Abstract
Primary care providers play an important gatekeeping role in ensuring appropriate referrals to secondary care facilities. This cross-sectional study aimed to determine the level, pattern and rate of referrals from health clinics to hospitals in the public sector, and whether the placement of resident family medicine specialist (FMS) had made a significant difference.
The study was carried out between March and April in 2012, involving 28 public primary care clinics. It showed that the average referral rate was 1.56% for clinics with resident FMS and 1.94% for those without resident FMS, but it was not statistically significant. Majority of referred cases were considered appropriate (96.1%). Results of the multivariate analysis showed that no prior consultation with senior healthcare provider and illnesses that were not severe and complex were independently associated with inappropriate referrals. Severity, complexity or uncertain diagnosis of patients’ illness or injury significantly contributed to unavoidable referrals. Adequate facilities or having more experienced doctors could have avoided 14.5% of the referrals. The low referral rate and very high level of appropriate referrals could indicate that primary care providers in the public sector played an effective role as gatekeepers in the Malaysian public healthcare system.
Keywords: Referral pattern, gatekeeping, primary care, public healthcare system
Introduction
Primary care providers (PCP) play an important role as gatekeepers in the healthcare system to ensure appropriate utilisation of expensive hospital and specialist services.1 Franks2 defined gatekeeping as a process of matching patients’ needs and preferences with the judicious use of medical services as primary care physicians possess more knowledge and information than patients to make the choices. Gatekeeping also ensures equity of access where resources are limited.3
Referral patterns have significant impact on cost in a country’s healthcare system. Countries with gatekeeping systems were reported to spend less on healthcare4 while the rising cost of healthcare in the US was postulated to be partly contributed by a near double increase in physician referrals between 1999 and 2009.5 While cost is an important factor for instituting gatekeeping, it was also argued that gatekeeping is to protect patients from overtreatment, as the intensity of care and use of expensive technology in hospitals and specialty centres tend to be higher with their easy availability and this exposes patients to potential risks.2
Malaysia has long practiced a gatekeeping system in the public healthcare sector where the government is a major healthcare provider.6 Access to a specialist care in hospitals is through a referral system based on needs,7 with clear guidelines on interfacility referrals and transfer of patients.8 Specialist resources in Malaysia is still very limited, especially in the public sector with 0.9 specialist per 1000 population compared to 3–5 specialists per 1000 for some developed countries.9 Thus, there is always a concern that limited specialist resources in hospitals should be optimally utilised by appropriate referrals.
FMS were placed in the government health clinics (primary care clinics) in 1997 with the first batch of FMS coming on stream.10 With that, specialist care has been brought down to the primary care level. However, they are only available in the bigger clinics and currently, only slightly more than 20% of health clinics in the country have FMS. This additional resource should help to strengthen the gatekeeping role of primary care clinics and reduce referrals to the hospitals.
This study aimed to determine the level, pattern and rate of referrals from health clinics to hospitals in the public sector, and whether the placement of resident FMS had made a significant difference.
Methods
Setting.
Malaysia has a well structured and comprehensive network of public sector health facilities ranging from primary care clinics (health clinics) to tertiary care referral hospitals. Health clinics provide maternal and child-health service, general outpatient service and other expanded scope of primary care. The largest clinic may have up to 1000 outpatient attendances in a day, while the smallest clinic may have less than 50 patients a day. The outpatient section are managed by primary healthcare providers consisting of non-specialist doctors (medical officers) and assisted by assistant medical officers (AMOs). Bigger clinics have FMS and are better equipped with basic laboratory and radiology facilities.
Private healthcare is very active in Malaysia with private hospitals providing slightly more than a quarter of hospital beds in the country6 and a very well distributed general practitioner clinics, especially in the urban areas. Access to private healthcare is mostly through a fee-forservice system and to a lesser extent, through third party payment system.
In 2010, there were 20.586 million outpatient attendances in 553 health clinics in Peninsular Malaysia. Referrals from health clinics to Ministry of Health (MOH) hospitals totaled 586,292 giving a referral rate of 2.85% based on computation from the MOH annual report.10 This constituted 65.3% of total referrals from public primary care providers for the year, with the balance of 34.7% from private general practitioners (GPs).
Study Design.
