Abstract
Coronary angiography can be a high-risk condition for the incidence of contrast-induced nephropathy (CIN) in elderly patients. Reduced glutathione, under a variety of mechanisms, may prevent CIN in this procedure. We prospectively examined whether hydration with reduced glutathione is superior to hydration alone for prevention of CIN in an elderly Han Chinese population. A total of 505 patients (271 males and 234 females) aged 75 years or older who underwent non-emergency coronary angiography or an intervention were randomly divided into two groups. The treatment group received hydration with reduced glutathione (n=262) and the control group received hydration alone (n=243). Serum creatinine and blood urea nitrogen levels were measured prior to coronary angiography and 48 h after this procedure. The primary endpoint was occurrence of CIN, which was defined as 25% or 44.2 µmol/L above baseline serum creatinine levels 48 h after the procedure. The overall incidence of CIN was 6.49% in the treatment group and 7.41% in the control group, with no significant difference between the groups (P=0.68). In subgroup analysis by percutaneous coronary intervention, no significant differences were found between the two groups. In summary, reduced glutathione added to optimal hydration does not further decrease the risk of CIN in elderly patients undergoing coronary angiography or an intervention.
Keywords: Contrast-induced nephropathy; Reduced glutathione; Randomized, controlled trial
Introduction
Contrast-induced nephropathy (CIN) is one of the complications of contrast media, which are used in diagnostic and interventional cardiology procedures. CIN is recognized as an important clinical problem following coronary angiography and percutaneous coronary intervention (PCI) in recent years. Therefore, an increase in the incidence of CIN has resulted in it being the third most common cause of hospital-acquired acute kidney injury ( 13).
Effective prophylactic and therapeutic regimens for decreasing the incidence of CIN are limited. Therefore, additional strategies are urgently required. However, except for intravenous hydration, the optimal strategy for preventing CIN remains uncertain ( 46). Because oxidative stress has been implicated as a contributing factor in the etiology of CIN ( 79), use of a potent antioxidant as a nephroprotective agent is logical. Reduced glutathione, under a variety of mechanisms, may prevent CIN. Limited information is available about the potential preventive benefits of reduced glutathione for CIN in the elderly Han Chinese population. Therefore, we prospectively examined whether hydration with reduced glutathione is superior to hydration alone for prevention of CIN in a randomized, controlled trial.
Material and Methods
Study population
This study was carried out at Huashan Hospital, Fudan University between February 2012 and January 2014. Eligibility for the study was defined as patients aged ≥75 years and those who had an estimated glomerular filtration rate ≥60 mL/min/1.73 m2 who underwent non-emergency coronary angiography or intervention. Exclusion criteria were acute myocardial infarction, congestive heart failure, and hemodynamic instability during the procedure. A total of 505 patients (271 males and 234 females) aged 75 years or older were eligible. The ethics review board of Huashan Hospital approved the study protocol, and written informed consent was obtained from all participants in the study.
Study design
This was a non-blinded, randomized, controlled clinical trial among the Han population aged 75 years or older. Consecutive eligible patients were randomly allocated to 2 groups: patients receiving saline plus reduced glutathione (n=262) or saline alone (n=243). Randomization was based upon computer-generated randomization numbers. No placebo was used in this randomized, controlled, clinical trial. The hydration protocol consisted of 1 mL/kg per h of saline for 6 h prior to, during, and 6 h after the procedure. Reduced glutathione (Shanghai Fudan Forward S&T Co., Ltd, China) was administered at the dosage of 2400 mg in saline on the day of the procedure. All of the patients received a non-ionic, iso-osmolar contrast agent (Shanghai Bracco Sine Pharmaceutical Co., Ltd, China) during the procedure. Serum creatinine and blood urea nitrogen levels were measured prior to the procedure and 48 h after the procedure by the same technician in the same laboratory. Paraclinical evaluations were performed in a single hospital laboratory, and laboratory staff were blinded to the study protocol. The primary endpoint of the study was the occurrence of CIN, which was defined as a minimum of 0.5 mg/dL or 25% increase in serum creatinine levels above the baseline 48 h after exposure to contrast media.
