Abstract
A chondrosarcoma in the anterior mediastinum is a rare finding with a relatively good prognosis. We describe a case of a 75-year-old man with a 2-year history of neck discomfort and weight loss. Imaging showed a homogenous tumor with a minor compression on the anterior part of the heart. It had close relation to the ribs, no surrounding fat, and a thymoma was suspected. Biopsy prior to surgery was impossible due to the location of the tumor. Unfortunately, final pathology from the surgical specimen revealed a chondrosarcoma.
Keywords: Thorax, computed tomography (CT), positron emission tomography (PET), mediastinum, neoplasms – primary
Introduction
Tumors of the anterior mediastinum are most frequently metastases originating from lymphatic spread of other cancers, but a variety of primary tumors may also be seen. Thymomas account for approximately 50% of primary tumors, while 20% are lymphomas, parathyroid or thyroid tumors, germ cell neoplasms, and neurogenic tumors (1). Thymomas are associated with myasthenia gravis and approximately 15–20% of patients with thymoma have clinical symptoms while another 25% have elevated biomarkers (2). Chondrosarcoma is the third most common primary malignant bone tumor which is most frequently found in the pelvis and long bones. Extra skeletal chondrosarcomas represent 2% of all soft tissue sarcomas and are most often found in the thoracic wall (3). We present a rare case of a chondrosarcoma in the anterior mediastinum.
Case report
A 75-year-old man with a 2-year history of intermittent chest discomfort, irritation from the left side of the neck, pain when swallowing, and a non-intentional weight loss of 3 kg in the last 3 months, was referred to an ear, nose, and throat specialist due to a suspicion of a tonsillar cancer. A physical exam and a computed tomography (CT) scan of the neck, chest, and abdomen were performed.
CT revealed a 4.3 × 2.6 × 3.3 cm, round, well-defined tumor with smooth borders in the anterior mediastinum with close relation to the ribs (Fig. 1). A low dose CT scan had been performed 4 years earlier, where the tumor had been overlooked (Fig. 2). Since then it had doubled its size. Positron emission tomography (PET-)CT was performed and showed a mean standardized uptake value of 1.57 with a maximum of 1.89 in the tumor indicating a low risk of malignancy. A thymoma was considered as diagnosis (Fig. 3). A neurophysiological examination was performed due to suspicion of myasthenia gravis, but did not reveal any abnormalities. No laboratory findings could support the suspicion of myasthenia. The tumor was not accessible for CT-guided biopsy and it could not be diagnosed on ultrasound due to poor visualization. Despite the lack of positive laboratory findings for myasthenia, the patient was referred under the diagnosis of myasthenia gravis for surgical removal of the suspected thymoma.
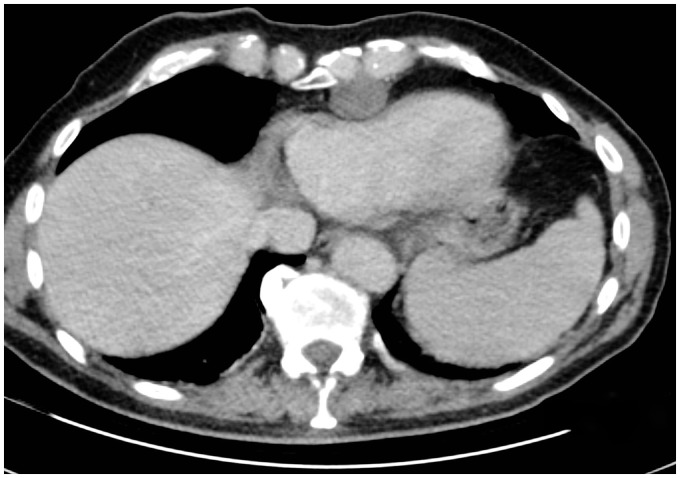
Fig. 1.
Second CT scan of the chondrosarcoma. Tumor makes a slight compression of the heart.
