Abstract
Background
Physicians can help guide teenagers in their emerging sexuality; however, teens rarely inform physicians about their sexual activity.
Methods
We audio-recorded annual visits between 365 teenagers and 49 physicians. sexual intercourse. Recordings were coded for teenage disclosures about previous sexual intercourse. We measured agreement between telephone survey responses and annual visit disclosures, and examined factors associated with agreement between the two.
Results
Fifty-six teenagers (15%) reported previous sexual intercourse in either the telephone survey or to their physician. Among those who reported sexual intercourse, 57% shared this information to both the telephone survey and their physician (κ = .72, confidence interval = 0.63–0.82).
Conclusions
Although a slight majority of teenagers disclosed their sexual activity to both the telephone survey and their doctor, a significant number disclosed to just one source.
Keywords: adolescent, patient participation, physician-patient communication, self-disclosure, sexual behavior, telephone
Clinician inquiry about adolescent patients' sexual history is a recommended element of routine health maintenance visits.1 Positive responses to inquiry about sexual activity can trigger discussion of pregnancy and sexually transmitted infection (STI) prevention. For young women patients aged 15 years and older, reports of any lifetime sexual activity should trigger genital chlamydia screening—now a widely accepted indicator of health care quality.2 More generally, clinicians are ideal sources for confidential and reliable information about sexual health and sexual identity, disclosure of sexual abuse and assault, as well as resources for provision of contraceptives and testing/treatment for sexually transmitted infections.
However, many adolescents do not disclose sexual behavior to physicians because of concerns about confidentiality, lack of trust, or lack of understanding the importance and potential helpfulness of having these discussions.3 Many clinicians assume that adolescents will not truthfully report sexual experiences, and concerns about truthfulness are cited as reasons for omitting sexual inquiry during health maintenance visits.4 The degree to which young people report accurate information in response to clinician inquiry is therefore of direct relevance to quotidian clinical practice. Potential interventions to improve clinical sexual histories of adolescents obviously depend on whether sources of inaccuracy derive from the adolescent, the clinician, or both. We know that clinicians often fail to discuss sexual activity at all, and that discussions that do occur are quite brief.5 Less is known about the accuracy of young people's reports of sexual experience.
A major reason for this lack of understanding is a limitation in methods to verify the accuracy of clinical responses. However, methods to establish accuracy of self-reports of sexual behavior are limited. Some approaches depend on logical contradictions, during which a response is considered invalid when inconsistent with an objective marker of sex. For example, of 186 adolescent women who reported consistently using condoms during vaginal intercourse, 63 were found to have signs of sperm in their vaginal fluid.6 In a trial designed to prevent HIV/STIs, 17% of young women reported lifetime abstinence or recent abstinence from vaginal sex, yet were diagnosed with an STI.7 Other studies using this approach have found better agreement of self-reported sexual behaviors and STI, however.8,9
Other approaches to validation of reports of sexual behavior depend on response cross-verification, using consistency of information from 2 or more sources to assess responses. Between-partner studies ask both partners questions about the occurrence of sexual behaviors, condom use, and orgasm. Substantial proportions of couples disagree in their responses, especially for frequency reports.10–14 Other cross-validation approaches use inquiry about the same behavior at 2 points in time.15–18 For example, a report of lifetime sexual experience at time 1 and denial of such experience at a subsequent time 2 creates a logical inconsistency calling into question the validity of both reports. A different approach—taken in this study—uses a triangulation approach by comparing agreement in key information points obtained by 2 different methods of inquiry.
Each of these approaches has limitations. For our purposes, a major limitation is that most studies of validity of adolescents' reports of sexual behavior were done in research rather than clinical settings. If improving sexual health care of young people is to be achieved, information about accuracy of self-reports in clinical settings is needed. Given the importance of accurate determination of sexual activity, we asked whether a combination of information collection methods could improve the reliability of determinations of adolescents' sexual activity. We examined the agreement between teenagers' disclosures of sexual intercourse in a confidential telephone survey conducted shortly before disclosures to physicians during annual office visits. We further explored patient and physician factors associated with agreement in the 2 inquiry approaches.