This was a cross-sectional study involving 28 health clinics in Peninsular Malaysia, comprising equal proportions of clinics with resident or visiting (non-resident) FMS randomly selected by multi-stage sampling and stratified by four geographical regions. The regions were the Northern region (Perlis, Kedah and Pulau Pinang), Central region (Perak, Selangor and Kuala Lumpur), Southern region (Negeri Sembilan, Melaka and Johor) and East Coast region (Pahang, Terengganu and Kelantan). One state from each of these regions was randomly selected. The selected states were Pulau Pinang, Perak, Johor and Terengganu. A total of 14 public health clinics with resident FMS and 14 public health clinics with visiting FMS were further randomly selected from each of these states. Study population were all outpatient referrals (universal sampling) made by primary healthcare providers in the selected public health clinics during the study period in 1 month between March and April 2012. Neonates and referrals from maternal and child-health section of the clinics were excluded as there were clear guidelines on their referrals. A minimum of 1140 respondents were needed using Dupont and Plummer’s Power and Sample size calculator,12 with an estimated referral rate of 2 and 4% for clinics with and without resident FMS (estimated based on national referral rate of 2.8%) at 95% confidence level with a power of 80% accuracy.
Medical officers-in-charge (MOic) of the clinics were briefed centrally on the study and the process of data collection. They were responsible for data collection in the clinics. There was no selection of favourable referrals by the MOic as all referrals were sampled (universal sampling), so there was no selection bias. Referrals were not screened by the MOic. The primary healthcare provider who made the referrals completed the forms before the MOic collected the completed forms. Answers were taken at face value, and missing data were retrieved by contacting the MOic of the clinic where the referral was made.
Details of all the referrals made during the study period were transcribed into a pretested structured format by the referring doctor or AMO. In addition, profile of each participating clinics was obtained separately.
Two forms were used. Survey Form A collected information on the clinic profile such as name of clinic, location, state, presence of resident or visiting FMS, availability of laboratory and imaging support, total number of outpatients during the study period, and details of the contact person in the clinic. Survey Form B collected information on the referral details such as date and time when the referral was made, diagnosis, co-morbidity, type of cases being referred (e.g., medical/surgical/paediatric/ orthopaedic/psychiatry/ENT/ophtalmology/ rehabilitation), job designation of the person who referred, availability of FMS on day of referral, reason for referral (nature of illness: complexity, severity of illness requiring admission, uncertain diagnosis requiring further investigation, special circumstances like disease outbreak, accident, multiple casualties, and on request by patient or family).
The referring personnel was also asked: if they had consulted a senior health provider; if they would still make a referral if they were able to consult the specialist directly or by telephonic communication; and if they were able to manage the patient at the clinic if support services/facility/drug were available.
Years of service of MOs and AMOs was obtained from the participating clinics directly based on the list of MOs and AMOs working in the clinic during the study period. For MOs, it was from the time they become medical officers, after housemanship training. For AMOs, it was the year of service after training.
FMS must be physically present at the clinic. Any consultations through phone calls when the FMS was not physically present at the clinic was considered as ‘FMS not available’.
The assessment of severity and complexity of illness were made according to the capability of the attending healthcare provider, that is, either doctor or AMO, and therefore there was no standardised definition of severity and complexity of illness.
Laboratory facilities like haematology machine, chemistry analyser, in addition to basic laboratory tests such as glucostix, urine dipstick and stool full examination, microscopic examination (FEME) were available. Unavailability of plain X-Ray was considered as not having imaging facility.
A pilot study was done on April 11, 2011 at Kelana Jaya Health Clinic in which 7 referrals were made out of 684 patients and the referral rate was 1.02%. The questionnaire was revised and retested on 26–28 July 2011 at Kelana Jaya Health Clinic and the findings were 27 referrals made out of 2773 patients and the referral rate was 0.97%. The survey forms were compiled at the clinic by the MOic and sent to the principal investigator where it was coded and anonymised. All the data were then transcribed and sent to individual FMS for independent assessment of appropriateness and avoidance of the referrals. Data with differences in assessment were corrected by consensus through face-to-face meeting. Data quality was checked by using Kappa’s Measure of Inter-rater Agreement.
After deciding on the appropriateness of referrals, additional information was sought for 103 cases where a clear decision could not be made due to inadequate information. The necessary information needed for each of these cases were sought from the clinic concerned as the patient’s name, IC number and date of referral were available.
