Abstract
Background and Objectives:
Extra-pancreatic cysts (EPCs) are incidentally found in patients with pancreatic cystic lesions (PCLs). The aim of this study is to find the prevalence of concurrent EPC in patients with PCLs, investigate associations with neoplastic lesions, and compare the prevalence of EPC to a control population.
Materials and Methods:
A retrospective study of patients who underwent endoscopic ultrasound (EUS) over a 3-year period. The study group consisted of patients with PCLs. The control group included equal number of matched (age and sex) patients who had undergone EUS for reasons other than evaluation of PCLs. All patients had undergone computed tomography (CT) that was reviewed for EPCs.
Results:
A total of 191 patients were found to have PCLs. One patient with Von Hippel-Lindau (VHL) disease was excluded. Majority of the patients were female (60%); most PCLs were solitary (68.9%), unilocular (56.8%), predominantly located in the head of the pancreas (37.4%); and mean PCL diameter was 28.12 ± 18.4mm. EUS-guided fine-needle aspiration (FNA) was performed in 171 (90%) patients with 73 (42.7%) PCLs demonstrating cysts with benign epithelial cells, 37 (21.6%) mucinous cysts, 18 (10.5%) mucinous adenocarcinomas, 11 (6.4%) neuroendocrine tumors, nine intraductal papillary mucinous cystic neoplasms (IPMNs), six pseudocysts, five serous cyst adenomas (SCAs), and five with inadequate sampling. An EPC was observed in 97 of 190 (51.18%) patients with PCLs and in 67 of 190 (35.3%) controls (P < 0.001). The distribution of EPCs in PCL patients and controls (n = 190) were 32.1% vs. 15.8% (P < 0.001) for liver cysts, 30.0% vs. 20.5% (P = 0.04) for renal cysts, and 3.7% vs. 1.6% (P = 0.34) for cysts in other organs. Mean liver cyst diameter (15.6 mm vs. 10.1 mm, P = 0.23) and renal cyst diameter (20.4 mm vs. 20.1 mm, P = 0.95) were not statistically different in PCL patients compared to controls. Multivariate analysis demonstrated that among patients with PCLs, EPCs increased with age (mean age 69.6 vs. 62.4 years, P ≤ 0.001, odds ratio (OR) 1.06, 95% confidence interval (CI) 1.03, 1.09), and male gender was associated with higher chance of finding renal cysts (OR 2.17, P = 0.021, 95% CI 1.13, 4.19). There was no association between FNA result and prevalence or type of EPC.
Conclusion:
The prevalence of EPCs in patients with PCLs was significantly higher than in a matched control group. Among patients with PCLs, a liver cyst is the most common EPC. Increasing age is associated with higher prevalence of EPCs.
Keywords: Cystic pancreatic neoplasms, endoscopic ultrasound, EUS, extra-pancreatic cyst, liver cyst, pancreatic cyst, renal cyst
INTRODUCTION
Cystic lesions of the pancreas consists of pseudocysts, congenital cysts (sometimes called simple cysts), and cystic neoplasms.[1] Ninety percent of pancreatic cystic lesions (PCLs) are benign nonneoplastic processes such as pseudocysts.[2] PCLs may be incidentally identified in asymptomatic patients or in patients with symptoms of biliary obstruction, pancreatitis, or abdominal pain. Patients who are symptomatic generally proceed to surgical resection. As a result of better radiological imaging, these lesions are being observed more frequently.
Pancreatic cystic neoplasms (PCNs) account for 10-15% of pancreatic cysts[3,4] and can be divided into nonmucinous (benign) and mucinous (premalignant or malignant) cyst. Nonmucinous cysts include serous cyst adenomas (SCAs) and cystic neuroendocrine tumors. SCAs are a benign type of PCNs that rarely get malignant.[5] Mucinous lesions include mucinous cystic neoplasms (MCNs) and intraductal papillary mucinous cystic neoplasms (IPMNs) and may be premalignant or malignant.[6,7]
Accurate diagnosis of these cysts is important, because mucinous cysts have the potential for malignant transformation and surgical resection should be considered.[8,9,10] Computed tomography (CT) and magnetic resonance imaging (MRI) have been used to characterize the morphology of PCLs. Conventional radiologic criteria alone are generally inadequate for distinguishing between benign and neoplastic PCLs. Endoscopic ultrasound (EUS) has become the preferred modality for diagnosing and localizing PCLs. EUS-guided fine-needle aspiration (FNA) for tumor cytology or for tumor marker immunoassay has emerged as one method for effectively identifying carcinoma and/or distinguishing mucinous from serous cystic lesions.[11,12]
There is insufficient data about extra-pancreatic cysts (EPC) in patients with PCLs. Zhang et al., reported the prevalence of liver cysts in 16.6% and renal cysts in 51.9% in 283 pancreatic cyst patients.[13] A more recent study reported a prevalence of 54.8% for EPCs among patients with PCLs.[14] The objective of this study was to compare the prevalence of EPCs in patients with and without PCLs after exclusion of known syndromes with such findings (Von Hippel-Lindau (VHL) disease). Secondary objectives included finding association of EPCs with different types of PCLs.