Methods
Overview
The data for this secondary analysis come from the Teen CHAT study, a study examining how physicians counseled overweight and obese teenagers about weight change (details reported elsewhere).19 The study began in November 2009. For this study, we included all teenager annual visits audio recorded between November 2009 and October 2012. For this study, we examined teenager's answers during a confidential telephone survey conducted by study staff during which staff asked them about previous sexual intercourse. Additionally, we reviewed audio-recorded encounters to determine whether a teenager self-disclosed their past sexual activity to their physician during the visit. Our analyses examined the agreement between telephone survey answers and self-disclosures to physician of previous sexual intercourse, and whether this agreement varied according to physician, teenager, and visit factors.
Study Sample and Procedures
We approached physicians in 8 community and 3 academic medical clinics in the Raleigh/Durham/Chapel Hill, North Carolina area for participation. Eligible physicians had to see teenage patients and plan to remain in the area for at least 3 years. Once enrolled, physicians provided written consent. We reviewed medical records from the consented physicians to identify eligible teenage patients who had a visit scheduled within the next 2 weeks. Eligible teenagers were between the ages of 12 and 18 years, had a body mass index z-score ≥85th percentile for age/gender, and were not pregnant. We called teenagers and their parents to obtain verbal consent (parents or 18-year-old teenager) and assent (teenagers younger than18 years). Before the visit, teenagers completed a confidential baseline telephone survey that included self-reported items relating to sexual intercourse. The teenager's visit was then audio-recorded.
Measures
Before their visit, study staff conducted a confidential telephone survey with teenagers during which teenagers were asked whether they have ever engaged in sexual intercourse. We also audio-recorded the teenager's annual visits and assessed whether the teenager told their physician if they ever engaged in sexually intercourse. Examples of self-disclosures to physicians ranged from statements such as “I am having sex,” “I need birth control because my boyfriend and I are having sex.” We also coded “Well, I am no longer sexually active” as “yes,” which occurred only once.
Analysis
We examined the associations of physician, teenager, and parent characteristics with confirming self-disclosures about previous sexually intercourse to the telephone survey or physician as well as the agreement between the telephone survey and physician answers. First, we calculated the kappa coefficient for agreement between telephone survey and physician disclosure. Second, we conducted multivariate logistic regression controlling for clustering within physicians to examine which variables were associated with agreement between telephone survey answers and self-disclosures to physicians during the annual visit.
Results
Most physicians were pediatricians (90%), 61% were female, 88% were white, they were on average 40.9 years old, and on average had been 12.5 years out of medical school. Teenagers averaged 14 years of age and evenly divided by gender (51% female). About half of the teenagers were African American, almost 40% were white, 8% identified themselves a multiracial, and 4% as other (see Table 1).
Table 1.
Physician and Teenager Characteristics.
| Variables | Physician (N = 49) | Teenager (N = 365) |
|---|---|---|
| Years since medical school, mean (SD) | 12.5 (9.1) | |
| Age, years, mean (SD) | 40.9 (8.5) | 14.3 (1.7) |
| Female, % | 61 | 51 |
| Black, % | 6 | 49 |
| White, % | 88 | 38 |
| Multiracial, % | 0 | 8 |
| Other, % | 6 | 4 |
| Pediatrician, % | 90 | |
| Female physician, % | 61 |
Fifty-six teenagers self-disclosed to either the telephone survey or their physician that they had sex intercourse. Forty-nine teenagers reported in the telephone survey that they had sexual intercourse (see Figure 1) and 32 of those teenagers disclosed this information to both the telephone survey and physician that they had had sexual intercourse. Twenty-four teenagers told their physician they had sex. Seventeen teenagers disclosed previous sexual intercourse in the telephone survey but not to their physicians. Finally, 7 teenagers disclosed to their physician they had had sexual intercourse but did not report this in the telephone survey. Interestingly, teens were less likely to report on the telephone survey that they had had sexual intercourse when their physician was a pediatrician (odds ratio [OR] = 0.25, confidence interval [CI] = 0.15–0.42). The level of agreement between answers indicates a significant level of agreement between telephone survey answers and self-disclosures to physicians greater than chance (κ = .69, CI = 0.57–0.81).
