A 60-year-old man presented with intermittent epigastric discomfort and postprandial vomiting. Physical exam and laboratory data were unremarkable. Computerized tomography of the abdomen [Figure 1] showed a 3.4 cm × 2.1 cm soft tissue mass in the duodenal bulb. Upper esophagogastroduodenoscopy (EGD) showed a medium-sized subepithelial mass in the duodenal apex [Figure 2]; pinch biopsies were unrevealing. Endoscopic ultrasound (EUS) showed a 27 mm × 16 mm isoechoic lesion originating from the deep mucosa and sub-mucosa without invasion to adjacent structures [Figure 3]; fine-needle aspiration (FNA): nondiagnostic. Follow-up EUS 2 years later revealed interval growth of the mass to 30 mm × 40 mm and new cystic changes [Figure 4]; repeat FNA with atypical cells. Due to the increase in lesion size, presence of atypia on cytology and persistence of symptoms, surgical resection was performed [Figure 5]. Surgical pathology showed Hyperplastic Brunner's glands (BG) with lymphoid aggregates consistent with BG adenoma (BGA) [Figure 6].
Figure 1.

Computerized tomography abdomen: Soft tissue mass in the duodenal bulb
Figure 2.

Esophagogastroduodenoscopy: Subepithelial mass in the duodenal apex
Figure 3.

Radial endoscopic ultrasound: Isoechoic lesion originating from the deep mucosa and sub-mucosa without invasion to adjacent structures
Figure 4.

Repeat radial endoscopic ultrasound exam (2 years later): Growth of the lesion, with new cystic changes
Figure 5.

Surgical pathology specimen
Figure 6.
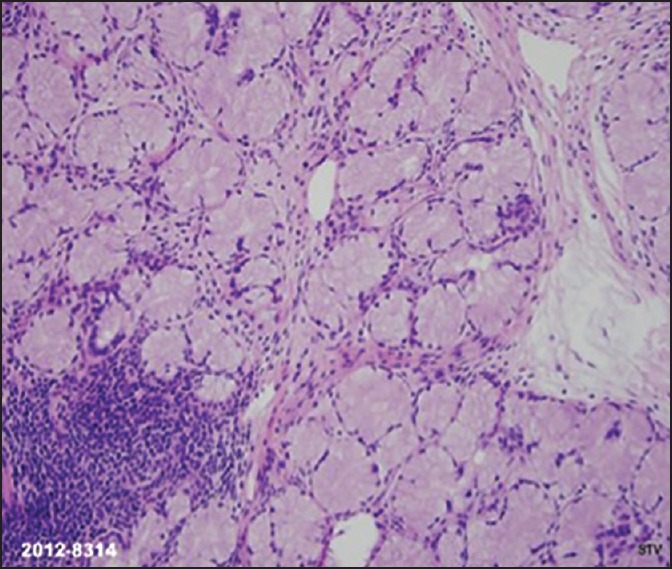
Hyperplastic Brunner's glands (BG) with lymphoid aggregates consistent with BG adenoma (H and E)
Brunner's glands are submucosal mucin-secreting glands predominantly located in the proximal duodenum. A BGA is a benign tumor arising from BG with an estimated incidence of 0.008%. It usually presents in the fifth to sixth decade of life and involves the posterior wall of the proximal duodenum. Its pathogenesis is thought to be related to acid hypersecretion.[1,2,3] Patients can be asymptomatic (11%), or more frequently have vague upper gastrointestinal symptoms. Clinical presentations may include obstructive symptoms, pancreatitis, and upper gastrointestinal bleeding.[2,4] The diagnosis of BGA can be difficult, it can be diagnosed by EGD; However, as BG proliferations may be covered with normal mucosa, pinch biopsies might be negative. Radiological findings are often nonspecific.[3] EUS can be useful to diagnose BGA; The features include: Involvement of the mucosa and submucosal layers; variable echogenicity (mixed to hypoechoic); and multiple cystic changes within the tumor.[2,3] Resection of an asymptomatic BGA is controversial. Traditionally, symptomatic BGA has been removed surgically. Endoscopic resection can be considered in smaller or pedunculated lesions in which EUS confirms only submucosal involvement. No recurrence has been reported after resection.[2,3]
Footnotes
Source of Support: Nil.
Conflicts of Interest: None declared.
REFERENCES
- 1.Rocco A, Borriello P, Compare D, et al. Large Brunner's gland adenoma: Case report and literature review. World J Gastroenterol. 2006;12:1966–8. doi: 10.3748/wjg.v12.i12.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gao YP, Zhu JS, Zheng WJ. Brunner's gland adenoma of duodenum: A case report and literature review. World J Gastroenterol. 2004;10:2616–7. doi: 10.3748/wjg.v10.i17.2616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ohba R, Otaka M, Jin M, et al. Large Brunner's gland hyperplasia treated with modified endoscopic submucosal dissection. Dig Dis Sci. 2007;52:170–2. doi: 10.1007/s10620-006-9607-1. [DOI] [PubMed] [Google Scholar]
- 4.Babich JP, Klein J, Friedel DM. Endoscopic removal of a brunneroma with EUS guidance. South Med J. 2010;103:250–2. doi: 10.1097/SMJ.0b013e3181c95727. [DOI] [PubMed] [Google Scholar]