MATERIALS AND METHODS
A total of 470 EUS studies for pancreatic lesions were reviewed from April 2006 to September 2009. Among these, 191 patients with PCLs were identified. As a comparable control group, 190 matched (age and sex) patients were selected. The patients in the control group had undergone EUS for indications other than evaluation of PCL. An additional 2-year follow-up period without additional patient recruitment ensued. The analysis was approved by our Institutional Review Board. Baseline demographic data (age, gender, and presenting signs and symptoms), EUS findings, EUS-guided FNA results, operative findings, cytopathology, histopathology, and immunocytochemistry results were reviewed and recorded. EUS was performed by board certified endosonographers who had completed an additional year of training. During each procedure, the following were noted: Cyst size, echogenicity, consistency, shape, and margins of any visible pancreatic lesions and the features of any fluid aspirated. A curvilinear echoendoscope (Olympus GF-UC140P-AL5 (Olympus America, Center Valley, PA, USA) with ProSound Alpha 5 or Alpha 10 (Aloka, Wallingford, Conn)) was used to evaluate and perform EUS, while FNA of PCLs was performed with a 22- or 25-gauge needle (EchoTip Cook Medical, Bloomington, USA). Color Doppler US was used to identify major vessels in the projected needle path. One pass was performed for cystic lesions and a minimum of two passes were obtained for mixed (cystic + solid) lesions. Cyst fluid when aspirated was processed for amylase, carcinoembryonic antigen (CEA), and cytology. All CT examinations were performed onsite with the use of multidetector technology (MDCT). The MDCT images and reports were evaluated for the presence of EPC in PCL patients and controls.
Statistical methods
Data were presented as numbers and percentages for categorical variables and as mean ± standard deviation (SD) and range (minimum, maximum) for continuous variables. All statistical analyses were performed using Statistical Package for Social Sciences (SPSS), version 20 (IBM Corporation, Somers, NY). Chi-square test was used for analysis of categorical data. A t-test was used to compare differences in continuous variables between groups. Binary logistic regression was performed for multivariate analysis and results were presented as odds ratios (OR) and 95% confidence interval (CI). Statistical significance was defined as P - value ≤ 0.05.
RESULTS
Characteristics of patients with PCLs
Among a total of 191 patients identified with PCLs, one patient with a diagnosis of VHL disease was excluded from the analysis. Majority of the patients were female (60%) with mean age ± standard deviation of 66.12 ± 12.02 years. The demographics, clinical presentation, and locations of the PCLs are as described in Table 1. A solitary cyst was observed in 131 (68.9%) patients. While 93 (48.9%) patients were asymptomatic, complaints of abdominal pain (n = 54), weight loss (n = 20), back pain (n = 14), and jaundice (n = 8) were observed in the symptomatic patients. Pancreatic EUS morphology showed unilocular cyst in 108 (56.8%) patients, and mixed type (cystic + solid) in 82 (43.2%) patients. Median PCL diameter was 28.50 ± 18.1mm. Diagnostic EUS-FNA was performed in 171 (90%) patients. No complications related to the procedure were observed. Cytopathology evaluation resulted in majority (73, 42.7%) of the diagnostic aspirations demonstrating benign epithelial cells, while 37 (21.6%) were mucinous cysts and 18 (10.5%) were adenocarcinomas. Figures 1 and 2 shows example of patients with PCLs and EPCs.
Table 1.