Figure 1.
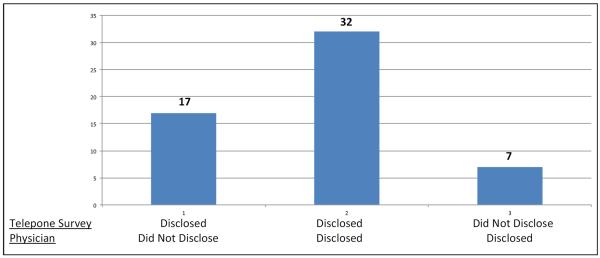
Consistency between teenagers' telephone survey answers and self-disclosures to their physician.
Table 2 shows the results of a logistic regression examining associations of teenagers' agreement between confidential disclosures to the telephone survey of previous sexual intercourse and verbal self-disclosure of sexual intercourse to their physician adjusted for teenagers clustered within physicians. Three variables were significantly associated with teenagers being consistent in their reporting about prior sexual intercourse: more years since medical school graduation led to more consistent teen disclosure (OR = 1.04, CI = 1.01–1.07); older teenagers were less likely to be consistent about their sexual experience (OR = 0.71, CI = 0.62–0.82); and females were also less likely to be consistent in reporting their sexual behavior (OR = 0.61, CI = 0.37–0.98).
Table 2.
Multivariate Logistic Regression: Factors Associated With Teenagers' Self-Report of Previous Sexually Intercourse.
| Agreement Between Telephone Survey Answers and Self-Disclosures to Physicians |
||
|---|---|---|
| Variables | Odds Ratio | Confidence Interval |
| MD pediatrician | 0.57 | 0.18–1.82 |
| Years since medical school | 1.04 | 1.01–1.07* |
| Teenagers | ||
| Age | 0.71 | 0.62–0.82** |
| Female | 0.61 | 0.37–0.99* |
p < 0.05
p < 0.001
Discussion
While there is no practical way to know for certain whether a teenager in this sample had previous sexual intercourse, we were able to examine the agreement between their answers on a confidential telephone survey and self-disclosures to their physician. We found that when teenagers reported previous sexual intercourse on a telephone survey, only half of the time did they tell their physician. Teenagers were less likely to report previous sexual intercourse to the telephone survey when their physician was a pediatrician. Agreement between telephone survey and physician answers was associated with seeing a physician who has been out of medical school longer. Older teenagers and females were less likely to be consistent in their responses to the telephone survey and their physician about previous sexual intercourse.
Our data suggest that teenager disclosures on a confidential telephone survey and their physician about previous sexual intercourse agreed greater than chance; yet, 43% of the time the answers were inconsistent. Teenagers gave more consistent self-disclosures of previous sexual intercourse to physicians who have been in practice longer. Two factors could be at play. First, experienced physicians may have greater skill at establishing trusting relationships with teenagers that encourages teenagers to be honest in their disclosures. Second, longer time in practice could also be a marker for a longer relationship with the teenager that has enabled such a trusting relationship to develop.
Older teenagers, who are more likely to be having sexual intercourse, are less likely to report it. It may be that they may not disclose sexual activity because they want to maintain boundaries between themselves and adult authority figures as they gain great personal autonomy as they age. Females may be less likely to disclose that they have had sexual intercourse due to the greater societal stigma on sexually active female adolescents than that on sexually active male adolescents.
