Abstract
One of the most difficult biliary drainages is the recurrence and stenosis on afferent loop after surgery. We report an original case of hepaticogastrostomy (HGE) in a patient who had malignant stenosis of afferent loop after cephalic duodenopancreatectomy (CDP). After failure of the gastrointestinal stent, two metal self-expandable stents were placed by endoscopic ultrasound (EUS) after puncture of the dilated left hepatic duct. On clinical improvement and disappearance of jaundice, palliative chemotherapy was started.
Keywords: Afferent loop obstruction, hepaticogastrostomy (HGE), self-expandable metal stent, therapeutic endoscopic ultrasound (EUS)
INTRODUCTION
Percutaneous drainage is still considered as a first-line treatment for malignant stenosis on afferent loop. Percutaneous drainage and surgery are conventionally used.[1,2,3,4] Endoscopic ultrasound (EUS) drainage was developed since 2001 as an additional option to percutaneous drainage and endoscopic retrograde choalangiopancreatography (ERCP).[5] One of the most difficult biliary drainages is the recurrence and stenosis on afferent loop after surgery. We report an original case of hepaticogastrostomy under EUS guidance (HGE) in a patient who had malignant stenosis of afferent loop after cephalic duodenopancreatectomy (CDP).
CASE REPORT
A 71-year old man, who had a CDP in 2008, presented with febrile jaundice. Imaging examinations revealed a malignant stricture on the afferent loop, the origin of the jaundice [Figure 1]. A first attempt of drainage by the endoscopic way (gastrointestinal stent) is a failure due to inaccessible stricture. A HGE was decided. By using an interventional echoendoscope (EG 3870UTKPENTAX-HITACHI™, Hambourg, Germany), the dilated left hepatic duct (segment III) was punctured with a 19G access needle (19 G, EchoTip Access Needle, Cook™ Ireland Ltd., Limerick, Ireland). Opacification demonstrated dilated intrabiliary ducts due to the complete obstruction of the afferent loop. The needle was exchanged over a guidewire for a 6.5-Fr diathermic cystotome, used to enlarge (endocut current) the channel between the stomach and the left hepatic duct punctured. After exchange over a guidewire (TFE-coated 0.035 inch: Jagwire™, Boston, Scientific Corp, Massachussets, USA) a special partially covered metal expandable stent (Giobor© 10 cm, TaewongNiti-S™ ) was positioned (uncovered part of the stent was inserted in the left hepatic duct and covered part in the stomach). The covered part reduced the risk of biliary leakage [Figure 2]. This prevention is associated to a 7-Fr nasobiliary drain during 48 h.
Figure 1.
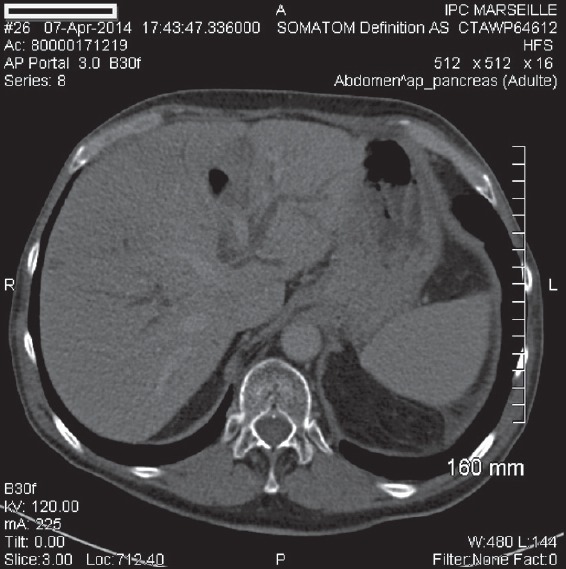
Bile ducts’ dilatation
Figure 2.
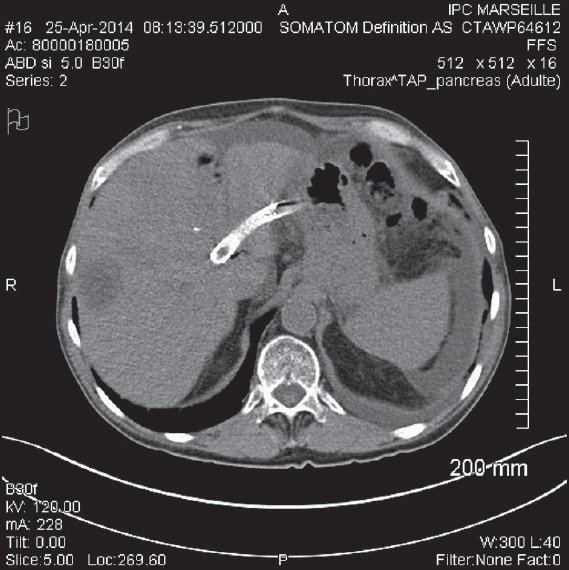
Hepaticogastric stent on computed tomography (CT) scan
Despite drainage, fever persisted and opacification by the nasobiliary drain showed poor emptying of the afferent loop. We decided to extend the stent by a novel uncovered stent from the middle part of first stent into the afferent loop [Figure 3]. At the end, contrast was emptied from the stent into the stomach. The postoperative course was uneventful with nasobiliary drain removal after 48 h and the disappearance of jaundice. A few days later, the patient was able to consult an oncologist to start palliative first-line chemotherapy.