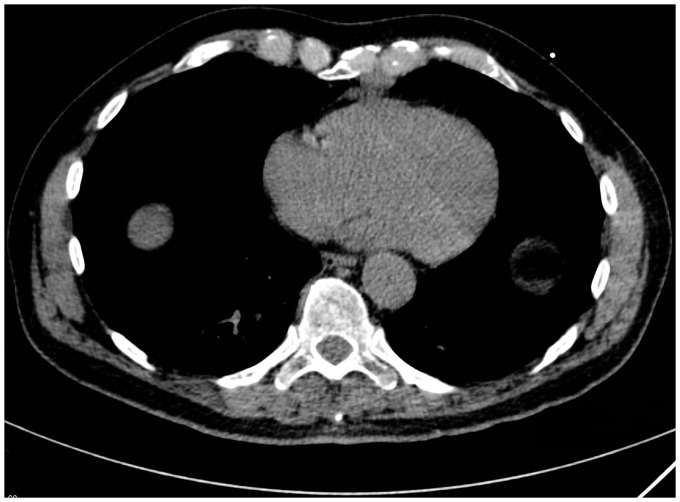
Fig. 2.
CT scan of the chondrosarcoma performed 4 years prior to diagnosis. Tumor is visible anterior to the heart, but unfortunately overlooked.
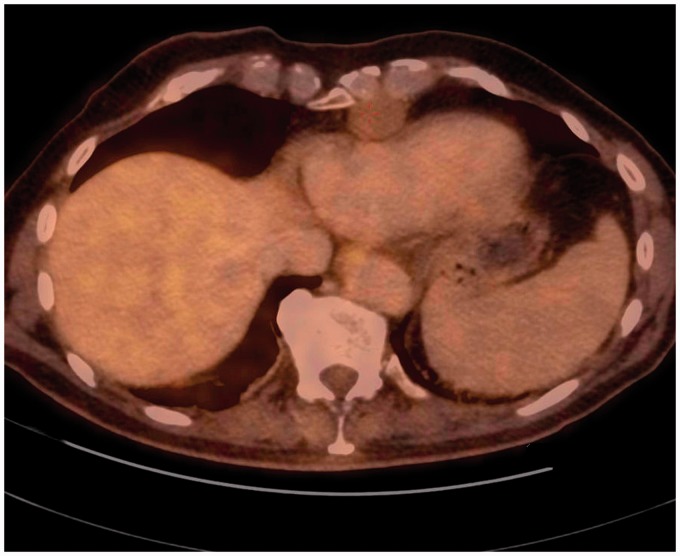
Fig. 3.
PET-CT scan showing a slight FDG uptake in the tumor with a minor compression of the heart.
At surgery the tumor looked like a benign, cartilaginous mass and not like a thymoma. A right-sided video-assisted thoracoscopic surgery (VATS) procedure was performed and the tumor was biopsied. Frozen sections revealed a benign cartilaginous tumor possibly an enchondroma and the tumor was removed. Final pathology revealed a grade 1 chondrosarcoma and the patient underwent surgery again where a larger area of the thoracic wall was resected.
A 6-month follow-up magnetic resonance imaging (MRI) scan revealed no signs of tumor.
Discussion
We have described a rare case of a chondrosarcoma originating from the cartilaginous part of the ribs, which has only been reported twice previously. The tumor in the reported case was strongly suspected to originate from the cartilaginous part of the ribs due to the localization on the CT scan where it was not in connection with the sternum. A search in PubMed revealed eight cases of chondrosarcoma in the anterior mediastinum: two cases originating from the sternum (4,5); one believed to arise from cartilage (6); one from the thyroid cartilage (7); and four without relation to ribs or sternum (8–11). All tumors were described as heterogeneous masses on CT without cystic components, but with calcifications. Five of the cases had initial symptoms of chest pain while two had impaired breathing. In our case the tumor was homogeneous, without calcifications and with low Hounsfield values (HU 17) indicating fluid/cysts. It is possible that the chest pain that led to the first CT scan was caused by the chondrosarcoma.