The demographic and clinical profile of all the referrals were tabulated including the profiles of officers who made the referral, reasons for referral, presence of FMS on day of referral, and whether there was prior consultation before a referral. The tabulations were printed out and reviewed by a panel of three senior FMS. These three senior FMSs act as the reviewers to determine whether a referral was appropriate or inappropriate, and whether it was avoidable or not avoidable using a broad definition. The senior FMSs had 20–25 years of working experience and worked in primary care for 17–22 years including 12–15 years as a FMS. They qualified as FMS after obtaining postgraduate degrees in MMed (Fam Med) and further received training in various subspecialities. The FMSs were blinded for the type of clinics and the name of the referring personnel. However, the years in service of the referring doctors/primary care providers were known to the FMSs assessing the appropriateness of referrals.
A referral was Appropriate if the referral was reasonable and necessary based on the overall patient’s condition, reason for referral and the capacity of the person making the referral or the facilities available in the clinic to manage such patients. It was Not Appropriate if the referral was deemed not reasonable or necessary.
Avoidable referral meant that there was a potential to remove the obstacle(s) hindering patient’s management at the clinic. This could be by having more senior/experienced officer, accessible consultation support from a more senior officer/specialist either from the clinic or the intended referring hospital, or access to necessary laboratory/imaging service/ drugs/treatment facilities without having to transfer the care of the patient to the hospital. Indeterminate was when it was not possible to determine the appropriateness or avoidance of a referral from the data gathered in the questionnaire.
Data analysis.
Initially assessment was done independently and differences were corrected by consensus in a face-to-face meeting subsequently. Additional information was sought via e-mail to the relevant clinic, where possible. If there was still a lack of clinical information to make decision after the additional information was obtained, the case was classified as indeterminate.
Obtaining agreement between the three reviewers in determining appropriateness of referral and whether a referral was avoidable or not, proved most problematic. Initial attempt with independent assessment showed a very low degree of agreement (kappa’s coefficient < 0.200). However, after several rounds of clarifications and examples of various possible scenario as a guide, it lead to better agreement with kappa value increasing to between 0.400 and 0.662 for Appropriateness and 0.393–0.701 on Avoidance between the three panel reviewers based on a sample study of 10% of the cases (140 cases). Thereafter, assessment was conducted together through consensus using the new understanding with the majority view as the outcome.
Average referral rates were based on referral rates of each of the clinics, and not based on total number of referrals against total number of outpatients. Hence, n = number of clinics, while Average means = (sum of rates of each clinic in the group)/n.
Data collected were analysed using IBM SPSS Statistics version 20.0. Referral characteristics were analysed, while referral rates were compared against various clinic characteristics using non-parametric Mann–Whitney U-test. Reasons for referral were compared between clinics with and without resident FMS using Pearson’s Chi Square test. Avoidable and inappropriate referrals were further analysed and compared to determine significant factors influencing such differences. This study had the approval of the Ministry of Health’s Medical Ethics Committee.
Results
A total of 1,380 referrals from 28 health clinics were analysed with an overall average referral rate of 1.76% for all clinics. It was 1.56% for clinics with resident FMS and 1.94% for clinics with visiting FMS but the difference was not statistically significant. The average referral rates for clinics without imaging facilities and laboratory facilities were also higher (1.34% and 1.46% versus 1.87% and 1.93%, respectively), but not statistically significant (Table 1).
Table 1. Average referral rates by clinic characteristics.
| Variable | Description | No. Clinics (%) | No. of Patients | No. of Referrals | Mean Referral Rate(%/SD) | p-value* |
|---|---|---|---|---|---|---|
| Referral Rate | All Clinics | 28 (100) | 89698 | 1380 | 1.76 (0.86) | - |
| Northern Region | 27680 | 342 | 1.40 (0.60) | |||
| Central Region | 21379 | 415 | 2.02 (0.63) | |||
| Southern Region | 21498 | 237 | 1.34 (0.89) | |||
| East Coast Region | 19141 | 386 | 2.28 (1.03) | |||
| Type of clinic | Resident FMS | 14 (50) | 53187 | 765 | 1.56 (0.75) | 0.289 |
| Visiting FMS | 14 (50) | 36511 | 615 | 1.94 (0.94) | ||
| Availability of Imaging Facility | Yes | 6 (21.4) | 1.34 | 0.208 | ||
| No | 22 (78.6) | 1.87 | ||||
| Availability of Lab. Facility (biochemistry tests) | Yes | 10 (35.7) | 1.46 | 0.221 | ||
| No | 18 (64.3) | 1.93 |
n=28
* Mann-Whitney U test
There was no significant difference in the reasons for referrals between clinics with resident FMS and visiting FMS under patients’ medical conditions, except for requests by patients and their families, which was higher in clinics without resident FMS (67.1% versus 32.9%, p < 0.001). Under limitation of facilities, referrals were higher in clinics without resident FMS for nonavailability of diagnostic imaging facilities (55.9% versus 44.1%, p = 0.001) while nonavailability of treatment facilities was a factor contributing to higher referrals for clinics with resident FMS (79.3% versus 20.7%, p < 0.001, Table 2).