Statistical analysis
Continuous variables with normal distribution are reported as means±SD. Comparisons between the two groups were performed by the Student’s t-test. Data analysis was performed with SPSS 12.0. P<0.05 was considered to be significant.
Results
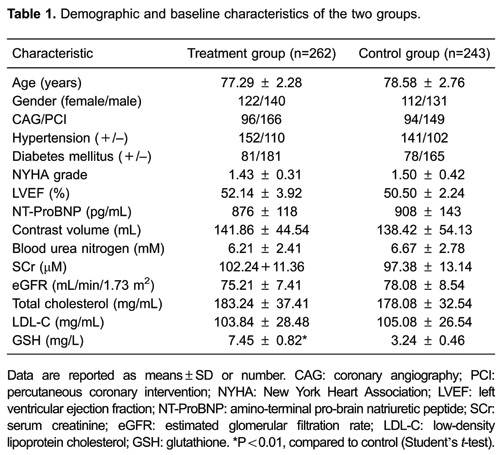
Demographic data of the patients are summarized in Table 1. The two study groups were generally similar in demographic and baseline characteristics.
The estimated glomerular filtration rate was not significantly different between the treatment group (72.08±8.31 mL/min/1.73 m2) and the hydration group (74.63±9.55 mL/min/1.73 m2, Table 2, P=0.64). Similarly, serum creatinine and blood urea nitrogen levels were not significantly different between the two groups after exposure to contrast media.
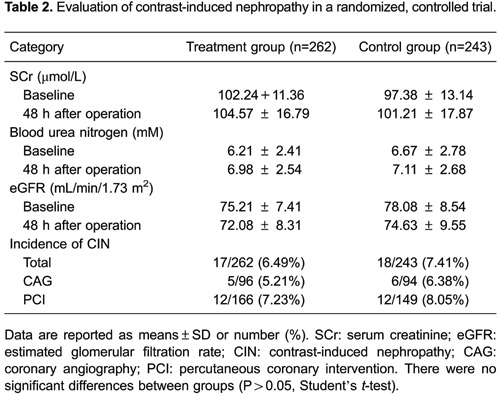
The overall incidence of CIN was 6.93% (35/505) in the Han population aged 75 years or older who underwent coronary angiography or intervention. The incidence of CIN was similar in both groups (6.49% [17/262] in the treatment group versus 7.43% [18/243] in the control group, P=0.68). In subgroup analysis by PCI, no significant differences were found between the two groups (Table 2). No patients required renal replacement therapy during or after the study. There was no mortality in either group during hospitalization.
Discussion
The main finding of our study was that, although reduced glutathione tended to reduce the occurrence of CIN, this reduction was not significant in elderly patients. Our clinical trial is the first study on the role of reduced glutathione in prevention of CIN in a Han population aged 75 years or older. The patients’ demographic data and baseline risk factors for CIN were similar in the two groups. The overall incidence of CIN is consistent with previous studies in which saline hydration was used as a preventive measure (10,11). Therefore, the lower incidence of CIN with hydration compared with its incidence in medically unprotected conditions is due to the effective hydration protocol.
The pathophysiology of CIN is unclear. Contrast-induced renal dysfunction appears to be due to a reduction in renal blood flow and direct tubular epithelial toxicity (12,13). As a potent antioxidant, reduced glutathione may counteract various pathological mechanisms underlying CIN (14,15). Additionally, glutathione can reduce inflammation, inhibit oxidative stress reactions, and protect the kidney from injury due to complement activation (16,17).
Results of previous studies are controversial regarding the preventive effects of reduced glutathione against CIN (18,19). We found no protective effect of reduced glutathione on serum creatinine levels after contrast material injection. Notably, the present study was conducted on elderly patients with a normal renal function who underwent coronary angiography or intervention.