Characteristics of pancreatic cysts
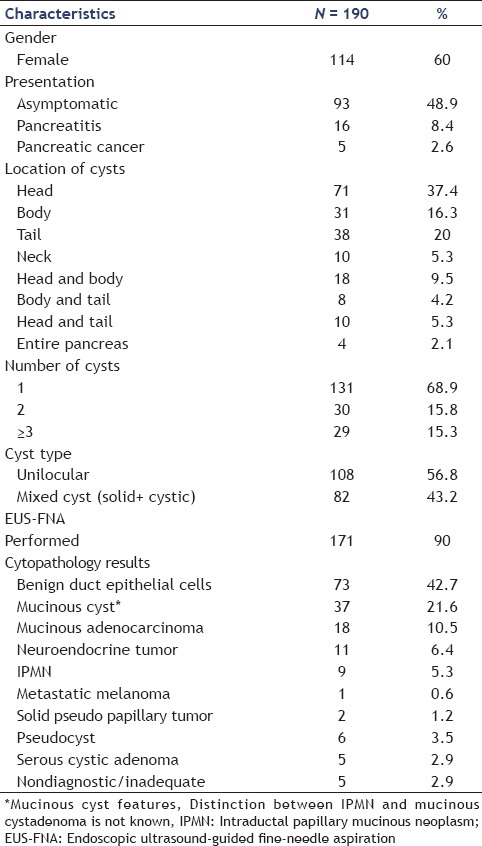
Figure 1.
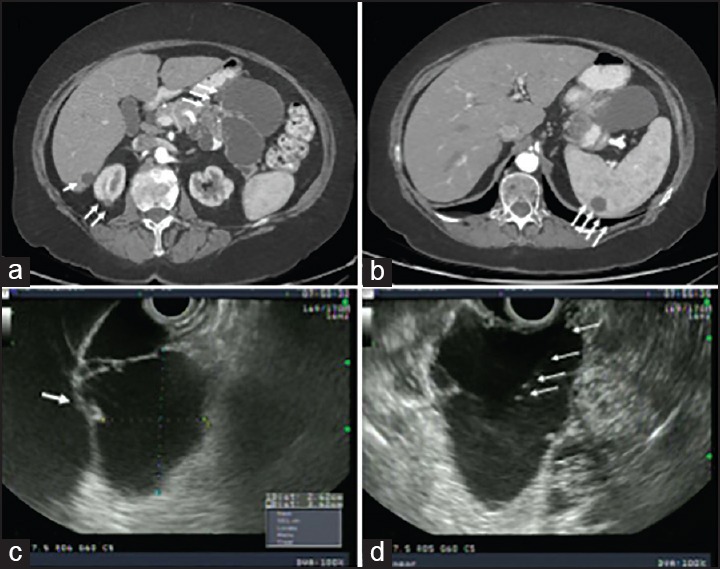
CT and EUS in a 77-year-old woman. (a) CT liver cyst in segment VI, small cyst in right kidney, 106 mm × 84 mm cystic lesion in tail of pancreas, and (b) 27 mm cystic lesion in the spleen. (c) EUS view of large multicystic lesion (37 mm × 37 mm) in pancreatic Tail and (d) EUS-FNA of pancreatic cyst. CT = Computed tomography, EUS = Endoscopic ultrasound, FNA = Fine-needle aspiration
Figure 2.
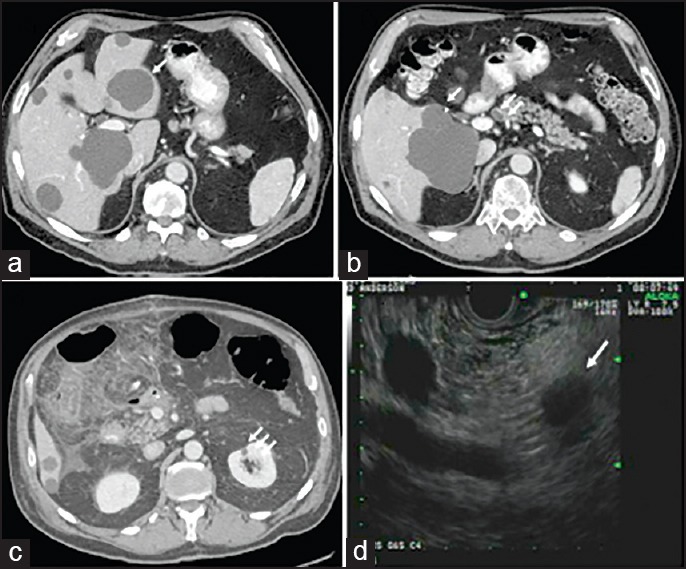
CT and EUS of a 81-year-old man. (a) Multiple liver cysts, (b) liver cyst, and 15 mm × 12 mm cyst in the head of the pancreas. (c) Liver cyst and thin cyst in right kidney. (d) EUS view of 11 mm cystic lesion in the head of the pancreas
Prevalence of EPC in cases and controls
From the EUS database, 190 patients comparable for both age and sex (54.2% female, mean age: 64.26 ± 10.35 years) were selected as the control group. In the control group, 124 had normal pancreas and 66 had solid pancreatic lesions. Table 2 depicts distribution of EPCs in both the study and control group. Among patients with PCLs, an EPC was observed in 97 of 190 (51.05%) patients. These included cysts in the liver (61, 32.1%) followed by renal cysts (57, 30%) and cysts in other organs (7, 3.7%). The prevalence of EPCs was 42.9, 34.5, and 10.7% in patients with simple cysts, mucinous cysts, and pancreatic adenocarcinomas, respectively.