Table 2. Reasons for referrals among health clinics with resident and visiting Family Medicine Specialists (FMS) (N=1380).
| Reason for Referral* | No. of cases | Proportion of all referrals | Health Clinics | P-value** | |
|---|---|---|---|---|---|
| Resident FMS | Visiting FMS | ||||
| I. Nature of Illness | |||||
| a) Severity of illness | 461 | 33.4% | 59.0% | 41.0% | 0.059 |
| b) Complexity of illness | 619 | 44.9% | 54.1% | 45.9% | 0.375 |
| c) Uncertain diagnosis | 342 | 24.8% | 53.5% | 46.5% | 0.409 |
| d) Request by patient/ family | 79 | 5.7% | 32.9% | 67.1% | < 0.001 |
| II. Non-Availability of Support Facilities or Services | |||||
| a) Test not available | 50 | 3.6% | 52.0% | 48.0% | 0.619 |
| b) Imaging facility not available | 195 | 14.1% | 44.1% | 55.9% | 0.001 |
| c) Drug not available | 45 | 3.3% | 62.2% | 37.8% | 0.352 |
| d) Treatment facilities not available | 145 | 10.5% | 79.3% | 20.7% | < 0.001 |
* Reason for referral could be more than one; ** Chi-square test
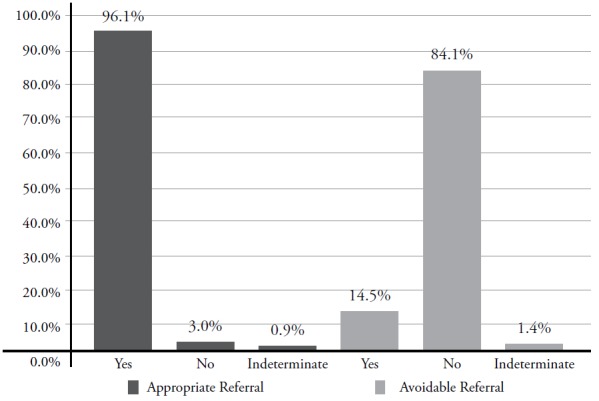
Almost all cases referred were deemed appropriate (96.1%) for the level and capability of personnel who made the referral and resources available at the clinics to support patient care. Only 14.5% (200 cases) could have been avoided if there were adequate facilities or more experienced medical officers at the clinics. A small proportion of the cases, were indeterminate from the available information captured in the questionnaire (Figure 1).
Figure 1: Appropriateness and avoidability of referrals.
Avoidable referrals were not significantly influenced by the status of whether a clinic had resident or visiting FMS, or whether FMS was present when the referral was made. There was also no significant difference in avoidable referrals made either by a medical officer or an AMO. However, referrals were more likely to be avoidable if there had been prior consultation before referral (p < 0.001); while more avoidable referrals were made by junior health care providers with less than 1 year experience (Table 3). Condition of patients’ illness or injury (severity, 93.2%; complexity, 88.5% and uncertain diagnosis, 80.5%) significantly contributed to referrals being unavoidable (p < 0.001; p = 0.003 and p = 0.004, respectively). Requests for referral by patients and their families, unavailability of imaging facilities and drugs were also significant in contributing to avoidable referrals (p = 0.032, p < 0.001 and p < 0.002, respectively, Table 3).