Most often tumors of the anterior mediastinum are metastases from lung, breast, thyroid, or renal cancers. The incidence of chondrosarcomas is only 0.5 in 1 million but it is the most common primary tumor of the thoracic wall (12). Small thymomas are often well-defined, non-infiltrating, and soft tumors without calcifications. Usually they respect their surroundings and are clearly separated from these by fat, but 30–40% are invasive (13). In this case the tumor’s close relation to cartilage, the missing fat, the irregular form, and the compression on the heart could indicate that the tumor was not a thymoma. Other differential diagnoses could have been pericardial cyst, teratoma/dermoid cyst, unicentric debut of Castleman disease, or a cystic thymoma.
The primary treatment of a chondrosarcoma is surgical resection because this tumor is resistant to radiation and chemotherapy. The prognosis for a grade 1 condrosarcoma is good with a 5-year survival of 90% (13). Due to the risk of local recurrence a wide surgical margin is recommended when resecting sarcomas of the thoracic wall.
In conclusion, a chondrosarcoma in the anterior mediastinum is a rare, but is a possible finding that should be kept in mind when diagnostic criteria of more commonly occurring tumors are not met.
Acknowledgements
The authors thank Dorthe C Skovgaard, Thora Buhl, and Lisbeth L Knudsen (Department of Radiology, Gentofte) for their help with and description of the PET-CT image.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Müller S, Silva C. Imaging of the chest, 2nd edn New York, NY: Saunders Elsevier, 2008, pp. 1473–1524. [Google Scholar]
- 2.Fujii Y. Thymus, thymoma and myasthenia gravis. Surg Today 2013; 43: 461–466. [DOI] [PubMed] [Google Scholar]
- 3.Greenspan A. Orthopedic Imaging: A Practical Approach, 5th edn Philadelphia, PA: Lippincott Williams & Wilkins, 2010, pp. 727–735. [Google Scholar]
- 4.Alpert JB, Nonaka D, Chachoua A, et al. Increasing dyspnea due to an anterior mediastinal mass. Chest 2011; 139: 217–223. [DOI] [PubMed] [Google Scholar]
- 5.Nosotti M, Rosso L, Mendogni P, et al. Reconstruction for unusual chondrosarcoma: innovative technique. J Cardiothorac Surg 2012; 7: 40–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Phillips GWL, Choong M. Case report: Chondrosarcoma presenting as an anterior mediastinal mass. Clin Radiol 1991; 43: 63–64. [DOI] [PubMed] [Google Scholar]
- 7.Guillem P, Porte H, Copin MC, et al. A case of giant chondrosarcoma of the cricoid cartilage presenting as a superior mediastinal tumour. Eur J Cardiothorac Surg 1998; 14: 520–522. [DOI] [PubMed] [Google Scholar]
- 8.Ozkaya S, Furtun K, Yuksel C, et al. An unusual cause of precordial chest pain. Case Rep Pulmonol 2013; 2013: 342096–342096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mulligan CR, Jr, Tavaf-Motamen H, Stewart R, et al. Chondrosarcoma masquerading as cardiomyopathy. Ann Thorac Surg 2008; 86: 297–299. [DOI] [PubMed] [Google Scholar]
- 10.Jindal T, Chaudhary R, Sharma N, et al. Primary mediastinal chondrosarcoma with Horner’s syndrome. Gen Thorac Cardiovasc Surg 2011; 59: 145–147. [DOI] [PubMed] [Google Scholar]
- 11.Jeong SS, Choi PJ, Kim DW, et al. Primary extraskeletal mesenchymal chondrosarcoma of the anterior mediastinum. Korean J Pathol 2013; 47: 492–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Widhe B, Bauer HCF. Scandinavian Sarcoma Group. Surgical treatment is decisive for outcome in chondrosarcoma of the chest wall: a population-based Scandinavian Sarcoma Group study of 106 patients. J Thorac Cardiovasc Surg 2009; 137: 610–614. [DOI] [PubMed] [Google Scholar]
- 13.Stoller D, Tirman P, Bredella M, et al. Diagnostic Imaging: Orthopaedics, 1st edn Salt Lake City, UT: AMIRSYS, 2003, pp. 35–38. [Google Scholar]