Table 2.
Distribution of extrapancreatic cysts in patients with pancreatic cystic lesions and control group
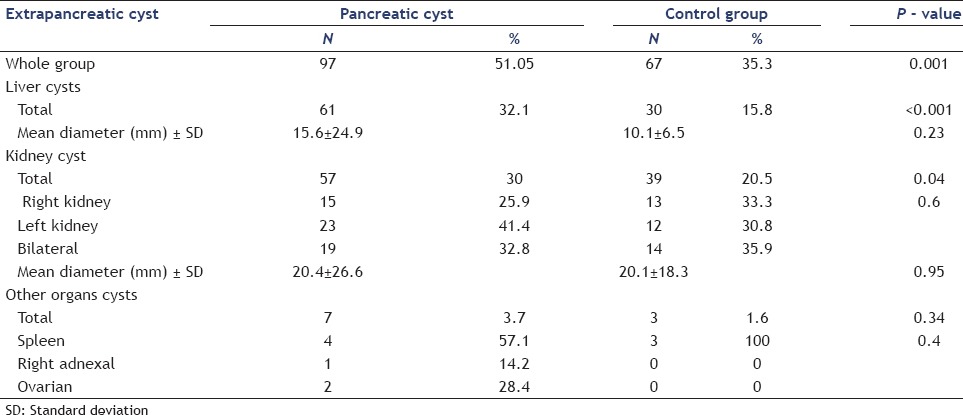
In the control group, EPC was observed in 35.3% (n = 67) patients of which liver cysts (30, 15.8%), renal cysts (39, 20.5%), and cysts in other abdominal organs (3, 1.6%) were observed respectively. Comparing the two groups, presence of PCL was associated with higher odds of having a liver cyst (OR 2.52, 95% CI 1.5, 4.3, P ≤ 0.001) and a renal cyst (OR 1.66, 95% CI 1.01, 2.73, P = 0.04). No significant differences were found among the groups regarding the size of liver cysts or renal cysts (P = 0.23 and 0.94, respectively).
By univariate analysis, among patients with PCLs, the prevalence of liver cysts was higher in those with renal cysts and increased age [Table 3]. Presence of renal cysts with PCLs was associated with the male gender, presence of liver cyst, increasing age, and increasing number of liver cysts. None of the cytological findings were associated with higher chance of finding liver or renal cysts [Table 3].
Table 3.
