Abstract
Purpose:
To determine the prevalence of various types of conjunctival lesions, at a tertiary ophthalmic center in Fars Province, South of Iran.
Methods:
Histopathologic slides and medical records of conjunctival lesions submitted to the pathology department of Khalili Hospital, Shiraz, Iran were reviewed from April, 2009 to July, 2013. The histopathologic diagnoses were categorized into benign, pre-malignant, and malignant lesions. The prevalence of various types of conjunctival lesions was calculated.
Results:
Histologic sections of 631 conjunctival lesions were reviewed. Benign lesions were most prevalent (81.8%), followed by premalignant (10.8%) and malignant (7.4%) lesions. Pterygia were the most common benign lesions (69.2%), intraepithelial dysplasia constituted most cases of premalignant lesions (94.1%), and squamous cell carcinoma was the most frequent malignant lesion (93.6%). Benign lesions were the most common type of lesions in all age groups, however the prevalence of malignant lesions increased significantly with age (P < 0.001).
Conclusion:
Benign lesions were the most common conjunctival lesions with pterygia on top of the list, while intraepithelial neoplasia and squamous cell carcinoma were the most common premalignant and malignant lesions, respectively. Conjunctival malignant lesions were more prevalent with older age.
Keywords: Conjunctival Lesions, Intraepithelial Dysplasia, Squamous Cell Carcinoma
INTRODUCTION
The conjunctiva is readily visible and partially exposed to sunlight; therefore, conjunctival tumors and related lesions are recognizable early in their course.[1] Conjunctival tumors, based on their origin, are categorized into melanocytic and non-melanocytic types, both arising from epithelial and stromal components.[2] Conjunctival epithelial lesions vary from benign tumors such as papillomas, to malignant lesions such as squamous cell carcinoma (SCC).[3] Melanocytic and non-melanocytic tumors have been reported to comprise 53 and 47% of all excised conjunctival tumors, respectively.[2]
Ocular surface squamous neoplasia (OSSN) are composed of epithelial lesions such as dysplasia, carcinoma in situ and SCC which involve the conjunctiva and cornea.[4] Main factors associated with conjunctival epithelial lesions include sunlight exposure, human papilloma virus (HPV) subtypes 6, 11, 16, 18, and human immunodeficiency (HIV) infection.[3,5] Other factors associated with OSSN are old age, male sex and fair skin.[6,7] According to Newton et al[8] the incidence of ocular SCC increases 49% with every 10-degree decline in latitude. Higher exposure of male subjects to sunlight while working outdoors may explain the higher prevalence of OSSN in males.[3,9]
Although, a previous study was conducted at Farabi Eye Hospital, a referral ophthalmology center in Iran, there is no information about the frequency of conjunctival lesions in other parts of Iran with different amounts of sun exposure. The current study was conducted to identify the prevalence of various types of conjunctival lesions at the pathology department of Khalili Hospital, Shiraz, Fars Province (a tertiary care referral center located in the south of Iran). It has a homogenous rural population composed of inhabitants (with a low immigration rate) with more intense and longer duration of sun exposure as compared to other parts the country.
METHODS
After obtaining permission from the Ethics Committee of the Pathology Department of Shiraz University of Medical Sciences, Iran, in a retrospective study, the histology slides and database of conjunctival specimens submitted to Khalili Hospital, Shiraz, Fars Province, Iran, between April 2009 and July 2013 were reviewed by three pathologists. The histologic diagnoses were categorized into three groups of benign, premalignant and malignant lesions according to the World Health Organization (WHO) classification of conjunctival tumors.[10] The prevalence of various types of conjunctival lesions was calculated and associations between conjunctival lesions as and demographic data were analyzed by SPSS version 17 (SPSS corporation, Chicago, Il, USA).