Table 3. Avoidable and non-avoidable cases referrals according to variables.
| Variable | Circumstances | Referral | P-value* | |
|---|---|---|---|---|
| Avoidable (%) | Not Avoidable (%) | |||
| Health Clinic | With Resident FMS (754) | 15.6 | 84.4 | 0.273 |
| With Visiting FMS(606) | 13.5 | 86.5 | ||
| FMS available during referral | Available (304) | 15.1 | 84.9 | 0.749 |
| Not available (1042) | 14.4 | 85.6 | ||
| Consulted senior health carev provider before referral | Consulted (306) | 7.2 | 92.8 | < 0.001 |
| Not consulted (1047) | 16.9 | 83.1 | ||
| Years in service (MOs and AMOs) | < 1 year (49) | 20.4 | 79.6 | 0.031 |
| 1- 2 years (216) | 14.4 | 85.6 | ||
| 3- 5 years (435) | 14.9 | 85.1 | ||
| 6- 10 years (246) | 16.7 | 83.3 | ||
| > 10 years (211) | 7.6 | 92.4 | ||
| Severity of illness | Severe (455) | 6.8 | 93.2 | < 0.001 |
| Not severe (905) | 18.7 | 81.3 | ||
| Complexity of illness | Complex (608) | 11.5 | 88.5 | 0.003 |
| Not complex (752) | 17.3 | 82.7 | ||
| Diagnosis | Certain diagnosis (338) | 19.5 | 80.5 | 0.004 |
| Uncertain diagnosis(1022) | 13.1 | 86.9 | ||
| Request by patient/family | Yes (78) | 23.1 | 76.9 | 0.032 |
| No (1282) | 14.2 | 85.8 | ||
| Laboratory facility | Available(1310) | 14.4 | 85.6 | 0.059 |
| Not available (50) | 24.0 | 76.0 | ||
| Imaging facility | Available (1166) | 13.4 | 86.6 | <0.001 |
| Not available (194) | 22.7 | 77.3 | ||
| Drug facility | Available (1315) | 14.1 | 85.9 | 0.002 |
| Not available (45) | 31.1 | 68.9 | ||
| Treatment facility | Available (1216) | 14.1 | 85.9 | 0.090 |
| Not available (144) | 19.4 | 80.6 | ||
* Chi-square test
Results of the multivariate analysis are detailed in Table 4. Absence of consultation with senior health care provider and illness which was not severe and complex was independently associated with inappropriate referrals.
Table 4. Inappropriateness of referral cases according to variables.
| Variable | Circumstances | Inappropriateness | P-value* | |
|---|---|---|---|---|
| AOR | CI | |||
| Health Clinic | With Resident FMS (757) | 1 | 0.055 | |
| With Visiting FMS (610) | 0.46 | 0.21-1.02 | ||
| FMS available during referral | Available (304) | 1 | 0.639 | |
| Not available (1049) | 0.80 | 0.32-2.00 | ||
| Consulted senior health carev provider before referral | Consulted (307) | 1 | 0.033 | |
| Not consulted (1053) | 8.87 | 1.20 - 65.88 | ||
| Years in service (MOs and AMOs) | < 1 year (49) | 1 | ||
| 1-2 years (221) | 0.91 | 0.15-5.53 | 0.917 | |
| 3-5 years (436) | 0.77 | 0.13-4.47 | 0.770 | |
| 6-10 years (246) | 0.65 | 0.11-3.92 | 0.635 | |
| > 10 years (211) | 0.45 | 0.07-3.05 | 0.415 | |
| Severity of illness | Severe (458) | 1 | 0.002 | |
| Not severe (909) | 6.89 | 1.99-23.87 | ||
| Complexity of illness | Complex (614) | 1 | 0.023 | |
| Not complex (753) | 2.40 | 1.13-5.13 | ||
| Diagnosis | Uncertain diagnosis(339) | 1 | 0.674 | |
| Certain diagnosis (1028) | 1.25 | 0.44-3.61 | ||
| Request by patient/family | Yes (78) | 1 | 1 | 0.922 |
| No (1289) | 0.93 | 0.23-3.75 | ||
| Laboratory facility | Not available(50) | 1 | 0.352 | |
| Available (1317) | 0.46 | 0.09-2.36 | ||
| Imaging facility | Not available (194) | 1 | 0.076 | |
| Available (1173) | 3.80 | 0.87-16.57 | ||
| Drug facility | Not available (45) | 1 | 0.998 | |
| Available (1322) | 5.267 | 0.00 | ||
| Treatment facility | Not available (145) | 1 | 0.876 | |
| Available (1222) | 1.09 | 0.37-3.21 | ||
Discussion
Many studies have shown wide variations in referral rates which are contributed by various factors.13–17 Literature reviews by O’Donnell13 on variations in GP referral rates ranged from a mean of 24 to 66 per 1000 consultations for 13 of the studies quoted. The variations were attributed to four factors—patient characteristics, practitioner, practice characteristics as well as case mix. Forrest18 found that patient determinants, which include clinical conditions, as the main deciding factor, while other contributing factors include physician behavior and healthcare system determinants like practice size, payment mechanism and degree of managed care in the system.