Univariate analysis of cysts in liver and kidney among patients with cystic pancreatic lesions
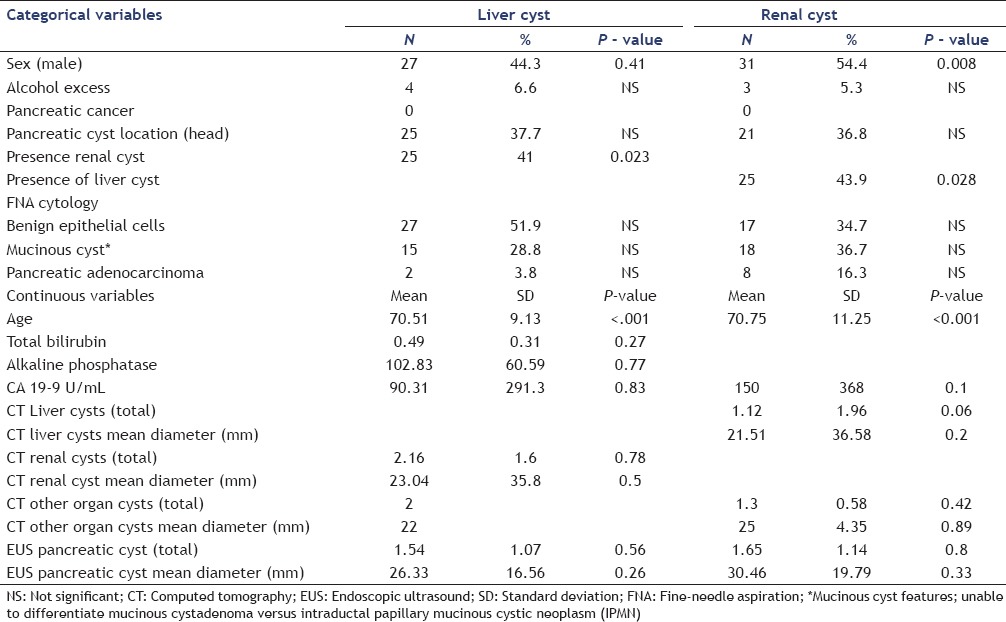
Following multivariate analysis, among patients with PCLs, higher age was associated with higher prevalence of liver cysts (OR 1.05, P = 0.003, 95% CI 1.02, 1.08) and renal cysts (OR 1.05, P = 0.004, 95% CI 1.02, 1.1). Male gender was associated with higher chance of finding renal cysts in patients with PCL (OR 2.17, P = 0.021, 95% CI 1.13, 4.19).
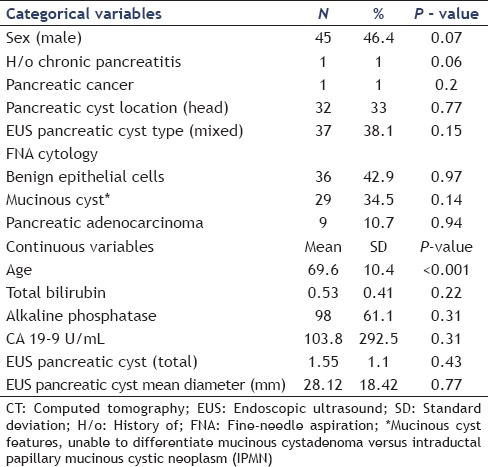
Grouping all EPCs together, multivariate analysis revealed that patients with PCLs who had EPCs tend to be older than patients with only PCLs (OR 1.06, 95% CI 1.03, 1.09, P ≤ 0.001) [Table 4]. There were no significant statistical differences between these groups when compared for type of cyst, cytopathology result, or cyst location in the pancreas.
Table 4.
Univariate analysis of all extrapancreatic cysts in patients with pancreatic cystic lesions
DISCUSSION
Patients with VHL and polycystic kidney disease are known to have cysts in multiple intra-abdominal organs.[15] In patients without this disease, there is limited data about association of PCLs with EPCs.[13,14] Zhang et al., evaluated the prevalence of pancreatic cysts in 1,444 patients with MRI. Among 283 (19.6%) patients who had at least one pancreatic cyst, the prevalence of liver and renal cysts were found to be 16.6% (47/283) and 51.9% (147/283), respectively.[13] Agrawal et al., reviewed 156 patients, of whom 85 (54.8%) had PCLs and at least one EPC. The most common type of PCL was a serous cyst and the most common EPC was a cyst in the kidney and the authors suggested a genetic evaluation in such patients since this could represent attenuated manifestation of diseases like VHL.[14]
Our study is unique for the following findings. First, the presence of EPCs in patients with PCLs was compared with a comparable control population evidencing their higher prevalence. Secondly, the finding of a liver cyst was the most common EPC in patients with PCL. Thirdly, that advancing age was associated with higher prevalence of EPCs in patients with PCLs. Cystic lesions of the liver have a broad differential diagnosis including simple cysts, polycystic disease, hemangiomas, abscesses, hydatid cysts, necrotic neoplasms, Caroli's disease, and other rare causes.[16] Nonparasitic liver cysts are relatively common, which can affect up to 5% of the population.[17] Simple renal cyst is the most common form of renal cystic disease with reported incidence of 4.8% in ultrasound studies and 24-41.2% in CT studies.[18,19] The prevalence of liver cysts in patients with PCLs (32.1%) was similar to a recent study[14] (30.6%) evaluating presence of liver cysts in patients with EUS-guided detection of PCLs. This is a higher prevalence than prior reported MRI-detection of PCLs and EPCs (16.6%).[13] The prevalence of renal cysts in patients with PCLs (30%) was lower than prior reported associations where 88.2% prevalence of renal cysts with EUS-detected PCLs and 51.9% prevalence of MRI-detected renal cysts with PCLs were reported.[13,14] This might be explained by differences in the populations examined, diagnostic methods, techniques, and experience of the examiners.