RESULTS
A total of 631 conjunctival specimens from 628 patients were analyzed. Patient age ranged from 2 to 88 (mean 45.7 ± 19.0) years and there was no sex predilection (50.7% of cases were female). Out of 631 specimens, 516 (81.8%) were categorized as benign, 68 (10.8%) as premalignant, and 47 (7.4%) as malignant lesions. Melanocytic lesions comprised (13.3%) of all excised lesions and included nevi, primary acquired melanosis (PAM) and malignant melanoma in 12.5%, 0.4% and 0.4% of cases, respectively. Data for the three types of conjunctival lesions are detailed in Table 1.
Table 1.
Classification and frequency of conjunctival lesions
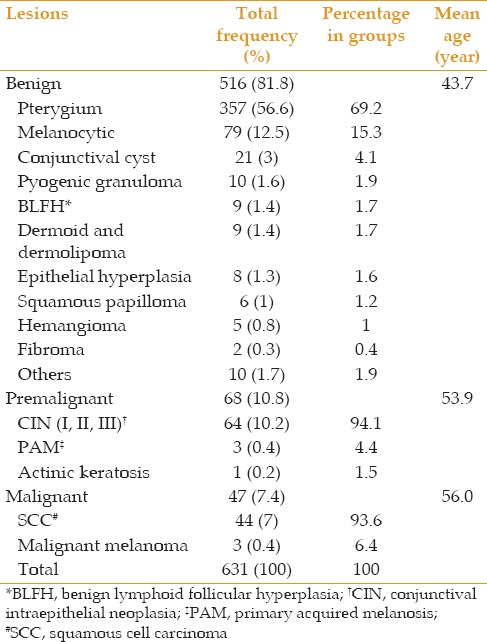
Pterygia were the most common benign lesions (69.2%) and were combined with cysts and nevi in 2.3% of cases. Melanocytic lesions such as nevi and lentigo were the second most common benign lesions (15.3%) followed by conjunctival cysts (4.1%). Conjunctival intraepithelial neoplasia (CIN) was the most common premalignant lesion (94.1%); these lesions had been diagnosed clinically as pterygia in 31.2% of cases. PAM and actinic keratosis were the second (4.4%) and third (1.5%) most frequent premalignant lesions respectively. SCC was the most common malignant lesion (93.6%), followed by malignant melanoma (6.4%).
Mean age of patients with benign, premalignant and malignant lesions was 43.7, 53.9 and 56.0 years, respectively. The age distribution of the patients with regard to the histological diagnosis is illustrated in Figure 1. No significant sex predilection was observed for benign (52.9% female cases) or malignant (51% female cases) conjunctival lesions, however premalignant lesions occurred twice as commonly in men (66.2% in males versus 33.8% in females). Although, benign lesions were most common in all age ranges, after the age of 60, a decline in the incidence of benign lesions and a significant increase in the prevalence of premalignant and malignant lesions was observed (P < 0.001).
Figure 1.
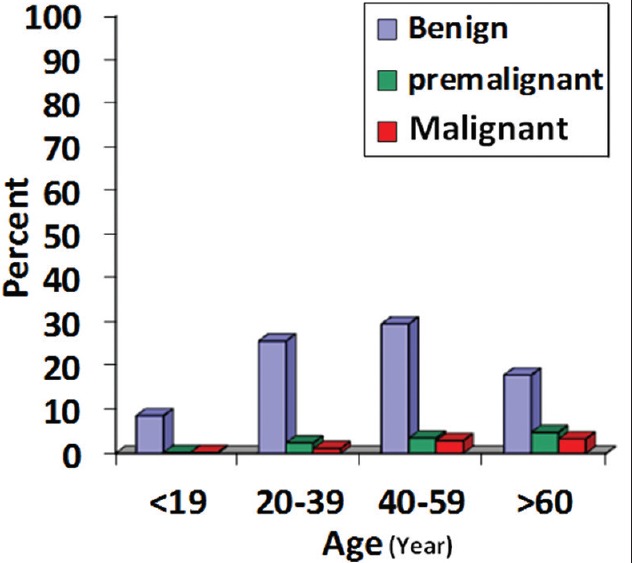
Prevalence of histologic diagnoses in relation to age.