The decision to disclose sexual intercourse is a difficult and complex one for teenagers. It is highly likely that more teenagers were sexually active in our sample than those who self-disclosed it.7 With physicians under increasing pressure to see more patients in less time, it may become more difficult for them to build trusting relationships with teenagers that would allow teenagers to assess them as safe persons to whom they could disclose their sexual activity and from whom they could receive helpful and nonjudgmental advice.
Limitations
There are a number of limitations to our study. First, the answers were all self-reported and cannot be confirmed. Second, we asked and examined disclosures only about sexual intercourse. Thus, our question excluded a lot of other sexual behaviors and activities in which teenagers may be engaging. Third, our sample consisted solely of teenagers who were either overweight or obese (ie, >85th weight percentile). This may influence generalizability to other teenagers; however, there is little evidence to suggest that teenager weight changes a teenagers' willingness to report sexual intercourse. Finally, because visits were audio recorded, it is possible that the presence of the recorder may have discouraged teenagers from disclosing their sexual behavior.
Conclusion
Not all teenagers disclose their sexual intercourse to their physicians during the annual visits. In our sample, in an anonymous survey, 49 teenagers reported having had sex, but during their physician visit only three-fourths of those teenagers verbally reported having previously had sex. Thus, physicians are not always hearing about sexual activity and this may affect their ability to provide adequate sexual health care.
Teenagers are reluctant to disclose sexual intercourse to their physicians, even when they are willing to admit they are sexually active to unfamiliar study staff during a confidential survey. One of the best approaches to help teenagers understand the need for sharing sexual activity to their physicians is for physicians to explain confidentiality and conduct confidential discussions during each visit. Confidential discussions allow for teenagers to have safe environments to talk about sexuality, sexual identity, and sexual activity.20 For physicians, this requires confidential discussions for all health visits.
Acknowledgments
Funding The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by grant R01HL092403.
Footnotes
Author Contributions SCA, conceptualized and designed the study, coordinated and supervised the transcription and coding of audio recordings, drafted the initial manuscript, and approved the final manuscript. JDF conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted. KIP designed the data collection instruments, coordinated and supervised data collection, and reviewed the final manuscript as submitted. TO, JAT, RD and TB critically reviewed the manuscript and approved the final manuscript as submitted. CGS conceptualized and designed the study, carried out the latent class analyses and binary, multinomial logistic regression models, drafted the initial manuscript, and approved the final manuscript as submitted.
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Hagan J, Shaw J, Duncan P, editors. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 3rd ed American Academy of Pediatrics; Elk Grove Village, IL: 2008. [Google Scholar]
- 2.Meyers D, Wolff T, Gregory K, et al. USPSTF recommendations for STI screening. Am Fam Physician. 2008;77:819–824. [PubMed] [Google Scholar]
- 3.Greene K. An integrated model of health disclosure decision-making. In: Afifi TAW, editor. Uncertainty and Information Regulation in Interpersonal Contexts: Theories and Applications. Routledge; New York, NY: 2009. pp. 226–253. [Google Scholar]
- 4.Henry-Reid LM, O'Connor KG, Klein JD, Cooper E, Flynn P, Futterman DC. Current pediatrician practices in identifying high-risk behaviors of adolescents. Pediatrics. 2010;125:e741–e747. doi: 10.1542/peds.2009-0271. [DOI] [PubMed] [Google Scholar]