The prevalence of simple renal and hepatic cysts using spiral CT in 617 patients was 41 and 18%, respectively, with increasing incidence of both with advancing age.[18] Liver cysts grow slowly and solitary cysts are not usually diagnosed before the age of 40 years. The incidence of liver cysts rises with age and they are found frequently, although incidentally with abdominal US or CT.[20] Renal cysts are rarely observed before the age of 40 years and prevalence increases with age and they are more common in men.[21] In the present study, among patients with PCLs, a higher percentage of renal and liver cysts were seen with increasing age and the prevalence of renal cysts was slightly greater in men.
We did not find any association between type of pancreatic cyst based on FNA and presence of EPC. There were a significant number of unknown pancreatic cysts where FNA demonstrated benign ductal epithelial cells. Additional criteria based on CEA levels below 192 ng/mL were applied. Continued follow-up of cysts with CEA levels between 0.5 ng/mL and 192 ng/mL with imaging studies and EUS has been suggested.[22] The associations with EPCs could have changed over long-term follow-up with eventual diagnosis of PCLs.
Among the limitations including inherent issues with retrospective studies, final pathology was not available in all patients. FNA was not performed for all PCLs. Surgery was performed only if PCLs satisfied criteria for resection or when there was a high suspicion or confirmation of malignancy. Diagnosis of PCLs continues to be challenging, especially when FNA yield is not conclusive and CEA values are below 192 ng/mL. There is likely a component of selection bias with a low prevalence of benign pancreatic diseases and chronic pancreatitis referred for evaluation to a tertiary cancer center accounting for the low number of benign PCLs. A family history of VHL and/or adult polycystic kidney disease was not available in all patients. Whether MRI would have detected more EPCs than multidetector CT is another issue to be considered.
In conclusion, the prevalence of EPCs was found in half of the patients with PCLs and was significantly higher than a comparable control group. Liver and renal cysts are the most common EPCs, the prevalence of which increases with age. Prospective investigation incorporating genetics studies may provide answers to some of the questions.
Footnotes
Source of Support: Nil.
Conflicts of Interest: None declared.
REFERENCES
- 1.Brugge WR, Lauwers GY, Sahani D, et al. Cystic neoplasms of the pancreas. N Engl J Med. 2004;351:1218–26. doi: 10.1056/NEJMra031623. [DOI] [PubMed] [Google Scholar]
- 2.Sohn TA, Yeo CJ, Cameron JL, et al. Intraductal papillary mucinous neoplasms of the pancreas: An increasingly recognized clinicopathologic entity. Ann Surg. 2001;234:313–21. doi: 10.1097/00000658-200109000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Warshaw AL, Rutledge PL. Cystic tumors mistaken for pancreatic pseudocysts. Ann Surg. 1987;205:393–8. doi: 10.1097/00000658-198704000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Le Borgne J. Cystic and intraductal tumors of the pancreas. Rev Prat. 2002;52:1540–5. [PubMed] [Google Scholar]
- 5.Galanis C, Zamani A, Cameron JL, et al. Resected serous cystic neoplasms of the pancreas: A review of 158 patients with recommendations for treatment. J Gastrointest Surg. 2007;11:820–6. doi: 10.1007/s11605-007-0157-4. [DOI] [PubMed] [Google Scholar]
