling procedure for retinal detachment. Ophthalmology. 2006;113:1734–1742. doi: 10.1016/j.ophtha.2006.03.064. [DOI] [PubMed] [Google Scholar]
- 3.Cleary PE, Leaver PK. Macular abnormalities in the reattached retina. Br J Ophthalmol. 1978;62:595–603. doi: 10.1136/bjo.62.9.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tani P, Robertson DM, Langworthy A. Prognosis for central vision and anatomic reattachment in rhegmatogenous retinal detachment with macula detached. Am J Ophthalmol. 1981;92:611–620. doi: 10.1016/s0002-9394(14)74651-3. [DOI] [PubMed] [Google Scholar]
- 5.Benson SE, Schlottmann PG, Bunce C, Xing W, Charteris DG. Optical coherence tomography analysis of the macula after vitrectomy surgery for retinal detachment. Ophthalmology. 2006;113:1179–1183. doi: 10.1016/j.ophtha.2006.01.039. [DOI] [PubMed] [Google Scholar]
- 6.Schocket LS, Witkin AJ, Fujimoto JG, Ko TH, Schuman JS, Rogers AH, et al. Ultrahigh-resolution optical coherence tomography in patients with decreased visual acuity after retinal detachment repair. Ophthalmology. 2006;113:666–672. doi: 10.1016/j.ophtha.2006.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wakabayashi T, Oshima Y, Fujimoto H, Murakami Y, Sakaguchi H, Kusaka S, et al. Foveal microstructure and visual acuity after retinal detachment repair: Imaging analysis by Fourier-domain optical coherence tomography. Ophthalmology. 2009;116:519–528. doi: 10.1016/j.ophtha.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 8.Sheth S, Dabir S, Natarajan S, Mhatre A, Labauri N. Spectral domain-optical coherence tomography study of retinas with a normal foveal contour and thickness after retinal detachment surgery. Retina. 2010;30:724–732. doi: 10.1097/iae.0b013e3181cd47bb. [DOI] [PubMed] [Google Scholar]
- 9.Wolfensberger TJ, Gonvers M. Optical coherence tomography in the evaluation of incomplete visual acuity recovery after macula-off retinal detachments. Graefes Arch Clin Exp Ophthalmol. 2002;240:85–89. doi: 10.1007/s00417-001-0410-6. [DOI] [PubMed] [Google Scholar]
- 10.Hagimura N, Iida T, Suto K, Kishi S. Persistent foveal retinal detachment after successful rhegmatogenous retinal detachment surgery. Am J Ophthalmol. 2002;133:516–520. doi: 10.1016/s0002-9394(01)01427-1. [DOI] [PubMed] [Google Scholar]
- 11.Smith AJ, Telander DG, Zawadzki RJ, Choi SS, Morse LS, Werner JS, et al. High-resolution Fourier-domain optical coherence tomography and microperimetric findings after macula-off retinal detachment repair. Ophthalmology. 2008;115:1923–1929. doi: 10.1016/j.ophtha.2008.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gharbiya M, Grandinetti F, Scavella V, Cecere M, Esposito M, Segnalini A, et al. Correlation between spectral-domain optical coherence tomography findings and visual outcome after primary rhegmatogenous retinal detachment repair. Retina. 2012;32:43–53. doi: 10.1097/IAE.0b013e3182180114. [DOI] [PubMed] [Google Scholar]
- 13.Nakanishi H, Hangai M, Unoki N, Sakamoto A, Tsujikawa A, Kita M, et al. Spectral-domain optical coherence tomography imaging of the detached macula in rhegmatogenous retinal detachment. Retina. 2009;29:232–242. doi: 10.1097/IAE.0b013e31818bcd30. [DOI] [PubMed] [Google Scholar]
- 14.Lai WW, Leung GY, Chan CW, Yeung IY, Wong D. Simultaneous spectral domain OCT and fundus autofluorescence imaging of the macula and microperimetric correspondence after successful repair of rhegmatogenous retinal detachment. Br J Ophthalmol. 2010;94:311–318. doi: 10.1136/bjo.2009.163584. [DOI] [PubMed] [Google Scholar]
- 15.Shimoda Y, Sano M, Hashimoto H, Yokota Y, Kishi S. Restoration of photoreceptor outer segment after vitrectomy for retinal detachment. Am J Ophthalmol. 2010;149:284–290. doi: 10.1016/j.ajo.2009.08.025. [DOI] [PubMed] [Google Scholar]
- 16.Delolme MP, Dugas B, Nicot F, Muselier A, Bron AM, Creuzot-Garcher C. Anatomical and functional macular changes after rhegmatogenous retinal detachment with macula off. Am J Ophthalmol. 2012;153:128–136. doi: 10.1016/j.ajo.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 17.Matsumoto H, Sato T, Kishi S. Outer nuclear layer thickness at the fovea determines visual outcomes in resolved central serous chorioretinopathy. Am J Ophthalmol. 2009;148:105–110.e1. doi: 10.1016/j.ajo.2009.01.018. [DOI] [PubMed] [Google Scholar]
- 18.Lewis GP, Charteris DG, Sethi CS, Fisher SK. Animal models of retinal detachment and reattachment: Identifying cellular events that may affect visual recovery. Eye (Lond) 2002;16:375–387. doi: 10.1038/sj.eye.6700202. [DOI] [PubMed] [Google Scholar]
- 19.Cook B, Lewis GP, Fisher SK, Adler R. Apoptotic photoreceptor degeneration in experimental retinal detachment. Invest Ophthalmol Vis Sci. 1995;36:990–996. [PubMed] [Google Scholar]
- 20.Hisatomi T, Sakamoto T, Goto Y, Yamanaka I, Oshima Y, Hata Y, et al. Critical role of photoreceptor apoptosis in functional damage after retinal detachment. Curr Eye Res. 2002;24:161–172. doi: 10.1076/ceyr.24.3.161.8305. [DOI] [PubMed] [Google Scholar]
- 21.Arroyo JG, Yang L, Bula D, Chen DF. Photoreceptor apoptosis in human retinal detachment. Am J Ophthalmol. 2005;139:605–610. doi: 10.1016/j.ajo.2004.11.046. [DOI] [PubMed] [Google Scholar]
- 22.Erickson PA, Fisher SK, Anderson DH, Stern WH, Borgula GA. Retinal detachment in the cat: The outer nuclear and outer plexiform layers. Invest Ophthalmol Vis Sci. 1983;24:927–942. [PubMed] [Google Scholar]