- 5.Alexander SC, Fortenberry JD, Pollak KI, et al. Sexuality talk during adolescent health maintenance visits. JAMA Pediatr. 2014;168:163–169. doi: 10.1001/jamapediatrics.2013.4338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rose E, DiClemente RJ, Wingood GM, et al. The validity of teens' and young adults' self-reported condom use. Arch Pediatr Adolesc Med. 2009;163:61–64. doi: 10.1001/archpediatrics.2008.509. [DOI] [PubMed] [Google Scholar]
- 7.Brown JL, Sales JM, DiClemente RJ, et al. Predicting discordance between self-reports of sexual behavior and incident sexually transmitted infections with African American female adolescents: results from a 4-city study. AIDS Behav. 2012;16:1491–1500. doi: 10.1007/s10461-012-0163-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Orr D, Fortenberry J, Blythe M. Adolescent women using biomarker outcomes. Sex Transm Dis. 1997;24:261–266. doi: 10.1097/00007435-199705000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Kahn J, Goodman E, Kaplowitz R, Slap G, Emans S. Validity of adolescent and young adult self-report of Papanicolaou smear results. Obstet Gynecol. 2000;96:625–631. doi: 10.1016/s0029-7844(00)00987-x. [DOI] [PubMed] [Google Scholar]
- 10.Drumright L, Gorbach P, Holmes K. Do people really know their sex partners? Concurrency, knowledge of partner behavior, and sexually transmitted infections within partnership. Sex Transm Dis. 2004;31:437–442. doi: 10.1097/01.olq.0000129949.30114.37. [DOI] [PubMed] [Google Scholar]
- 11.Seal D. Interpartner concordance of self-reported sexual behavior among college dating couples. J Sex Res. 1997;34:39–55. [Google Scholar]
- 12.Ellen J, Vittinghoff E, Bolan G, Boyer C, Padisan N. Individuals' perceptions about their sex patners' risk behaviors. J Sex Res. 1998;35:328–332. [Google Scholar]
- 13.Niccolai L, Farley T, Ayoub M, Magnus Y, Kissinger P. HIV-infected persons' knowledge of their sexual partners' HIV status. AIDS Educ Prev. 2002;14:183–189. doi: 10.1521/aeap.14.3.183.23893. [DOI] [PubMed] [Google Scholar]
- 14.Harvey S, Bird S, Henderson J, BEckman L, Juszti H. He said, she said: concordance between sexual partners. Sex Transm Dis. 2004;31:185–191. doi: 10.1097/01.olq.0000114943.03419.c4. [DOI] [PubMed] [Google Scholar]
- 15.Graham M, Friedman S, Neaigus A, Jose B, Ildefonso G, Curtis R. Recalling sexual behavior: a methodological analysis of memory recall bias via interview using the diary as the gold standard. J Sex Res. 2003;40:325–332. doi: 10.1080/00224490209552198. [DOI] [PubMed] [Google Scholar]
- 16.Carey M, Casey K, Maisto S, Gordon C, Weinhardt L. Assessing sexual risk behavior with the Timeline Followback (TLFB) approach: Continued development and pyychometric evaluation with psychiatric outpaitents. Int J STDs AIDS. 2001;12:365–375. doi: 10.1258/0956462011923309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schrimshaw E, Roasrio M, Meyer-Bahlburg H, Schraf-Matlick A. Test-retest reliability of self-reported sexual behavior, sexual orientation, and psychosexual milestones among gay, lesbian, and bisexual youths. Arch Sex Behav. 2006;35:225–234. doi: 10.1007/s10508-005-9006-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vanable P, Carey M, Brown J, et al. Test-retest reliability of self-reported HIV/STD-related measures among African-American adolescent in the four U.S. cities. J Adolesc Health. 2009;44:214–221. doi: 10.1016/j.jadohealth.2008.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bravender T, Tulsky JA, Farrell D, et al. Teen CHAT: development and utilization of a web-based intervention to improve physician communication with adolescents about healthy weight. Patient Educ Couns. 2013;93:525–531. doi: 10.1016/j.pec.2013.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McKee M, Rubin S, Campos G, O'Sullivan LF. Challenges of providing confidential care to adolescents in urban primary care: clinician perspectives. Ann Fam Med. 2011;9:37–43. doi: 10.1370/afm.1186. [DOI] [PMC free article] [PubMed] [Google Scholar]