- 6.Zamboni G, Scarpa A, Bogina G, et al. Mucinous cystic tumors of the pancreas: Clinicopathological features, prognosis, and relationship to other mucinous cystic tumors. Am J Surg Pathol. 1999;23:410–22. doi: 10.1097/00000478-199904000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Sarr MG, Carpenter HA, Prabhakar LP, et al. Clinical and pathologic correlation of 84 mucinous cystic neoplasms of the pancreas: Can one reliably differentiate benign from malignant (or premalignant) neoplasms? Ann Surg. 2000;231:205–12. doi: 10.1097/00000658-200002000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ryu JK, Woo SM, Hwang JH, et al. Cyst fluid analysis for the differential diagnosis of pancreatic cysts. Diagn Cytopathol. 2004;31:100–5. doi: 10.1002/dc.20085. [DOI] [PubMed] [Google Scholar]
- 9.Moparty B, Logrono R, Nealon WH, et al. The role of endoscopic ultrasound and endoscopic ultrasound-guided fine-needle aspiration in distinguishing pancreatic cystic lesions. Diagn Cytopathol. 2007;35:18–25. doi: 10.1002/dc.20558. [DOI] [PubMed] [Google Scholar]
- 10.Goh BK, Tan YM, Cheow PC, et al. Cystic lesions of the pancreas: An appraisal of an aggressive resectional policy adopted at a single institution during 15 years. Am J Surg. 2006;192:148–54. doi: 10.1016/j.amjsurg.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 11.Khalid A, Brugge W. ACG practice guidelines for the diagnosis and management of neoplastic pancreatic cysts. Am J Gastroenterol. 2007;102:2339–49. doi: 10.1111/j.1572-0241.2007.01516.x. [DOI] [PubMed] [Google Scholar]
- 12.Bhutani MS. Role of endoscopic ultrasonography in the diagnosis and treatment of cystic tumors of the pancreas. JOP. 2004;5:266–72. [PubMed] [Google Scholar]
- 13.Zhang XM, Mitchell DG, Dohke M, et al. Pancreatic cysts: Depiction on single-shot fast spin-echo MR images. Radiology. 2002;223:547–53. doi: 10.1148/radiol.2232010815. [DOI] [PubMed] [Google Scholar]
- 14.Agrawal D, Maimone SS, Wong RC, et al. Prevalence and clinical significance of pancreatic cysts associated with cysts in other organs. Dig Liver Dis. 2011;43:797–801. doi: 10.1016/j.dld.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 15.Hammel PR, Vilgrain V, Terris B, et al. Pancreatic involvement in von Hippel-Lindau disease. The Groupe Francophone d’Etude de la Maladie de von Hippel-Lindau. Gastroenterology. 2000;119:1087–95. doi: 10.1053/gast.2000.18143. [DOI] [PubMed] [Google Scholar]
- 16.Murphy BJ, Casillas J, Ros PR, et al. The CT appearance of cystic masses of the liver. Radiographics. 1989;9:307–22. doi: 10.1148/radiographics.9.2.2538868. [DOI] [PubMed] [Google Scholar]
- 17.Gaines PA, Sampson MA. The prevalence and characterization of simple hepatic cysts by ultrasound examination. Br J Radiol. 1989;62:335–7. doi: 10.1259/0007-1285-62-736-335. [DOI] [PubMed] [Google Scholar]
- 18.Carrim ZI, Murchison JT. The prevalence of simple renal and hepatic cysts detected by spiral computed tomography. Clin Radiol. 2003;58:626–9. doi: 10.1016/s0009-9260(03)00165-x. [DOI] [PubMed] [Google Scholar]
- 19.Laucks SP, Jr, McLachlan MS. Aging and simple cysts of the kidney. Br J Radiol. 1981;54:12–4. doi: 10.1259/0007-1285-54-637-12. [DOI] [PubMed] [Google Scholar]
- 20.Caremani M, Vincenti A, Benci A, et al. Ecographic epidemiology of non-parasitic hepatic cysts. J Clin Ultrasound. 1993;21:115–8. doi: 10.1002/jcu.1870210207. [DOI] [PubMed] [Google Scholar]
- 21.Pedersen JF, Emamian SA, Nielsen MB. Simple renal cyst: Relations to age and arterial blood pressure. Br J Radiol. 1993;66:581–4. doi: 10.1259/0007-1285-66-787-581. [DOI] [PubMed] [Google Scholar]
- 22.Brugge WR. Management and outcomes of pancreatic cystic lesions. Dig Liver Dis. 2008;40:854–9. doi: 10.1016/j.dld.2008.03.023. [DOI] [PubMed] [Google Scholar]