Compared to most studies quoted, referral rate in this study was relatively low at 17.6 per 1000 outpatient attendances. Unlike GP practice, health clinics in Malaysia are polyclinics providing comprehensive services and are equipped with basic diagnostic facilities. However, this was still lower than the national referral rate of 28.5 per 1000, which included maternal and neonatal referrals (excluded in this study). The referral rate could be higher as there was a possibility that some referrals might not have been reported in the survey. Although clinics with resident FMS had lower referral rates, the lack of statistical difference in the findings could be due to sample size constraint for the small difference encountered.
Nevertheless, the low referral rate could be a reflection of an effective public sector primary care system and its gatekeeping role through a referral system, which need to be investigated further. However, this does not prevent patients from using other alternative ways to access hospital care like getting referrals through private GPs who are not bound by the Ministry’s referral policy. Some by-pass the system and self-refer through the hospital emergency department. For the private sector, there is no gatekeeping and patients go direct to specialists in a fee-for-service system.
In this study, appropriateness was based on clinical necessity from the referrer’s perspective, and did not take into consideration outcome. This definition was rather subjective as every case had to be weighed against three perspectives—patient’s condition and clinical need, referring doctor’s capacity by the level of formal training received, as well as the capacity of the clinic in terms of resources available to manage patients.
Donohoe’s study used an equally broad and subjective definition for Appropriateness under the conditions of (i) patient’s problem definitely requires the skills and knowledge of a specialist, (ii) failure to refer might be construed as malpractice using a Likert scale of 1–9.19 Thom et al. developed an appropriateness measuring tool (APCSS— Appropriateness of 14 Primary Care Service Scale) for referral, and found that inter-rater agreement was only fair, with kappa coefficient ranging from 0.15 to 0.38 for the individual criteria and overall agreement of 0.40–0.41. The study used three criteria to measure appropriateness, namely clinically indicated, to the correct specialist timely, and considering risk to benefit.20
It appears that there is a lack of consensus on what constitutes an appropriate referral. Decisions on referral were said to be complex and the result of many interacting factors, making it difficult to reach consensus on what is appropriate. Its interpretation is context dependent, and also varies depending on the perspective of the referring doctor, receiving doctor or patients’21. Blundell (2010)22 derived three attributes of referral appropriateness from interviews with senior staff of clinical and non-clinical backgrounds. These were clinical necessity, appropriateness of destination and quality of cases referred; one of which was having all necessary tests and investigations carried out before a referral was made.
This study found that only 3% of the referrals were inappropriate. This could be either because the referring doctors or AMOs were discerning, or more likely, it was because the criteria for appropriateness were too encompassing. However, avoidable referrals were much higher at 14.5% and could have been averted if the clinics had better support facilities or services. Prior consultation with FMS or senior colleagues could have further reduced 16.9% of avoidable referrals and was an effective strategy to improve referrals. A high level of appropriate referrals was also seen in two studies which reported an appropriate referral rates of 90.4% and 90.6% respectively, based on receiving specialists’ evaluation of referrals.23,24
However, Elwyn and Scott25 found a much lower level of appropriate level at 65% with a third of the referrals considered theoretically avoidable if adequate resources were available.
Referral rates between clinics with resident and with visiting FMS were not statistical different. It was likely that availability of FMS alone might not be adequate to prevent referrals to the hospitals as they require support facilities to diagnose and manage more complex conditions in the clinics. The majority of referrals made were due to the severity and complexity of illness or injury which could not be managed in the clinic and hence, not avoidable. Referrals can further be avoided if the primary healthcare providers are better trained to diagnose and manage more severe and complex diseases. The effect of current health promotion and prevention activities may minimise the severity of disease at first presentation, but whether it contribute to the reduction of referrals in the future is yet to be ascertained. Referrals can also be potentially be reduced by improving diagnostic and treatment facilities in the clinics. Basic eye and ENT equipment would allow some eye and ENT cases being managed in the clinics. A dedicated multi-purpose and properly equipped procedure room would enable small surgical procedures to be carried out under local anaesthesia. This would certainly enhance accessibility to better and more timely healthcare for patients.