DISCUSSION
This study showed that benign conjunctival lesions were the most common type of lesions across all age groups. Premalignant and malignant cases were the second and third leading lesions of the conjunctiva, and a significant increasing trend was observed in their prevalence with older age. The results of this study are comparable to previous reports with regard to the prevalence of conjunctival lesions,[4,11] and were consistent with the report by Lee and Hirst,[6] in which aging was stated as an important risk factor for premalignant and malignant conjunctival epithelial lesions.
The average age of OSSN is reported to be 56 years but it may occur in younger subjects living closer to the equator. Average age of patients with carcinoma in situ, is 5 to 9 years less than those with invasive carcinoma, suggesting the progressive nature of the neoplasm.[6,12] In this study, average age of patients with premalignant and malignant lesions was 53.9 and 56.0 years, which is consistent with previous reports.[6,12] However, malignant lesions can occur in younger cases with xeroderma pigmentosum (XP)[13] as evident in one of our patients who was a 12-year-old XP case with conjunctival SCC.
In spite of more intense sun exposure in Fars Province, located in the south of Iran, the prevalence of premalignant and malignant lesions in the study by Amoli and Heidari[14] was more than twice that of the current study (41.6% versus 18.1%). This can be attributed to different referral patterns of the centers (i.e., more patients with clinically diagnosed malignant conjunctival lesions are referred to Farabi Eye Hospital as compared to Khalili Eye Hospital). The difference can also be caused by non-homogeneity of patients referred from all parts of Iran and the Middle East region to Farabi Eye Hospital. Moreover, in the study by Amoli and Heidari[14] unlike the current study, pterygia were not included and it seems that premalignant and malignant lesions in this study might have been under-represented due to the large numbers of pterygia cases.
In contrast to previous studies where benign and malignant conjunctival lesions were more prevalent in male subjects,[3,9] no sex predilection was found for such lesions in the current series. This can be explained by the theory that social and economical conditions present in this part of Iran, cause female subjects to spend more time working outdoors, as also observed in a study conducted in Zimbabwe,[15] with OSSN lesions being more frequent in female subjects.
In the current study, 31.2% (about one third) of all CIN lesions were clinically diagnosed with pterygia and the overall rate of CIN in the entire spectrum of pterygia was 5.3%. The prevalence of OSSN in surgically excised pterygia was reported to be 1.7% by Oellers et al[16] and 9.8% by Hirst et al[17] confirming the importance of histopathological evaluation of all excised pterygia.
In summary, benign lesions were the most common conjunctival lesions in all age groups in the current series, with premalignant and malignant lesions occurring more frequently with older age. Since dysplastic or malignant changes may occur on a pterygium, histological evaluation is necessary in any pterygia like lesion.