Even minimal changes in post-procedural serum creatinine levels are associated with increased mortality in patients undergoing coronary angiography (20). Although these changes may be clinically subtle in terms of manifestations, they may signify a great decline in renal function in elderly patients. In the current trial, serum creatinine was studied in both groups. No significant difference in serum creatinine levels was observed between the groups in this study.
Some limitations of our study should be acknowledged. First, the trial was a single-center study, which may reduce its generalizability. Second, the small sample size may have impaired the statistical power of the study in detecting a difference between the groups. Significance might be achieved in larger populations. Third, we did not measure markers of oxidative stress in the present study because of the high cost involved. Finally, short-term administration of hydration with reduced glutathione resulted in a low rate of events in elderly patients with a normal renal function. Further clinical trials in patients with renal impairment are warranted to define the role of hydration with reduced glutathione.
In conclusion, the present study indicated that reduced glutathione added to optimal hydration does not further decrease the risk of CIN in elderly patients undergoing coronary angiography or intervention. However, despite these negative results, a causal relationship may exist in the development of CIN. Well-designed studies with a larger sample size and longer follow-up should be conducted to confirm our results.
Acknowledgments
We gratefully acknowledge Dr. Ying Shan for her editorial suggestions for the article. This study was supported in part by a grant from the National Natural Science Foundation in China (#81470496).
Footnotes
First published online.
References
- 1.Maeder M, Klein M, Fehr T, Rickli H. Contrast nephropathy: review focusing on prevention. J Am Coll Cardiol. 2004;44:1763–1771. doi: 10.1016/j.jacc.2004.06.075. [DOI] [PubMed] [Google Scholar]
- 2.Mohammed NM, Mahfouz A, Achkar K, Rafie IM, Hajar R. Contrast-induced nephropathy. Heart Views. 2013;14:106–116. doi: 10.4103/1995-705X.125926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Golshahi J, Nasri H, Gharipour M. Contrast-induced nephropathy; A literature review. J Nephropathol. 2014;3:51–56. doi: 10.12860/jnp.2014.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maioli M, Toso A, Leoncini M, Gallopin M, Tedeschi D, Micheletti C, et al. Sodium bicarbonate versus saline for the prevention of contrast-induced nephropathy in patients with renal dysfunction undergoing coronary angiography or intervention. J Am Coll Cardiol. 2008;52:599–604. doi: 10.1016/j.jacc.2008.05.026. [DOI] [PubMed] [Google Scholar]
- 5.de Bie MK, van Rees JB, Herzog CA, Rabelink TJ, Schalij MJ, Jukema JW. How to reduce the incidence of contrast induced acute kidney injury after cardiac invasive procedures, a review and practical recommendations. Curr Med Res Opin. 2011;27:1347–1357. doi: 10.1185/03007995.2011.580732. [DOI] [PubMed] [Google Scholar]
- 6.Davenport MS, Cohan RH, Khalatbari S, Ellis JH. The challenges in assessing contrast-induced nephropathy: where are we now? AJR Am J Roentgenol. 2014;202:784–789. doi: 10.2214/AJR.13.11369. [DOI] [PubMed] [Google Scholar]