While gatekeeping may be good to ensure judicious use of limited resources, it is also equally important to ensure patients who need higher level of care are not being deprived. The level of referral on request by patient or family was low at 5.7% in this study compared to 13.6% by Forrest et al. in the US26 and 19.2% by Rosemann et al. in Germany.24 This could be due to the fact that patients in Malaysia, in particular those using public healthcare facilities, are not as assertive or demanding. Deciding whether to refer or not to refer, and hence gatekeeping, is a complex balance of priorities—from the health system, physician and patient’s perspective.
A Cochrane review on interventions to improve patient referrals found that among the various strategies adopted in different studies, the most likely effective strategy was having clear referral guideline and a standard format for referral, in addition to having senior healthcare professionals involved in teaching about appropriate referrals.27
The limitations of this study are having only FMSs to judge the referrals. The involvement of hospital specialists to assess the referrals may provide another perspective as they are at the receiving end and may have different views of the referrals. Objective reports of the nature of illness and verification of pertinent information in the Survey Form B by another person such as the MOic may further improve the validity of the study finding.
This study’s finding of a low referral rate with very high level of appropriate referrals from health clinics to hospitals in Malaysia as judged from the perspective of the FMSs as the main clinical stakeholders of the public health clinics, could indicate that primary care providers in the public sector have been able to play their gatekeeping role in controlling referrals to hospitals.
Further study is needed to determine the reason for this study’s finding of no significant difference between clinics with resident FMS and clinics with visiting FMS. Provision of appropriate diagnostic and treatment facilities, especially minor procedure room in bigger clinics could further reduce referrals to hospitals.
Acknowledgements
The authors wish to thank the Deputy Director General of Health (Research and Technical Support) for her permission to undertake this study, the participating clinics for their kind cooperation and the Director General of Health Malaysia, for approving the publication of this study.
Footnotes
Funding
The Ministry of Health allocation on research development.
Conflicts of interest
None.
Ang KT, Ho BK, Mimi O, Salmah N, Salmiah MS, Noridah MS. Factors influencing the role of primary care providers as gatekeepers in the Malaysian public healthcare system. Malays Fam Physician. 2014;9(3):2-11.
References
- 1.Gross R, Tabenkin H, Brammli-Greenberg S. Gatekeeping: A challenge in the management of primary care physicians. J Manag Med. 2001;15(4-5):283–98. doi: 10.1108/02689230110403795. [DOI] [PubMed] [Google Scholar]
- 2.Franks P, Clancy CM, Nutting PA. Gatekeeping revisited-protecting patients from overtreatment. N Engl J Med. 1992;327(6):424–9. doi: 10.1056/NEJM199208063270613. [DOI] [PubMed] [Google Scholar]
- 3.Forrest CB. Primary care gate keeping and referrals: Effective filter or failed experiment? BMJ. 2003;326(5):692. doi: 10.1136/bmj.326.7391.692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Velasco Garrido M, Zentner A, Busse R. The effects of gatekeeping: A systematic review of the literature. Scand J Prim Health Care. 2011;29(1):28–38. doi: 10.3109/02813432.2010.537015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barnett ML, Song ZR, Landon BE. Trends in physician referrals in the United States, 1999–2009. Arch Intern Med. 2012;172(2):163–70. doi: 10.1001/archinternmed.2011.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ministry of Health Malaysia, Planning and Development Division. Health Facts, 2012. Available from: http://www.pnd.moh.gov my. Accessed on June 15, 2013.