Financial support and sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Shields CL, Shields JA. Tumors of the conjunctiva and cornea. Surv Ophthalmol. 2004;49:3–24. doi: 10.1016/j.survophthal.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 2.Shields CL, Demirci H, Karatza E, Shields JA. Clinical survey of 1643 melanocytic and nonmelanocytic conjunctival tumors. Ophthalmology. 2004;111:1747–1754. doi: 10.1016/j.ophtha.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 3.Alves LF, Fernandes BF, Burnier JV, Zoroquiain P, Eskenazi DT, Burnier MN., Jr Incidence of epithelial lesions of the conjunctiva in a review of 12,102 specimens in Canada (Quebec) Arq Bras Oftalmol. 2011;74:21–3. doi: 10.1590/s0004-27492011000100005. [DOI] [PubMed] [Google Scholar]
- 4.Grossniklaus HE, Green WR, Luckenbach M, Chan CC. Conjunctival lesions in adults. A clinical and histopathologic review. Cornea. 1987;6:78–116. doi: 10.1097/00003226-198706020-00002. [DOI] [PubMed] [Google Scholar]
- 5.Pe'er J. Ocular surface squamous neoplasia. Ophthalmol Clin North Am. 2005;18:1–13. doi: 10.1016/j.ohc.2004.08.001. vii. [DOI] [PubMed] [Google Scholar]
- 6.Lee GA, Hirst LW. Ocular surface squamous neoplasia. Surv Ophthalmol. 1995;39:429–450. doi: 10.1016/s0039-6257(05)80054-2. [DOI] [PubMed] [Google Scholar]
- 7.Sun EC, Fears TR, Goedert JJ. Epidemiology of squamous cell conjunctival cancer. Cancer Epidemiol Biomarkers Prev. 1997;6:73–77. [PubMed] [Google Scholar]
- 8.Newton R, Ferlay J, Reeves G, Beral V, Parkin DM. Effect of ambient solar ultraviolet radiation on incidence of squamous-cell carcinoma of the eye. Lancet. 1996;347:1450–1451. doi: 10.1016/s0140-6736(96)91685-2. [DOI] [PubMed] [Google Scholar]
- 9.Lee GA, Hirst LW. Retrospective study of ocular surface squamous neoplasia. Aust NZ J Ophthalmol. 1997;25:269–276. doi: 10.1111/j.1442-9071.1997.tb01514.x. [DOI] [PubMed] [Google Scholar]
- 10.Campbell RJ, Sobin LH. 2nd ed. Berlin: Springer; 1998. In Collaboration with Pathologists in 11 Countries. World Health Organization International Histological Classification of Tumors, Histological Typing of Tumors of the Eye and Its Adnexa. [Google Scholar]
- 11.Mondal SK, Nag DR, Bandyopadhyay R, Adhikari A, Mukhopadhyay S. Conjunctival biopsies and ophthalmic lesions: A histopathologic study in eastern India. J Res Med Sci. 2012;17:1176–1179. [PMC free article] [PubMed] [Google Scholar]
- 12.Elsas FJ, Green WR. Epibulbar tumors in childhood. Am J Ophthalmol. 1975;79:1001–1007. doi: 10.1016/0002-9394(75)90685-6. [DOI] [PubMed] [Google Scholar]
- 13.Hertle RW, Durso F, Metzler JP, Varsa EW. Epibulbar squamous cell carcinomas in brothers with Xeroderma pigmentosa. J Pediatr Ophthalmol Strabismus. 1991;28:350–353. doi: 10.3928/0191-3913-19911101-15. [DOI] [PubMed] [Google Scholar]
- 14.Amoli FA, Heidari AB. Survey of 447 patients with conjunctival neoplastic lesions in Farabi Eye Hospital, Tehran, Iran. Ophthalmic Epidemiol. 2006;13:275–279. doi: 10.1080/09286580600801036. [DOI] [PubMed] [Google Scholar]
- 15.Pola EC, Masanganise R, Rusakaniko S. The trend of ocular surface squamous neoplasia among ocular surface tumour biopsies submitted for histology from Sekuru Kaguvi Eye Unit, Harare between 1996 and 2000. Cent Afr J Med. 2003;49:1–4. [PubMed] [Google Scholar]
- 16.Oellers P, Karp CL, Sheth A, Kao AA, Abdelaziz A, Matthews JL, et al. Prevalence, treatment, and outcomes of coexistent ocular surface squamous neoplasia and pterygium. Ophthalmology. 2013;120:445–450. doi: 10.1016/j.ophtha.2012.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hirst LW, Axelsen RA, Schwab I. Pterygium and associated ocular surface squamous neoplasia. Arch Ophthalmol. 2009;127:31–32. doi: 10.1001/archophthalmol.2008.531. [DOI] [PubMed] [Google Scholar]