- 7.Heyman SN, Rosen S, Khamaisi M, Idee JM, Rosenberger C. Reactive oxygen species and the pathogenesis of radiocontrast-induced nephropathy. Invest Radiol. 2010;45:188–195. doi: 10.1097/RLI.0b013e3181d2eed8. [DOI] [PubMed] [Google Scholar]
- 8.Au TH, Bruckner A, Mohiuddin SM, Hilleman DE. The prevention of contrast-induced nephropathy. Ann Pharmacother. 2014;48:1332–1342. doi: 10.1177/1060028014541996. [DOI] [PubMed] [Google Scholar]
- 9.Han Y, Zhu G, Han L, Hou F, Huang W, Liu H, et al. Short-term rosuvastatin therapy for prevention of contrast-induced acute kidney injury in patients with diabetes and chronic kidney disease. J Am Coll Cardiol. 2014;63:62–70. doi: 10.1016/j.jacc.2013.09.017. [DOI] [PubMed] [Google Scholar]
- 10.Firouzi A, Eshraghi A, Shakerian F, Sanati HR, Salehi N, Zahedmehr A, et al. Efficacy of pentoxifylline in prevention of contrast-induced nephropathy in angioplasty patients. Int Urol Nephrol. 2012;44:1145–1149. doi: 10.1007/s11255-011-0053-4. [DOI] [PubMed] [Google Scholar]
- 11.Yavari V, Ostovan MA, Kojuri J, Afshariani R, Hamidian JA, Roozbeh J, et al. The preventive effect of pentoxifylline on contrast-induced nephropathy: a randomized clinical trial. Int Urol Nephrol. 2014;46:41–46. doi: 10.1007/s11255-013-0420-4. [DOI] [PubMed] [Google Scholar]
- 12.McCullough PA. Contrast-induced acute kidney injury. J Am Coll Cardiol. 2008;51:1419–1428. doi: 10.1016/j.jacc.2007.12.035. [DOI] [PubMed] [Google Scholar]
- 13.Jorgensen AL. Contrast-induced nephropathy: pathophysiology and preventive strategies. Crit Care Nurse. 2013;33:37–46. doi: 10.4037/ccn2013680. [DOI] [PubMed] [Google Scholar]
- 14.Dodd S, Dean O, Copolov DL, Malhi GS, Berk M. N-acetylcysteine for antioxidant therapy: pharmacology and clinical utility. Expert Opin Biol Ther. 2008;8:1955–1962. doi: 10.1517/14728220802517901. [DOI] [PubMed] [Google Scholar]
- 15.Rushworth GF, Megson IL. Existing and potential therapeutic uses for N-acetylcysteine: the need for conversion to intracellular glutathione for antioxidant benefits. Pharmacol Ther. 2014;141:150–159. doi: 10.1016/j.pharmthera.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 16.Kelly AM, Dwamena B, Cronin P, Bernstein SJ, Carlos RC. Meta-analysis: effectiveness of drugs for preventing contrast-induced nephropathy. Ann Intern Med. 2008;148:284–294. doi: 10.7326/0003-4819-148-4-200802190-00007. [DOI] [PubMed] [Google Scholar]
- 17.O'Sullivan S, Healy DA, Moloney MC, Grace PA, Walsh SR. The role of N-acetylcysteine in the prevention of contrast-induced nephropathy in patients undergoing peripheral angiography: a structured review and meta-analysis. Angiology. 2013;64:576–582. doi: 10.1177/0003319712467223. [DOI] [PubMed] [Google Scholar]
- 18.Quintavalle C, Donnarumma E, Fiore D, Briguori C, Condorelli G. Therapeutic strategies to prevent contrast-induced acute kidney injury. Curr Opin Cardiol. 2013;28:676–682. doi: 10.1097/HCO.0b013e3283653f41. [DOI] [PubMed] [Google Scholar]
- 19.Bouzas-Mosquera A, Recio-Mayoral A. Sodium bicarbonate, N-acetylcysteine, and saline for the prevention of contrast-induced nephropathy. Am Heart J. 2008;155:e31. doi: 10.1016/j.ahj.2008.01.022. [DOI] [PubMed] [Google Scholar]
- 20.Weisbord SD, Chen H, Stone RA, Kip KE, Fine MJ, Saul MI, et al. Associations of increases in serum creatinine with mortality and length of hospital stay after coronary angiography. J Am Soc Nephrol. 2006;17:2871–2877. doi: 10.1681/ASN.2006030301. [DOI] [PubMed] [Google Scholar]