Figure 3.
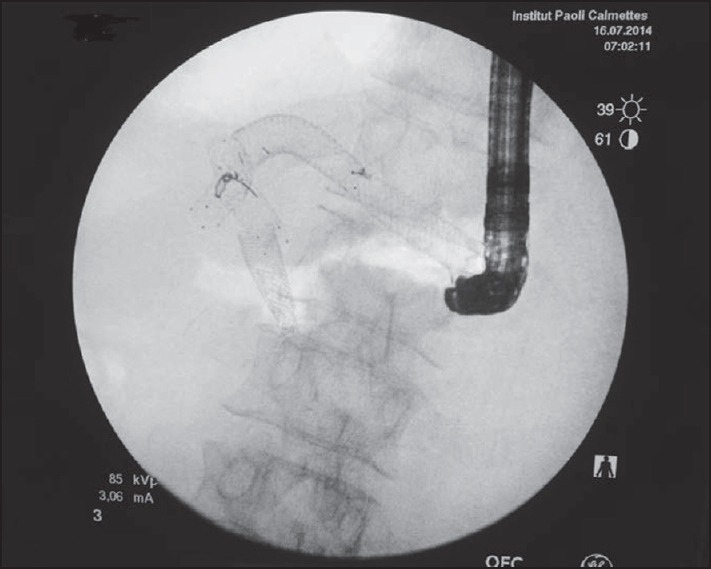
Fluoroscopic view of metal stents
The patient passed away 5 months later with evolution of the disease (relapse of pancreatic adenocarcinoma). We had to drain the right lobe at 3 months of HGE by the percutaneous way with a stent from the right lobe to the afferent loop.
DISCUSSION
In the case of jaundice due to afferent loop malignant stricture, there is not really an efficient reference procedure. The less invasive technique seems to be the gastrointestinal stent but it is not always feasible. Percutaneous drainage and surgery are already used.[1,2,3,4] Due to advanced disease (stage peritoneal carcinomatosis), surgery can be difficult and the postoperative course can often be long. Percutaneous drainage is not always easy and requires the maintenance of a drain to the skin at least temporarily. This can be uncomfortable for patients in a palliative situation.
In this case, we used a new technique. We report the first case of HGE of malignant afferent loop stricture after CDP. The postoperative course was uneventful, allowing a resumption of chemotherapy quickly. Another advantage can be easy access of the stent using a gastroscope in case of stent stricture.
Since the first publication, the technique has become safer and more standardized.[6] The procedure will continue to improve, as recent publications show.[7,8]
For us, it is a feasible and effective alternative to percutaneous treatment for patients undergoing palliative treatment. The problem remains the drainage of afferent loop through the liver to the stomach. A possible evolution could be drainage of the afferent loop directly in the stomach.
CONCLUSION
In the case of complete stricture of afferent loop with tumor recurrence, HGE by EUS appears to be feasible and effective. A randomized trial comparing different techniques’ drainage could confirm these clinical impressions but the relative rarity of this situation is a limit to a large study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chevallier P, Novellas S, Motamedi JP, et al. Percutaneous jejunostomy and stent placement for treatment of malignant Roux-en-Y obstruction: A case report. Clin Imaging. 2006;30:283–6. doi: 10.1016/j.clinimag.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 2.Aimoto T, Uchida E, Nakamura Y, et al. Malignant afferent loop obstruction following pancreaticoduodenectomy: Report of two cases. J Nippon Med Sch. 2006;73:226–30. doi: 10.1272/jnms.73.226. [DOI] [PubMed] [Google Scholar]
- 3.Hosokawa I, Kato A, Shimizu H, et al. Percutaneous transhepatic metallic stent insertion for malignant afferent loop obstruction following pancreaticoduodenectomy: A case report. J Med Case Rep. 2012;6:198. doi: 10.1186/1752-1947-6-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bakes D, Cain C, King M, et al. Management of afferent loop obstruction from recurrent metastatic pancreatic cancer using a venting gastrojejunostomy. World J Gastrointest Oncol. 2013;5:235–9. doi: 10.4251/wjgo.v5.i12.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giovannini M, Moutardier V, Pesenti C, et al. Endoscopic ultrasound-guided bilioduodenal anastomosis: A new technique for biliary drainage. Endoscopy. 2001;33:898–900. doi: 10.1055/s-2001-17324. [DOI] [PubMed] [Google Scholar]
- 6.Burmester E, Niehaus J, Leineweber T, et al. EUS-cholangio-drainage of the bile duct: Report of 4 cases. Gastrointest Endosc. 2003;57:246–51. doi: 10.1067/mge.2003.85. [DOI] [PubMed] [Google Scholar]
- 7.Park do H, Song TJ, Eum J, et al. EUS-guided hepaticogastrostomy with a fully covered metal stent as the biliary diversion technique for an occluded biliary metal stent after a failed ERCP (with videos) Gastrointest Endosc. 2010;71:413–9. doi: 10.1016/j.gie.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 8.Song TJ, Lee SS, Park DH, et al. Preliminary report on a new hybrid metal stent for EUS-guided biliary drainage (with videos) Gastrointest Endosc. 2014;80:707–11. doi: 10.1016/j.gie.2014.05.327. [DOI] [PubMed] [Google Scholar]