- 7.Hanafiah J. Public health care provisions: Access and equity. Soc Sci Med. 1996;43(5):759–68. doi: 10.1016/0277-9536(96)00120-7. [DOI] [PubMed] [Google Scholar]
- 8.Office of Director General of Health, Ministry of Health Malaysia. Guideline on patient referral and transfer between hospitals. Director General’s circular No. 2/2009, May 2009. Available from: http://www.moh.gov.my/circulars. [Google Scholar]
- 9.World Health Organization, Global Atlas of the Health Workforce. Physician per 1000 population, 2010. Available from: http://apps.who.int/globalatlas/Accessed on January 21, 2013. [Google Scholar]
- 10.Ministry of Health Malaysia. Family medicine service in chapter 2, health service development, Malaysia’s health 2002. Technical report of the Director General of Health Malaysia. 2002 [Google Scholar]
- 11.Ministry of Health Malaysia. Outpatient attendances—new and total for health clinics (PER-PL211), and outpatient attendances at government hospitals by primary source of referrals (PER-PL205) HMIS Annual Report, Medical-Care Subsystem, 2010 [Google Scholar]
- 12.Dupont WD, Plummer WD. Power and sample size calculation version 3.0, 2009. Available from: http://biostat.mc.vanderbilt.edu/ [Google Scholar]
- 13.Delnoij DM, Spreeuwenberg PMM. Variations in GP referral rates to specialists in internal medicine. Eur J Pub Health. 1997;7(4):427–35. [Google Scholar]
- 14.O’ Donnell CA. Variations in GP referral rates : what can we learn from the literature? Fam Pract. 2000;17(6):462–71. doi: 10.1093/fampra/17.6.462. [DOI] [PubMed] [Google Scholar]
- 15.Franks P, Zwanziger J, Mooney C. Variations in Primary Care Physician referral rates. Health Serv Res. 1999;34(1):323–9. [PMC free article] [PubMed] [Google Scholar]
- 16.Moore AT, Roland MO. How much variation in referral rates among general practitioners is due to chance? BMJ. 1989;298:500–2. doi: 10.1136/bmj.298.6672.500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Noone A, Goldacre M, Coulter A. et al. Do referral rates vary widely between practices and does supply of services affect demand? A study in Milton Keynes and the Oxford region. J R Coll Gen Pract. 1989;39(327):404–7. [PMC free article] [PubMed] [Google Scholar]
- 18.Forrest CG, Nutting PA, Schrader S. et al. Primary care physicians’ speciality referral decision making: Patient, physician and healthcare system determinants. Med Decis Mak. 2006;26(1):76–85. doi: 10.1177/0272989X05284110. [DOI] [PubMed] [Google Scholar]
- 19.Donohoe MT, Kravitz RL, Wheeler DB. et al. Reasons for outpatient referrals from generalists to specialists. Gen Intern Med. 1999;14(5):281–6. doi: 10.1046/j.1525-1497.1999.00324.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thom DH, Kravitz RL, Kelly-Reif S. et al. A new instrument to measure appropriateness of services in primary care. Int J Qual Health Care. 2004;16(2):133–4. doi: 10.1093/intqhc/mzh029. [DOI] [PubMed] [Google Scholar]
- 21.Coulter A. Managing demand at the interface between primary and secondary care. BMJ. 1998;316:1974–6. doi: 10.1136/bmj.316.7149.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blundell N, Clarke A, Mays N. Interpretations of referral appropriateness by senior health managers in five PCT areas in England: A qualitative investigation. Qual Saf Health Care. 2010;10:182–6. doi: 10.1136/qshc.2007.025684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fertig A, Roland M, King H. et al. Understanding variations in rates of referral among general practitioners: are inappropriate referrals important and would guidelines help to reduce rates? BMJ. 1993;307:1467–70. doi: 10.1136/bmj.307.6917.1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rosemann T, Rüter G, Wensing M. et al. Referrals from primary to secondary care. Dtsch Arztebl. 2006;103(37):A2387–92. [translated from German]. Available from www.aerzteblatt.de/pdf/DI/103/37/a2387e.pdf. [Google Scholar]
- 25.Elwyn GJ, Stott NCH. Avoidable referrals? Analysis of 170 consecutive referrals to secondary care. BMJ. 1994;309:576–8. doi: 10.1136/bmj.309.6954.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Forrest CB, Majeed A, Wiener JP. et al. Comparison of specialty referral rates in the United Kingdom and United States: Retrospective cohort analysis. BMJ. 2002;325:370–1. doi: 10.1136/bmj.325.7360.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Akbari A, Mayhew A, Al-Alawi MA. et al. Interventions to improve outpatient referrals from primary care to secondary care. Cochrane Database Syst Rev. 2008;(4) doi: 10.1002/14651858.CD005471.pub2. CD005471. doi: 10.1002/14651858.CD005471.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]


